Laparoscopic Placement of the Tenckhoff Catheter with a New Regional Anesthesia: A Two-Year Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
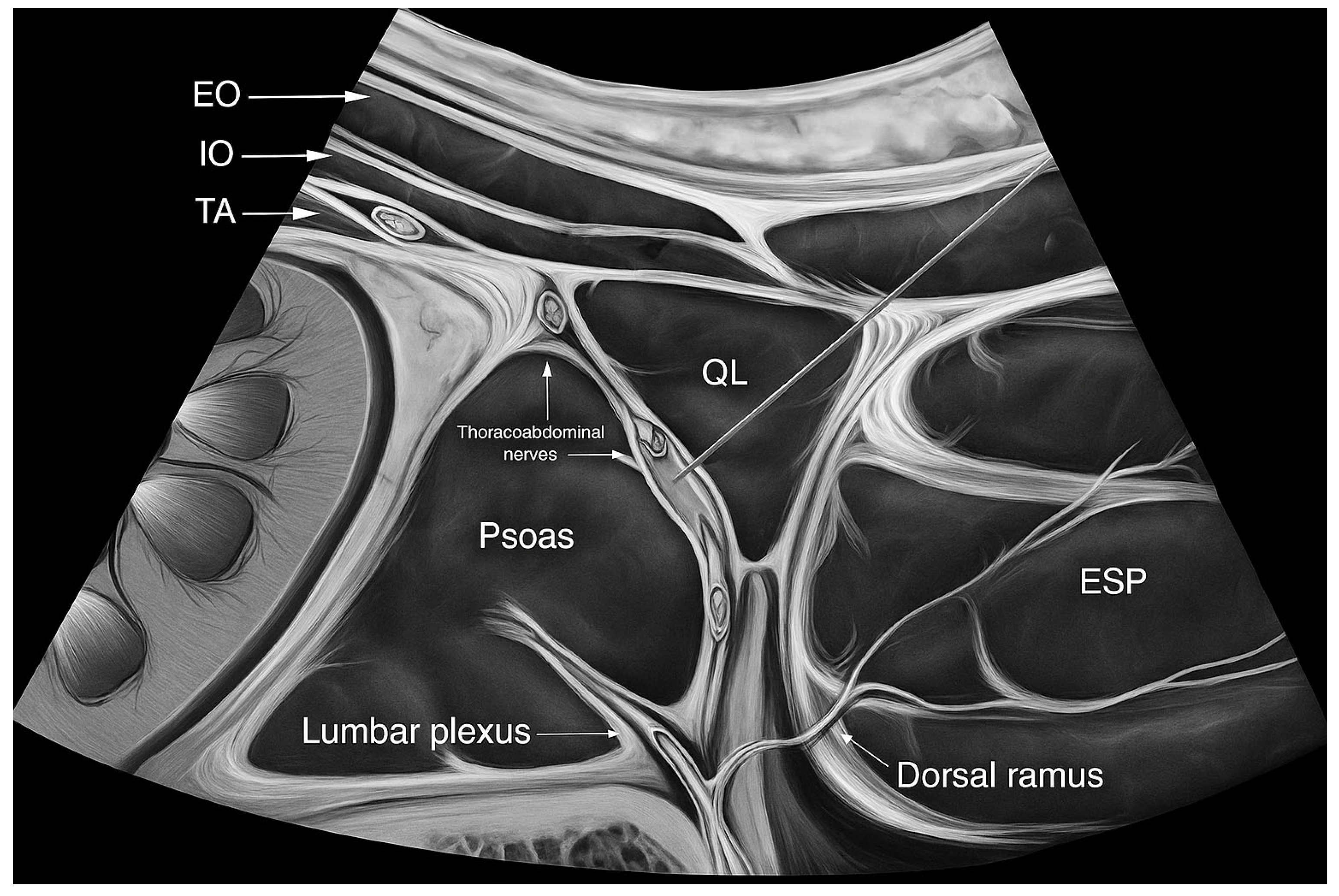
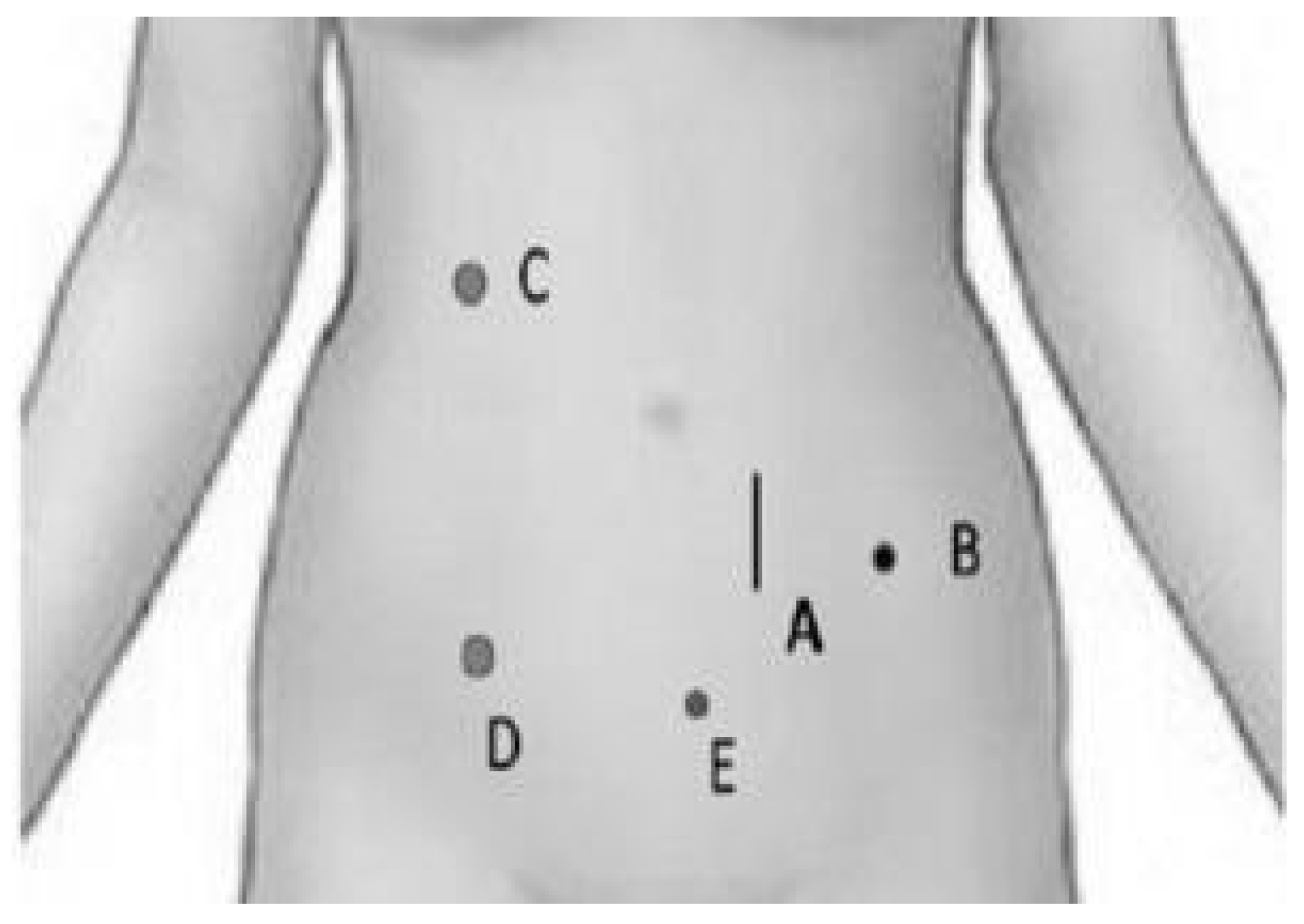
2.2. Anesthetic Procedure
2.3. Surgical Procedure
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. Post-Operative Outcomes
3.2. Long-Term Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chaudhary, K.; Sangha, H.; Khanna, R. Peritoneal dialysis first: Rationale. Clin. J. Am. Soc. Nephrol. 2011, 6, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Hryszko, T.; Suchowierska, E.; Rydzewska-Rosolowska, A.; Brzosko, S.; Mysliwiec, M. Factors associated with early catheter-related complications in peritoneal dialysis. Adv. Med. Sci. 2012, 57, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Davidson, I.; Minhajuddin, A.; Gieser, S.; Nurenberg, M.; Saxena, R. Risk factors associated with peritoneal dialysis catheter survival: A 9-year single-center study in 315 patients. J. Vasc. Access 2010, 11, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Crabtree, J.H.; Chow, K.M. Peritoneal dialysis catheter insertion. Semin. Nephrol. 2017, 37, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.L.; Zhang, Y.; Wang, B.; Ma, T.A.; Jiang, H.; Hu, S.L.; Zhang, P.; Tuo, Y.H. Randomized controlled trials for comparison of laparoscopic versus conventional open catheter placement in peritoneal dialysis patients: A meta-analysis. BMC Nephrol. 2020, 21, 60. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Qiao, Q.; Zhou, L.; Hu, K.; Xu, D.; Li, L.; Lu, G. Laparoscopic versus traditional peritoneal dialysis catheter insertion: A meta-analysis. Ren. Fail. 2016, 38, 838–848. [Google Scholar] [CrossRef] [PubMed]
- Zang, Z.; Qiu, X.; Yang, L.; Wang, X.; Li, Z. Different techniques for peritoneal dialysis catheter implantation: A systematic review and network meta-analysis. Perit. Dial. Int. 2021, 41, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Crabtree, J.H.; Fishman, A. A laparoscopic approach under local anesthesia for peritoneal dialysis access. Perit. Dial. Int. 2000, 20, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Ueshima, H.; Otake, H.; Lin, J.A. Ultrasound-Guided Quadratus Lumborum Block: An Updated Review of Anatomy and Techniques. Biomed. Res. Int. 2017, 2017, 2752876. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dam, M.; Moriggl, B.; Hansen, C.K.; Hoermann, R.; Bendtsen, T.F.; Børglum, J. The Pathway of Injectate Spread With the Transmuscular Quadratus Lumborum Block: A Cadaver Study. Anesth. Analg. 2017, 125, 303–312. [Google Scholar] [CrossRef] [PubMed]
- El-Boghdadly, K.; Wolmarans, M.; Stengel, A.D.; Albrecht, E.; Chin, K.J.; Elsharkawy, H.; Kopp, S.; Mariano, E.R.; Xu, J.L.; Adhikary, S.; et al. Standardizing nomenclature in regional anesthesia: An ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg. Anesth. Pain Med. 2021, 46, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Crabtree, J.H.; Fishman, A.; Huen, I.T. Videolaparoscopic peritoneal dialysis catheter implant and rescue procedures under local anesthesia with nitrous oxide pneumoperitoneum. Adv. Perit. Dial. 1998, 14, 83–86. [Google Scholar] [PubMed]
- Keshvari, A.; Najafi, I.; Jafari-Javid, M.; Yunesian, M.; Chaman, R.; Taromlou, M.N. Laparoscopic peritoneal dialysis catheter implantation using a Tenckhoff trocar under local anesthesia with nitrous oxide gas insufflation. Am. J. Surg. 2009, 197, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Aldohayan, A.; AlSehli, R.; Alosaimi, M.M.; AlMousa, A.M.; AlOtaibi, A.F.; Al-Dhayan, A.Z.; Alanazi, A.Z.; Aldohayan, N.A.; Eldawlatly, A. Preperitoneal Local Anesthesia Technique in Laparoscopic Peritoneal Dialysis Catheter Placement. JSLS 2022, 26, e2021.00093. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Desai, N.; El-Boghdadly, K.; Albrecht, E. Peripheral nerve blockade and novel analgesic modalities for ambulatory anesthesia. Curr. Opin. Anaesthesiol. 2020, 33, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Ricci, M.; Bonfigli, A.R.; Protic, O.; Olivieri, F.; Starnari, R.; Iuorio, S.; Lenci, F. Thoracic spinal anesthesia for laparoscopic peritoneal dialysis catheter placement in older high-risk end-stage kidney disease patients. Perit. Dial. Int. 2025, 23, 8968608251336674, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Ash, S.R. Bedside peritoneoscopic peritoneal catheter placement of Tenckhoff and newer peritoneal catheters. Adv. Perit. Dial. 1998, 14, 75–79. [Google Scholar] [PubMed]
| Patient | Age | Gender | GFR | BMI | Kidney Disease | DM | CVD | Prior Abdominal Surgery | Concomitant Surgery |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 44 | M | 8 | 29.7 | Unknown | NO | NO | Inguinal hernia + sleeve GS | NO |
| 2 | 58 | M | 9 | 27.4 | GN | NO | NO | NO | NO |
| 3 | 33 | M | 7 | 24.2 | DKD | YES | NO | NO | NO |
| 4 | 22 | M | 7 | 35.0 | Unknown | NO | NO | NO | NO |
| 5 | 62 | M | 8 | 25.2 | HTN | NO | NO | NO | NO |
| 6 | 65 | M | 10 | 25.3 | DKD | YES | NO | NO | NO |
| 7 | 71 | F | 9 | 28.2 | DKD | YES | NO | NO | NO |
| 8 | 71 | M | 8 | 24.5 | Unknown | NO | YES | Inguinoscrotal hernia | Inguinal hernia |
| 9 | 71 | M | 10 | 23.2 | TIN | YES | YES | Cholecystectomy | NO |
| 10 | 71 | M | 10 | 28.3 | GN | NO | NO | Inguinoscrotal hernia | Inguinal hernia |
| 11 | 56 | F | 9 | 29.7 | Unknown | NO | NO | NO | NO |
| 12 | 44 | F | 10 | 35.5 | TIN | NO | NO | NO | NO |
| 13 | 53 | M | 9 | 27.4 | Unknown | NO | NO | NO | NO |
| 14 | 69 | F | 10 | 31.4 | Unknown | NO | YES | NO | NO |
| 15 | 62 | M | 7 | 28.5 | Unknown | NO | NO | NO | NO |
| 16 | 46 | F | 6 | 25.4 | Unknown | NO | NO | NO | NO |
| 17 | 74 | M | 7 | 26.4 | DKD | YES | NO | NO | NO |
| 18 | 52 | M | 8 | 34.8 | DKD | YES | YES | NO | NO |
| 19 | 69 | M | 8 | 26.3 | Unknown | NO | YES | NO | NO |
| 20 | 69 | F | 3 | 24.9 | ADPKD | NO | YES | NO | NO |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Somma, G.; Ruotolo, C.; Auricchio, M.R.; Cappiello, A.; De Luca, M.; Selvaggi, L.; Romano, F.M.; Capozzi, F.; Marzano, F.; Borrelli, S.; et al. Laparoscopic Placement of the Tenckhoff Catheter with a New Regional Anesthesia: A Two-Year Experience. Kidney Dial. 2025, 5, 55. https://doi.org/10.3390/kidneydial5040055
Somma G, Ruotolo C, Auricchio MR, Cappiello A, De Luca M, Selvaggi L, Romano FM, Capozzi F, Marzano F, Borrelli S, et al. Laparoscopic Placement of the Tenckhoff Catheter with a New Regional Anesthesia: A Two-Year Experience. Kidney and Dialysis. 2025; 5(4):55. https://doi.org/10.3390/kidneydial5040055
Chicago/Turabian StyleSomma, Giovanni, Chiara Ruotolo, Maria Rita Auricchio, Antonio Cappiello, Michele De Luca, Lucio Selvaggi, Francesco Maria Romano, Federica Capozzi, Federica Marzano, Silvio Borrelli, and et al. 2025. "Laparoscopic Placement of the Tenckhoff Catheter with a New Regional Anesthesia: A Two-Year Experience" Kidney and Dialysis 5, no. 4: 55. https://doi.org/10.3390/kidneydial5040055
APA StyleSomma, G., Ruotolo, C., Auricchio, M. R., Cappiello, A., De Luca, M., Selvaggi, L., Romano, F. M., Capozzi, F., Marzano, F., Borrelli, S., De Nicola, L., & Garofalo, C. (2025). Laparoscopic Placement of the Tenckhoff Catheter with a New Regional Anesthesia: A Two-Year Experience. Kidney and Dialysis, 5(4), 55. https://doi.org/10.3390/kidneydial5040055









