The Role of L-Carnitine in Kidney Disease and Related Metabolic Dysfunctions
Abstract
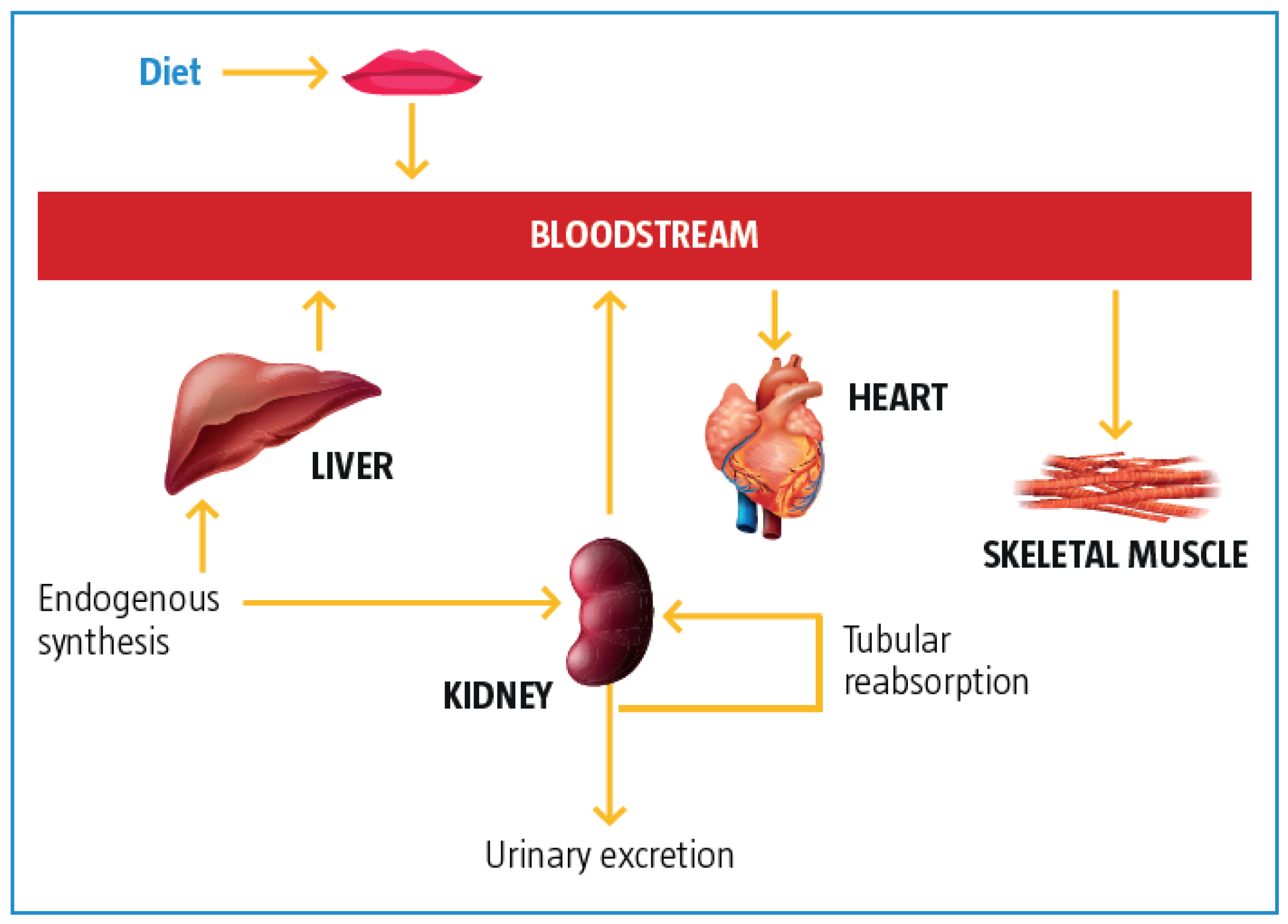
1. Pathophysiology of Kidney Disease and Relationship between Carnitine Metabolism and Kidney Function
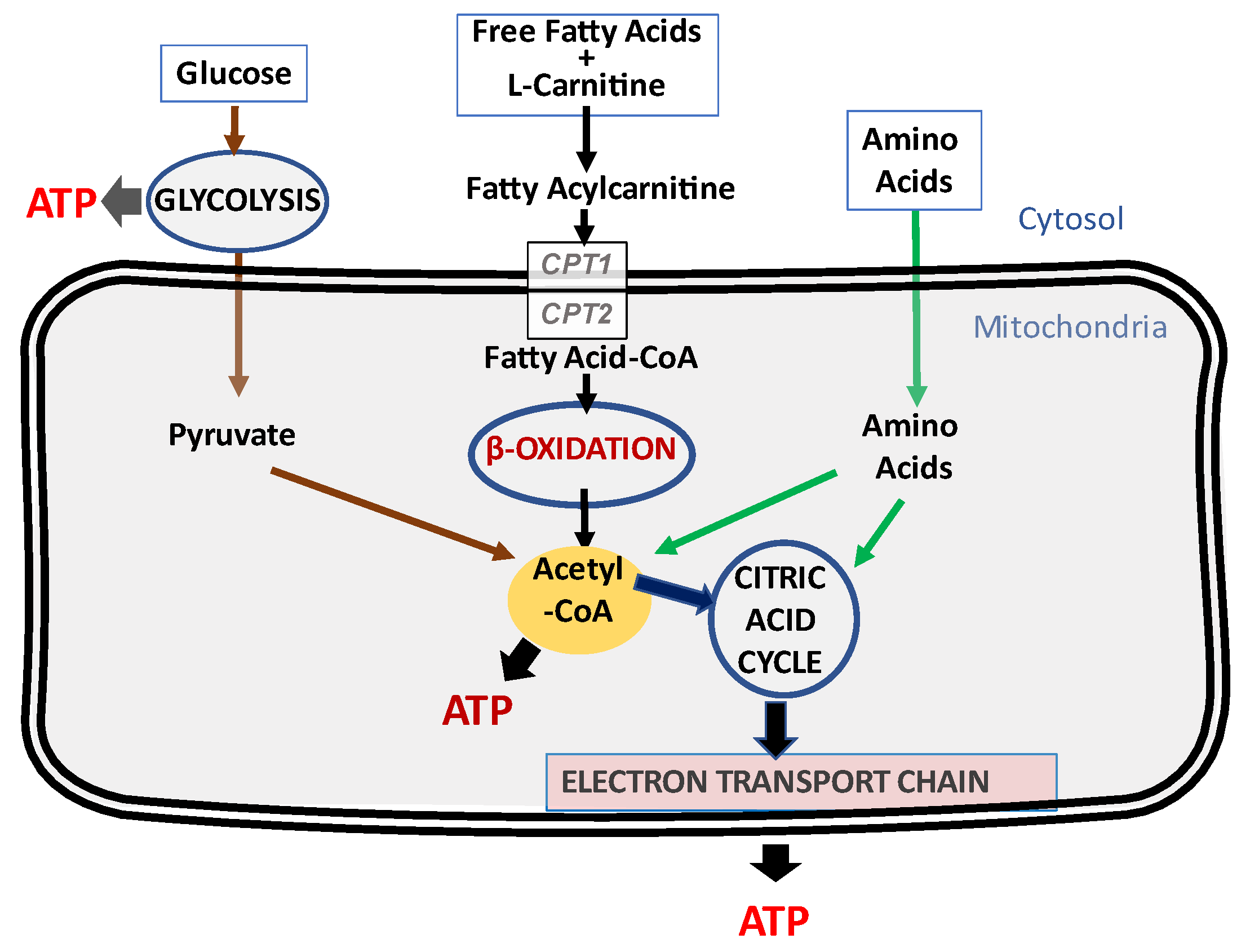
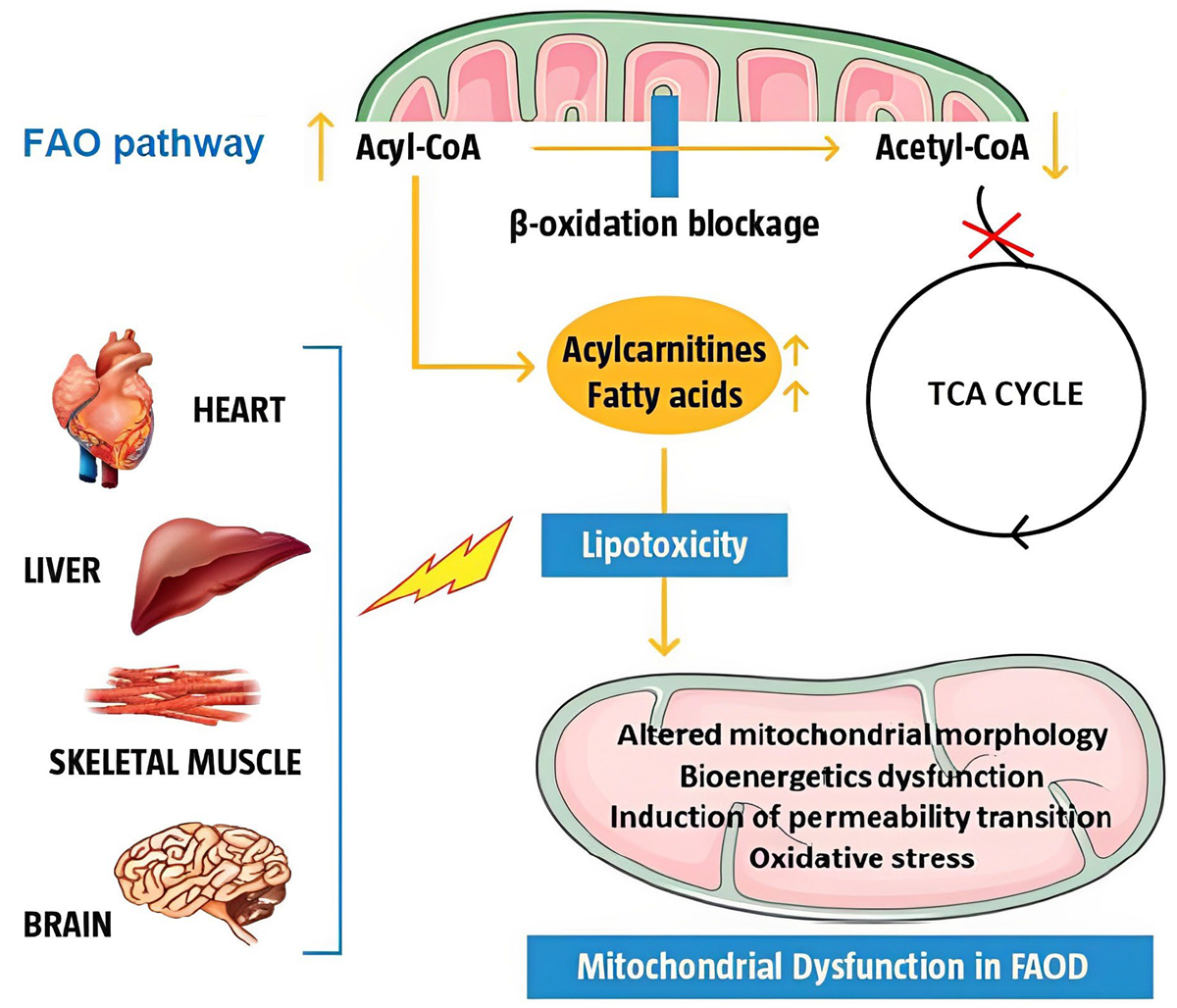
1.1. Metabolic Alterations in Kidney Disease and Potential Protective Role of L-Carnitine
1.2. Role of the Mitochondria in Kidney Disease
2. Diet in Chronic Kidney Disease
- Hyperkalemia with a risk of arrhythmia;
- An increase in plasma urea leading to neurotoxicity and cardiac toxicity;
- An increase in phosphate, which can damage the arterial structure and thereby lead to an increase of the left ventricular volume due to the increased afterload;
- Hypervolemia with a risk of arterial hypertension and pulmonary edema.
3. L-Carnitine in Acute Kidney Injury
4. Acute Kidney Injury from Infection and Drugs
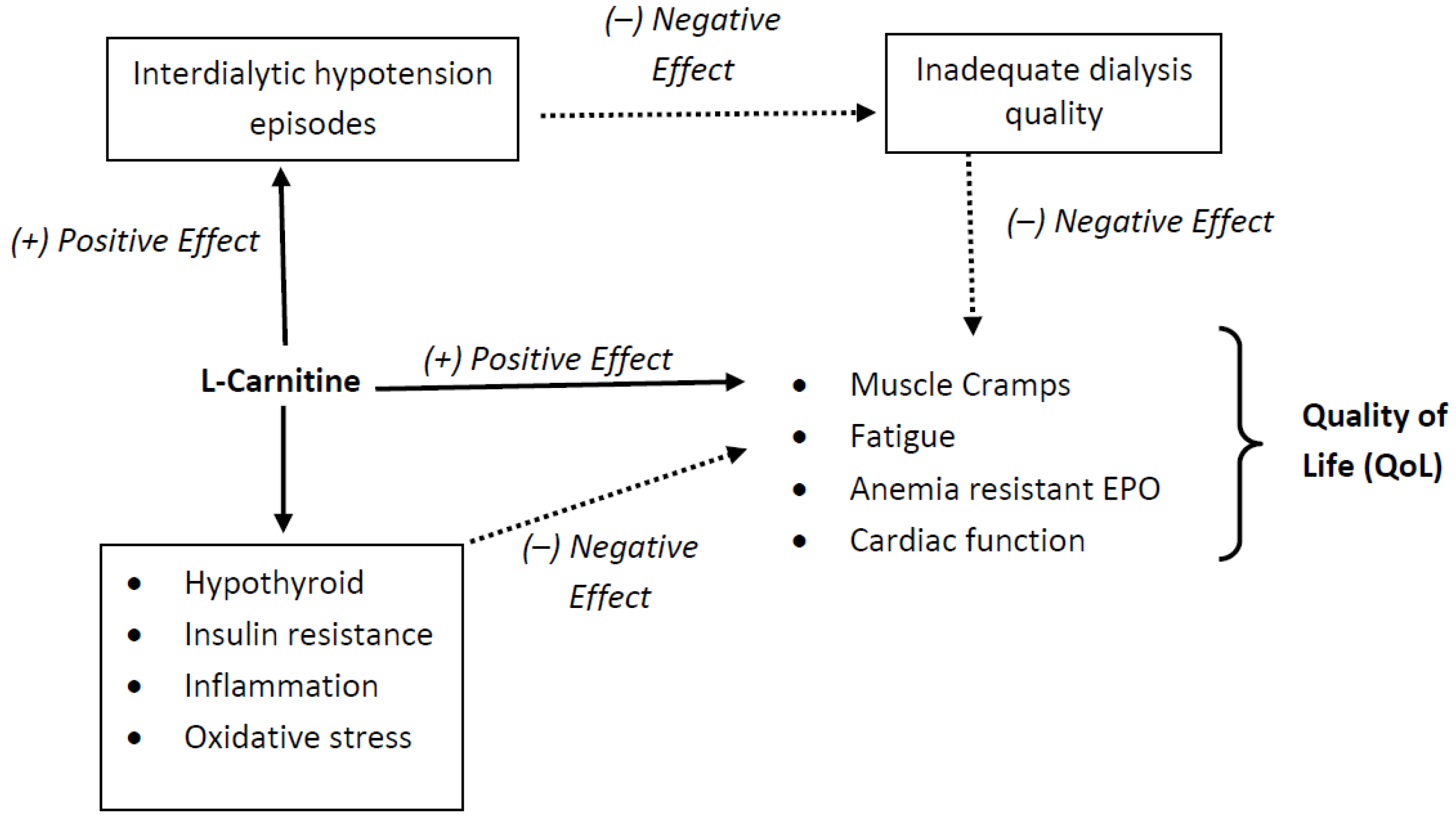
5. Dialysis Related Complications
5.1. L-Carnitine in Anemia and Response to Erythropoietin
- Increased plasma L-carnitine concentrations (p < 0.00001);
- Improved the response to erythropoiesis-stimulating agents (ESA) (p < 0.00001);
- Decreased the required ESA doses in patients receiving hemodialysis (p < 0.00001);
- Maintained hemoglobin and hematocrit levels.
- Adults: 20 mg/kg or 1–2 g L-carnitine IV after each dialysis session
- Children: 20 mg/kg after each dialysis session or
- o
- Children >40 kg: 1 g L-carnitine IV
- o
- Children 20–40 kg: 500 mg L-carnitine IV
- o
- Children 10–20 kg: 200 mg L-carnitine IV
5.2. L-Carnitine and Intradialytic Hypotension
- Adults: 20 mg/kg or 1–2 g L-carnitine IV after each dialysis session
- Children: 20 mg/kg or
- o
- Children >40 kg: 1 g L-carnitine IV
- o
- Children 20–40 kg: 500 mg L-carnitine IV
- o
- Children 10–20 kg: 200 mg L-carnitine IV
5.3. Role of Carnitine in Reducing Cardiovascular Complications
6. Future Perspectives in the Management of Kidney Disease: The Role of Genomics, Proteomics, Metabolomics, and the Microbiome
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Longo, N.; Frigeni, M.; Pasquali, M. Carnitine Transport and Fatty Acid Oxidation. Biochim. Biophys. Acta 2016, 1863, 2422–2435. [Google Scholar] [CrossRef]
- Virmani, M.A.; Cirulli, M. The Role of l-Carnitine in Mitochondria, Prevention of Metabolic Inflexibility and Disease Initiation. Int. J. Mol. Sci. 2022, 23, 2717. [Google Scholar] [CrossRef] [PubMed]
- Evans, A. Dialysis-Related Carnitine Disorder and Levocarnitine Pharmacology. Am. J. Kidney Dis. 2003, 41, S13–S26. [Google Scholar] [CrossRef] [PubMed]
- Rebouche, C.J. Kinetics, Pharmacokinetics, and Regulation of l-Carnitine and Acetyl-l-Carnitine Metabolism. Ann. N. Y. Acad. Sci. 2004, 1033, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Reuter, S.E.; Faull, R.J.; Evans, A.M. l-carnitine Supplementation in the Dialysis Population: Are Australian Patients Missing Out? Nephrology 2008, 13, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Wasserstein, A.G. l-carnitine Supplementation in Dialysis: Treatment in Quest of Disease. Semin. Dial. 2013, 26, 11–15. [Google Scholar] [CrossRef]
- Wanner, C.; Hörl, W.H. Carnitine Abnormalities in Patients with Renal Insufficiency. Pathophysiological and Therapeutical Aspects. Nephron 1988, 50, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Virmani, A.; Binienda, Z. Role of Carnitine Esters in Brain Neuropathology. Mol. Asp. Med. 2004, 25, 533–549. [Google Scholar] [CrossRef]
- Fouque, D.; Holt, S.; Guebre-Egziabher, F.; Nakamura, K.; Vianey-Saban, C.; Hadj-Aïssa, A.; Hoppel, C.L.; Kopple, J.D. Relationship Between Serum Carnitine, Acylcarnitines, and Renal Function in Patients with Chronic Renal Disease. J. Ren. Nutr. 2006, 16, 125–131. [Google Scholar] [CrossRef]
- Hatanaka, Y.; Higuchi, T.; Akiya, Y.; Horikami, T.; Tei, R.; Furukawa, T.; Takashima, H.; Tomita, H.; Abe, M. Prevalence of Carnitine Deficiency and Decreased Carnitine Levels in Patients on Hemodialysis. Blood Purif. 2019, 47, 38–44. [Google Scholar] [CrossRef]
- Almannai, M.; Alfadhel, M.; El-Hattab, A.W. Carnitine Inborn Errors of Metabolism. Molecules 2019, 24, 3251. [Google Scholar] [CrossRef]
- Che, R.; Yuan, Y.; Huang, S.; Zhang, A. Mitochondrial Dysfunction in the Pathophysiology of Renal Diseases. Am. J. Physiol. Renal. Physiol. 2014, 306, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Virmani, A.; Pinto, L.; Binienda, Z.; Ali, S. Food, Nutrigenomics, and Neurodegeneration—Neuroprotection by What You Eat! Mol. Neurobiol. 2013, 48, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Dan Dunn, J.; Alvarez, L.A.; Zhang, X.; Soldati, T. Reactive Oxygen Species and Mitochondria: A Nexus of Cellular Homeostasis. Redox Biol. 2015, 6, 472–485. [Google Scholar] [CrossRef] [PubMed]
- Duann, P.; Lin, P.H. Mitochondria Damage and Kidney Disease. Adv. Exp. Med. Biol. 2017, 982, 529–551. [Google Scholar] [CrossRef]
- Bhatia, D.; Capili, A.; Choi, M.E. Mitochondrial Dysfunction in Kidney Injury, Inflammation, and Disease: Potential Therapeutic Approaches. Kidney Res. Clin. Pract. 2020, 39, 244–258. [Google Scholar] [CrossRef]
- Berezhnov, A.V.; Fedotova, E.I.; Nenov, M.N.; Kasymov, V.A.; Pimenov, O.Y.; Dynnik, V.V. Dissecting Cellular Mechanisms of Long-Chain Acylcarnitines—Driven Cardiotoxicity: Disturbance of Calcium Homeostasis, Activation of Ca2+-dependent Phospholipases, and Mitochondrial Energetics Collapse. Int. J. Mol. Sci. 2020, 21, 7461. [Google Scholar] [CrossRef] [PubMed]
- Weidemann, M.J.; Krebs, H.A. The Fuel of Respiration of Rat Kidney Cortex. Biochem. J. 1969, 112, 149–166. [Google Scholar] [CrossRef]
- Weinberg, G.L.; Baughman, V. Carnitine Deficiency, Mitochondrial Metabolism, and Abnormal Response to Anesthetics. Anesthesiology 2006, 104, 1343. [Google Scholar] [CrossRef]
- Ertunc, M.E.; Hotamisligil, G.S. Lipid Signalling and Lipotoxicity in Metaflammation: Indications for Metabolic Disease Pathogenesis and Treatment. J. Lipid Res. 2016, 57, 2099–2114. [Google Scholar] [CrossRef]
- Nishi, H.; Higashihara, T.; Inagi, R. Lipotoxicity in Kidney, Heart, and Skeletal Muscle Dysfunction. Nutrients 2019, 11, 1664. [Google Scholar] [CrossRef]
- Schrauwen, P.; Hesselink, M.K. Oxidative Capacity, Lipotoxicity, and Mitochondrial Damage in Type 2 Diabetes. Diabetes 2004, 53, 1412–1417. [Google Scholar] [CrossRef]
- Schrauwen, P.; Schrauwen-Hinderling, V.; Hoeks, J.; Hesselink, M.K. Mitochondrial Dysfunction and Lipotoxicity. Biochim. Biophys. Acta 2010, 1801, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Sergi, D.; Naumovski, N.; Heilbronn, L.K.; Abeywardena, M.; O’Callaghan, N.; Lionetti, L.; Luscombe-Marsh, N. Mitochondrial (Dys)Function and Insulin Resistance: From Pathophysiological Molecular Mechanisms to the Impact of Diet. Front. Physiol. 2019, 10, 532. [Google Scholar] [CrossRef]
- Wajner, M.; Amaral, A.U. Mitochondrial Dysfunction in Fatty Acid Oxidation Disorders: Insights from Human and Animal Studies. Biosci. Rep. 2015, 36, e00281. [Google Scholar] [CrossRef]
- Katsoulieris, E.; Mabley, J.G.; Samai, M.; Sharpe, M.A.; Green, I.C.; Chatterjee, P.K. Lipotoxicity in Renal Proximal Tubular Cells: Relationship Between Endoplasmic Reticulum Stress and Oxidative Stress Pathways. Free. Radic. Biol. Med. 2010, 48, 1654–1662. [Google Scholar] [CrossRef] [PubMed]
- Simon, N.; Hertig, A. Alteration of Fatty Acid Oxidation in Tubular Epithelial Cells: From Acute Kidney Injury to Renal Fibrogenesis. Front. Med. 2015, 2, 52. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Takabatake, Y.; Takahashi, A.; Kimura, T.; Namba, T.; Matsuda, J.; Minami, S.; Kaimori, J.Y.; Matsui, I.; Matsusaka, T.; et al. High-Fat Diet-Induced Lysosomal Dysfunction and Impaired Autophagic Flux Contribute to Lipotoxicity in the Kidney. J. Am. Soc. Nephrol. 2017, 28, 1534–1551. [Google Scholar] [CrossRef] [PubMed]
- Takemura, K.; Nishi, H.; Inagi, R. Mitochondrial Dysfunction in Kidney Disease and Uremic Sarcopenia. Front. Physiol. 2020, 11, 565023. [Google Scholar] [CrossRef]
- Melov, S.; Coskun, P.; Patel, M.; Tuinstra, R.; Cottrell, B.; Jun, A.S.; Zastawny, T.H.; Dizdaroglu, M.; Goodman, S.I.; Huang, T.-T.; et al. Mitochondrial Disease in Superoxide Dismutase 2 Mutant Mice. Proc. Natl. Acad. Sci. USA 1999, 96, 846–851. [Google Scholar] [CrossRef]
- Park, Y.; Kim, H.; Park, L.; Min, D.; Park, J.; Choi, S.; Park, M.H. Effective Delivery of Endogenous Antioxidants Ameliorates Diabetic Nephropathy. PLoS ONE 2015, 10, e0130815. [Google Scholar] [CrossRef]
- Alicic, R.Z.; Rooney, M.T.; Tuttle, K.R. Diabetic Kidney Disease: Challenges, Progress, and Possibilities. Clin. J. Am. Soc. Nephrol. 2017, 12, 2032–2045. [Google Scholar] [CrossRef]
- Forbes, J.M.; Thorburn, D.R. Mitochondrial Dysfunction in Diabetic Kidney Disease. Nat. Rev. Nephrol. 2018, 14, 291–312. [Google Scholar] [CrossRef]
- Konari, N.; Nagaishi, K.; Kikuchi, S.; Fujimiya, M. Mitochondria Transfer from Mesenchymal Stem Cells Structurally and Functionally Repairs Renal Proximal Tubular Epithelial Cells in Diabetic Nephropathy In Vivo. Sci. Rep. 2019, 9, 5184. [Google Scholar] [CrossRef]
- Ito, S.; Nakashima, M.; Ishikiriyama, T.; Nakashima, H.; Yamagata, A.; Imakiire, T.; Kinoshita, M.; Seki, S.; Kumagai, H.; Oshima, N. Effects of l-Carnitine Treatment on Kidney Mitochondria and Macrophages in Mice with Diabetic Nephropathy. Kidney Blood Press. Res. 2022, 47, 277–290. [Google Scholar] [CrossRef] [PubMed]
- Rees, L.; Shaw, V. Nutrition in Children with CRF and on Dialysis. Pediatr. Nephrol. 2007, 22, 1689–1702. [Google Scholar] [CrossRef]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Martin, W.F.; Armstrong, L.E.; Rodriguez, N.R. Dietary Protein Intake and Renal Function. Nutr. Metab. 2005, 2, 25. [Google Scholar] [CrossRef]
- Ko, G.J.; Rhee, C.M.; Kalantar-Zadeh, K.; Joshi, S. The Effects of High-Protein Diets on Kidney Health and Longevity. J. Am. Soc. Nephrol. 2020, 31, 1667–1679. [Google Scholar] [CrossRef] [PubMed]
- Molina, P.; Gavela, E.; Vizcaíno, B.; Huarte, E.; Carrero, J.J. Optimizing Diet to Slow CKD Progression. Front. Med. 2021, 8, 654250. [Google Scholar] [CrossRef] [PubMed]
- Sherman, R.A. Modifying the Dialysis Prescription to Reduce Intradialytic Hypotension. Am. J. Kidney Dis. 2001, 38, S18–S25. [Google Scholar] [CrossRef]
- Rostoker, G.; Griuncelli, M.; Loridon, C.; Benmaadi, A.; Illouz, E. Left-Ventricular Diastolic Dysfunction as A Risk Factor for Dialytic Hypotension. Cardiology 2009, 114, 142–149. [Google Scholar] [CrossRef]
- Chewcharat, A.; Chewcharat, P.; Liu, W.; Cellini, J.; Phipps, E.A.; Melendez Young, J.A.; Nigwekar, S.U. The Effect of Levocarnitine Supplementation on Dialysis-Related Hypotension: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis. PLoS ONE 2022, 17, e0271307. [Google Scholar] [CrossRef]
- Bazargani, B.; Mojtahedi, S.Y.; Fahimi, D.; Askarian, F.; Moghtaderi, M.; Abbasi, A.; Samimi, M.; Bakhtiari Koohsorkhi, M. Evaluation of the Relationship Between Serum Carnitine Levels and Intradialytic Complications in Children with Kidney Failure. Pediatr. Nephrol. 2022, 37, 2179–2183. [Google Scholar] [CrossRef] [PubMed]
- Sgambat, K.; Clauss, S.; Moudgil, A. Effect of Levocarnitine Supplementation on Myocardial Strain in Children With Acute Kidney Injury Receiving Continuous Kidney Replacement Therapy: A Pilot Study. Pediatr. Nephrol. 2021, 36, 1607–1616. [Google Scholar] [CrossRef]
- Gheissari, A.; Aslani, N.; Eshraghi, A.; Moslehi, M.; Merikhi, A.; Keikhah, M.; Haghjoo Javanmard, S.; Vaseghi, G. Preventive Effect of l-Carnitine on Scar Formation During Acute Pyelonephritis: A Randomized Placebo-Controlled Trial. Am. J. Ther. 2020, 27, e229–e234. [Google Scholar] [CrossRef] [PubMed]
- Van de Wyngaert, C.; Dewulf, J.P.; Collienne, C.; Laterre, P.F.; Hantson, P. Carnitine Deficiency after Long-Term Continuous Renal Replacement Therapy. Case Rep. Crit. Care 2022, 2022, 4142539. [Google Scholar] [CrossRef]
- Mohammadi, M.; Hajhossein Talasaz, A.; Alidoosti, M.; Pour Hosseini, H.R.; Gholami, K.; Jalali, A.; Aryannejad, H. Nephro-protective Effects of l-Carnitine Against Contrast-Induced Nephropathy in Patients Undergoing Percutaneous Coronary Intervention: A Randomized Open-Labelled Clinical Trial. J. Tehran Heart Cent. 2017, 12, 57–64. [Google Scholar]
- Vandijck, D.M.; Reynvoet, E.; Blot, S.I.; Vandecasteele, E.; Hoste, E.A. Severe Infection, Sepsis and Acute Kidney Injury. Acta Clin. Belg. 2007, 62, 332–336. [Google Scholar] [CrossRef]
- Sayed-Ahmed, M.M.; Eissa, M.A.; Kenawy, S.A.; Mostafa, N.; Calvani, M.; Osman, A.M. Progression of Cisplatin-Induced Nephrotoxicity in a Carnitine-Depleted Rat Model. Chemotherapy 2004, 50, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Heuberger, W.; Berardi, S.; Jacky, E.; Pey, P.; Krähenbühl, S. Increased Urinary Excretion of Carnitine in Patients Treated with Cisplatin. Eur. J. Clin. Pharmacol. 1998, 54, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Cayir, K.; Karadeniz, A.; Yildirim, A.; Kalkan, Y.; Karakoc, A.; Keles, M.; Tekin, S. Protective Effect Of L-Carnitine Against Cisplatin-Induced Liver and Kidney Oxidant Injury in Rats. Cent. Eur. J. Med. 2009, 4, 184–191. [Google Scholar] [CrossRef]
- Yürekli, Y.; Unak, P.; Yenisey, C.; Ertay, T.; Biber Müftüler, F.Z.; Medine, E.İ. l-Carnitine Protection Against Cisplatin Nephrotoxicity in Rats: Comparison with Amifostin Using Quantitative Renal Tc 99m DMSA Uptake. Mol. Imaging Radionucl. Ther. 2011, 20, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Elkomy, A.; Abdelhiee, E.Y.; Fadl, S.E.; Emam, M.A.; Gad, F.A.; Sallam, A.; Alarifi, S.; Abdel-Daim, M.M.; Aboubakr, M. l-Carnitine Mitigates Oxidative Stress and Disorganization of Cytoskeleton Intermediate Filaments in Cisplatin-Induced Hepato-Renal Toxicity in Rats. Front. Pharmacol. 2020, 11, 574441. [Google Scholar] [CrossRef]
- Haghighatdoost, F.; Jabbari, M.; Hariri, M. The Effect Of L-Carnitine on Inflammatory Mediators: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Eur. J. Clin. Pharmacol. 2019, 75, 1037–1046. [Google Scholar] [CrossRef]
- Bárány, P.; Müller, H.J. Maintaining Control over Haemoglobin Levels: Optimizing the Management of Anaemia in Chronic Kidney Disease. Nephrol. Dial. Transplant. 2007, 22, iv10–iv18. [Google Scholar] [CrossRef]
- Ritz, E.; Bommer, J. Cardiovascular Problems on Hemodialysis: Current Deficits and Potential Improvement. Clin. J. Am. Soc. Nephrol. 2009, 4, S71–S78. [Google Scholar] [CrossRef]
- Kuwasawa-Iwasaki, M.; Io, H.; Muto, M.; Ichikawa, S.; Wakabayashi, K.; Kanda, R.; Nakata, J.; Nohara, N.; Tomino, Y.; Suzuki, Y. Effects Of L-Carnitine Supplementation in Patients Receiving Hemodialysis or Peritoneal Dialysis. Nutrients 2020, 12, 3371. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Xue, C.; Ou, J.; Xie, Z.; Deng, J. Effect of l-Carnitine Supplementation on Renal Anemia in Patients on Hemodialysis: A Meta-Analysis. Int. Urol. Nephrol. 2021, 53, 2149–2158. [Google Scholar] [CrossRef]
- Lankhorst, C.E.; Wish, J.B. Anemia in Renal Disease: Diagnosis and Management. Blood Rev. 2010, 24, 39–47. [Google Scholar] [CrossRef]
- Bonomini, M.; Zammit, V.; Pusey, C.D.; De Vecchi, A.; Arduini, A. Pharmacological Use of l-Carnitine in Uremic Anemia: Has Its Full Potential Been Exploited? Pharmacol. Res. 2011, 63, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Labonia, W.D. l-Carnitine Effects on Anemia in Hemodialyzed Patients Treated with Erythropoietin. Am. J. Kidney Dis. 1995, 26, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Bérard, E.; Barrillon, D.; Iordache, A.; Bayle, J.; Cassuto-Viguier, E. Low Dose of l-Carnitine Impairs Membrane Fragility of Erythrocytes in Hemodialysis Patients. Nephron 1994, 68, 145. [Google Scholar] [CrossRef]
- Matsumura, M.; Hatakeyama, S.; Koni, I.; Mabuchi, H.; Muramoto, H. Correlation Between Serum Carnitine Levels and Erythrocyte Osmotic Fragility in Hemodialysis Patients. Nephron 1996, 72, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Nikolaos, S.; George, A.; Telemachos, T.; Maria, S.; Yannis, M.; Konstantinos, M. Effect of l-Carnitine Supplementation on Red Blood Cells Deformability in Hemodialysis Patients. Ren. Fail. 2000, 22, 73–80. [Google Scholar] [CrossRef]
- Vlassopoulos, D.A.; Hadjiyannakos, D.K.; Anogiatis, A.G.; Evageliou, A.E.; Santikou, A.V.; Noussias, C.V.; Papandreou, P.T.; Hadjiconstantinou, V.E. Carnitine Action on Red Blood Cell Osmotic Resistance in Hemodialysis Patients. J. Nephrol. 2002, 15, 68–73. [Google Scholar]
- Savica, V.; Santoro, D.; Mazzaglia, G.; Ciolino, F.; Monardo, P.; Calvani, M.; Bellinghieri, G.; Kopple, J.D. l-Carnitine Infusions May Suppress Serum C-Reactive Protein and Improve Nutritional Status in Maintenance Hemodialysis Patients. J. Ren. Nutr. 2005, 15, 225–230. [Google Scholar] [CrossRef]
- Steiber, A.L.; Davis, A.T.; Spry, L.; Strong, J.; Buss, M.L.; Ratkiewicz, M.M.; Weatherspoon, L.J. Carnitine Treatment Improved Quality-of-Life Measure in A Sample of Midwestern Hemodialysis Patients. J. Parenter. Enter. Nutr. 2006, 30, 10–15. [Google Scholar] [CrossRef]
- Di Iorio, B.R.; Guastaferro, P.; Cillo, N.; Cucciniello, E.; Bellizzi, V. Long-Term l-Carnitine Administration Reduces Erythropoietin Resistance in Chronic Hemodialysis Patients with Thalassemia Minor. Drug Target Insights 2007, 2, 117739280700200001. [Google Scholar] [CrossRef]
- Naini, A.E.; Moradi, M.; Mortazavi, M.; Harandi, A.A.; Hadizadeh, M.; Shirani, F.; Ghafoori, H.B.; Naini, P.E. Effects of Oral l-Carnitine Supplementation on Lipid Profile, Anemia, and Quality of Life in Chronic Renal Disease Patients Under Hemodialysis: A Randomized, Double-Blinded, Placebo-Controlled Trial. J. Nutr. Metab. 2012, 2012, 510483. [Google Scholar] [CrossRef]
- El-Mashad, G.M.; El-Hawy, M.A.; NaserBahbah, H.M.; Bedair, H.M.; Habib, M.I. The Effect of l-Carnitine Therapy on Anaemia Therapy in Paediatric Patients on Regular Haemodialysis. Pediatria. Polska 2021, 96, 238–244. [Google Scholar] [CrossRef]
- Lynch, K.E.; Feldman, H.I.; Berlin, J.A.; Flory, J.; Rowan, C.G.; Brunelli, S.M. Effects of l-Carnitine on Dialysis-Related Hypotension and Muscle Cramps: A Meta-Analysis. Am. J. Kidney Dis. 2008, 52, 962–971. [Google Scholar] [CrossRef] [PubMed]
- Aoun, B.; Bérard, E.; Vitkevic, R.; Dehée, A.; Bensman, A.; Ulinski, T. l-Carnitine Supplementation and EPO Requirement in Children on Chronic Hemodialysis. Pediatr. Nephrol. 2010, 25, 557–560. [Google Scholar] [CrossRef]
- Sgambat, K.; Frank, L.; Ellini, A.; Sable, C.; Moudgil, A. Carnitine Supplementation Improves Cardiac Strain Rate in Children on Chronic Hemodialysis. Pediatr. Nephrol. 2012, 27, 1381–1387. [Google Scholar] [CrossRef]
- Ibarra-Sifuentes, H.R.; Del Cueto-Aguilera, Á.; Gallegos-Arguijo, D.A.; Castillo-Torres, S.A.; Vera-Pineda, R.; Martínez-Granados, R.J.; Atilano-Díaz, A.; Cuellar-Monterrubio, J.E.; Pezina-Cantú, C.O.; Martínez-Guevara, E.D.J.; et al. Levocarnitine Decreases Intradialytic Hypotension Episodes: A Randomized Controlled Trial. Ther. Apher. Dial. 2017, 21, 459–464. [Google Scholar] [CrossRef]
- Fischbach, M.; Terzic, J.; Menouer, S.; Dheu, C.; Seuge, L.; Zalosczic, A. Daily Online Haemodiafiltration Promotes Catch-Up Growth in Children on Chronic Dialysis. Nephrol. Dial. Transplant. 2010, 25, 867–873. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, C.W. Calcium Balance During Hemodialysis. Semin. Dial. 2008, 21, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, B.D. Debate Forum: Levocarnitine Therapy Is Rational and Justified in Selected Dialysis Patients. Blood Purif. 2006, 24, 128–139. [Google Scholar] [CrossRef]
- Tislér, A.; Akócsi, K.; Borbás, B.; Fazakas, L.; Ferenczi, S.; Görögh, S.; Kulcsár, I.; Nagy, L.; Sámik, J.; Szegedi, J.; et al. The Effect of Frequent or Occasional Dialysis-Associated Hypotension on Survival of Patients on Maintenance Haemodialysis. Nephrol. Dial. Transplant. 2003, 18, 2601–2605. [Google Scholar] [CrossRef]
- Shoji, T.; Tsubakihara, Y.; Fujii, M.; Imai, E. Hemodialysis-Associated Hypotension as An Independent Risk Factor for Two-Year Mortality in Hemodialysis Patients. Kidney Int. 2004, 66, 1212–1220. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Rhee, C.M.; Sim, J.J.; Kim, Y.L.; Ricks, J.; Streja, E.; Vashistha, T.; Tolouian, R.; Kovesdy, C.P.; Kalantar-Zadeh, K. A Comparative Effectiveness Research Study of The Change in Blood Pressure During Hemo-Dialysis Treatment and Survival. Kidney Int. 2013, 84, 795–802. [Google Scholar] [CrossRef]
- Hayes, W.; Hothi, D.K. Intradialytic Hypotension. Pediatr. Nephrol. 2011, 26, 867–879. [Google Scholar] [CrossRef]
- Herrera, M.D.; Bueno, R.; De Sotomayor, M.A.; Pérez-Guerrero, C.; Vázquez, C.M.; Marhuenda, E. Endothelium-Dependent Vasorelaxation Induced by l-Carnitine in Isolated Aorta from Normotensive and Hypertensive Rats. J. Pharm. Pharmacol. 2002, 54, 1423–1427. [Google Scholar] [CrossRef] [PubMed]
- Raina, R.; Lam, S.; Raheja, H.; Krishnappa, V.; Hothi, D.; Davenport, A.; Chand, D.; Kapur, G.; Schaefer, F.; Sethi, S.K.; et al. Pediatric Intradialytic Hypotension: Recommendations from the Pediatric Continuous Renal Replacement Therapy (PCRRT) Workgroup. Pediatr. Nephrol. 2019, 34, 925–941. [Google Scholar] [CrossRef] [PubMed]
- Chanchlani, R.; Young, C.; Farooq, A.; Sanger, S.; Sethi, S.; Chakraborty, R.; Tibrewal, A.; Raina, R. Evolution and Change in Paradigm of Hemodialysis in Children: A Systematic Review. Pediatr. Nephrol. 2021, 36, 1255–1271. [Google Scholar] [CrossRef]
- Valgas da Silva, C.P.; Rojas-Moscoso, J.A.; Antunes, E.; Zanesco, A.; Priviero, F.B. l-Carnitine Supplementation Impairs Endothelium-Dependent Relaxation in Mesenteric Arteries from Rats. Arch. Physiol. Biochem. 2014, 120, 112–118. [Google Scholar] [CrossRef]
- Atalay Guzel, N.; Erikoglu Orer, G.; Sezen Bircan, F.; Coskun Cevher, S. Effects of Acute l-Carnitine Supplementation on Nitric Oxide Production and Oxidative Stress After Exhaustive Exercise in Young Soccer Players. J. Sports Med. Phys. Fit. 2015, 55, 9–15. [Google Scholar]
- Signorelli, S.S.; Fatuzzo, P.; Rapisarda, F.; Neri, S.; Ferrante, M.; Conti, G.O.; Fallico, R.; Di Pino, L.; Pennisi, G.; Celotta, G.; et al. Propionyl-l-Carnitine Therapy: Effects on Endothelin-1 and Homocysteine Levels in Patients with Peripheral Arterial Disease and End-Stage Renal Disease. Kidney Blood Press. Res. 2006, 29, 100–107. [Google Scholar] [CrossRef]
- Riley, S.; Rutherford, S.; Rutherford, P.A. Low Carnitine Levels in Hemodialysis Patients: Relationship with Functional Activity Status and Intra-Dialytic Hypotension. Clin. Nephrol. 1997, 48, 392–393. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S. l-Carnitine in Dialysis Patients. Semin. Dial. 2001, 14, 209–217. [Google Scholar] [CrossRef]
- Kudoh, Y.; Aoyama, S.; Torii, T.; Chen, Q.; Nagahara, D.; Sakata, H.; Nozawa, A. Hemodynamic Stabilizing Effects of l-Carnitine in Chronic Hemodialysis Patients. Cardiorenal Med. 2013, 3, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Remppis, A.; Ritz, E. Cardiac Problems in The Dialysis Patient: Beyond Coronary Disease. Semin. Dial. 2008, 21, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Herzog, C.A.; Asinger, R.W.; Berger, A.K.; Charytan, D.M.; Díez, J.; Hart, R.G.; Eckardt, K.-U.; Kasiske, B.L.; McCullough, P.A.; Passman, R.S.; et al. Cardiovascular Disease in Chronic Kidney Disease. A Clinical Update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2011, 80, 572–586. [Google Scholar] [CrossRef] [PubMed]
- Jablonski, K.L.; Chonchol, M. Recent Advances in The Management of Hemodialysis Patients: A Focus on Cardiovascular Disease. F1000 Prime Rep. 2014, 6, 72. [Google Scholar] [CrossRef] [PubMed]
- Romagnoli, G.F.; Naso, A.; Carraro, G.; Lidestri, V. Beneficial Effects of l-Carnitine in Dialysis Patients with Impaired Left Ventricular Function: An Observational Study. Curr. Med. Res. Opin. 2002, 18, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Sakurabayashi, T.; Miyazaki, S.; Yuasa, Y.; Sakai, S.; Suzuki, M.; Takahashi, S.; Hirasawa, Y. l-Carnitine Supplementation De-Creases the Left Ventricular Mass in Patients Undergoing Hemodialysis. Circ. J. 2008, 72, 926–931. [Google Scholar] [CrossRef]
- Nishimura, M.; Tokoro, T.; Takatani, T.; Sato, N.; Nishida, M.; Hashimoto, T.; Yamazaki, S.; Kobayashi, H.; Ono, T. Effects of Intravenous l-Carnitine on Myocardial Fatty Acid Imaging in Hemodialysis Patients: Responders or Non-Responders to l-Carnitine. Springerplus 2015, 4, 353. [Google Scholar] [CrossRef]
- Higuchi, T.; Abe, M.; Yamazaki, T.; Okawa, E.; Ando, H.; Hotta, S.; Oikawa, O.; Kikuchi, F.; Okada, K.; Soma, M. Levocarnitine Improves Cardiac Function in Hemodialysis Patients with Left Ventricular Hypertrophy: A Randomized Controlled Trial. Am. J. Kidney Dis. 2016, 67, 260–270. [Google Scholar] [CrossRef]
- Huda, M.N.; Kim, M.; Bennett, B.J. Modulating the Microbiota as A Therapeutic Intervention for Type 2 Diabetes. Front. Endo-crinol. 2021, 12, 632335. [Google Scholar] [CrossRef]
- Sikalidis, A.K.; Maykish, A. The Gut Microbiome and Type 2 Diabetes Mellitus: Discussing a Complex Relationship. Biomedicines 2020, 8, 8. [Google Scholar] [CrossRef]
- Sumida, K.; Lau, W.L.; Kalantar-Zadeh, K.; Kovesdy, C.P. Novel Intestinal Dialysis Interventions and Microbiome Modulation to Control Uremia. Curr. Opin. Nephrol. Hypertens. 2022, 31, 82–91. [Google Scholar] [CrossRef]
- Rhee, E.P. How Omics Data Can Be Used in Nephrology. Am. J. Kidney Dis. 2018, 72, 129–135. [Google Scholar] [CrossRef]
- Dubin, R.F.; Rhee, E.P. Proteomics and Metabolomics in Kidney Disease, Including Insights into Etiology, Treatment, and Prevention. Clin. J. Am. Soc. Nephrol. 2020, 5, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Trionfini, P.; Benigni, A. MicroRNAs as Master Regulators of Glomerular Function in Health and Disease. J. Am. Soc. Nephrol. 2017, 28, 1686–1696. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Agborbesong, E.; Li, X. The Role of Mitochondria in Acute Kidney Injury and Chronic Kidney Disease and Its Therapeutic Potential. Int. J. Mol. Sci. 2021, 22, 11253. [Google Scholar] [CrossRef] [PubMed]
- Fontecha-Barriuso, M.; Lopez-Diaz, A.M.; Guerrero-Mauvecin, J.; Miguel, V.; Ramos, A.M.; Sanchez-Niño, M.D.; Ruiz-Ortega, M.; Ortiz, A.; Sanz, A.B. Tubular Mitochondrial Dysfunction, Oxidative Stress, And Progression of Chronic Kidney Disease. Antioxidants 2022, 11, 1356. [Google Scholar] [CrossRef] [PubMed]
- Idrovo, J.P.; Yang, W.L.; Nicastro, J.; Coppa, G.F.; Wang, P. Stimulation of Carnitine Palmitoyltransferase 1 Improves Renal Function and Attenuates Tissue Damage after Ischemia/Reperfusion. J. Surg. Res. 2012, 177, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Miguel, V.; Tituaña, J.; Herrero, J.I.; Herrero, L.; Serra, D.; Cuevas, P.; Barbas, C.; Puyol, D.R.; Márquez-Expósito, L.; Ruiz-Ortega, M.; et al. Renal Tubule Cpt1a Overexpression Protects from Kidney Fibrosis by Restoring Mitochondrial Homeostasis. J. Clin. Investig. 2021, 131, e140695. [Google Scholar] [CrossRef]
- Gao, Z.; Zhang, C.; Peng, F.; Chen, Q.; Zhao, Y.; Chen, L.; Wang, X.; Chen, X. Hypoxic Mesenchymal Stem Cell-Derived Extra-Cellular Vesicles Ameliorate Renal Fibrosis after Ischemia-Reperfusion Injury by Restoring CPT1A Mediated Fatty Acid Oxidation. Stem Cell Res. Ther. 2022, 13, 191. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ulinski, T.; Cirulli, M.; Virmani, M.A. The Role of L-Carnitine in Kidney Disease and Related Metabolic Dysfunctions. Kidney Dial. 2023, 3, 178-191. https://doi.org/10.3390/kidneydial3020016
Ulinski T, Cirulli M, Virmani MA. The Role of L-Carnitine in Kidney Disease and Related Metabolic Dysfunctions. Kidney and Dialysis. 2023; 3(2):178-191. https://doi.org/10.3390/kidneydial3020016
Chicago/Turabian StyleUlinski, Tim, Maria Cirulli, and Mohamed Ashraf Virmani. 2023. "The Role of L-Carnitine in Kidney Disease and Related Metabolic Dysfunctions" Kidney and Dialysis 3, no. 2: 178-191. https://doi.org/10.3390/kidneydial3020016
APA StyleUlinski, T., Cirulli, M., & Virmani, M. A. (2023). The Role of L-Carnitine in Kidney Disease and Related Metabolic Dysfunctions. Kidney and Dialysis, 3(2), 178-191. https://doi.org/10.3390/kidneydial3020016





