Abstract
During the COVID-19 pandemic, vaccination hesitancy (VH) posed an equally unexpected and significant obstacle to the effectiveness of public health interventions. VH has not only the potential to stir up public unrest, but it may also impede the success of entire immunization programs and thus prevent the attainment of herd immunity. This cross-sectional, quantitative, and descriptive study examined VH and vaccination behavior (VB) among 3486 university students in Ghana, using a standardized self-administered questionnaire based on the 5Cs model among other relevant variables. The findings confirm a significant VH and a VB influenced by both sociodemographic factors, such as gender (OR: 1.45; [CI: 1.26–1.67]), study program (OR: 0.55; [CI: 0.47–0.64]), and ethnicity (OR: 1.31; [CI: 1.12–1.52]) and also four of the 5Cs, i.e., Confidence (OR:1.56; [CI: 1.45–1.68]), Constraints (OR: 0.83; [CI: 0.78–0.87]), Calculation (OR:0.85; [CI: 0.78–0.92]), and Collective Responsibility (OR:1.27; [CI: 1.16–1.38]), yet not Complacency, nor religion. Notably, VH was further shaped by previous vaccine experience, information sources, vaccine attributes, stance on vaccine passport, and conspiracy beliefs, with misinformation from unofficial sources playing a key role. The multiple regression models explained 11% to 34% of the variance in the 5Cs, indicating varying degrees of explanatory power for each factor influencing VB and eventually also VH. This study highlights the urgent need for targeted public health interventions, such as integrating vaccine education into university orientation programs, streamlining vaccination processes, and leveraging influencers for trust-building campaigns.
1. Introduction
Although the COVID-19 pandemic of about five years ago has been superseded in the news by war and other natural and manmade disasters, this viral outbreak has claimed over 6 million lives worldwide [1,2]. In many countries of the Global South, such as Ghana, the effects of COVID-19, combined with other infections, continue to be significant, exacerbating a constant strain on the healthcare system and the economy [3,4,5]. Confronted by other infectious diseases, such as Ebola, influenza, malaria, cholera, meningitis, HIV/AIDS, and a very recent outbreak of Mpox, vaccination in these countries is as important as ever and indeed the most effective antidote to future epidemics and pandemics.
Yet, despite modern research and the development of effective and safe vaccines for many of these infectious diseases, vaccination is not simply an automatism. Even during the COVID-19 outbreak, large sections of populations in many countries worldwide have refused to take the vaccines available [6,7]. In some countries, such as Germany, this has even led to protests, riots, and new political parties ready to fight for the “right” to not be vaccinated [8,9]. Indeed, the underlying behavior, known as “vaccination hesitancy” (VH), and defined by the Strategic Advisory Group of Experts on Immunization (SAGE) affiliated with the WHO as “the refusal or a delay in accepting vaccines despite their availability” [10,11], remains a major hindrance to achieving herd immunity in many countries [12]. Studies have confirmed that vaccination hesitancy poses a major obstacle in the fight against the outbreaks of infectious diseases, which may lead to epidemics and eventually to pandemics [13,14,15,16,17]. In some cases, such as cholera and meningitis, VH—and not limited access to or effectiveness of modern, adequate vaccines—may even turn out to be the main factor behind those outbreaks [18].
Ghana stands out among the African countries not only because of the devastating impact of COVID-19 on its society, but it was also the first country to receive COVID-19 vaccines through the COVID-19 Vaccines Global Access (COVAX) Facility on 24 February 2021. Yet, despite this “early” access to COVID-19 vaccines, only 16% of Ghanaians were fully vaccinated by March 2022, with 71% not receiving the second dose [19,20,21]. Even in 2023, Ghana’s COVID-19 vaccination rate was still less than 32% and thus behind many African countries such as Rwanda and Mozambique [22]. Indeed, published studies have reported some possible reasons, including concerns about vaccine safety, origins, limited funds, and logistical requirements with the limited shelf-life of vaccines [23,24].
Low vaccination willingness remains a major issue to this day, especially among highly educated young adults. At first, this may be rather surprising as one often instinctively associates the educated “informed citizen” with rational decisions and choices. Nonetheless, our previous study already reported a mismatch between high levels of knowledge about infectious diseases including influenza, cholera, and COVID-19 on the one side and a surprisingly low, often irresponsible practice of preventive measures on the other, including, indeed, a low willingness to be vaccinated [25]. This poses the question of why educated and informed young adults exhibit such a pronounced hesitancy towards being vaccinated despite obviously “knowing it better”. In that study [25], higher levels of knowledge about infectious diseases correlated positively with higher levels of education and younger adults. Indeed, the decision to accept or to refuse a vaccine is influenced by an individual’s psychological factors which may not always follow a predictable or definite pattern. This choice may come after an intricate deliberation process possibly affected by a myriad of personal and social factors [26].
The 5Cs model developed and validated by Betsch et al. (2018) and built upon established theoretical frameworks, such as the Health Belief Model and the Theory of Planned Behavior, is widely adopted and accepted in the literature for predicting hesitancy behavior [27]. It employs five psychological constructs, called “antecedents of vaccinations”, namely Confidence, Complacency, Constraints/Convenience, Calculation, and Collective Responsibility. These constructs, in turn, may be influenced by various environmental factors subsumed under the so-called “epidemiological triad of the environment”, composed of (a) social determinants, such as public health policies, messages spread by media, and social factors, (b) the vaccine and disease itself (perception of vaccine safety, effectiveness, and perceived susceptibility to the disease), and (c) the host (i.e., knowledge, previous experience, and educational level) [10,27,28,29,30,31,32]. The five antecedents and their predictive roles in influencing VH are presented in Figure 1.
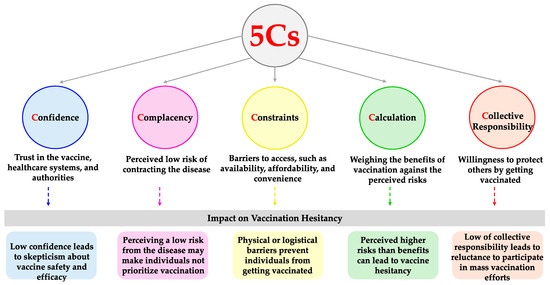
Figure 1.
Schematic representation of the ‘5Cs psychological antecedents’ and their predictive influence on VH.
Is it possible to identify the factors underlying this VH and thus develop strategies to influence them in order to minimize VH and increase the success of vaccination campaigns? This study therefore aims to assess VH among university students in Ghana, utilizing the 5Cs model, in order to examine the influence of each of the 5Cs psychological antecedents of vaccination behavior and to explore the impact of multiple external, environmental variables, such as vaccination experience/history, conspiracy mentality/misinformation, sources of vaccination information (official and unofficial), vaccine passport and vaccine attributes on these 5Cs, and subsequently the individual inclination towards vaccination.
2. Materials and Methods
2.1. Questionnaire
The standardized 51-item questionnaire consisted of three main sections (https://doi.org/10.17605/OSF.IO/AFUP7, accessed on 25 March 2025) The first section probed sociodemographic information of participants including age (year of birth), gender, religion, ethnicity, and study program. The second section included participants’ information regarding vaccines, that is, their vaccine experience (whether they have previously received eight specific vaccines such as against COVID-19, polio, and yellow fever), sources of information about vaccines such as governmental agencies, social influencers and/or scientific literature, and misinformation about vaccines (conspiracy theories regarding vaccines which were common around the time of this study and featured in local news or social media platforms such as vaccines being ineffective, causing infertility, or simply produced for financial gain). It should be noted that one item exploring misinformation about vaccines was true, “Vaccines sensitize the body and offer protection against diseases”, and was included to enhance quality during data collection. The third section was dedicated to evaluating psychological antecedents regarding vaccines. Here, the participants’ responses to the 5Cs (Confidence, Complacency, Constraints, Calculation, and Collective Responsibility), adopted from Betsch et al. (2018) were assessed [26]. Each antecedent of the 5Cs was measured through three items; the long version of the model, consisting of 15 items, was employed. Afterwards, the influence of attributes related to vaccines (origin, brand name, and popularity) on participants’ willingness to accept such vaccines, as well as participants’ perception of the effectiveness and acceptability of vaccine passports was each measured with one item. It should be noted that, despite the questionnaire consisting of 51 items, only data pertaining to 45 items were processed and presented in the current study.
2.2. Study Design and Data Collection
The questionnaire was distributed physically (paper form) and digitally (sharing of link or scanning of a QR code) between July 2022 and October 2022 by the principal investigator and trained volunteers at the designated locations, Kwame Nkrumah University of Science and Technology (KNUST), University of Ghana (UG), and University of Cape Coast (UCC), after acquiring consent, and the questionnaire was self-administered by participants (https://doi.org/10.17605/OSF.IO/AFUP7, accessed on 25 March 2025). The digital data were collected through Google Forms and stored in a password-protected electronic format. Ethical clearance for this study was granted by the Ethics Committee on Human Research Publication and Ethics, School of Medicine and Dentistry, KNUST, Kumasi, Ghana (Ref#: CHRPE/AP/345/22). The purposively selected locations, (i.e., KNUST, UG, and UCC), satisfied this study’s criteria of having health and non-health-related study programs and also having a student population of no less than 25,000. These criteria were set by the researchers to account for variability and improve the generalizability of this study’s outcomes.
Faculties and departments at each of the three study sites were classified and structured based on scientific discipline as being either medical (fields of study related to health, disease prevention, treatment, and healthcare systems) or non-medical and were selected upon balloting. Once a faculty or department was balloted, the principal investigator and trained volunteers visited the location and distributed the questionnaire through convenience sampling at lecture halls and campuses and asked participants to share the link to the questionnaire on electronic group-study platforms, such as WhatsApp, to reach as many students as possible.
2.3. Statistical Analysis
The raw data were transferred to Microsoft Excel version 16.78.3 (2019) where it was validated qualitatively, checked, and cleaned. All subsequent analyses were conducted using R (R core team, 2021) including the packages car [33], and mice [34] at the Department for Economics and Sociology of Sports, Faculty of Economics and Empirical Human Sciences, Saarland University, Germany. All items in the questionnaire were collected as categorical variables (Yes/No/Prefer not to say/Don’t know) apart from year of birth, which was afterwards converted to age (ordinal scale), the 5Cs antecedents, and vaccine attributes which have been measured based on a Likert-type scale from 1 (strongly disagree) to 7 (strongly agree). A seven-point scale was to increase granularity leading to the enhanced robustness and reliability of the measurement. The religion variable, which consisted of six categories, ethnicity variable, which had 13 categories, and study program were dichotomized and reduced to Christians/non-Christians, Akans/non-Akans, and medical/non-medical, respectively, for convenience. Furthermore, for vaccine experience, misinformation (conspiracy mentality), vaccine attributes, and vaccine passport, the answers were summed up and divided by the number of the items in each part resulting in a score ranging from 1 to 0. In the case of vaccine experience which had 8 items, for example, “No” answers were coded as having the value of 1, while “Yes” answers were 0. The sum was then divided by 8 and, therefore, a score closer to 0 indicates a higher number of vaccines received. In the case of misinformation (conspiracy mentality), which consisted of 4 items, values closer to 0 indicate a higher level of misinformation about vaccines.
A total of 4126 individuals participated in this study. This included university students at different levels of their studies, non-student university community members, and others. The data set was filtered to include only students, i.e., undergraduates and postgraduates, eventually resulting in a data set: n = 3486. As for missing data, multiple imputation (100 iterations) was performed for participants who answered “Prefer not to say” or “Don’t know”, to deal with item non-responses. Missing data accounted for 16.9% cases. In the regression analysis, two models were employed. The first model applied binary logistic regression to predict adulthood vaccination behavior (VB) using acceptance of the COVID-19 vaccine as a dependent variable. Here, the starting model, Basic Model, included only the sociodemographic variables (age, gender, religion, ethnicity, and field of study) as independent variables. The Extended Model to explain VB further included the 5Cs antecedents as additional predictors. As for reference categories, in gender it was “female”, “Akan” in ethnicity, “Christian” in religion, and “non-health students” in study program. The assumptions of multicollinearity were tested, and heteroscedasticity was assessed using the Goldfeld–Quandt t-test. There were no repeated observations in the data and the observations were random and without biases. Due to the multiple imputation technique, t-tests were employed to compare the Akaike Information Criterion (AIC) and Nagelkerke R-squared distributions between the Basic Model and the Extended Model. Additionally, to confirm the improved prediction by the Extended Model, two-way ANOVA was used to evaluate differences between the models. For all statistical tests, the level of significance was 5%.
The second model aimed to explain vaccine hesitancy (VH) deploying a multivariate regression method having each of the 5Cs as dependent variables, hence resulting in five different sub-models. This multivariate multiple regression model included the following independent variables: gender, religion, ethnicity, study program, vaccination experience, vaccine misinformation, information sources, vaccine attributes, and the respondent’s stances towards a vaccine passport. The analysis provides the following statistical information about factors influencing hesitancy: regression/beta coefficients indicative of the strength and direction of the association between the predictors and the outcome when holding other variables constant, odds ratios (OR) with 95% confidence intervals as measures of the impact of predictors on outcome, and p-values as appropriate. Additional information, including t-values showing if the regression/beta coefficients significantly differ from zero, pseudo R-squared values measuring the proportions of variance in the outcome explained by the predictors, and F-statistics assessing the overall significance of the models are also provided in the results and in analytical documentation (https://doi.org/10.17605/OSF.IO/AFUP7).
3. Results
Among the total participants, about 40% had not taken the COVID-19 vaccine (the reference vaccine for VB) out of which 71% were non-health subject students. The findings also support the notion that the 5Cs are crucial for assessing VB and VH, as four of the 5Cs, namely Confidence (OR = 1.56 [1.44–1.68), Constraints (OR = 0.83 [0.78–0.97]), Calculation (OR = 0.85 [0.78–0.87]) and Collective Responsibility (OR = 1.26 [1.16–1.38])—not Complacency—significantly predicted VB (p < 0.001). Notably, the 5Cs themselves seem to be significantly influenced by several factors. Vaccine attributes, for example, had a significant influence on all the 5Cs. This is also the case for misinformation (conspiracy mentality). In the next subsection, the sociodemographic details of the participants are first presented, followed by the descriptive statistics on participants’ information regarding vaccines and their psychological antecedents. Later on, results from the inferential statistics are demonstrated to attempt at explicating first the vaccine behavior (VB) and then vaccine hesitancy (VH) based on the 5Cs.
3.1. Descriptive Statistics
3.1.1. Sociodemographic Information
The sample included in the statistical analysis was n = 3486. The median age of the participants was 21 years, with an interquartile range (IQR) of 19–28 years. Most of the participants were males (55.8%), Christians (92.2%), and Akan (64.3). The study participants were predominantly from non-medical-related study disciplines (62.4%) compared to medical-related disciplines. The overall characteristics of this study is summarized in Figure 2.
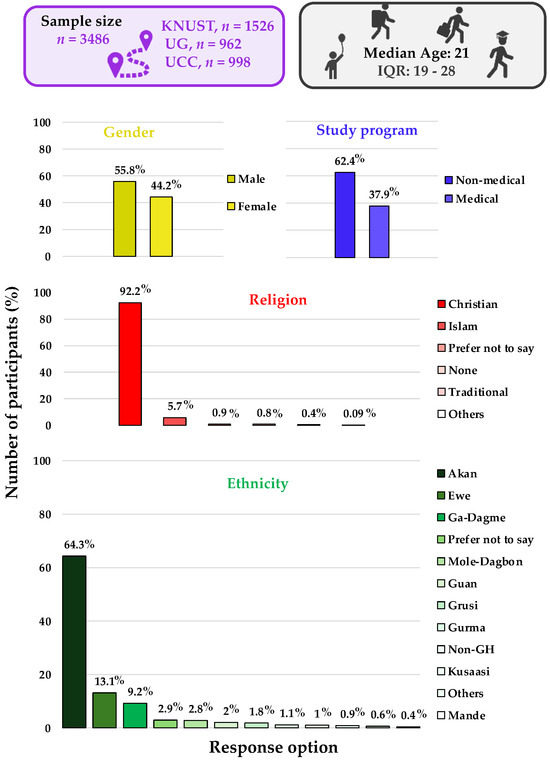
Figure 2.
Sociodemographic of participants.
3.1.2. Factors Influencing Vaccination
In this subsection, the results pertaining to mean values and standard deviations of participants’ vaccine experience, conspiracy mentality (misinformation), and vaccine attributes are presented. See Table 1.

Table 1.
Mean scores and standard deviations for factors influencing vaccination.
When participants were asked about vaccine information sources influencing their vaccination decision, official sources were the most utilized. The scientific literature on vaccines (articles, books, journals, etc.) and international agencies on health (e.g., the WHO, USAID, CDC UNICEF, etc.) were leading sources with 2545 and 2491 respondents, respectively. Unofficial sources, such as family and friends, were also preferred by about two-thirds of the respondents. Governmental agencies and traditional media outlets had a notable influence, while social media and influencers were less preferred, as represented in Figure 3a.
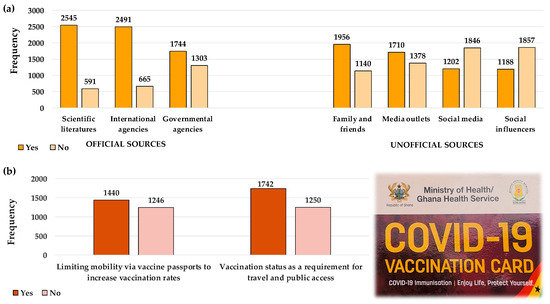
Figure 3.
The influence of vaccine information sources and vaccine passport on vaccination. (a) Distribution of preferred sources for vaccine information among respondents; (b) respondents’ stances on vaccine passports, alongside Ghana’s COVID-19 vaccination card (photograph by author).
As vaccine passports were mandatory in Ghana, this study assessed respondents’ opinions on vaccine passports and their influence on vaccination. The results showed that 1440 respondents supported them. Whilst a small majority supported the use of vaccination status as a criterion for accessing public places such as restaurants, tourist sites, and universities, a notable number of respondents were against this, as represented in Figure 3b.
3.1.3. Distribution and Mean Scores of the 5Cs
The results interpreted on a seven-point Likert-type scale from 1 (strongly disagree) to 7 (strongly agree) are presented as mean and standard deviations of the 5Cs construct in analytical documentation (https://doi.org/10.17605/OSF.IO/AFUP7, accessed on 25 March 2025) Table 2.

Table 2.
5Cs of the Ghanaian university students.
3.2. Inferential Statistics
3.2.1. Evaluation of Factors Influencing Vaccination Behavior
A logistic regression model was employed to investigate vaccination behavior (VB) (whether the participant has received the COVID-19 vaccine or not) of participants. Initially, a Basic Model based on sociodemographic predictors was calculated (https://doi.org/10.17605/OSF.IO/AFUP7). According to this Basic Model, all the sociodemographic predictors provided a significant correlation with VB (p < 0.001). The results revealed that religion (non-Christian), gender (male), ethnicity (non-Akans), and study program (non-medical student) significantly correlated with VB in a negative manner with OR values of 1.72 [1.31–2.26], 1.45 [1.26–1.67], 1.31 [1.12–1.52], and 0.548 [0.47–0.64], respectively. The male population exhibited higher odds of not being vaccinated compared to the female population. Moreover, the participants of non-medical programs showed lower odds of being vaccinated than students from courses related to health and medicine. This model explains only 5% of the variability in VB by the sociodemographic data, indicating that these factors could have a limited ability to predict vaccination behavior. Subsequently, when extending the Basic Model by adding the 5Cs, the significant influence of sociodemographic variables persists except for the influence of religion. Beyond sociodemographic determinants, the Extended Model highlights an influence of Confidence on vaccines, Constraints on vaccination, Calculation (i.e., risks–benefits assessment of vaccines), and sense of Collective Responsibility on an individual’s VB, as indicated in Figure 4.
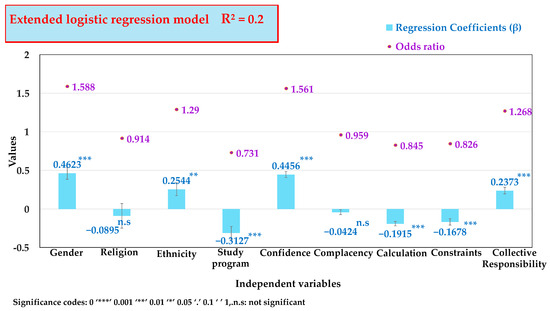
Figure 4.
Extended logistic regression model illustrating the influence of sociodemographic variables and 5Cs constructs on VB. This model explains the variance in VB by 20% by (R2 = 0.20).
Odd ratios of 1.56 [1.45–1.68] and 1.27 [1.16–1.38] for getting vaccinated have been estimated for Confidence and Collective Responsibility, respectively, making these two antecedents stand out positively and show that participants high in these antecedents are more likely to be vaccinated. Constraints (OR = 0.83 [0.78–0.87]) and Calculation (OR = 0.85 [0.78–0.92]) show a decreased likelihood of being vaccinated among the cohort high in these antecedents, and Complacency has no significant influence. Notably, the Extended Model including the 5Cs explains about 20% of the variance in VB. Comparison of the two models showed that adding the 5Cs significantly improves the explanation of variance in VB compared to the Basic Model.
3.2.2. Multivariate Regression Explicating the 5Cs Model for Vaccination Hesitancy
In order to evaluate factors influencing vaccination hesitancy, a multivariate regression model was employed to explore the impact of different factors on each of the 5Cs. This model was built to analyze the impact of sociodemographic (study program [medical] and religion [non-Christians]), vaccine experience, conspiracy mentality/misinformation, vaccine information sources, vaccine attributes, and vaccine passport/policies on the 5Cs psychological antecedents. The influences of the different factors on each of the 5Cs are presented in Figure 5.
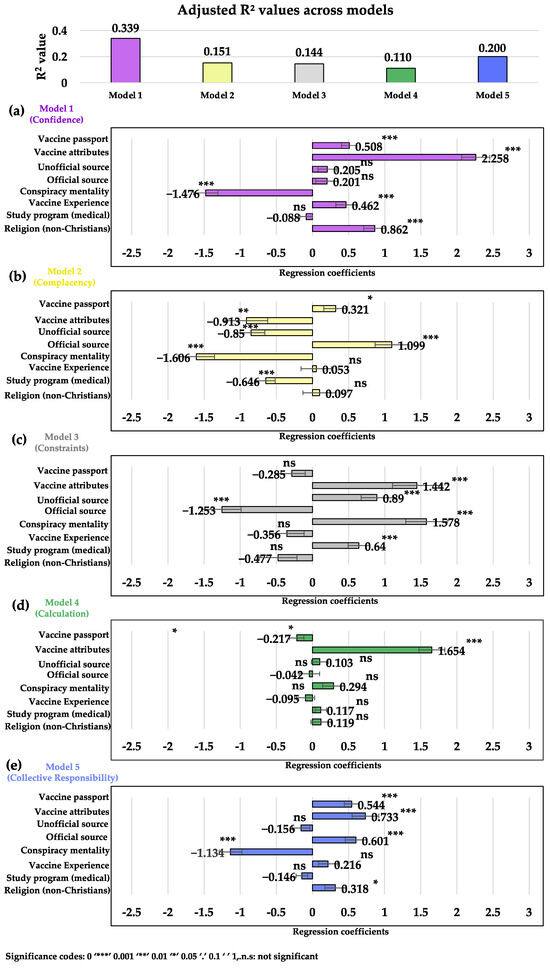
Figure 5.
Multivariate regression analysis predicts the influence of different factors on the 5Cs psychological antecedents. Sub-models (a–e) explicate the proportion of the explained variance in confidence, complacency, constraints, calculation and collective responsibility by the predictors. SE = error bar.
Amongst all the 5Cs, the variance among the participants in their Confidence (sub-model a) was best explained by the predictors, followed by Collective Responsibility with adjusted R-squared values of 0.339 and 0.200, respectively. Complacency and Constraints were explained to a similar level with adjusted R-squared values of 0.151 and 0.144, respectively, whilst variance in Calculation could be explained the least with an adjusted R-squared value of 0.110.
Conspiracy mentality and unofficial (mis-)information consistently showed a negative impact on the (positive) vaccination traits across each of the antecedents studied, while (reliable) official information sources and vaccine attributes had positive effects on the 5Cs variance. Conspiracy mentality, for instance, negatively impacts the Confidence (β = −1.476), Complacency (β = −1.607), and Collective Responsibility (β = −1.135) and positively influences the Constraints (β = 1.578), contributing to an overall significant VH among the educated population. Reliable official information sources and vaccine attributes had positive effects on the 5Cs, with vaccine attributes significantly contributing to the explaining the variance in Confidence (β = 2.258, p < 0.001), Calculation (β = 1.655, p < 0.001), and Collective Responsibility (β = 0.734, p < 0.001).
On one hand, unofficial sources of vaccine information had significantly increased the level of Constraints in individuals (β = 0.890, p < 0.001), while on the other hand, decreased the level of Complacency (β = −0.850, p < 0.001), thus, significantly promoting VH. Official information (β = 1.099, p < 0.001 for Complacency; β = 0.602, p < 0.001 for Collective Responsibility) and studying a medical-related subject (β = −0.646, p < 0.001 for Complacency) may directly, via increased knowledge or indirectly via the 5Cs, guard against the influence of unofficial vaccine information sources. Additionally, vaccine passports were reported as a significant influence on a positive prediction for Confidence (β = 0.508, p < 0.001) and Collective Responsibility (β = 0.545, p < 0.001).
4. Discussion
This study contributes to the existing body of research by examining factors influencing vaccination behavior as well as vaccination hesitancy among highly educated individuals in Ghana. It provides insights which can inform targeted healthcare strategies and policies to enhance vaccination uptake. This study confirms VH among university students, where 40% of the sample remained unvaccinated against COVID-19 with 71% of them who studied non-health disciplines. Confidence and Collective Responsibility increased vaccination likelihood, whilst Constraints and Calculation decreased it. The study also showed that gender (males), ethnicity (non-Akans), and study discipline (non-medical students) exhibited higher VH. Official vaccine information sources were the most trusted, whilst misinformation/conspiracy beliefs increased VH. Vaccine passports encouraged vaccination and the addition of the 5Cs model improved the prediction of VB, accentuating the role of trust, policy, and vaccine information sources in shaping VB.
Our findings among 3486 highly educated young persons in Ghana are in line with recent studies, for instance by Yeboah et al. (2020) [25,35], which reported VH among educated populations. Indeed, this study unveiled a substantial gap between high educational backgrounds and the actual practice of preventive measures against infectious diseases, including vaccinations. In addition, Arko AB, 2023 [36] also reported VH among similar young and highly educated cohorts with ‘supposed’ access to considerable information on health and health-related issues. Indeed, it is more likely that psychological antecedents of vaccination shape vaccination behavior and in doing so are often themselves influenced by other environmental factors, such as sociodemographic factors and (mis)information via official and unofficial vaccine information sources. These relationships not only expose a set of potential obstacles towards effective vaccination campaigns. They also provide impetus to deal with some of these issues openly and effectively, for instance by addressing possible concerns on the one side and building on existing strengths on the other.
The 5Cs assessment reveals contributive elements of VH among the participants (as shown in Table 2, Figure 4 and Figure 5). Notably, similar to a study conducted in the USA [37], Confidence—or lack thereof—is likely the most significant driver of VH, followed by Collective Responsibility. The analysis of statistical means showed that Complacency, Constraints, and Calculation exhibited patterns indicating either no significant effects or positive association with VH. However, further analysis showed significant influence on VB and thus, VH. The strong associations between VB, gender, ethnic groupings, and VH factors, for instance, point to the need for individually tailored and more targeted public health strategies [38,39]. On a gender-specific note, male-tailored education and vaccination campaigns can alleviate the gender disparity towards vaccination. In Ghana, ethnic variations, including geographical location, socioeconomic status, educational level, religious beliefs, and cultural or traditional systems between Akans and non-Akan groupings impact VH determinants. These factors are reported in many studies to be significantly associated with VB and thus VH [40,41,42], concurring with our studies where non-Akans are more likely to not get vaccinated compared to Akans. For instance, Akan communities, by virtue of their geographical locations in more developed regions, have more economic opportunities [43,44], hence increasing their ability to afford and access vaccines in contrast to non-Akans who are mostly in less economically developed regions and face financial and logistical constraints to vaccination.
Ethnic-centric vaccination campaign strategies and policies in light of the aforementioned ethnic differences are pivotal to addressing unique vaccination concerns. In addition, since ethnic groupings are mostly localized to specific regions in Ghana, the training and involvement of localized leadership including traditional leaders (i.e., kings, chiefs, and queen mothers), religious leaders, opinion leaders, or people of influence in public health promotions is imperative as reported in other studies [45,46]. Moreover, with the reported levels of Constraints and its significant influence on VB, policies to reduce vaccination constraints including lack of access, affordability, and availability should be top of the agenda in public health interventions.
On the upside, this study also shows that a higher sense of Collective Responsibility actually increases the likeliness to get vaccinated, similar to findings from a study conducted in Kenya [47], and thus social responsibility should be promoted and rewarded, also in public. At the same time, governments and public health institutions in charge of vaccinations should formulate policies and direct education that increases vaccine confidence via official, trustworthy communication. It would be easy, for instance, to introduce relevant seminars at the three Universities involved in this study and beyond, recruiting medical students to inform non-medical students about infectious diseases, vaccines, and vaccination. Similarly, non-governmental public influencers and political leaders themselves taking the vaccines could play a positive role.
This “role model” approach has already shown to be highly beneficial during the COVID-19 pandemic to boost interest in vaccination and may also safeguard against misinformation which has a distinctly negative influence on VB [48,49]. Whilst misinformation concerning vaccine safety, efficacy, or ingredients can promote doubt and fear, they are further exacerbated by conspiracy theories that suggest vaccines are part of a larger, nefarious agenda [50,51]. Furthermore, the influence of misinformation on 5Cs and thus VH, align with the findings of a study conducted in six Asian and African regions [35] where there was a significant positive correlation between conspiracy beliefs and vaccine hesitancy. Official sources, such as government health agencies, international organizations like the WHO, and healthcare professionals, generally enhance public confidence in vaccines [52]. These sources are often trusted due to their perceived expertise, authority, and commitment to public health and, together with accurate, transparent, and consistent communication from official sources may reassure the public about vaccine safety and efficacy, thus advancing confidence and reducing VH.
The findings presented in this study demonstrate vaccine hesitancy among university students in Ghana as a complex issue requiring integrated clinical and public health approaches. The significant role of psychological factors, such as low confidence, high complacency and constraints, and sociodemographic influences among male, non-Akan, non-medical students, and conspiracy mentality suggests the need for targeted interventions at several levels. Public health policymakers may benefit from adopting behavioral science methods, which include peer testimonies, transparent communication about vaccine safety, and perhaps small incentives, e.g., “thank you” certificates or vaccination pins, to foster trust and collective responsibility. Traditional vaccination campaigns could introduce focused vaccine education and practical tools such as an Email or SMS reminders to simplify vaccination access. Healthcare providers, including campus clinics, can empathetically discuss individual concerns, communicate early and clearly about vaccine efficacy, and possible side effects, and thus, positively shape vaccination attitudes. These coordinated efforts, informed by this study’s results, can meaningfully improve vaccine uptake and strengthen community readiness for future health challenges.
5. Limitations of This Study
Our study is limited in generalizability as it has only been carried out on young university students with no prior specific sample size calculations being made and participants sampled by convenience. However, a larger and more varied sample may in part minimize this limitation and improve external validity.
Like any other survey study, our research was partly limited by a social desirability bias [53]. This bias mostly affects the measurement of vaccination behavior and the 5Cs and was not directly addressed by adding a social desirability scale [54]. Nevertheless, the sample is characterized by a broad variety of ethnic and religious groups and study courses. These differences may well concur with different (sub-) cultural social norms and thus, this bias in individual answers may well be assumed to (partly) level out on the collective level.
Another shortcoming of our approach results from the operationalization of vaccination hesitancy only as the contrary of positive vaccination behavior. Besides vaccination hesitancy, vaccination behavior may well be influenced by other circumstances like legal or contractual requirements for certain occupations. Additionally, not being vaccinated may as well depend on other issues than mere hesitancy like chronic illnesses or lacking access to vaccines. Future research may account for this by not only measuring vaccination behavior but also addressing such factual reasons both for being vaccinated or not vaccinated.
While these limitations may be overcome in future research on VB/VH, we trust that our study, nevertheless, provides valuable basic insights into the relevant determinants of VB/VH.
6. Conclusions
Our study on highly educated young respondents in Ghana has confirmed varying levels of VH in this section of society and shown that both sociodemographic factors and the 5Cs significantly influence VB. These findings also provide renewed impetus for addressing some of the influences, concerns, and mechanisms that determine individual’s VB and possibly lead to VH. Males, non-Akans, and those enrolled in non-health study programs were less likely to be vaccinated and thus may require tailor-made, community-specific information campaigns to overcome their inherent VH. Greater Confidence and a sense of Collective Responsibility increase the likelihood of vaccination. Additionally, open and transparent discussions about diseases, available vaccines, and the benefits of vaccination for individuals and society are essential for overcoming misinformation. This may also remediate higher Constraints and (negative outcomes of) Calculation, which lead to a decrease in the likelihood of vaccination. Notably, context-specific health interventions augmenting policymakers and healthcare professionals in advancing vaccine up-take and achieving community herd immunity against vaccine-preventable diseases should therefore be promoted. Together, these measures are important to enhance the preparedness for potential future epidemics or pandemics, especially in countries of the Global South.
Author Contributions
Conceptualization, P.Y., A.R. and A.Y.A.; methodology, P.Y. and T.O.G.; validation, N.O., M.O.B., A.B.P. and C.J.; formal analysis, P.S. and W.P.; investigation, P.Y., T.O.G. and N.O.; data curation, P.Y., P.A., P.S. and W.P.; writing—original draft preparation, P.Y., C.J.; writing—review and editing, P.Y., A.Y.A., T.O.G., P.A., N.O., A.R., M.J.N. and M.O.B.; visualization, P.Y.; supervision, A.B.P. and C.J.; project administration, P.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical clearance for this study was granted by the Ethics Committee on Human Research Publication and Ethics, School of Medicine and Dentistry, KNUST, Kumasi, Ghana (Ref#: CHRPE/AP/345/22).
Informed Consent Statement
Informed consent was obtained from all respondents involved in this study.
Data Availability Statement
Data are available upon request.
Acknowledgments
The authors would like to acknowledge Isaac Hene Tabiri (University of Cape Coast, Ghana), Clement Okoh Acheampong (University of North Carolina, Chapel Hill, USA), and Christopher Wiesen (University of North Carolina, Chapel Hill, USA) for their immense contribution and support in making this research a success.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- COVID-19 Cases|WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/cases (accessed on 2 September 2024).
- Pitlik, S.D. COVID-19 Compared to Other Pandemic Diseases. Rambam Maimonides Med. J. 2020, 11, e0027. [Google Scholar] [CrossRef] [PubMed]
- Boakye, E.A.; Hongjiang, Z.; Ahia, B.N.K.; Damoah, M.A. COVID-19 Pandemic: Exploring the Fiscal and Monetary Policies for Mitigating the Socio-Economic Impact on Ghana’s Economy. In New Innovations in Economics, Business and Management Vol. 9; Erokhin, V., Ed.; Book Publisher International (A Part of SCIENCEDOMAIN International): London, UK, 2022; pp. 22–39. ISBN 978-93-5547-719-4. [Google Scholar]
- Barrett, R.; Zuckerman, M.; Dudgeon, M.R.; Armelagos, G.J. Emerging Infections: Three Epidemiological Transitions from Prehistory to the Present; Oxford University Press: Oxford, UK, 2024; ISBN 978-0-19-265484-7. [Google Scholar]
- Awedoba, A.K.; Kamski, B.; Mehler, A.; Sebudubudu, D. Africa Yearbook Volume 16: Politics, Economy and Society South of the Sahara in 2019. In Africa Yearbook Volume 16; Brill: Leiden, The Netherlands, 2020; ISBN 978-90-04-43001-3. [Google Scholar]
- Journell, W. Post-Pandemic Social Studies: How COVID-19 Has Changed the World and How We Teach; Teachers College Press: New York, NY, USA, 2021; ISBN 978-0-8077-8068-8. [Google Scholar]
- Fieselmann, J.; Annac, K.; Erdsiek, F.; Yilmaz-Aslan, Y.; Brzoska, P. What Are the Reasons for Refusing a COVID-19 Vaccine? A Qualitative Analysis of Social Media in Germany. BMC Public Health 2022, 22, 846. [Google Scholar] [CrossRef]
- Heinze, A.-S.; Weisskircher, M. How Political Parties Respond to Pariah Street Protest: The Case of Anti-Corona Mobilisation in Germany. Ger. Politics 2022, 32, 563–584. [Google Scholar]
- Klich-Kluczewska, B.; von Puttkamer, J.; Rebitschek, I. (Eds.) Biopolitics in Central and Eastern Europe in the 20th Century: Fearing for the Nation; Routledge: London, UK, 2022; ISBN 978-1-003-16108-0. [Google Scholar]
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Bedford, H.; Attwell, K.; Danchin, M.; Marshall, H.; Corben, P.; Leask, J. Vaccine Hesitancy, Refusal and Access Barriers: The Need for Clarity in Terminology. Vaccine 2018, 36, 6556–6558. [Google Scholar] [CrossRef]
- COVID-19 Vaccines. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 2 September 2024).
- Sinuraya, R.K.; Nuwarda, R.F.; Postma, M.J.; Suwantika, A.A. Vaccine Hesitancy and Equity: Lessons Learned from the Past and How They Affect the COVID-19 Countermeasure in Indonesia. Glob. Health 2024, 20, 11. [Google Scholar] [CrossRef]
- Nuwarda, R.F.; Ramzan, I.; Weekes, L.; Kayser, V. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines 2022, 10, 1595. [Google Scholar] [CrossRef]
- Hamson, E.; Forbes, C.; Wittkopf, P.; Pandey, A.; Mendes, D.; Kowalik, J.; Czudek, C.; Mugwagwa, T. Impact of Pandemics and Disruptions to Vaccination on Infectious Diseases Epidemiology Past and Present. Hum. Vaccines Immunother. 2023, 19, 2219577. [Google Scholar] [CrossRef]
- Snyder, M.R.; McGinty, M.D.; Shearer, M.P.; Meyer, D.; Hurtado, C.; Nuzzo, J.B. Outbreaks of Hepatitis A in US Communities, 2017–2018: Firsthand Experiences and Operational Lessons From Public Health Responses. Am. J. Public Health 2019, 109, S297–S302. [Google Scholar] [CrossRef]
- Abdin, A.Y.; De Pretis, F.; Landes, J. Fast Methods for Drug Approval: Research Perspectives for Pandemic Preparedness. Int. J. Environ. Res. Public Health 2023, 20, 2404. [Google Scholar] [CrossRef]
- Buonomo, B.; Della Marca, R. A Behavioural Vaccination Model with Application to Meningitis Spread in Nigeria. Appl. Math. Model. 2024, 125, 334–350. [Google Scholar] [CrossRef]
- Immunization Coverage. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 2 September 2024).
- Atinga, R.A.; Koduah, A.; Abiiro, G.A. Understanding the Policy Dynamics of COVID-19 Vaccination in Ghana through the Lens of a Policy Analytical Framework. Health Res. Policy Syst. 2022, 20, 94. [Google Scholar] [CrossRef] [PubMed]
- Nonvignon, J.; Owusu, R.; Asare, B.; Adjagba, A.; Aun, Y.W.; Yeung, K.H.T.; Azeez, J.N.K.; Gyansa-Lutterodt, M.; Gulbi, G.; Amponsa-Achiano, K.; et al. Estimating the Cost of COVID-19 Vaccine Deployment and Introduction in Ghana Using the CVIC Tool. Vaccine 2022, 40, 1879–1887. [Google Scholar] [CrossRef]
- COVID-19 Data|WHO COVID-19 Dashboard. Available online: https://data.who.int/dashboards/covid19/data (accessed on 11 November 2024).
- Geoghegan, S.; O’Callaghan, K.P.; Offit, P.A. Vaccine Safety: Myths and Misinformation. Front. Microbiol. 2020, 11, 372. [Google Scholar] [CrossRef]
- Peters, M.D.J. Addressing Vaccine Hesitancy and Resistance for COVID-19 Vaccines. Int. J. Nurs. Stud. 2022, 131, 104241. [Google Scholar] [CrossRef] [PubMed]
- Yeboah, P.; Daliri, D.B.; Abdin, A.Y.; Appiah-Brempong, E.; Pitsch, W.; Panyin, A.B.; Adusei, E.B.A.; Razouk, A.; Nasim, M.J.; Jacob, C. Knowledge into the Practice against COVID-19: A Cross-Sectional Study from Ghana. Int. J. Environ. Res. Public Health 2021, 18, 12902. [Google Scholar] [CrossRef]
- Poland, C.M.; Jacobson, R.M.; Opel, D.J.; Marcuse, E.K.; Poland, G.A. Political, Ethical, Social, and Psychological Aspects of Vaccinology. In Vaccinology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015; pp. 335–357. ISBN 978-1-118-63803-3. [Google Scholar]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond Confidence: Development of a Measure Assessing the 5C Psychological Antecedents of Vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Daley, M.F.; Narwaney, K.J.; Shoup, J.A.; Wagner, N.M.; Glanz, J.M. Addressing Parents’ Vaccine Concerns: A Randomized Trial of a Social Media Intervention. Am. J. Prev. Med. 2018, 55, 44–54. [Google Scholar] [CrossRef]
- Askelson, N.M.; Campo, S.; Lowe, J.B.; Smith, S.; Dennis, L.K.; Andsager, J. Using the Theory of Planned Behavior to Predict Mothers’ Intentions to Vaccinate Their Daughters Against HPV. J. Sch. Nurs. 2010, 26, 194–202. [Google Scholar] [CrossRef]
- Omer, S.B.; Orenstein, W.A.; Koplan, J.P. Go Big and Go Fast—Vaccine Refusal and Disease Eradication. N. Engl. J. Med. 2013, 368, 1374–1376. [Google Scholar] [CrossRef] [PubMed]
- Petrocelli, J.V. Factor Validation of the Consideration of Future Consequences Scale: Evidence for a Short Version. J. Soc. Psychol. 2003, 143, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression; SAGE Publications: Los Angeles, CA, USA, 2018; ISBN 978-1-5443-3648-0. [Google Scholar]
- Buuren, S.V.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Salman, M.; Mallhi, T.H.; Tanveer, N.; Shehzadi, N.; Khan, H.M.; Mustafa, Z.U.; Khan, T.M.; Hussain, K.; Mohamed, M.S.; Maqbool, F.; et al. Evaluation of Conspiracy Beliefs, Vaccine Hesitancy, and Willingness to Pay towards COVID-19 Vaccines in Six Countries from Asian and African Regions: A Large Multinational Analysis. Vaccines 2022, 10, 1866. [Google Scholar] [CrossRef] [PubMed]
- Arko, A.B. COVID-19 Vaccine Hesitancy and Acceptance among University Students in Ghana. ADRRI J. Arts Soc. Sci. 2023, 20, 52–74. [Google Scholar]
- Rancher, C.; Moreland, A.D.; Smith, D.W.; Cornelison, V.; Schmidt, M.G.; Boyle, J.; Dayton, J.; Kilpatrick, D.G. Using the 5C Model to Understand COVID-19 Vaccine Hesitancy across a National and South Carolina Sample. J. Psychiatr. Res. 2023, 160, 180–186. [Google Scholar] [CrossRef]
- Willis, D.E.; Andersen, J.A.; Bryant-Moore, K.; Selig, J.P.; Long, C.R.; Felix, H.C.; Curran, G.M.; McElfish, P.A. COVID-19 Vaccine Hesitancy: Race/Ethnicity, Trust, and Fear. Clin. Transl. Sci. 2021, 14, 2200–2207. [Google Scholar] [CrossRef]
- Howard, M.C. Gender and Vaccination: Understanding the Multifaceted Role of a Multidimensional Conceptualization of Vaccine Hesitancy. Psychol. Health Med. 2024, 29, 1055–1062. [Google Scholar] [CrossRef]
- Saaka, S.A.; Mohammed, K.; Pienaah, C.K.A.; Luginaah, I. Child Malaria Vaccine Uptake in Ghana: Factors Influencing Parents’ Willingness to Allow Vaccination of Their Children under Five (5) Years. PLoS ONE 2024, 19, e0296934. [Google Scholar] [CrossRef]
- Kibongani Volet, A.; Scavone, C.; Catalán-Matamoros, D.; Capuano, A. Vaccine Hesitancy Among Religious Groups: Reasons Underlying This Phenomenon and Communication Strategies to Rebuild Trust. Front. Public Health 2022, 10, 824560. [Google Scholar] [CrossRef]
- Asuman, D.; Ackah, C.G.; Enemark, U. Inequalities in Child Immunization Coverage in Ghana: Evidence from a Decomposition Analysis. Health Econ. Rev. 2018, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Kuuyi, A.; Kogi, R. Factors Contributing to Immunization Coverage among Children Less than 5 Years in Nadowli-Kaleo District of Upper West Region, Ghana. PLoS Glob. Public Health 2024, 4, e0002881. [Google Scholar] [CrossRef]
- Asante, R.; Gyimah-Boadi, E. Ethnic Structure, Inequality and Governance of the Public Sector in Ghana; United Nations Research Institute for Social Development: Geneva, Switzerland, 2004. [Google Scholar]
- Nicola, M.; Sohrabi, C.; Mathew, G.; Kerwan, A.; Al-Jabir, A.; Griffin, M.; Agha, M.; Agha, R. Health Policy and Leadership Models during the COVID-19 Pandemic: A Review. Int. J. Surg. 2020, 81, 122–129. [Google Scholar] [CrossRef]
- Nwachukwu, G.; Rihan, A.; Nwachukwu, E.; Uduma, N.; Elliott, K.S.; Tiruneh, Y.M. Understanding COVID-19 Vaccine Hesitancy in the United States: A Systematic Review. Vaccines 2024, 12, 747. [Google Scholar] [CrossRef]
- Mudhune, V.; Ondeng’e, K.; Otieno, F.; Otieno, D.B.; Bulinda, C.M.; Okpe, I.; Nabia, S.; Bar-Zeev, N.; Otieno, O.; Wonodi, C. Determinants of COVID-19 Vaccine Acceptability among Healthcare Workers in Kenya—A Mixed Methods Analysis. Vaccines 2023, 11, 1290. [Google Scholar] [CrossRef] [PubMed]
- Dureab, F.; Al-Awlaqi, S.; Jahn, A. COVID-19 in Yemen: Preparedness Measures in a Fragile State. Lancet Public Health 2020, 5, e311. [Google Scholar] [CrossRef] [PubMed]
- Mercola, J.; Cummins, R. The Truth About COVID-19: Exposing The Great Reset, Lockdowns, Vaccine Passports, and the New Normal; Chelsea Green Publishing: Chelsea, VT, USA, 2021; ISBN 978-1-64502-088-2. [Google Scholar]
- Fuchs, C. Communicating COVID-19: Everyday Life, Digital Capitalism, and Conspiracy Theories in Pandemic Times; Emerald Group Publishing: Leeds, UK, 2021; ISBN 978-1-80117-720-7. [Google Scholar]
- Sundstrom, B.; Cartmell, K.B.; White, A.A.; Well, H.; Pierce, J.Y.; Brandt, H.M. Correcting HPV Vaccination Misinformation Online: Evaluating the HPV Vaccination NOW Social Media Campaign. Vaccines 2021, 9, 352. [Google Scholar] [CrossRef]
- Cao, A.; Ueta, M.; Uchibori, M.; Murakami, M.; Kunishima, H.; Santosh Kumar, R.; Prommas, P.; Tomoi, H.; Gilmour, S.; Sakamoto, H.; et al. Trust in Governments, Public Health Institutions, and Other Information Sources as Determinants of COVID-19 Vaccine Uptake Behavior in Japan. Vaccine 2024, 42, 3684–3692. [Google Scholar] [CrossRef]
- Edwards, A.L. The Social Desirability Variable in Personality Assessment and Research; Dryden Press: Ft Worth, TX, USA, 1957; pp. viii, 108. [Google Scholar]
- Stöber, J. The Social Desirability Scale-17 (SDS-17). Eur. J. Psychol. Assess. 2001, 17, 222–232. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).