Abstract
Mindfulness and meditation was explored with the view to support the use of trauma-sensitive mindfulness (TSM) in clinical practice with survivors of war refugees in the treatment of post-traumatic stress disorders. The following questions were explored: (1) How are mindfulness and meditation defined? (2) What are the practices and perceived value of mindfulness practices? (3) What are the evidence and non-evidence-based treatments for post-traumatic stress disorder (PTSD)? (4) What are the possibilities of using TSM to support war-traumatised refugees in the treatment of PTSD in a refugee camp setting? Findings that measured currently actioned interventions for war-traumatised refugees did not account for psychological support that could be implemented in a refugee camp setting on a once-off basis. In response to the gaps and limitations highlighted, the study suggests an adaptation of the TSM intervention and professional development of practitioners in the art of TSM therapy.
1. Introduction
More than 5.6 million Syrians have fled the country as refugees, and another 6.2 million people have been displaced within Syria [1], creating one of the largest refugee and displacement crises. According to Lindert et al. [2] (p. 374), during displacement, before being forced to flee, refugees may experience imprisonment, torture, loss of property, malnutrition, physical assault, extreme fear, rape, and loss of livelihood. Communities have been destroyed by disrupting core attachments to families, friends, and cultural systems. The impact of these stressors on mental health is confounded by exposure to violent, traumatic events in the flight itself. Many of those refugees, especially female refugees, and unaccompanied minors, are likely to be exposed to a wide variety of violent events.
The increasing need for psychological services to address the mental health needs of war-traumatised refugees is paramount to attending to their physical and social needs. Due to their foundations, methods, adaptability to the times and the number of refugees that require urgent psychological assistance to address mental health challenges which arise from trauma, mindfulness-based interventions such as trauma-sensitive mindfulness (TSM) have provided unique and appropriate responses to the inimitable challenges experienced by war-traumatised refugees.
This article explores the construct of mindfulness and how the clinical practice thereof was adapted to meet the limited time frame to provide psychological interventions to war-traumatised refugees during a relief mission. The restrictions of the relief missions highlight the need to endorse trauma-sensitive mindfulness as an intervention to meet the once-off sessions with war-traumatised refugees. The article aims to synthesise the research evidence for this postmodern form of therapeutic intervention for supporting war trauma survivors who receive psychological support at relief missions. It has been developed to provide a map of the existing literature in an attempt to clarify the working definitions and conceptual boundaries of this technique and its applications for TSM interventions. The study is part of a larger study that has reported on the use of TSM in Syria with approximately 70 war-traumatised refugees over a period of 10 days. Case study reports of those experiences are reported elsewhere.
2. Materials and Methods
In order to define mindfulness as a construct, it was necessary to achieve an understanding of the foundations of mindfulness. This led to accessing literature on Buddhist psychology, which provided a thick description of the concept of Vipassana, which is a Sanskrit term for insight meditation which preceded the concept of mindfulness. This understanding of the application of Vipassana created a need to understand the traditional meditation practices and the theoretic framework which guides them. Meditation as a construct, the definition, and the theoretical framework of Buddhist meditation, was therefore explored. Furthermore, the application of Vipassana and transition into mindfulness were thereafter clarified. Once clarity was achieved on the concept of meditation, and the transition of Vipassana into the concept of mindfulness, literature examining the adaptation of mindfulness-based interventions into TSM was investigated.
3. Results
3.1. Mindfulness Definitions and Applications
Follette, Palm and Pearson [3] indicate that mindfulness is originally a construct used in Eastern spiritual and philosophical traditions that have found new utility in psychotherapy practice. The authors explain that mindfulness practices have recently been applied to the treatment of several psychological and health-related problems, and research shows successful outcomes in psychological interventions incorporating mindfulness practices. Lin [4] highlights that, in the field of psychology, the studies drawing on Eastern philosophies have been the most successful (in the sense of having received the most acceptance from the scientific community) as the studies are centred on empirical validation of Asian techniques.
3.1.1. Meditation and Mindfulness
The concepts of meditation and mindfulness are very similar [5]. While meditation typically involves the practice of accessing a different state of consciousness, mindfulness means becoming aware of the present moment. Both meditation and mindfulness practices are renowned for reducing anxiety because the combination of the practices permits the reduction of stress without increasing distress [6]. Meditation used in the treatment of anxiety disorders typically takes the form of mindfulness-based meditation. This type of meditation was founded by Jon Kabat-Zinn, the founder of the approach to mindfulness-based stress reduction. Kabat-Zinn [6] demonstrated that the basic premise of the mindfulness-based stress-reduction approach is to learn to detach from anxious thoughts. This is achieved by practising awareness, identifying tension in the body, understanding thinking patterns and learning how to deal with challenging emotions.
A further conceptualisation of mindfulness proposed a two-component model. One component involves self-regulation of attention to the experience of the present moment, and the other involves adopting an orientation of openness and acceptance toward one’s experience [7]. Therefore, these interventions teach mindfulness skills to increase intentional attention, develop a different relationship with one’s thoughts and practise different strategies in relation to distressing thoughts and emotions in a non-judgemental way. Shapero et al. [8] explain that mindfulness meditation is steeped in centuries of Buddhist practices and philosophy. In the late 20th century, these practices were incorporated into Western interventions to treat physical and mental illnesses.
Mindfulness-based interventions teach how to pay attention and become more aware of internal emotions instead of allowing them to dominate thoughts and actions. Through mindfulness intervention, the identification of when and what emotional states or feelings of distress are most intense is achievable. This identification can help in the acceptance of the moment, letting the emotions pass or reduce in intensity so that it becomes easier to use the other skills needed.
Several definitions of mindful meditation theory describe mindful meditation to be the training of your concentration by bringing non-judgemental awareness or focusing on a single object of attention [6,9,10]. Mindfulness meditation often uses breath, sound, or physical sensations to train concentration. Mosby’s Medical Dictionary (2013) [11] (p. 35) defines mindful meditation as "a technique of meditation in which distracting thoughts and feelings are not ignored but are rather acknowledged and observed nonjudgmentally as they arise to create a detachment from them and gain insight and awareness".
Nhat Hanh in Kabat-Zinn [6] defines mindful meditation as a practice that shows us what is happening in our bodies, our emotions, our minds and in the world. Nhat Hanh explains that through the practice of mindfulness, we avoid harming ourselves and others. Kabat-Zinn [6] supports the definition of mindful meditation by describing the practice as the act of paying attention in a particular way: on purpose, in the present moment and non-judgementally.
3.1.2. Mindfulness Theory
Mindfulness-based practices have become globally prevalent over the past decade. However, as supported by Fossas [12], research indicates that the origins of mindfulness meditation practices extend approximately 2500 years into the past, and they have firm origins in Hinduism and Buddhism. The diagram (Figure 1) below provides a timeline which indicates the transition of the clinical application of mindfulness as an intervention from its origins to the present application of the practice.
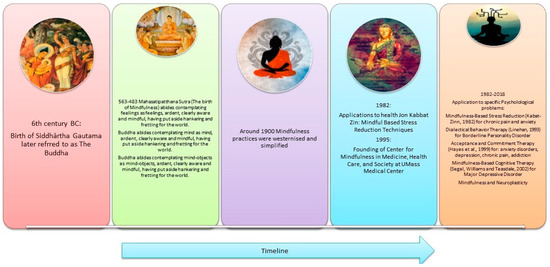
Figure 1.
Timeline of the transition of the clinical adaptation of mindfulness practice [13].
Although this study acknowledges a brief historical introduction of Eastern philosophies into Western societies, the discussion of the transition of the clinical application of mindfulness mainly focuses on the clinical adaptation of mindfulness practices as an intervention. Research from Miles (2013), Frey and Spakowski (2016), and Borup (2013); highlights increased interest in Eastern philosophies and associated mind-body practices in the 1960s that were noted with the arrival of the countercultural revolution (including Qigong, Tai Chi, Transcendental Meditation, Chakra Meditation, numerous Yoga traditions, breathwork and other breathing techniques, various martial arts forms from many East Asian cultures, Buddhist meditation and other practices). The arrival of rishis, gurus, senseis, Buddhist monks and many other expert practitioners and scholars from these Asian cultures to Western shores piqued interest in Eastern-based practises. They thus created subsequent travels of many Westerners to these cultures to apprentice and learn various Eastern techniques and bring them to the West, such as the United States of America and Europe in the 1960s.
Knight [14] (p. 5) explains the importance of mindfulness in the human experience. Mindfulness technologies have been applied in human endeavours over the decades. They have been found to be of great value by Hindus, Buddhists, Muslims, and Christians; in India, Asia, Europe and America, and in the far past, in the Middle Ages and in modern times. The depth and breadth of human experience with mindfulness technologies argue very powerfully for their intrinsic worth in solving problems of inner experiences, which is arguably the metier of clinical psychology [14].
The translation of the Sanskrit term ′Vipassana meditation, which is also known as insight meditation, translates into "to see things as they really are" [15]. It is a process of self-purification by self-observation [16]. A clarification provided by Thatcher [15] defines insight meditation as being concerned with the present consciousness, in other words, being conscious of the present moment and “staying in the now” to the most extreme degree possible. It consists of observing the body (rupa) and mind (nama) with bare attention and is an ancient technique derived from India, which was originally taught by the Buddha. This method was pre-eminently taught in the Buddhist term Satipatthana Sutta, the most important discourse taught by the Buddha on meditation and practice in everyday life. The essence of this practice is the moment-to-moment awareness of the rise and fall of all mind-body phenomena. Thus, Satipatthana and Vipassana are virtually synonymous.
Knight [14] simplifies the interpretation of mindfulness to be an English word which defines a technique for profoundly changing our relationship with our thoughts and feelings and the perspective one gains from practising that technique. It names a temporary state that is potentially accessible to any human being and a set of permanent traits that may grow in a person who practices mindfulness. Brown et al. [17] explain that the term ‘mindfulness’ derives from the Pali word sati meaning “to remember” but as a mode of consciousness, it commonly signifies presence of mind.
Brown et al. [17] (p. 7) clarify that:
“The concept of mindfulness is most firmly rooted in Buddhist psychology, but it shares conceptual kinship with ideas advanced by a variety of philosophical and psychological traditions, including ancient Greek philosophy; phenomenology, existentialism, and naturalism in later Western European thought; and transcendentalism and humanism in America”.
The four noble truths of Buddhism reflect the following themes that are echoed in mindfulness practice. Therefore, a brief discussion of the four noble truths and the link to the noble eightfold path is provided to illustrate how Eastern philosophy is integrated into a Western adaptation known as a mindfulness practice. A summary of the four noble truths provided for this study are:
- (a)
- The truth of suffering
- (b)
- The truth of the cause of suffering
- (c)
- The truth at the end of suffering
- (d)
- The truth of the path that leads to the end of suffering
Referring to the fourth noble truth, Buddhist teachings [18] acknowledge that the path that leads to the end of suffering is achievable through an understanding of the practice of the noble eightfold path. A brief understanding of the concepts of the noble eightfold path is necessary as they link to the understanding of mindfulness teachings. The summary of the concepts is supported by Kumar [18] and Brown [19], who found that each path of the noble eightfold path is relevant to the approach of using mindfulness as a treatment, such as a clinical application to reduce the effects of trauma. The authors′ guide that the eightfold path focuses on bodily sensations, states of mind and interactions between behaviour and the environment.
Traditionally, mindfulness is referred to as ‘sati’, which is linked to awareness or attention to both our mental and physical states. Mindfulness is thus viewed as focused attention on private experiences to achieve calmness and stability [6]. Feelings and thoughts are observed and brought into awareness without being judged, analysed, suppressed, or ignored. Mindfulness meditation is considered a method to achieve commitment, willingness, and awareness to experience emotional distress, referred to as the Buddhist notion of suffering by being present. Practising behaviours that create both pleasant and unpleasant experiences allows one to be aware of the changing emotions and, thus, the impermanent nature of both positive and negative circumstances. This approach is based on the core understanding of other clinical practices, such as acceptance-based therapy, discussed by Brown [17], who clarifies that:
“The concept of mindfulness is most firmly rooted in Buddhist psychology, but it shares conceptual kinship with ideas advanced by a variety of philosophical and psychological traditions, including ancient Greek philosophy; phenomenology, existentialism, and naturalism in later Western European thought; and transcendentalism and humanism in America”.
Mindfulness is thus viewed as being rooted in the fundamental activities of consciousness with a particular focus on attention and awareness.
3.1.3. Mindfulness Practice and Its Value
Tang and Posner [18] conducted a study on mindfulness meditation known as integrative body-mind training (IBMT), which confirmed improved mood changes along with increased brain-signalling connections after practising 11 h of IBMT. They also found an expansion of myelin, the protective fatty tissue that surrounds the nerves, in the brain’s anterior cingulate region. Deficits in the activation of this area of the brain have been associated with attention deficit disorder, dementia, depression, schizophrenia, and many other disorders.
Hölzel et al. [19] found that mindfulness meditation alters the structure of the brain. The study reported that eight weeks of mindfulness-based stress reduction (MBSR) was found to increase cortical thickness in the hippocampus, which governs learning and memory and in certain areas of the brain that play a role in emotion regulation and self-referential processing [19]. Decreases in brain cell volume in the amygdala were also evident, which is responsible for fear, anxiety, and stress. Consequently, changes in brain structure were congruent with the participants’ self-reports of their stress levels, indicating that meditation not only changes the brain but also changes our subjective perceptions and feelings.
With reference to both IBMT and neurological, structural alterations of the brain, the polyvagal theory provided by Porges [20] examines the neurological components of PTSD and mindfulness-based interventions. According to Porges [20], "Basic safety is essential not only for having satisfying relationships but also for optimally activating the higher brain structures responsible for creativity and generativity".
Previous research conducted by Lazar [21] on American men and women who meditated a mere 40 min a day showed that they had thicker cortical walls than non-meditators. What this meant is that their brains were ageing at a slower rate. Cortical thickness is also associated with decision-making, attention, and memory.
Hunot et al. [22] provide an evidenced-based understanding of mindfulness as the “third wave behaviourism” and state that third-wave approaches use strategies such as mindfulness exercises (e.g., body scan, mindfulness of senses meditation), acceptance of unwanted thoughts and feelings and/or cognitive diffusion (stepping back and seeing thoughts as just thoughts) to elicit change in the thinking process and to reduce symptoms of specific disorders.
Hunot et al. [22] state that the “third wave of behaviourism” integrates mindfulness and acceptance techniques with behavioural activation and cognitive change technologies from the first and second waves. These treatments are evidence-based, meaning that research trials have proven their effectiveness in reducing the suffering caused by many kinds of psychological problems.
Peteet [23] discusses the conceptual, practical, and ethical challenges of a "fourth wave" of psychological therapies, which rests on a foundation of existential, humanistic and spiritual/religious philosophies. This approach to positive psychology interventions comprises the themes of compassion-focused therapy, loving-kindness meditation, meaning-focused and spiritually-informed treatments, and various strength-based and virtue-centred interventions (e.g., treatments that promote dignity, forgiveness, gratitude, and hope).
In support of Peteet’s findings, Emamzadeh [24] states that unlike older interventions (e.g., psychodynamic, or cognitive behavioural therapy) and their predominant concern with treating dysfunction, this latest wave of therapies also aims to increase one’s general sense of well-being.
Follette et al. [3] hypothesise that the population which would theoretically benefit from mindfulness practice in treatment consists of individuals who have experienced traumatic events and are exhibiting PTSD and/or related correlates of past trauma. This theoretical finding supports the aim of this study which provides mindfulness-based interventions for the trauma experienced by refugees and the secondary trauma experienced by humanitarian volunteers who provide medical support to refugees.
The experiments from the studies above have advanced the understanding of different phenomena such as brain plasticity, and—as a curiosity—gamma waves have been documented with intensity for the first time in the history of science. In addition, psychological proposals drawing inspiration from Eastern worldviews are also numerous and significant; for example, in psychotherapy, Cortright [25] highlights Carl Jung and Michael Washburn’s new analytical psychology; Stanislav Grof’s holotropic model; Ken Wilber’s spectrum model; Hameed Ali’s diamond approach; Roberto Assagioli’s psychosynthesis; and other transpersonal (existential, psychoanalytic, and body-centred) approaches.
3.1.4. TSM Definitions and Practices in the Treatment of PTSD
The principle of TSM is supported by case studies in Treleaven [26], which illustrate the ways mindfulness can help or hinder trauma recovery. Treleaven [26] provides insights into five key principles for TSM, namely attention, arousal, relationship, dissociation and social context within a trauma-informed practice.
Mindfulness meditation—practised without an awareness of trauma—can exacerbate symptoms of traumatic stress [26]. He explains that if clients are instructed to pay close, sustained attention to their inner world, survivors may experience flashbacks, dissociation and even re-traumatisation. To address the need for TSM, Treleaven [26] (p. 8) states:
"Before we can respond to trauma, we first need to recognise it. As mindfulness providers, it′s up to us to notice nonverbal cues that someone is struggling with traumatic stress. Because of the way mindfulness meditation is generally practiced, this presents a unique challenge. Mental health professionals can assess trauma through direct conversation—reading facial expressions and noticing nonverbal cues—but silent meditation practice minimises such contact. Those of us teaching mindfulness to groups rely heavily on observation”.
Treleaven [26] proposes techniques of observation and intervention-based dialogues that assist therapists in fostering an environment of trauma sensitivity when employing the practice of mindfulness intervention for trauma. Mindfulness-based treatments for PTSD have emerged as promising adjunctive or alternative intervention approaches. Boyd, Lanius, and McKinnon [27] provided a review of the literature on PTSD treatment studies, including approaches such as MBSR, mindfulness-based cognitive therapy and metta mindfulness, a Pali term which refers to positive energy and kindness to others, which revealed low attrition with medium to large effect sizes. Boyd et al. [27] examined the convergence between neurobiological models of PTSD and neuroimaging findings in the mindfulness literature, where mindfulness interventions may target emotional under and overmodulation, both of which are critical features of PTSD symptomatology. The result of the study indicated that mindfulness-based treatments have proven to be effective in restoring connectivity between large-scale brain networks among individuals with PTSD, including connectivity between the default mode network and the central executive and salience networks [27].
Lang, Strauss, Bomyea, Bormann, Hickman, Good, and Essex [28] discuss three components of mindfulness that may promote recovery from PTSD, including attention, a mindful cognitive style and non-judgement. The authors specify how mindfulness, or intentional shifting of attention to the present moment, fosters a capacity for attentional control and may lead to reductions in attentional bias to trauma-related stimuli.
3.1.5. Trauma and Polyvagal Theory
According to Porges’ polyvagal theory, the existence of unresolved trauma in our past results in a perpetual state of fight or flight [29]. The polyvagal theory implies that fight-or-flight anxiety can be projected by engaging in activities. However, for some trauma survivors, no activity successfully channels their fight-or-flight sensations. As a result, they feel trapped, and their bodies shut down; these clients may live in a version of perpetual shutdown. Levine′s [30] consideration of Porge’s polyvagal theory offered somatic experience as a treatment for trauma and traumatised patients. Levine developed an approach that focuses on including, and putting emphasis on, the physiological aspects of trauma. Concerning Porge’s theory, Levine believes that working with the trauma through the body is necessary for any trauma resolution and a required step before addressing emotional and cognitive issues. Levine [30] explains that emerging from shutdown requires a somatic experience, such as a shudder or shake, to discharge suspended fight-or-flight energy. He proposes that "during a life-threatening situation if we have shut down and an opportunity for active survival presents itself, we can wake ourselves up" [30] (p. 26).
Both Levine and Porges highlight the necessity of encouraging the activation of the parasympathetic nervous system in an attempt to encourage clients to transition from a traumatic state to one of safety. Based on his understanding of the effects of the vagus nerve, Porges [31] notes that extending exhales longer than inhales for some time activates the parasympathetic nervous system, which helps clients who are stuck in forms of a fight-or-flight response to move into a sense of safety.
The theories put forward by Levine et al. [32] suggest that focused breathing and movement are recommended as an attempt to encourage clients to transit from a state of traumatic immobility to a sense of safety. Similarly, Grossman et al. [33] concur that a structured group programme should employ mindfulness meditation practices, such as awareness of breath, to alleviate suffering associated with physical, psychosomatic and psychiatric disorders.
Lucas et al. [34] (p. 5) confirm that the polyvagal theory serves as the foundation for the mindfulness-based movement:
“Recruiting and exercising the social engagement system is the ‘go-to’ default activity that humans use to modulate stress. This capacity resides within the social engagement system because positive face-to-face interactions activate neural pathways through the vagus nerve that downregulate the sympathetic activation associated with both exercise and stress”.
Similar findings from van der Kolk (2015) support the notion of the physiological effects of trauma and the changes in the biological stress response. Van der Kolk presents his findings of how veterans and their families are affected by trauma and highlight scientific studies that indicate how trauma changes the body and the brain, which impacts the capacity to experience pleasure, engagement, self-control and trust. The author encourages body-mind integrated interventions such as meditation as the evidence provided shows encouraging changes in neuroplasticity. Van der Kolk’s research has explored a variety of therapeutic approaches, including many mind-body and other approaches (including MDMA, yoga, neurofeedback, hypnosis, eye movement desensitisation and reprocessing, and brief eclectic psychotherapy) as a treatment for PTSD experienced by both adults and children.
Brown et al. [9] point out that mindfulness awareness involves the conscious registration of events and experiences and that it is our most proximal contact with reality.
TSM is informed by the polyvagal theory as it considers the relationship between the sympathetic and parasympathetic nervous systems in the aftermath of trauma. Treleaven [26] explores how mindfulness can exacerbate symptoms of traumatic stress if not modified skilfully and explains how to modify practices by offering 36 specific modifications designed to support survivors’ safety and stability.
3.1.6. Mindfulness from the Perspective of Polyvagal Theory
Lucas et al. [34] argue that from the perspective of polyvagal theory, mindfulness-based movements function as a neural exercise in which the physiological state is manipulated by exercise, social engagement and mindfulness-focused attention. During calm states in which the social engagement system is functioning, the social cues from voice and face maintain a physiology of safety characterised by a strong vagal influence on the heart that supports health, growth and restoration.
Exercise requires an increase in cardiac output through both the removal of vagal inhibition and an increase in sympathetic influences on the heart. The time course of alternating physical activity and social engagement behaviours provides opportunities to exercise the neural regulation of the autonomic nervous system. Through the repeated withdrawal of vagal inhibition to support movement and the recovery of vagal inhibition, the autonomic nervous system develops and promotes a more efficient shift from a physiological state of arousal to calm.
3.1.7. Mindfulness Meditation and Neuroplasticity: The East-Meets-West Dichotomy
According to Siegel [35] (p. 113), “Neuroplasticity is the term used to describe the capacity for creating new neural connections and growing neurons in response to experience.” It occurs throughout the lifespan as we are consistently exposed to experiences.
Neurophysiology of mindfulness training has attempted to map out possible changes in brain pathways associated with changes in behaviour related to the neuroplasticity of mindfulness. As stated by Cayoun [36] (p. 39):
“Neuroplasticity is the capacity of neurons to adapt to a changed environment (FitzGerald & Folan-Curran, 2002). According to Hebbian learning, pre-synaptic terminals change in numbers according to usage and each learning experience strengthens existing neuronal connections (Hebb, 1949).”
A randomised controlled study by Davidson [37] measured the effects of mindfulness training on brain and immune functions in healthy employees of a biotechnology firm. The group trained with mindfulness showed significant increases in activation in the left prefrontal region post-treatment, which lasted up to four months. As shown by previous research, regions of the left prefrontal cortex are associated with the arousal of pleasant emotions such as fun, kindness and compassion, whereas the right prefrontal cortex is associated with the arousal of unpleasant emotions (anger, fear, sadness, etc.) [37]. There was no such effect in the control group. The maintenance of this change highlights the role of mindfulness training in inducing neuroplasticity in pathways necessary for the self-regulation of emotions.
Cayoun [36] explains that in the clinical environment, when clients learn to practise the body scan techniques as part of mindfulness training [6,36], they usually report an increased ability to feel sensations throughout the body, including those that were previously below an awareness threshold; e.g., increased perception of internal states or introspection [6]. What is most remarkable is the persistence of this ability following long periods during which training has stopped. This effect is usually termed “between session plasticity” [38].
3.1.8. Available Psychological Interventions for War-Traumatised Refugees
Evidence-based and non-evidenced-based interventions for war-traumatised refugees that are currently implemented are recorded below. The tables highlight that there is a lack of information and literature on mindfulness-based interventions that can be adapted to cater to a once-off session to accommodate relief mission time limitations. With reference to the available psychological interventions for war-traumatised refugees, Nocon et al. [39] (pp. 5–6) examined the effect of 13 out of 23 studies which implemented evidence-based treatments. Table 1 indicates the various available evidence-based treatments for trauma that have been updated and reformed over 15 years.

Table 1.
Evidence-based treatments for PTSD adapted from Nocon et al. (2017) [39].
Table 2 illustrates the non-evidence-based treatment examined by Nocon et al. [39], either in the experimental or the control condition. Meditation and relaxation techniques, which are synonymous with mindfulness-based techniques are shown, however, information about the use of TSM has not been included in these treatments.

Table 2.
Non-evidence-based treatments for PTSD adapted from Nocon et al. [39].
Nocon et al. [39] (illustrated in both Table 1 and Table 2) concluded that given the considerable number of children and adolescents displaced by war, there were regrettably few treatment studies available, and many of them were of low methodological quality. The effect sizes lagged the effects observed in traumatised minors in general and often were small or non-significant. However, CBT and IPT showed capable results that need further replication. Nocon’s findings support the need to implement further evidence-based treatments for trauma. Regarding the findings provided by Nocon, the study provides information on the use of mindfulness-based interventions as an evidence-based treatment for trauma that can also be adapted for a once-off session during the conditions of relief missions.
The studies examined by Nocon et al. [39] provided findings which measured interventions that were implemented over a few sessions with war-traumatised refugees. The study did not account for interventions that can be implemented in a refugee camp setting in which war-traumatised refugees could only be assisted with psychological assistance on a once-off basis [39].
Although there is no stipulation on the prescribed duration of TSM as a mindfulness-based intervention, Treleaven [26] informs that the adaptation of TSM involves trauma-sensitive informed mindfulness to assist clients in understanding physical sensations; improve self-regulation; ease their experiences of trauma, and cultivate mindfulness during regular therapeutic sessions or during a 6–8 week mindfulness-based intervention programme to ascertain the client’s experience of their practice of the techniques that are explored during sessions.
4. Discussion
Van der Kolk [62] and Porge’s polyvagal theory [20] offers an understanding of how trauma is experienced as an integrative process which affects the brain and the body. The research provided by the authors supports mindfulness as an intervention to address the integrated conflict experienced by trauma. Trauma-sensitive mindfulness techniques allow for the ethical implementation of mindfulness techniques to adequately address challenges derived from trauma or symptoms related to PTSD.
Although the literature provided on current methods used to address PTSD, such as CBT, has the most empirical support for the treatment of trauma, a gap in the adaptability of such techniques on a once-off basis, such as during relief missions, is not provided. Trauma-sensitive mindfulness provides an adaptive intervention that addresses the complexities of trauma that offers a necessary modification to both the brain and body. For the purpose of the study, the researcher examined the necessary training needed to endorse such a treatment on a once-off basis for war-traumatised refugees.
Treleaven [26] cautions that while mindfulness does not cause trauma, it may uncover it. The practices by which mindfulness is pursued can land trauma survivors in difficulty. The author highlights the necessity to implement TSM as an intervention to minimise the potentially harmful effects of re-traumatising survivors. In response to the caution raised about using mindfulness as an intervention for trauma, Treleaven [26] proposed using TSM as a response to adverse reactions to mindfulness meditation.
5. Conclusions
This article begins by providing a conceptualisation of Buddhist psychology as the theoretical framework of mindfulness practices and links it to trauma, the polyvagal theory and possible changes in brain pathways associated with changes in behaviour related to the neuroplasticity of mindfulness.
To indicate research gaps and limitations, the article examined current available psychological interventions for war-traumatised refugees, which indicated that although few treatment studies for the treatment of PTSD for war-traumatised refugees were available, many treatments were of low methodological quality. The findings discussed indicated that CBT and IPT showed capable results that need further replication. However, the article examined research which indicated that insufficient trained psychological assistance is available to treat the population of refugees that experience PTSD in refugee camp settings.
The article, therefore, highlighted findings by Nocon et al. [39] illustrated in Table 1 and Table 2, which measured currently actioned interventions that have been implemented over a few sessions with war-traumatised refugees. It did not account for interventions that can be implemented or adapted in a refugee camp relief mission setting, in which war-traumatised refugees could only be assisted with psychological assistance on a one-off basis, yet they were enabled to continue mindfulness practices independently thereafter. In response to the gaps and limitations highlighted, the suggestion is made for an adaptation of the TSM intervention for the treatment of PTSD for war-traumatised refugees by educational psychologists. Adequate training in mindfulness-based interventions for educational psychologists is further highlighted as extremely important so that trained practitioners will be able to observe and intervene in any distress that clients may experience to prevent clients from experiencing further trauma.
Author Contributions
Writing Original Draft: L.J.-D.; Supervision and reviewing: V.M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The manuscript is part of a larger study that was conducted in accordance with the National Research Ethics Committee of THE UNIVERSITY OF JOHANNESBURG (SEM 1-2021-128).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Vision. From the Field: Syrian Refugee Crisis: Facts, FAQs, and How to Help. 2018. Available online: https://www.worldvision.org/refugees-news-stories/syrian-refugee-crisis-facts (accessed on 10 July 2022).
- Lindert, J.; Carta, M.G.; Schäfer, I.; Mollica, R.F. Refugees mental health. A public mental health challenge. Eur. J. Public Health 2016, 26, 374–375. [Google Scholar] [CrossRef]
- Follette, V.; Palm, K.M.; Pearson, A.N. Mindfulness and trauma: Implications for treatment. J. Ration. -Emot. Cogn. -Behav. Ther. 2006, 24, 45–61. [Google Scholar] [CrossRef]
- Lin, Y.; Swanson, D.P.; Rogge, R.D. The Three Teachings of East Asia (TTEA) Inventory: Developing and Validating a Measure of the Interrelated Ideologies of Confucianism, Buddhism, and Taoism. Frontiers in Psychology: Cultural Psychology 2021. 2021. Available online: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.626122/full (accessed on 12 July 2022).
- Cuncic, A. The Anxiety Workbook: A 7-Week Plan to Overcome Anxiety, Stop Worrying, and End Panic; Althea Press: Emeryville, CA, USA, 2017. [Google Scholar]
- Kabat-Zinn, J. Coming to Our Senses: Healing Ourselves and the World Through Mindfulness; Hyperion: New York, NY, USA, 2005. [Google Scholar]
- Sigel, D.; Bryson, T. The Whole-Brain Child: 12 Revolutionary Strategies to Nurture Your Child′s Developing Mind; Bantam Books Trade Paperbacks: New York, NY, USA, 2012. [Google Scholar]
- Shapero, B.G.; Greenberg, J.; Pedrelli, P.; de Jong, M.; Desbordes, G. Mindfulness-Based Interventions in Psychiatry. Focus 2018, 16, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological wellbeing. J. Personal. Soc. Psychol. 2003, 8, 822–848. [Google Scholar] [CrossRef]
- Greenberg, M. The Stress-Proof Brain: Master Your Emotional Response to Stress Using Mindfulness and Neuroplasticity; Raincoast Books/New Harbinger: Vancouver, BC, Canada, 2017. [Google Scholar]
- Mosby. Mosby’s Medical Dictionary, 9th ed.; Mosby Elsevier: St. Louis, MO, USA, 2013. [Google Scholar]
- Fossas, A. The Basics of Mindfulness: Where did IT Come from? Available online: https://welldoing.org/article/basics-of-mindfulness-come-from (accessed on 19 July 2022).
- Jeebodh-Desai, L. The Implementation Of Trauma-Sensitive Mindfulness By An Educational Psychologist To Address Post-Traumatic Stress Disorder (Ptsd) Of War-Traumatised Refugees. Doctoral Dissertation, University of Johannesburg, Johannesburg, South Africa, 2022. [Google Scholar]
- Knight, F.L.M. Mindfulness: History, Technologies, Research, Applications. Techniques of Psychotherapy; Pepperdine University: Malibu, CA, USA, 2010. [Google Scholar]
- Thatcher, C. (Ed.) Insight Meditation: Practical Steps to Ultimate Truth; Vipassana Dhura Meditation Society: Aurora, CO, USA, 2011; Available online: https://www.vipassanadhura.com/PDF/practicalsteps.pdf (accessed on 10 May 2022).
- Goenka, S.N. Ten Discourses on Vipassana Meditation; Vipassana Mediation Association: India. 2013. Available online: https://www.dhamma.org/en-US/index (accessed on 18 July 2022).
- Brown, K.W.; Ryan, R.M.; Creswell, J.D. Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychol. Inq. 2007, 18, 211–237. [Google Scholar] [CrossRef]
- Tang, Y.-Y.; Hölzel, B.K.; Posner, M.I. The neuroscience of mindfulness meditation. Nat. Rev. Neurosci. 2015, 16, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Hölzel, B.K.; Carmody, J.; Vangel, M.; Congleton, C.; Yerramsetti, S.M.; Gard, T.; Lazar, S.W. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011, 191, 36–43. [Google Scholar] [CrossRef]
- Porges, S.W. The polyvagal perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef] [PubMed]
- Lazar, S.W.; Kerr, C.E.; Wasserman, R.H.; Gray, J.R.; Greve, D.N.; Treadway, M.T.; McGarvey, M.; Quinn, B.T.; Dusek, J.A.; Benson, H.; et al. Meditation experience is associated with increased cortical thickness. Neuroreport 2005, 16, 1893–1897. [Google Scholar] [CrossRef]
- Hunot, V.; Moore, T.H.M.; Caldwell, D.M.; Furukawa, T.A.; Davies, P.; Jones, H.; Honyashiki, M.; Chen, P.; Lewis, G.; Churchill, R. “Third wave” cognitive and behavioural therapies versus other psychological therapies for depression. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef]
- Peteet, J.R. A fourth wave of psychotherapies: Moving beyond recovery toward well-being. Harv. Rev. Psychiatry 2018, 26, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Emamzadeh, A. The Fourth Wave of Psychotherapies: The Challenges Associated with the Latest Group of Psychotherapies. Psychology Today. [Blog Posted 18 April 2018]. Available online: https://www.psychologytoday.com/intl/blog/finding-new-home/201804/the-fourth-wave-psychotherapies (accessed on 10 June 2022).
- Cortright, B. Integral Psychology: Yoga, Growth, and Opening the Heart; State University of New York Press: Albany, NY, USA, 2007; Available online: https://www.amazon.com/Integral-Psychology-Opening-Transpersonal-Humanistic/dp/0791470725?asin=0791470725&revisionId=&format=4&depth=1 (accessed on 12 July 2022).
- Treleaven, D.A. Trauma-Sensitive Mindfulness: Practices for Safe and Transformative Healing; W.W. Norton: New York, NY, USA, 2018. [Google Scholar]
- Boyd, J.E.; Lanius, R.A.; McKinnon, M.C. Mindfulness-based treatments for posttraumatic stress disorder: A review of the treatment literature and neurobiological evidence. J. Psychiatry Neurosci. 2018, 43, 7–25. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.J.; Strauss, J.L.; Bomyea, J.; Bormann, J.E.; Hickman, S.D.; Good, R.C.; Essex, M. The theoretical and empirical basis for meditation as an intervention for PTSD. Behav. Modif. 2012, 36, 759–786. [Google Scholar] [CrossRef] [PubMed]
- Wagner, D. Polyvagal Theory in Practice. 2016. Counselling Today. Available online: https://ct.counseling.org/2016/06/polyvagal-theory-practice/ (accessed on 5 July 2022).
- Levine, P.A. Waking the Tiger: Healing Trauma: The Innate Capacity to Transform Overwhelming Experiences; North Atlantic Books: London, UK, 1997. [Google Scholar]
- Porges, S.W. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation; W. W. Norton: New York, NY, USA, 2011. [Google Scholar]
- Levine, P.; Porges, S.W.; Phillips, M. Healing Trauma and Pain through Polyvagal Science. 2015. Available online: https://maggiephillipsphd.com/Polyvagal/EBookHealingTraumaPainThroughPolyvagalScience.pdf (accessed on 5 June 2022).
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J. Psychosom. Res. 2004, 57, 35–43. [Google Scholar] [CrossRef]
- Lucas, A.R.; Klepin, H.D.; Porges, S.W.; Rejeski, J. Mindfulness-based movement: A Polyvagal perspective. Integr. Cancer Ther. 2016, 17, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Siegel, D.J. The Mindful Therapist: A Clinician′s Guide to Mindsight and Neural Integration (Norton Series on Interpersonal Neurobiology); W. W. Norton: New York, NY, USA, 2010. [Google Scholar]
- Cayoun, B. Mindfulness-integrated CBT: Principles and Practice; John Wiley & Sons: London, UK, 2011. [Google Scholar] [CrossRef]
- Davidson, R.J.; Kabat-Zinn, J.; Schumacher, J.; Rosenkrantz, M.; Muller, D.; Santorelli, S.F.; Sheridan, J.F. Alterations in brain and immune function produced by mindfulness meditation. Psychosom. Med. 2003, 65, 564–570. [Google Scholar] [CrossRef]
- Sanes, J.N.; Donoghue, J.P. Plasticity and primary motor cortex. Annu. Rev. Neurosci. 2000, 23, 393–415. [Google Scholar] [CrossRef]
- Nocon, A.; Eberle-Sejari, R.; Unterhitzenberger, J.; Rosner, R. The effectiveness of psychosocial interventions in war-traumatized refugee and internally displaced minors: Systematic review and meta-analysis. Eur. J. Psychotraumatol. 2017, 8, 1388709. [Google Scholar] [CrossRef]
- Šehović, M. Evaluation of results of cognitive-behavioural therapy with traumatised children of dis-placed persons. In The Psychosocial Consequences of War: Results of Empirical Research from the Territory of Former Yugoslavia; Powell, S., Durakovic-Belko, E., Powell, S., Durakovic-Belko, E., Eds.; Otisak d.o.o.: Sarajevo, Bosnia-Herzegovina, 2002; pp. 265–266. [Google Scholar]
- Oras, R.; de Ezpeleta, S.C.; Ahmad, A. Treatment of traumatized refugee children with Eye Movement Desensitization and Reprocessing in a psychodynamic context. Nordic J. Psychiatry 2004, 58, 199–203. [Google Scholar] [CrossRef]
- Onyut, L.P.; Neuner, F.; Schauer, E.; Ertl, V.; Odenwald, M.; Schauer, M.; Elbert, T. Narrative Exposure Therapy as a treatment for child war survivors with posttraumatic stress disorder: Two case reports and a pilot study in an African refugee settlement. BMC Psychiatry 2005, 5, 7. [Google Scholar] [CrossRef]
- Ehntholt, K.A.; Smith, P.A.; Yule, W. School based cognitive-behavioural therapy group intervention for refugee children who have experienced war-related trauma. Clin. Child Psychol. Psychiatry 2005, 10, 235–250. [Google Scholar] [CrossRef]
- Möhlen, H.; Parzer, P.; Resch, F.; Brunner, R. Psychosocial support for war-traumatized child and adolescent refugees: Evaluation of a short-term treatment program. Aust. N. Z. J. Psychiatry 2005, 39, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Catani, C.; Kohiladevy, M.; Ruf, M.; Schauer, E.; Elbert, T.; Neuner, F. Treating children traumatized by war and Tsunami: A comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry 2009, 9, 22. [Google Scholar] [CrossRef]
- Schauer, E. Trauma Treatment for Children in War: Build-up of an Evidence-Based Large-Scale Mental Health Intervention in North-Eastern Sri Lanka. Doctoral Dissertation, University of Konstanz, Konstanz, Germany, 2008. [Google Scholar]
- Schottelkorb, A.A.; Doumas, D.M.; Garcia, R. Treatment for childhood refugee trauma: A randomized, controlled trial. Int. J. Play. Ther. 2012, 21, 57–73. [Google Scholar] [CrossRef]
- Ooi, C.S. The Efficacy and Social Validity of A Group Cognitive Behavioural Therapy for Young Migrants from War-Affected Countries. Doctoral Dissertation, Curtin University, Perth, Australia, 2012. [Google Scholar]
- Tol, W.A.; Komproe, I.H.; Jordans, M.J.D.; Vallipuram, A.; Sipsma, H.; Sivayokan, S.; Macy, R.D.; de Jong, J.T. Outcomes and moderators of a preventive school-based mental health intervention for children affected by war in Sri Lanka: A cluster randomized trial. World Psychiatry Off. J. World Psychiatr. Assoc. 2012, 11, 114–122. [Google Scholar]
- Betancourt, T.S.; Newnham, E.A.; Layne, C.M.; Kim, S.; Steinberg, A.M.; Ellis, H.; Birman, D. Trauma history and psychopathology in war-affected refugee children referred for trauma-related mental health services in the USA. J. Traumatic Stress 2012, 25, 682–690. [Google Scholar] [CrossRef]
- Ooi, C.S.; Rooney, R.M.; Roberts, C.; Kane, R.T.; Wright, B.; Chatzisarantis, N. The efficacy of a group cognitive behavioral therapy for war-affected young migrants living in Australia: A cluster randomized controlled trial. Front. Psychol. 2016, 7, 1641. [Google Scholar] [CrossRef]
- Pfeiffer, E.; Goldbeck, L. Evaluation of a Trauma-Focused Group Intervention for Unaccompanied Young Refugees: A Pilot Study. J. Traumatic Stress 2017, 30, 531–536. [Google Scholar] [CrossRef]
- O’Shea, B.; Hodes, M.; Down, G.; Bramley, J. A school-based mental health service for refugee children. Clin. Child Psychol. Psychiatry 2000, 5, 189–201. [Google Scholar] [CrossRef]
- Dybdahl, R. Children and mothers in war: An outcome study of a psychosocial intervention program. Child Dev. 2001, 72, 1214–1230. [Google Scholar] [CrossRef]
- Šestan, D. Participation in a program of psychosocial support and reduction of posttraumatic symptoms in preschool children and their mothers. In The Psychosocial Consequences of War: Results of Empirical Research from the Territory of Former Yugoslavia; Powell, S., Durakovic-Belko, E., Eds.; Otisak d.o.o.: Sarajevo, Bosnia-Herzegovina, 2002; pp. 255–257. [Google Scholar]
- Thabet, A.A.; Vostanis, P.; Karim, K. Group crisis intervention for children during ongoing war conflict. Eur. Child Adolesc. Psychiatry 2005, 14, 262–269. [Google Scholar] [CrossRef]
- Fazel, M.; Doll, H.; Stein, A. A school-based mental health intervention for refugee children: An exploratory study. Clin. Child Psychol. Psychiatry 2009, 14, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Betancourt, T.S.; Newnham, E.A.; Brennan, R.T.; Verdeli, H.; Borisova, I.; Neugebauer, R.; Bass, J.; Bolton, P. Moderators of treatment effectiveness for war-affected youth with depression in northern Uganda. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2012, 51, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Kalantari, M.; Yule, W.; Dyregrov, A.; Neshatdoost, H.; Ahmadi, S.J. Efficacy of writing for recovery on traumatic grief symptoms of Afghani refugee bereaved adolescents: A randomized control trial. Omega 2012, 65, 139–150. [Google Scholar] [CrossRef]
- Lange-Nielsen, I.I.; Kolltveit, S.; Thabet, A.A.M.; Dyregrov, A.; Pallesen, S.; Johnsen, T.B.; Laberg, J.C. Short-term effects of a writing intervention among adolescents in Gaza. J. Loss Trauma 2012, 17, 403–422. [Google Scholar] [CrossRef]
- Ellis, B.H.; Miller, A.B.; Abdi, S.; Barrett, C.; Blood, E.; Betancourt, T.S. Multi-tier mental health program for refugee youth. J. Consult. Clin. Psychol. 2013, 81, 129–140. [Google Scholar] [CrossRef]
- Van der Kolk, B. The Body Keeps the Score: Brain, Mind and Body in the Healing of Trauma; Penguin Books: New York, NY, USA, 2015. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).