Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures
Abstract
1. Introduction
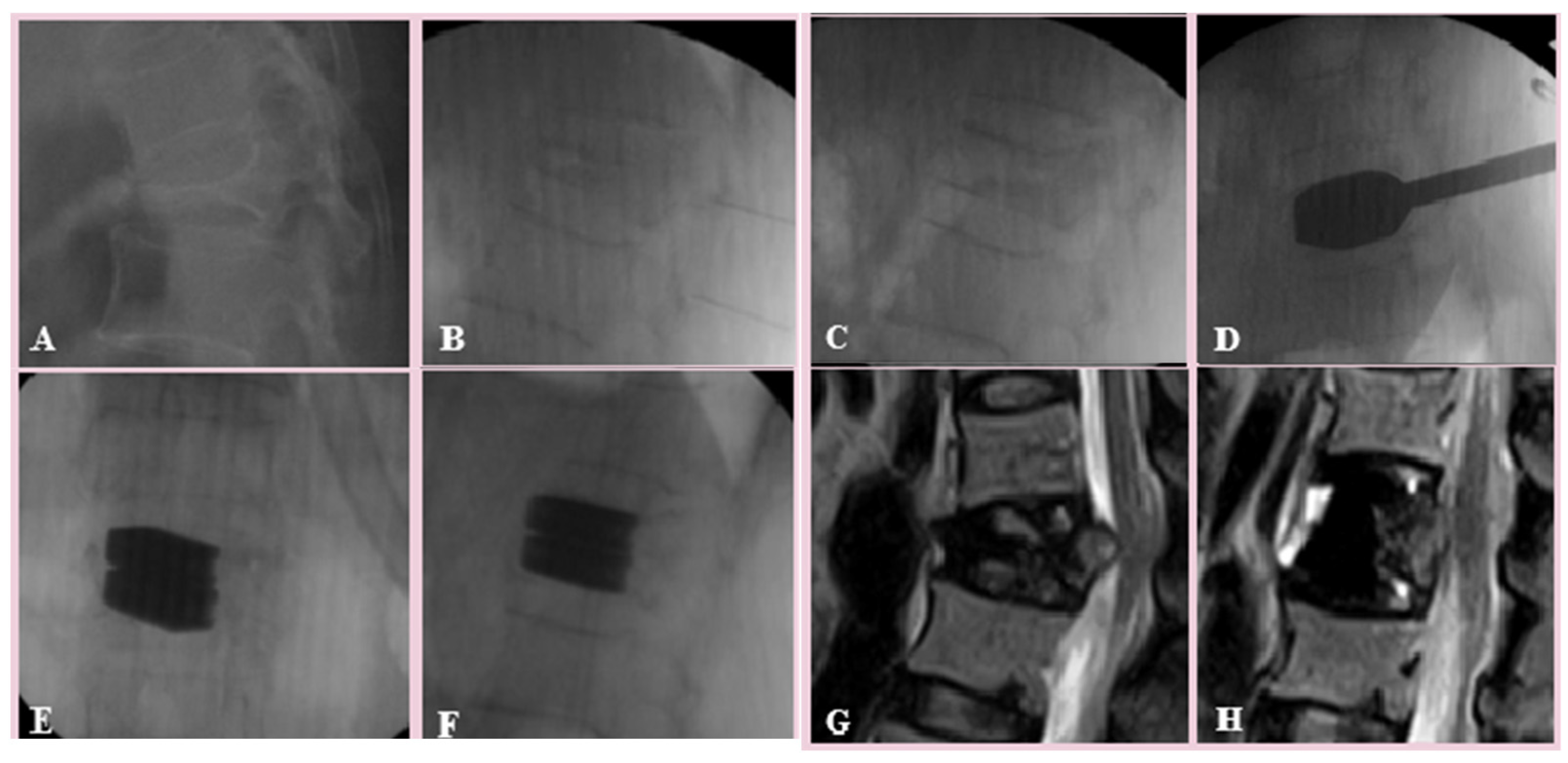
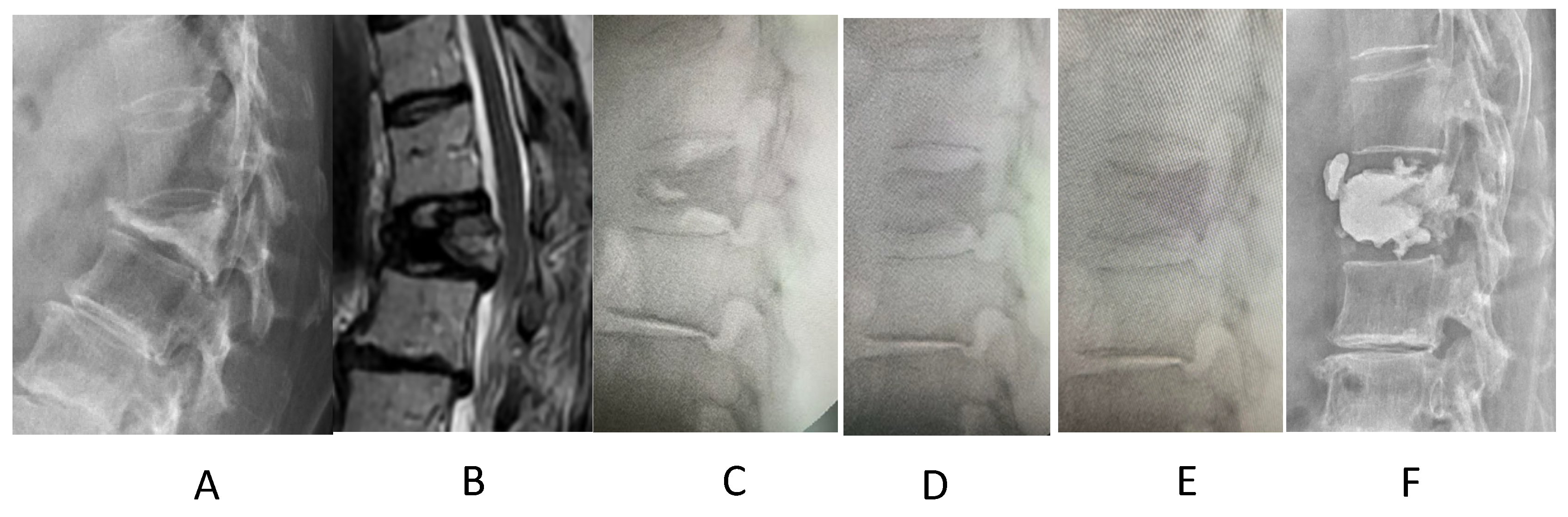
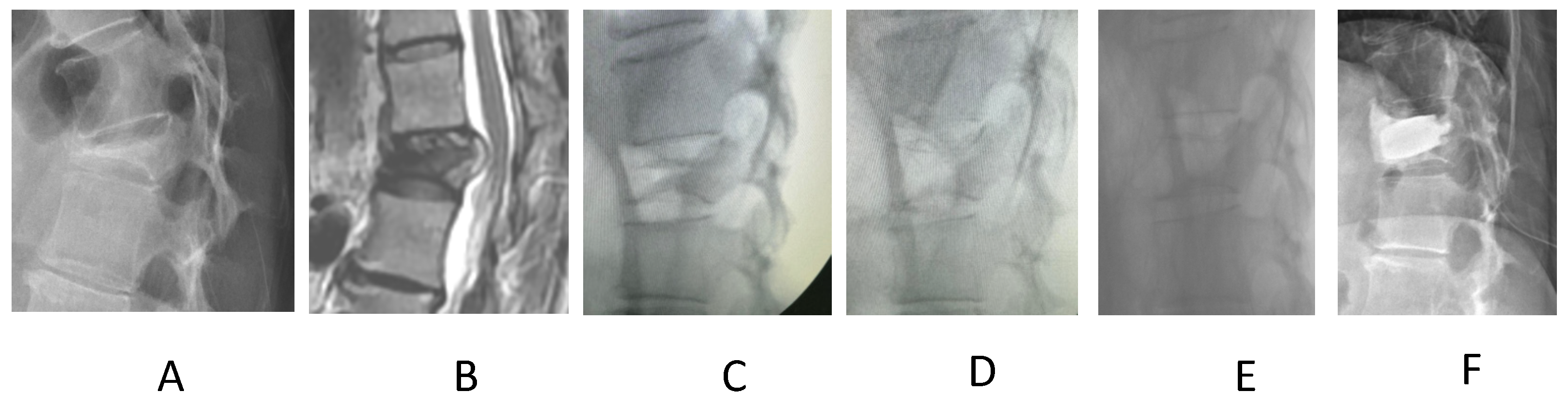
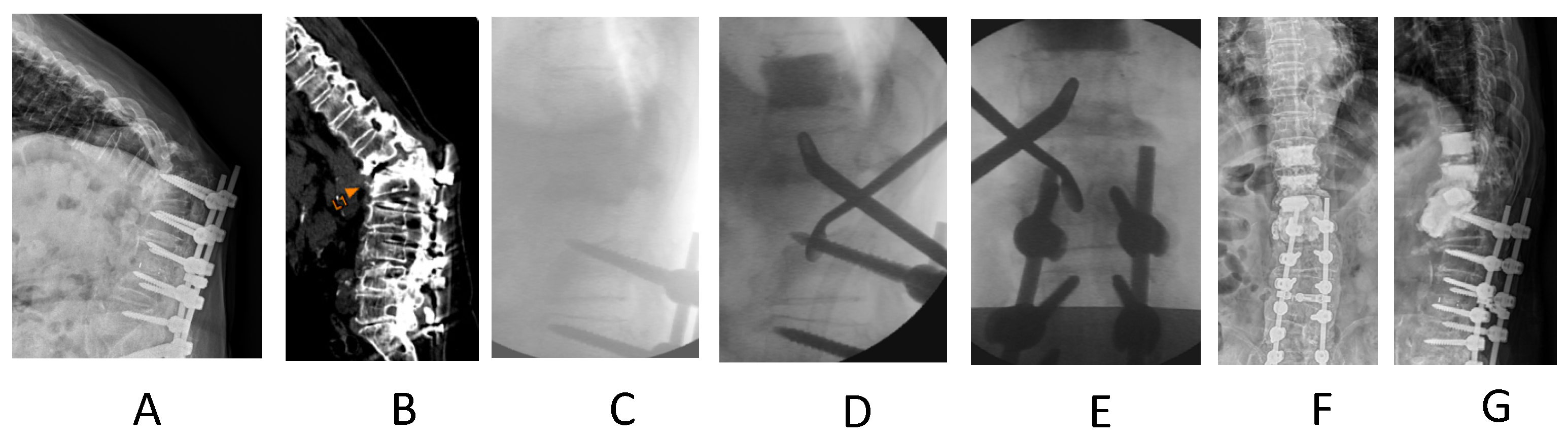
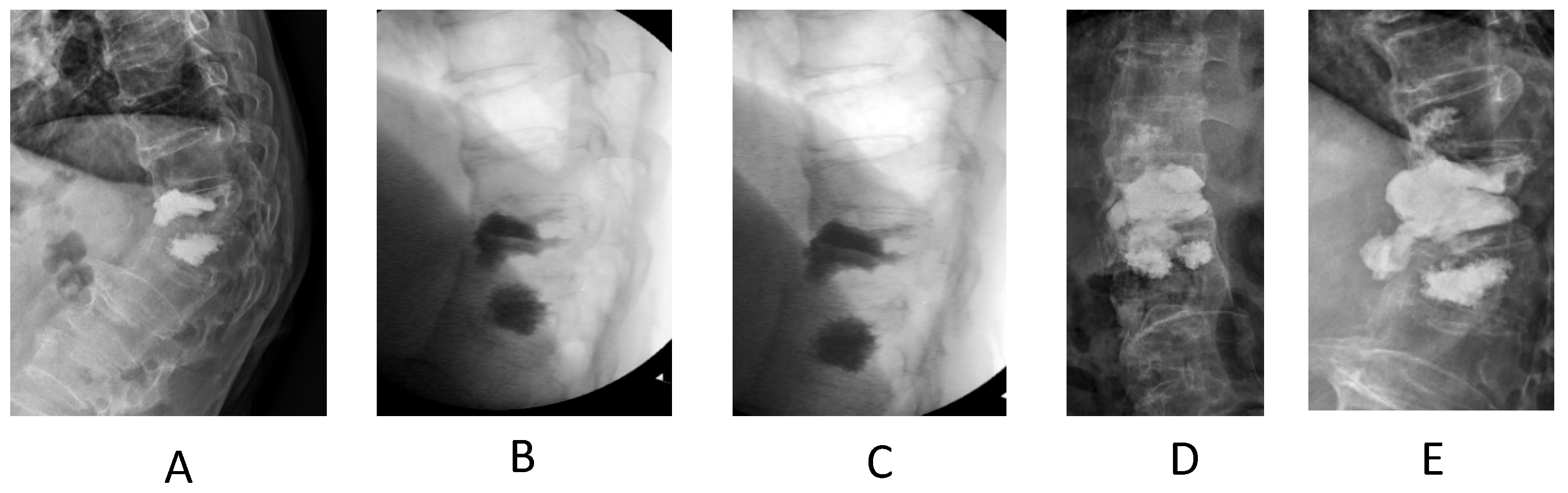
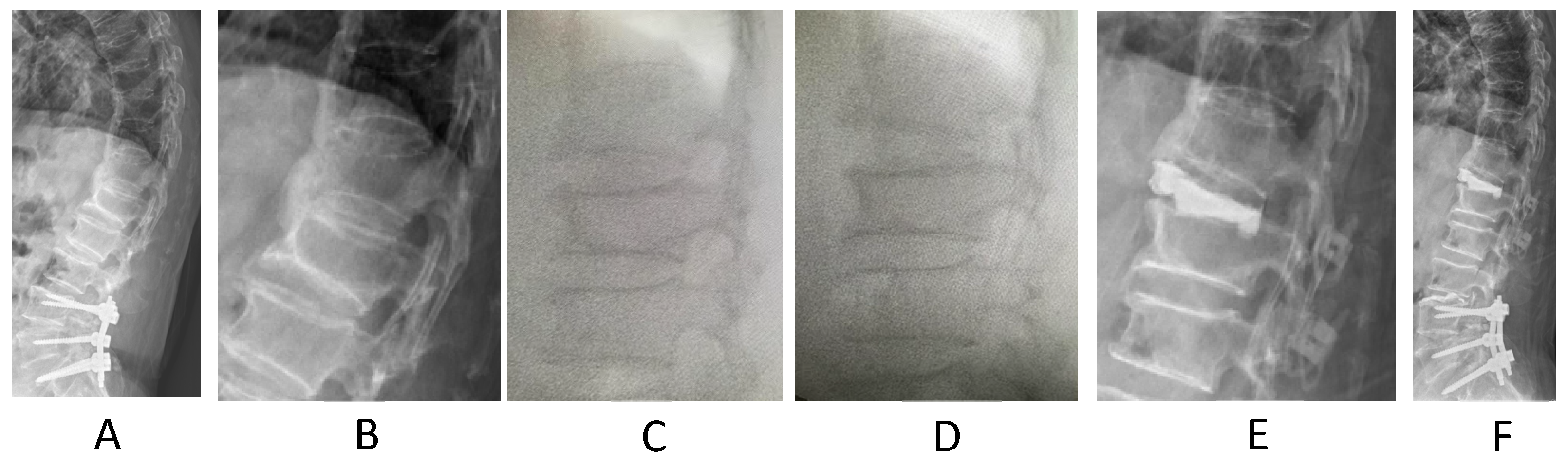
2. Materials and Methods
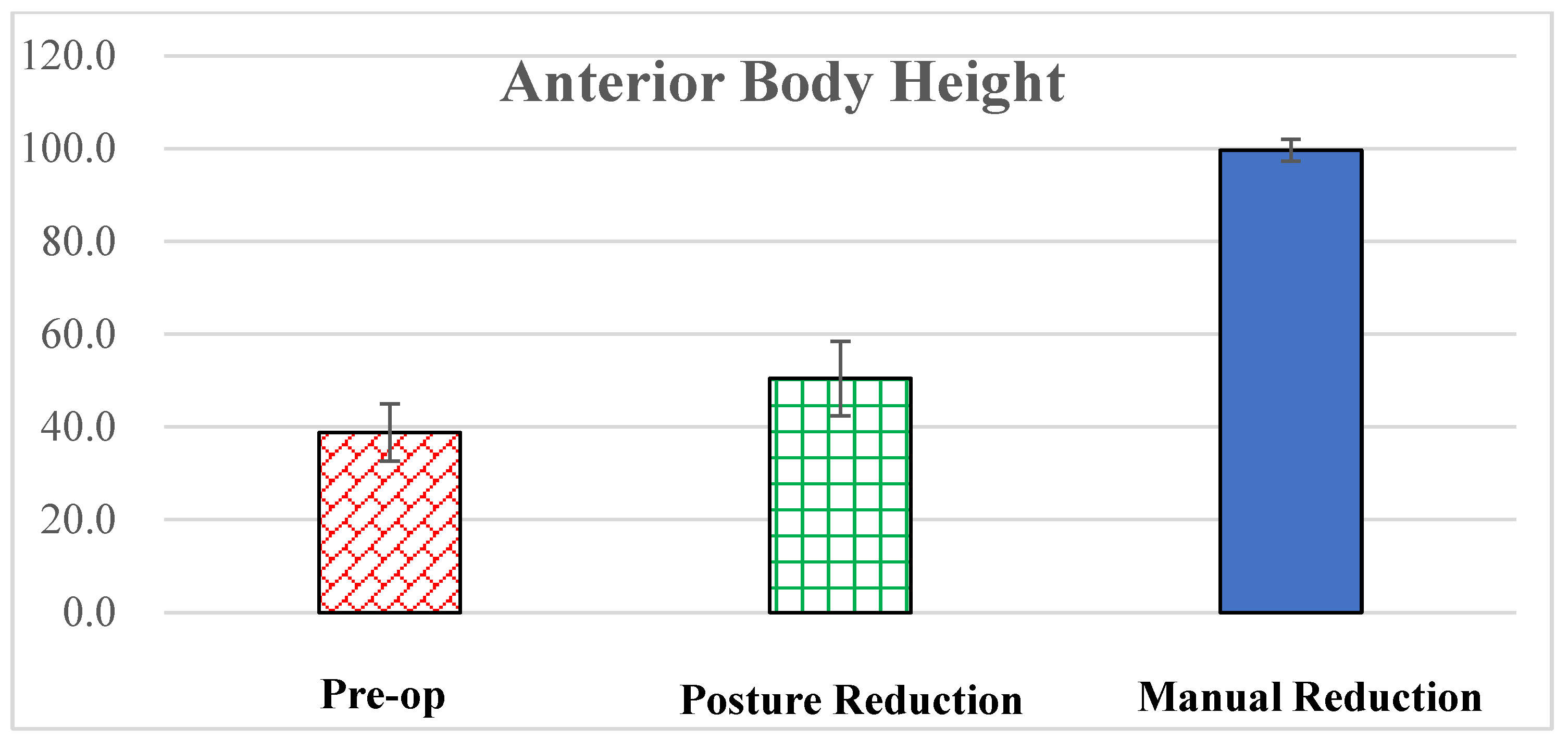
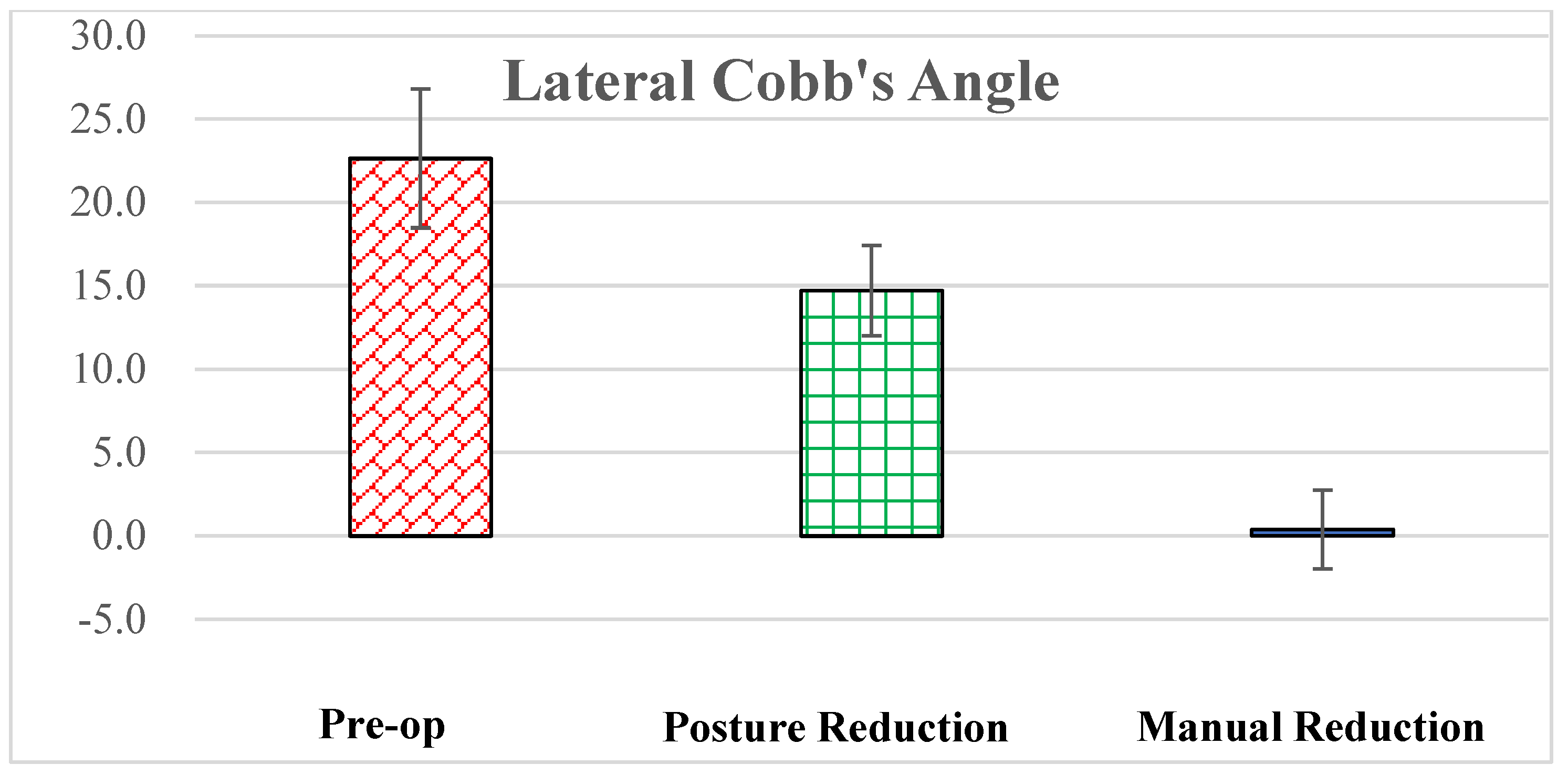
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buchbinder, R.; Johnston, R.V.; Rischin, K.J.; Homik, J.; Jones, C.A.; Golmohammadi, K.; Kallmes, D.F. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst. Rev. 2018, 4, CD006349, Update in Cochrane Database Syst. Rev. 2018, 11, CD006349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zuo, X.H.; Zhu, X.P.; Bao, H.G.; Xu, C.J.; Chen, H.; Gao, X.Z.; Zhang, Q.X. Network meta-analysis of percutaneous vertebroplasty, percutaneous kyphoplasty, nerve block, and conservative treatment for nonsurgery options of acute/subacute and chronic osteoporotic vertebral compression fractures (OVCFs) in short-term and long-term effects. Medicine 2018, 97, e11544. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fredrickson, B.; Edwards, W.; Rauschning, W.; Bayley, J.; Yuan, H. Volvo award in experimental studies vertebral burst fractures: An experimental, morphologic, and radiographic study. Spine 1992, 17, 1012–1021. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, B.E.; Mann, K.A.; Yuan, H.A.; Lubicky, J.P. Reduction of the intracanal fragment in experimental burst fractures. Spine 1988, 13, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Frankel, H.L.; O Hancock, D.; Hyslop, G.; Melzak, J.; Michaelis, L.S.; Ungar, G.H.; Vernon, J.D.S.; Walsh, J.J. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Spinal Cord. 1969, 7, 179–192. [Google Scholar] [CrossRef] [PubMed]
- Tropiano, P.; Huang, R.C.; Louis, C.A.; Poitout, D.G.; Louis, R.P. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine 2003, 28, 2459–2465. [Google Scholar] [CrossRef] [PubMed]
- Li, K.-C.; Hsieh, C.-H.; Lee, C.-Y.; Chen, T.-H. Transpedicle body augmenter: A further step in treating burst fractures. Clin. Orthop. Relat. Res. (1976–2007) 2005, 436, 119–125. [Google Scholar] [CrossRef]
- Li, K.-C.; Li, A.F.-Y.; Hsieh, C.-H.; Chen, H.-H. Transpedicle body augmenter in painfulo steoporotic compression fractures. Eur. Spine J. 2007, 16, 589–598. [Google Scholar] [CrossRef] [PubMed]
- Carlo, P.; Francesco, C. Preoperative manual on-table-traction for the reduction of thoracolumbar burst fractures: A technical note. J. Craniovertebral Junction Spine 2018, 9, 73. [Google Scholar] [CrossRef]
- Li, Y.; Du, Y.; Ji, A.; Wang, Q.; Li, L.; Wu, X.; Wang, P.; Chen, F. The clinical effect of manual reduction combined with internal fixation through Wiltse Paraspinal approach in the treatment of thoracolumbar fracture. Orthop. Surg. 2021, 13, 2206–2215. [Google Scholar] [CrossRef]
- Huang, J.; Zhou, L.; Yan, Z.; Zhou, Z.; Gou, X. Effect of manual reduction and indirect decompression on thoracolumbar burst fracture: A comparison study. J. Orthop. Surg. Res. 2020, 15, 532. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rousing, R.; Andersen, M.O.; Jespersen, S.M.; Thomsen, K.; Lauritsen, J. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: Three-months follow-up in a clinical randomized study. Spine 2009, 34, 1349–1354. [Google Scholar] [CrossRef] [PubMed]
- Li, K.C. IntechOpen: Manual Reduction, Subpedicle Approach, and Body Cage to Treat Burst Fracture. IntechOpen 2023. Available online: https://www.intechopen.com/profiles/518621 (accessed on 1 June 2023).
- Khan, M.R.; Mirdad, T.M. Ipsilateral dislocation of the shoulder and elbow. Saudi Med. J. 2001, 22, 1019–1021. [Google Scholar] [PubMed]
- Bohlman, H.H.; Ducker, T.B. Spine and Spine Cord Injuries. In Rothman-Simeone the Spine, 4th ed.; Herkowitz, H.N., Garfin, S.R., Balderston, R.A., Eismont, F.J., Bell, G.R., Eds.; WB Saunders Company: Philadelphia, PA, USA, 1999; Volume 2, pp. 889–1002. [Google Scholar]
- Harrington, R.; Budorick, T.; Hoyt, J.; Anderson, P.; Tencer, A. Biomechanics of indirect reduction of bone retropulsed into the spinal canal in vertebral fracture. Spine 1993, 18, 692–699. [Google Scholar] [CrossRef]
- Lin, R.M.; Panjabi, M.M.; Oxland, T.R. Functional radiographs of acute thoracolumbar burst fractures: A biomechanical study. Spine 1993, 18, 2431–2437. [Google Scholar] [CrossRef] [PubMed]
- Mumford, J.; Weinstein, J.N.; Spratt, K.F.; Goel, V.K. Thoracolumbar burst fractures: The clinical efficacy and outcome of nonoperative management. Spine 1993, 18, 955–970. [Google Scholar] [CrossRef] [PubMed]
- Deramond, H.; Depriester, C.; Galibert, P.; Le Gars, D. Percutaneous vertebroplasty with polymethylmethacrylate: Technique, indications, and results. Radiol. Clin. N. Am. 1998, 36, 533–546. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, R.W.; Dick, W. The fixateur interne in the reduction and stabilization of thoracolumbar spine fractures in patients with neurologic deficit. Spine 1991, 16 (Suppl. S3), S140–S145. [Google Scholar] [CrossRef]
- Duan, Y.; Feng, D.; Chen, J.; Wu, Y.; Li, T.; Jiang, L.; Huang, Y. Anterior, Posterior and Anterior-Posterior Approaches for the Treatment of Thoracolumbar Burst Fractures: A Network Meta-Analysis of Randomized Controlled Trials. J. Investig. Surg. 2024, 37, 2301794. [Google Scholar] [CrossRef] [PubMed]
- Li, K.-C.; Li, A.F.; Hsieh, C.-H.; Liao, T.-H.; Chen, C.-H. Another option to treat Kümmell’s disease with cord compression. Eur. Spine J. 2007, 16, 1479–1487. [Google Scholar] [CrossRef]
- Van Eenenaam, D.P.; Georges, Y. Delayed post-traumatic vertebral collapse (Kummell’s disease): Case report with serial radiographs, computed tomographic scans, and bone scans. Spine 1993, 18, 1236–1241. [Google Scholar] [CrossRef] [PubMed]
- Golimbu, C.; Firooznia, H.; Rafii, M. The intravertebral vacuum sign. Spine 1986, 11, 1040–1043. [Google Scholar] [CrossRef] [PubMed]
- Osterhouse, M.D.; Kettner, N.W. Delayed posttraumatic vertebral collapse with intravertebral vacuum cleft. J. Manip. Physiol. Ther. 2002, 25, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Garfin, S.R.; Yuan, H.A.; Reiley, M.A. New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001, 26, 1511–1515. [Google Scholar] [CrossRef] [PubMed]
- Hiwatashi, A.; Moritani, T.; Numaguchi, Y.; Westesson, P.-L. Increase in vertebral body height after vertebroplasty. Am. J. Neuroradiol. 2003, 24, 185–189. [Google Scholar] [PubMed]
- McKiernan, F.; Jensen, R.; Faciszewski, T. The dynamic mobility of vertebral compression fractures. J. Bone Miner. Res. 2003, 18, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Fukuta, S.; Miyamoto, K.; Masuda, T.; Hosoe, H.; Kodama, H.; Nishimoto, H.; Sakaeda, H.; Shimizu, K. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine 2003, 28, E302–E308. [Google Scholar] [CrossRef]
- Perrin, R.G.; McBroom, R.J. Spinal fixation after anterior decompression for symptomatic spinal metastasis. Neurosurgery 1988, 22, 324–327. [Google Scholar] [CrossRef]
- Walker, M.P.; Yaszemski, M.J.; Kim, C.W.; Talac, R.; Currier, B.L. Metastatic disease of the spine: Evaluation and treatment. Clin. Orthop. Relat. Res. (1976–2007) 2003, 415, S165–S175. [Google Scholar] [CrossRef]
- Sieradzki, J.P.; Sarwark, J.F. Thoracolumbar fracture-dislocation in child abuse: Case report, closed reduction technique and review of the literature. Pediatr. Neurosurg. 2008, 44, 253–257. [Google Scholar] [CrossRef]
- Li, K.-C.; Hsieh, C.-H.; Liao, T.-H. Clinical outcome-supported advance of cement lumber interbody fusion for degenerative lumbar scoliosis. J. Surg. 2023, 8, 1697. [Google Scholar] [CrossRef]



| Items | Data |
|---|---|
| Gender | 73 females |
| 28 males | |
| (Total: 101) | |
| Age | 77.4 ± 8.5 |
| (61 to 94) | |
| DEXA | 3.2 ± 4.5 |
| (2.9 to 4.2) | |
| Injury mechanism | Fall: 54 cases |
| RTA: 13 cases | |
| Minor trauma 1: 34 cases | |
| Fracture level | T10: 5 |
| T11: 19 | |
| T12: 29 | |
| L1: 31 | |
| L2: 17 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, K.-C.; Hsieh, C.-H.; Liao, T.-H.; Chen, C.-H. Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures. BioMed 2024, 4, 136-145. https://doi.org/10.3390/biomed4020011
Li K-C, Hsieh C-H, Liao T-H, Chen C-H. Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures. BioMed. 2024; 4(2):136-145. https://doi.org/10.3390/biomed4020011
Chicago/Turabian StyleLi, Kung-Chia, Ching-Hsiang Hsieh, Ting-Hua Liao, and Chih-Hung Chen. 2024. "Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures" BioMed 4, no. 2: 136-145. https://doi.org/10.3390/biomed4020011
APA StyleLi, K.-C., Hsieh, C.-H., Liao, T.-H., & Chen, C.-H. (2024). Manual Reduction for Subacute Osteoporotic Burst and Severe Compression Thoracolumbar Fractures. BioMed, 4(2), 136-145. https://doi.org/10.3390/biomed4020011







