Abstract
The prevention of peritoneal dialysis (PD) catheter complications is essential to achieve a successful outcome. In recent years, nephrologists have performed more PD catheter insertion surgeries in Japan. The prevention of catheter complications is crucial for nephrologists who do not have all-around surgical skills. PD catheter tip migration is a common complication and a significant cause of catheter malfunction. Several preventive techniques have been reported for the PD catheter tip migration. This perspective described the following: (1) surgical technique in laparotomy, (2) laparoscopic surgery, (3) peritoneal wall anchor technique, and (4) catheter type selection. We hope that more effective methods of preventing catheter complications will be developed to ensure the success of PD treatment.
1. Introduction
Peritoneal dialysis (PD) is an excellent renal replacement therapy, providing a better quality of life [1], prognosis comparable to hemodialysis [2,3,4,5], and preservation of residual renal function [6]. However, PD remains underutilized in Japan. One of the reasons for this is that nephrologists in Japan tend to hesitate to ask the surgeons to perform PD catheter placement surgery. In recent years, nephrologists themselves have performed a high number of PD catheter insertion surgeries with successful outcomes [7,8,9]. However, the prevention of catheter complications is crucial for nephrologists who do not have all-around surgical skills. PD catheter tip migration is a common complication and a significant cause of catheter malfunction [10,11]. Successful PD depends on avoiding this complication. Recently, several techniques and modifications have been reported for the prevention of PD catheter tip migration. This perspective aimed to introduce and outline several methods of preventing PD catheter migration.
2. The Procedures to Prevent PD Catheter Tip Migration
2.1. Surgical Technique in Laparotomy
2.1.1. Modification of Deep Cuff Fixation
PD catheter placement surgery in laparotomy is a standard and widely performed procedure. Most nephrologists are trained in this procedure. The standard procedure involves putting a peritoneum purse-string suture just under the deep cuff to fix the catheter to the peritoneum. A concern with this fixation design is that the external force used to position the deep cuff perpendicular to the abdominal wall may cause the catheter tip to easily lift from the pouch of Douglas.
A Japanese textbook described an unique technique involving the deep cuff being placed 2–3 cm away from the peritoneum purse-string suture [12]. As the catheter around the deep cuff is fixed in parallel with the anterior sheath of the rectus abdominis, the catheter in the abdominal cavity is subjected to a reaction force toward the anterior abdominal wall, with the purse-string suture as a leverage point. Accordingly, the force lifting the catheter tip from the pouch of Douglas attenuates and prevents the catheter tip from lifting (Figure 1). This method is also effective in preventing deep cuff infection during PD-related peritonitis because of the distance between the deep cuff and the peritoneum [12]. Using a catheter reinforced with thicker silicone around the deep cuff would also prevent catheter migration.
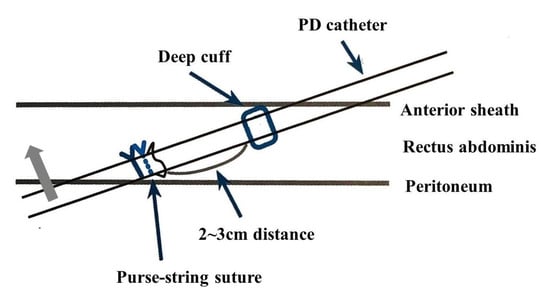
Figure 1.
Unique deep cuff fixation (modified from reference [12] with permission). The deep cuff is placed 2–3 cm away from the peritoneum purse-string suture. The gray arrow indicates the reaction force from the catheter tip to the anterior abdominal wall.
2.1.2. Insert Position
Generally, the PD catheter is inserted from a paramedian–subumbilical position of the abdomen. Some studies have reported using the “very low site approach” to reduce the risk of catheter migration. With this approach, the catheter is inserted a few centimeters above the suprapubic margin, reducing the risk of catheter migration [13,14,15]. This approach requires an adaptative catheter cut extending from the insertion point at the peritoneum to the pelvic floor. Although the authors did not report any complications due to the catheter cut, careful consideration before using this technique is necessary since it is undeniable that additional cutting degrades the catheter’s strength. Recently, a successful approach from Mcburney points with laparoscopic assistance has been reported [16]. This procedure is one of the very low site approaches.
A very low site approach could be one of the options depending on the patient’s condition. These procedures shorten the catheter’s intra-abdominal length and reduce the free part of the catheter in the abdominal cavity. Consequently, these procedures enhance resilience by positioning the catheter tip at the bottom of the abdominal cavity and lowering its migration risk.
Japanese surgeons have reported fixating the PD catheter to the recto-uterine or rectovesical pouch under direct vision [17]. In this procedure, a catheter was inserted from the lower abdomen where the bladder or uterine could be seen directly. Greater success was demonstrated in preventing PD catheter migration using this method, compared with the conventional procedure. Nevertheless, the method seems challenging to nephrologists.
2.2. Laparoscopic Catheter Placement
Laparoscopic PD catheter placement surgery is an important option. It has a significant advantage of being less invasive. In laparoscopic surgery, the PD catheter tip can be placed in the pouch of Douglas directly with visual assistance. Recent systematic reviews have shown that the incidence of catheter migration is significantly lowered in laparoscopic catheterization than in open surgery [18,19]. On the contrary, a subgroup analysis has revealed that fixing sutures of the catheter to the abdominal wall contributed to reducing the risk of catheter dislocation and not the laparoscopic technique [19]. Another meta-analysis has shown that advanced laparoscopic intervention produces a better outcome than basic laparoscopy used to verify the catheter position. The advanced technique is indicated for omentopexy, adhesiolysis, excision of appendix epiploica (epiploectomy), salpingectomy, and colopexyx [20]. Essentially, skilled surgeons, rather than general nephrologists, should perform these laparoscopic surgeries. Further analysis is needed to determine whether laparoscopic surgery is effective in preventing catheter tip dislocation.
In Japan, national medical insurance does not cover laparoscopic PD catheter placement, so the hospitals that use this modality have to bear the surgery cost. Currently, the Guidelines for PD from the Japanese Society of Dialysis Treatment do not recommend laparoscopic catheter insertion [21]. Laparoscopic catheter insertion should be selected according to the situation, including hospital capability and the risk-benefit for the patients.
2.3. Peritoneal Wall Anchor Technique (PWAT)
In Japan, a unique technique of fixing a catheter to the anterior peritoneal wall called PWAT has been developed and applied widely. Fixing the suture of the catheter to the anterior peritoneal wall prevents excessive movement of the catheter and tip migration. The original method of PWAT requires laparoscopic assistance or a particular device named the PWAT applicator [22,23]. Recently, a simple modified PWAT, which does not require laparoscopic assistance or special devices has been established [24]. It was reported that the modified PWAT achieved a better catheter survival rate than the traditional method by preventing catheter tip migration [24].
We use the modified PWAT, in combination with the peritoneum purse-string suture, 2–3 cm away from the deep cuff, as described earlier. This combined method prevented catheter tip migration by PWAT technique and minimized the reactive force directing the catheter to the anterior abdominal wall (Figure 2). Since we started using this combined procedure, we have not experienced any catheter dysfunction clinically.
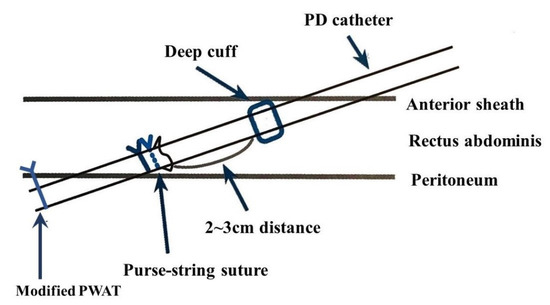
Figure 2.
Unique deep cuff fixation combined with the modified PWAT (modified from reference [12] with permission).
2.4. Catheter Type Selection
Many comparative studies investigating the effect of PD catheter tip design on catheter complications have been conducted. Significantly, comparisons between the coiled type catheters and straight type catheters are still controversial. Some meta-analyses have found no significant difference in the risk of catheter tip migration between the two types of PD catheter [25,26]. However, the results of another pooled meta-analysis have suggested that coiled catheters may be more prone to migration [27]. Further large-scale comparative studies are expected to be conducted.
In Europe, the self-locating catheter with small tungsten weights attached to its tip is available. The tungsten 12-g weights prevent the catheter from moving out of the pouch of Douglas under its weight [28,29,30]. However, it is not marketed in Japan. We obtained the catheters by personally importing them and used them in some patients with the permission of the Ethics Committee of our hospital (Figure 3). Catheter migration did not occur in the procedure we experienced using the self-locating catheter [31]. We hope that the catheter will officially become available in Japan in the future.
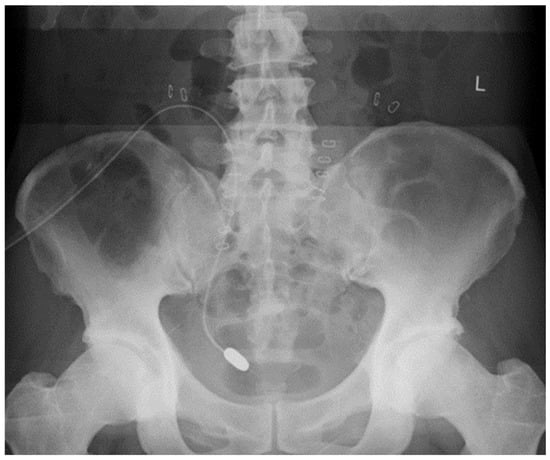
Figure 3.
Abdominal X-ray image of the correct positioning of the self-locating catheter. The patient was a man, aged 64 years. A self-locating catheter was placed due to repeated catheter migration. The patient’s written consent was obtained for the publication of the image.
3. Conclusions
In this perspective, we presented the methods for preventing PD catheter migration (Table 1). All of the methods described have been reported to be highly effective. However, some methods require greater surgical skills. We recommend that a method be selected on the basis of the patient’s condition and the surgical skills of the nephrologist. It never denies that nephrologists can not perform highly technical operations. Rather, we believe that nephrologists can acquire advanced surgical skills and perform highly technical operations if they want. Although there are no accurate data available, the number of medical facilities providing PD is overwhelmingly tiny compared to those providing hemodialysis in Japan. Even some training hospitals do not offer PD, suggesting that young nephrologists have limited opportunities to learn about PD-related surgery. It is conceivable that increasing the number of facilities to learn PD-related surgery is essential in Japan.

Table 1.
Summary of methods to prevent PD catheter tip migration.
It is hoped that more effective methods of preventing catheter complications will be developed to ensure the success of PD treatment, achieving a better quality of life for PD patients.
Author Contributions
Conceptualization, M.I. and M.K.; writing—original draft preparation, M.I.; writing—review and editing, M.I. and M.K. Both authors have read and agreed to the published version of the manuscript.
Funding
This perspective received no external funding.
Acknowledgments
We thank Toshihide Naganuma, the chairman of the 24th Annual Meeting of the Japanese Society of Dialysis Access, for allowing us to write a perspective for this journal. Furthermore, we are very grateful to the Japanese Society for Peritoneal Dialysis for their permission to use a figure from a textbook.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Segall, L.; Nistor, I.; Van Biesen, W.; Brown, E.A.; Heaf, J.G.; Lindley, E.; Farrington, K.; Covic, A. Dialysis modality choice in elderly patients with end-stage renal disease: A narrative review of the available evidence: Table 1. Nephrol. Dial. Transplant. 2015, 32, gfv411. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-K.; Hsu, C.-C.; Hwang, S.-J.; Chen, P.-C.; Huang, C.-C.; Li, T.-C.; Sung, F.-C. A Comparative Assessment of Survival Between Propensity Score-Matched Patients With Peritoneal Dialysis and Hemodialysis in Taiwan. Medicine 2012, 91, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Yeates, K.; Zhu, N.; Vonesh, E.; Trpeski, L.; Blake, P.; Fenton, S. Hemodialysis and peritoneal dialysis are associated with similar outcomes for end-stage renal disease treatment in Canada. Nephrol. Dial. Transplant. 2012, 27, 3568–3575. [Google Scholar] [CrossRef]
- Lukowsky, L.R.; Mehrotra, R.; Kheifets, L.; Arah, O.A.; Nissenson, A.R.; Kalantar-Zadeh, K. Comparing Mortality of Peritoneal and Hemodialysis Patients in the First 2 Years of Dialysis Therapy: A Marginal Structural Model Analysis. Clin. J. Am. Soc. Nephrol. 2013, 8, 619–628. [Google Scholar] [CrossRef]
- Kumar, V.A.; Sidell, M.A.; Jones, J.P.; Vonesh, E.F. Survival of propensity matched incident peritoneal and hemodialysis patients in a United States health care system. Kidney Int. 2014, 86, 1016–1022. [Google Scholar] [CrossRef]
- Tam, P. Peritoneal Dialysis and Preservation of Residual Renal Function. Perit. Dial. Int. 2009, 29, 108–110. [Google Scholar] [CrossRef]
- Osako, K.; Sakurada, T.; Koitabashi, K.; Sueki, S.; Shibagaki, Y. Early Postoperative Complications of Peritoneal Dialysis Catheter Surgery Conducted by Nephrologists: A Single-Center Experience Over an Eight-Year Period. Adv. Perit. Dial. Conf. Perit. Dial. 2017, 33, 26–30. [Google Scholar]
- Washida, N.; Aikawa, K.; Inoue, S.; Kasai, T.; Shinozuka, K.; Morimoto, K.; Hosoya, K.; Hayashi, K.; Itoh, H. Impact of Peritoneal Dialysis Catheter Insertion by a Nephrologist: Results of a Questionnaire Survey of Patients and Nurses. Adv. Perit. Dial. Conf. Perit. Dial. 2015, 31, 59–68. [Google Scholar]
- Asif, A.; Pflederer, T.A.; Vieira, C.F.; Diego, J.M.; Roth, D.A.; Agarwal, A. American Society of Diagnostic and Interventional Nephrology Section Editor: Stephen Ash: Does Catheter Insertion by Nephrologists Improve Peritoneal Dialysis Utilization? A Multicenter Analysis. Semin. Dial. 2008, 18, 157–160. [Google Scholar] [CrossRef]
- Crabtree, J. Selected best demonstrated practices in peritoneal dialysis access. Kidney Int. 2006, 70, S27–S37. [Google Scholar] [CrossRef][Green Version]
- Crabtree, J.H. Peritoneal Dialysis Catheter Implantation: Avoiding Problems and Optimizing Outcomes. Semin. Dial. 2014, 28, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Tanno, A. Peritoneal Dialysis Catheter Insertion Surgery. In Text Book of Peritoneal Dialysis; Jun, M., Ed.; Japanese Society for Peritoneal Dialysis: Tokyo, Japan, 2020; pp. 48–53. [Google Scholar]
- Zhang, L.; Liu, J.; Shu, J.; Hu, J.; Yu, X.; Mao, H.; Ren, H.; Hong, H.; Xing, C. Low-site peritoneal catheter implantation decreases tip migration and omental wrapping. Perit. Dial. Int. 2011, 31, 202–204. [Google Scholar] [CrossRef] [PubMed]
- Gong, L.-F.; Lu, J.-K.; Tang, W.-G.; Xu, W.; Xu, M.; Ma, G.-X. Peritoneal dialysis catheter insertion using a very-low-site approach: A 5-year experience. Int. Urol. Nephrol. 2019, 51, 1053–1058. [Google Scholar] [CrossRef]
- Gong, L.; Xu, W.; Tang, W.; Lu, J.; Li, Y.; Jiang, H.; Li, H. Low-site versus traditional peritoneal dialysis catheterization. Medicine 2020, 99, e23311. [Google Scholar] [CrossRef]
- Ogawa, K.; Maruyama, Y.; Matsuo, N.; Tanno, Y.; Ohkido, I.; Hirano, K.; Ikeda, M.; Yokoo, T. The efficacy and safety of a novel method of peritoneal dialysis catheter insertion from the McBurney point. Ren. Replace. Ther. 2020, 6, 1–6. [Google Scholar] [CrossRef]
- Kume, H.; Miyazaki, H.; Nagata, M.; Ishikawa, A.; Ishibashi, Y.; Fujita, T.; Homma, Y. Peritoneal Fixation Prevents Dislocation of Tenckhoff Catheter. Perit. Dial. Int. 2011, 31, 694–697. [Google Scholar] [CrossRef]
- Chen, Y.; Shao, Y.; Xu, J. The Survival and Complication Rates of Laparoscopic Versus Open Catheter Placement in Peritoneal Dialysis Patients. Surg. Laparosc. Endosc. Percutaneous Tech. 2015, 25, 440–443. [Google Scholar] [CrossRef]
- Sakurada, T.; Ueda, A.; Komukai, D.; Uchiyama, K.; Tsujimoto, Y.; Yuasa, H.; Ryuzaki, M.; Ito, Y.; Tomo, M.; Nakamoto, H. Outcomes after peritoneal dialysis catheter placement by laparoscopic surgery versus open surgery: Systematic review and meta-analysis. Ren. Replace. Ther. 2019, 5, 1–13. [Google Scholar] [CrossRef]
- Shrestha, B.M.; Shrestha, D.; Kumar, A.; Shrestha, A.; Boyes, S.A.; Wilkie, M. Advanced Laparoscopic Peritoneal Dialysis Catheter Insertion: Systematic Review and Meta-Analysis. Perit. Dial. Int. 2018, 38, 163–171. [Google Scholar] [CrossRef]
- Working Group on Revision of Peritoneal Dialysis Guidelines, J.; Therapy, S. for D. Part 2. In 2019 JSDT Giudelines for Peritoneal Dialysis; Japanese Society for Dialysis Therapy, Ed.; Igakutosho Syuppann: Tokyo, Japan, 2019; pp. 115–128. (In Japanese) [Google Scholar]
- Fukasawa, M.; Matsushita, K.; Kamiyama, M.; Mochizuki, T.; Mikami, Y.; Zakouji, H.; Araki, I.; Takeda, M. A new peritoneal wall anchor technique (PWAT) for peritoneal catheter malposition. Nihon Toseki Igakkai Zasshi 2006, 39, 235–242. [Google Scholar] [CrossRef][Green Version]
- Fukasawa, M.; Matsushita, K.; Teramoto, S.; Miyamoto, T.; Zakouji, H.; Araki, I.; Tanabe, N.; Takeda, M. Two Catheter Case Reports of Peritoneal by Wall Anchor Technique for Peritoneal Tip Translocation Using Laparoscopy; Department of Urology, Faculty of Medicine, Nihon Toseki Igakkai Zasshi: Tokyo, Japan, 2003; pp. 1567–1572. [Google Scholar]
- Oka, H.; Yamada, S.; Kamimura, T.; Hara, M.; Hirashima, Y.; Matsueda, S.; Shukuri, T.; Aihara, S.; Koresawa, M.; Eriguchi, M.; et al. Modified Simple Peritoneal Wall Anchor Technique (Pwat) in Peritoneal Dialysis. Perit. Dial. Int. 2017, 37, 103–108. [Google Scholar] [CrossRef]
- Hagen, S.M.; Lafranca, J.; Ijzermans, J.N.; Dor, F.J. A systematic review and meta-analysis of the influence of peritoneal dialysis catheter type on complication rate and catheter survival. Kidney Int. 2014, 85, 920–932. [Google Scholar] [CrossRef]
- Chow, K.M.; Wong, S.S.M.; Ng, J.K.C.; Cheng, Y.L.; Leung, C.B.; Pang, W.F.; Fung, W.W.S.; Szeto, C.C.; Li, P.K.T. Straight Versus Coiled Peritoneal Dialysis Catheters: A Randomized Controlled Trial. Am. J. Kidney Dis. 2020, 75, 39–44. [Google Scholar] [CrossRef]
- Xie, J.; Kiryluk, K.; Ren, H.; Zhu, P.; Huang, X.; Shen, P.; Xu, T.; Chen, X.; Chen, N. Coiled Versus Straight Peritoneal Dialysis Catheters: A Randomized Controlled Trial and Meta-analysis. Am. J. Kidney Dis. 2011, 58, 946–955. [Google Scholar] [CrossRef]
- Di Paolo, N.; Petrini, G.; Garosi, G.; Buoncristiani, U.; Brardi, S.; Monaci, G. A New Self-Locating Peritoneal Catheter. Perit. Dial. Int. 1996, 16, 623–627. [Google Scholar] [CrossRef]
- Di Paolo, N.; Capotondo, L.; Brardi, S.; Nicolai, G. The Self-Locating Peritoneal Catheter: Fifteen Years of Experience. Perit. Dial. Int. 2010, 30, 504–505. [Google Scholar] [CrossRef] [PubMed]
- Bergamin, B.; Senn, O.; Corsenca, A.; Dutkowski, P.; Weber, M.; Wüthrich, R.P.; Segerer, S.; Thut, M.P. Finding the Right Position: A Three-Year, Single-Center Experience with the “Self-Locating” Catheter. Perit. Dial. Int. 2010, 30, 519–523. [Google Scholar] [CrossRef]
- Ito, M. Experimetal Use of Self-Locating Catheter. Kidney Dial. 2012, 73, 184–185. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).