The Harmful Impact of COVID-19 on Adiposity Markers and Cognitive Development in Maya Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Somatometric and Clinical Evaluation
2.3. Cognitive Evaluation
2.4. Dietetic Evaluation
2.5. Statistical Analysis
3. Results
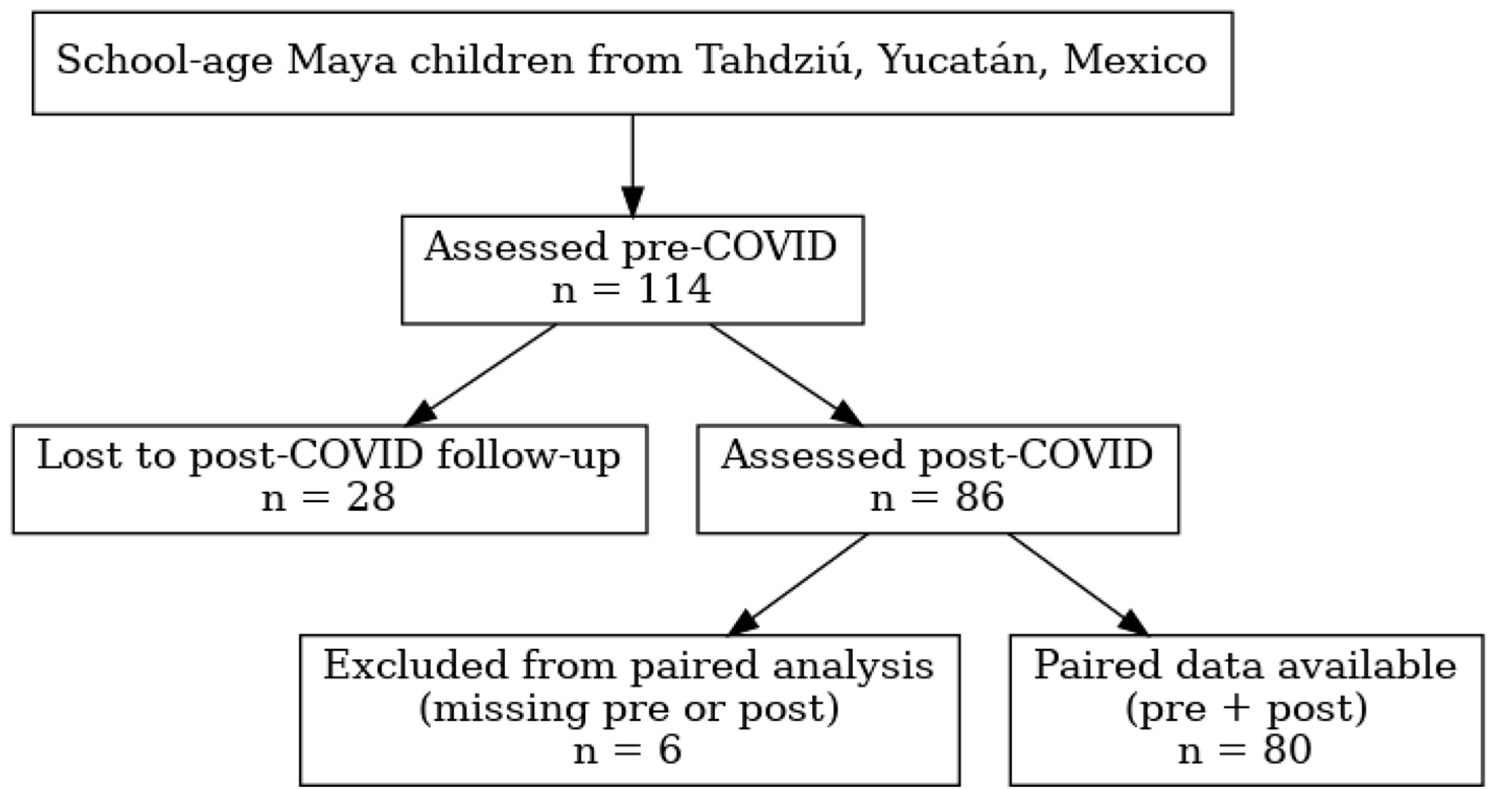
3.1. Follow-Up Evaluation
3.2. Comparisons Between Boys and Girls
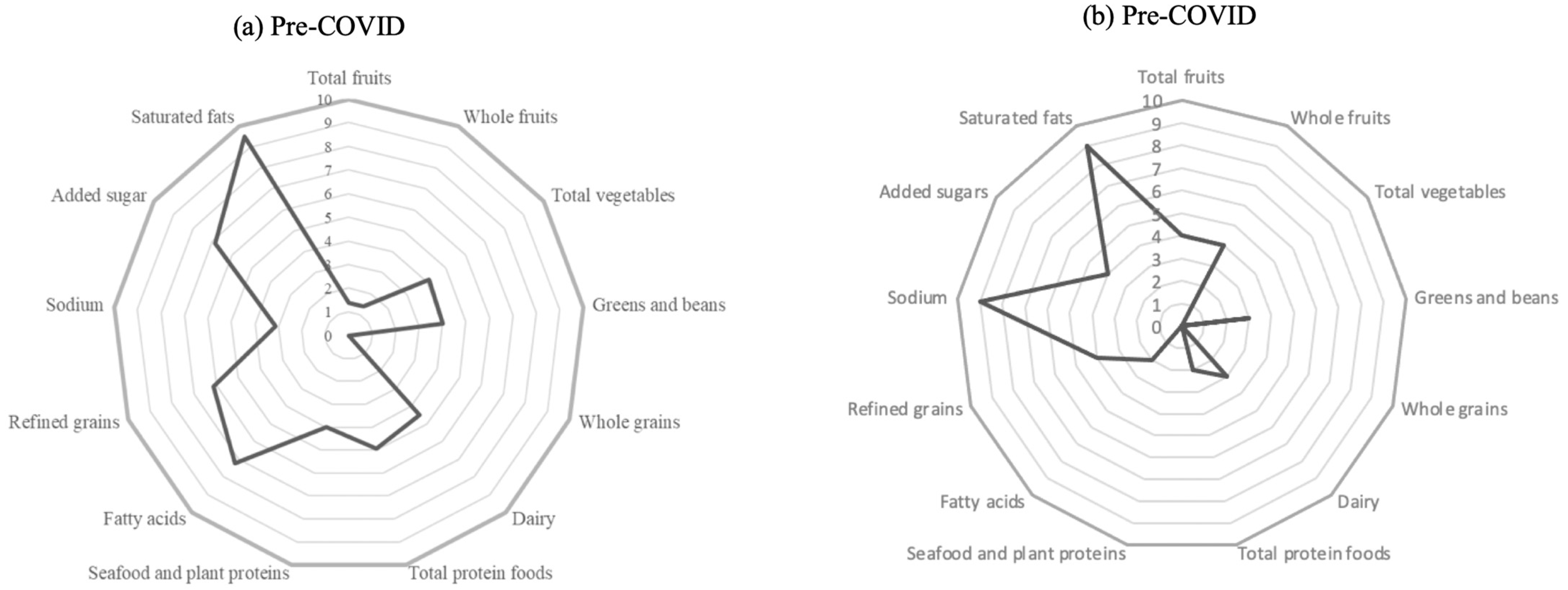
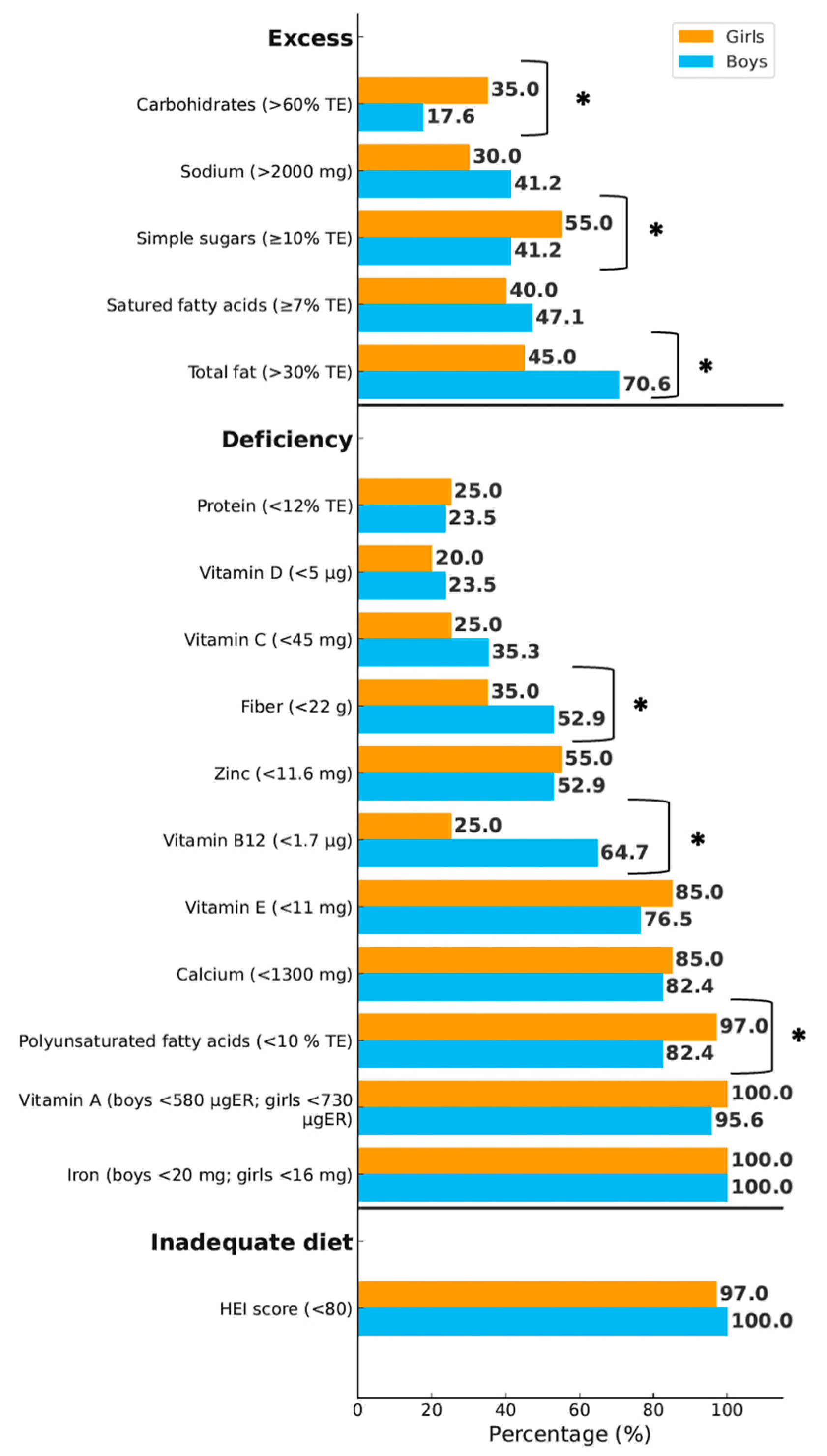
3.3. Dietetic Evaluation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HRAEPY | Hospital Regional de Alta Especialidad de la Península de Yucatán |
| HAZ | Z-Score of Height for age |
| BMIZ | Z-Score of Body Mass Index for age |
| FMI | Fat Mass Index |
| WHtR | Waist to Height Ratio |
| LGD | Linear Growth Deficiency |
| BDM | Double Burden Malnutrition |
| HFD | Human Figure Drawing |
| RDAs | Recommended Dietary Advances |
| HEI | Healthy Eating Index |
| USDA | Food and Nutrition Service of the U.S. Department of Agriculture |
| SD | Standard Deviation |
| IQ | Intelligence Quotient |
References
- Robles-Zavala, E. Los múltiples rostros de la pobreza en una comunidad maya de la Península de Yucatán. Estud. Soc. 2010, 18, 100–133. Available online: https://core.ac.uk/reader/25649660 (accessed on 1 July 2023).
- Instituto Nacional de Estadística y Geografía (INEGI). Información Por Entidad. Yucatán. Población. Published 2010. Available online: https://cuentame.inegi.org.mx/monografias/informacion/yuc/poblacion/diversidad.aspx?tema%3Dme%26e%3D31 (accessed on 27 February 2023).
- Consejo Nacional de Evaluación de la Política de Desarrollo Social (CONEVAL). Informe de Pobreza y Evaluación. Yucatán. 2020. Available online: https://www.coneval.org.mx/coordinacion/entidades/Documents/Informes_de_pobreza_y_evaluacion_2020_Documentos/Informe_Yucatan_2020.pdf (accessed on 1 July 2023).
- May-Kim, S.; Peña-Espinoza, B.I.; Menjivar, M. Malnutrition in Maya children: High prevalence of linear growth deficiency. Am. J. Biol. Anthropol. 2022, 177, 620–629. [Google Scholar] [CrossRef]
- Grey, K.; Gonzales, G.B.; Abera, M.; Lelijveld, N.; Thompson, D.; Berhane, M.; Abdissa, A.; Girma, T.; Kerac, M. Severe malnutrition or famine exposure in childhood and cardiometabolic non-communicable disease later in life: A systematic review. BMJ Glob. Health 2021, 6, e003161. [Google Scholar] [CrossRef] [PubMed]
- Uday, S.; Manaseki-Holland, S.; Bowie, J.; Mughal, M.Z.; Crowe, F.; Högler, W. The effect of vitamin D supplementation and nutritional intake on skeletal maturity and bone health in socio-economically deprived children. Eur. J. Nutr. 2021, 60, 3343–3353. [Google Scholar] [CrossRef]
- Alam, M.A.; Richard, S.A.; Fahim, S.M.; Mahfuz, M.; Nahar, B.; Das, S.; Shrestha, B.; Koshy, B.; Mduma, E.; Seidman, J.C.; et al. Impact of early-onset persistent stunting on cognitive development at 5 years of age: Results from a multi-country cohort study. PLoS ONE 2020, 15, e0227839. [Google Scholar] [CrossRef]
- Alpízar, M.; Frydman, T.D.; de Reséndiz-Rojas, J.; Trejo-Rangel, M.A.; De Aldecoa-Castillo, J.M. Fat Mass Index (FMI) as a Trustworthy Overweight and Obesity Marker in Mexican Pediatric Population. Children 2020, 7, 19. [Google Scholar] [CrossRef]
- Rundle, A.G.; Factor-Litvak, P.; Suglia, S.F.; Susser, E.S.; Kezios, K.L.; Lovasi, G.S.; Cirillo, P.M.; Cohn, B.A.; Link, B.G. Tracking of Obesity in Childhood into Adulthood: Effects on Body Mass Index and Fat Mass Index at Age 50. Child. Obes. 2020, 16, 226–233. [Google Scholar] [CrossRef]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Wrottesley, S.V.; Mates, E.; Brennan, E.; Bijalwan, V.; Menezes, R.; Ray, S.; Ali, Z.; Yarparvar, A.; Sharma, D.; Lelijveld, N. Nutritional status of school-age children and adolescents in low- and middle-income countries across seven global regions: A synthesis of scoping reviews. Public Health Nutr. 2023, 26, 63–95. [Google Scholar] [CrossRef]
- Azcorra, H.; Vázquez-Vázquez, A.; Baqueiro, J.; Salazar-Rendón, J.C. Crecimiento y estado nutricional de escolares de tres comunidades de Yucatán, México. Arch. Latinoam. Nutr. 2016, 66, 135–141. [Google Scholar]
- Vazquez-Gomez, A.; Ávila-Escalante, M.L.; Azcorra, H.; Varela-Silva, M.I.; Dickinson, F. Body proportionality and adiposity are not related in 6- to 8-year-old Yucatec Maya children. Am. J. Hum. Biol. 2019, 31, e23254. [Google Scholar] [CrossRef]
- Uuh Narvaez, J.J.; Segura Campos, M.R. Foods from Mayan Communities of Yucatán as Nutritional Alternative for Diabetes Prevention. J. Med. Food 2020, 23, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.; Tolar-Peterson, T.; Reynolds, A.; Wall, C.; Reeder, N.; Rico Mendez, G. The Effects of Nutritional Interventions on the Cognitive Development of Preschool-Age Children: A Systematic Review. Nutrients 2022, 14, 532. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.P.; Sathiyamoorthy, T.; Giruparajah, M.; Toulany, A.; Hamilton, J.K. Weighing in on COVID-19: The impact of the pandemic on children and adolescents with obesity participating in a weight management program. Pediatr. Obes. 2022, 17, e12948. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Luo, C.; Feng, X.; Qi, W.; Qu, S.; Zhou, Y.; Sun, L.; Wu, H. Changes in obesity and lifestyle behaviours during the COVID-19 pandemic in Chinese adolescents: A longitudinal analysis from 2019 to 2020. Pediatr. Obes. 2022, 17, 11. [Google Scholar] [CrossRef]
- Bussières, E.-L.; Malboeuf-Hurtubise, C.; Meilleur, A.; Mastine, T.; Hérault, E.; Chadi, N.; Montreuil, M.; Généreux, M.; Chantal Camden and PRISME-COVID Team. Consequences of the COVID-19 Pandemic on Children’s Mental Health: A Meta-Analysis. Front. Psychiatry 2021, 12, 10. [Google Scholar] [CrossRef]
- Instituto Nacional de Salud Pública (INSP). Prevención de Mala Nutrición en Niñas y Niños en México Ante la Pandemia de COVID-19. Published online 2020:10. Available online: https://www.insp.mx/micrositio-covid-19/prevencion-de-mala-nutricion-en-ninas-y-ninos-en-mexico-ante-la-pandemia-de-covid-19-recomendaciones-dirigidas-a-tomadores-de-decisiones (accessed on 1 July 2023).
- Ironman, T.; InnerScan DUAL. Intruction Manual Model BC-1500 Plus. Published online 2017:1. Available online: https://www.tanitachile.cl/bc-1500-plus-ironman/ (accessed on 1 July 2023).
- Muntner, P.; Shimbo, D.; Carey, R.M.; Charieston, J.B.; Gaillard, T.; Misra, S.; Myers, M.G.; Ogedegbe, G.; Schwaartz, J.E.; Townsend, R.R.; et al. Measurement of Blood Pressure in Humans: A Scientific Statement from the American Heart Association. Hypertension 2019, 73, 35–66. [Google Scholar] [CrossRef]
- Marfell-Jones, M.; Olds, T.; Stewart, A.; Carter, L. International Standards for Anthropometric Assessment; International Society for the Advancenment of Kinanthropometry (ISAK): Glasgow, UK, 2016. [Google Scholar]
- Ramírez, E.; Valencia, M.E.; Bourges, H.; Espinosa, T.; Moya-Camarena, S.Y.; Salazar, G.; Alemán-Mateo, H. Body composition prediction equations based on deuterium oxide dilution method in Mexican children: A national study. Eur. J. Clin. Nutr. 2012, 66, 1099–1103. [Google Scholar] [CrossRef]
- de Onis, M. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Frisancho, R. Anthropometric Standards: An Interactive Nutritional Reference of Body Size and Body Composition for Children and Adults; University of Michigan Press: Ann Arbor, MI, USA, 2008. [Google Scholar]
- de Ferranti, S.D.; Gauvreau, K.; Ludwig, D.S.; Neufeld, E.J.; Newburger, J.W.; Rifai, N. Prevalence of the Metabolic Syndrome in American Adolescents. Circulation 2004, 110, 2494–2497. [Google Scholar] [CrossRef]
- Münsterberg Koppitz, E. El Dibujo de La Figura Humana En Los Niños, 12th ed.; Gabriel Forqueda, A. El dibujo de la figura humana en niños Koppitz. El Dibujo De La Figura Humana En Los Niños, 2006. Available online: https://www.academia.edu/57035669/El_dibujo_de_la_figura_humana_en_niños_Koppitz (accessed on 11 October 2023).
- Bourges, H.; Casanueva, E.; Rosado, J.L. Recomendaciones de Ingestión de Nutrimentos Para La Población Mexicana. In Cuadernos de nutrición; Editorial Médica Panamericana: Madrid, Spain, 2010. [Google Scholar]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, Y. Campo yucateco, el más afectado por hucarán “Delta” . El Universal 2020. Available online: https://www.eluniversal.com.mx/estados/huracan-delta-campo-yucateco-el-mas-afectado/ (accessed on 12 October 2021).
- Solomons, N.W.; Mazariegos, M.; Vettorazzi, C.; Valdez, C.; Grazioso, C.; Romero-Abal, M.E.; Caballero, B. Growth Faltering, Protein Metabolism and Immunostimulation: New Speculations on the Nature of the Relationship with Notes from Observations and Analyses in Guatemala; International Atomic Energy Agency: Vienna, Austria, 1993. [Google Scholar]
- Ramírez-Luzuriaga, M.J.; Kobes, S.; Sinha, M.; Knowler, W.C.; Hanson, R.L. Increased Adiposity and Low Height-for-Age in Early Childhood Are Associated With Later Metabolic Risks in American Indian Children and Adolescents. J. Nutr. 2022, 152, 1872–1885. [Google Scholar] [CrossRef] [PubMed]
- Zachurzok, A.; Wójcik, M.; Gawlik, A.; Starzyk, J.B.; Mazur, A. An Attempt to Assess the Impact of Pandemic Restrictions on the Lifestyle, Diet, and Body Mass Index of Children with Endocrine Diseases—Preliminary Results. Nutrients 2021, 14, 156. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Osiac, L.; Egaña Rojas, D.; Gálvez Espinoza, P.; Navarro-Rosenblatt, D.; Araya B, M.; Carroza, M.B.; Baginsky G, C. Evitemos la inseguridad alimentaria en tiempos de COVID-19 en Chile. Rev. Chil. Nutr. 2020, 47, 347–349. [Google Scholar] [CrossRef]
- Barrios, P.L.; Garcia-Feregrino, R.; Rivera, J.A.; Albino, B.-V.; Leticia, H.-C.; Isabel, R.; Ines, G.-C.; Usha, R.; Daniel J, H. Height Trajectory During Early Childhood Is Inversely Associated with Fat Mass in Later Childhood in Mexican Boys. J. Nutr. 2019, 149, 2011–2019. [Google Scholar] [CrossRef]
- Long, K.Z.; Beckmann, J.; Lang, C.; Seelig, H.; Nqweniso, S.; Probst-Hensch, N.; Müller, I.; Pühse, U.; Steinmann, P.; du Randt, R.; et al. Associations of Growth Impairment and Body Composition among South African School-Aged Children Enrolled in the KaziAfya Project. Nutrients 2021, 13, 2735. [Google Scholar] [CrossRef]
- Ramirez-Zea, M.; Kroker-Lobos, M.F.; Close-Fernandez, R.; Kanter, R. The double burden of malnutrition in indigenous and nonindigenous Guatemalan populations. Am. J. Clin. Nutr. 2014, 100, 1644S–1651S. [Google Scholar] [CrossRef]
- Kroker-Lobos, M.F.; Pedroza-Tobías, A.; Pedraza, L.S.; Rivera, J.A. The double burden of undernutrition and excess body weight in Mexico. Am. J. Clin. Nutr. 2014, 100, 1652S–1658S. [Google Scholar] [CrossRef]
- Hulst, J.M.; Huysentruyt, K.; Gerasimidis, K.; Shamir, R.; Koletzko, B.; Chourdakis, M.; Fewtrell, M.; Joosten, K.F. A Practical Approach to Identifying Pediatric Disease-Associated Undernutrition. J. Pediatr. Gastroenterol. Nutr. 2022, 74, 693–705. [Google Scholar] [CrossRef]
- Nauli, A.M.; Matin, S. Why Do Men Accumulate Abdominal Visceral Fat? Front. Physiol. 2019, 10, 10. [Google Scholar] [CrossRef]
- Yılmazbaş, P.; Haşlak, G.V.; Dursun, H. The relationship between body fat ratio and blood pressure in school-age children. J. Hum. Hypertens. 2020, 34, 826–832. [Google Scholar] [CrossRef]
- Baglio, G.; Blasi, V.; Intra, F.S.; Castelli, I.; Massaro, D.; Baglio, F.; Valle, A.; Zanette, M.; Marchetti, A. Social Competence in Children with Borderline Intellectual Functioning: Delayed Development of Theory of Mind Across All Complexity Levels. Front. Psychol. 2016, 7, 1604. [Google Scholar] [CrossRef]
- Santegoeds, E.; van der Schoot, E.; Roording-Ragetlie, S.; Klip, H.; Rommelse, N. Neurocognitive functioning of children with mild to borderline intellectual disabilities and psychiatric disorders: Profile characteristics and predictors of behavioural problems. J. Intellect. Disabil. Res. 2022, 66, 162–177. [Google Scholar] [CrossRef]
- López-Olmedo, N.; Carriquiry, A.L.; Rodríguez-Ramírez, S.; Espinosa-Montero, J.; Hernández-Barrera, L.; Campirano, F.; Martínez-Tapia, B.; Rivera, J.A. Usual Intake of Added Sugars and Saturated Fats Is High while Dietary Fiber Is Low in the Mexican Population. J. Nutr. 2016, 146, 1856S–1865S. [Google Scholar] [CrossRef] [PubMed]
- van der Wurff, I.S.M.; Meyer, B.J.; de Groot, R.H.M. Effect of Omega-3 Long Chain Polyunsaturated Fatty Acids (n-3 LCPUFA) Supplementation on Cognition in Children and Adolescents: A Systematic Literature Review with a Focus on n-3 LCPUFA Blood Values and Dose of DHA and EPA. Nutrients 2020, 12, 3115. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.A.; Cannavale, C.; Iwinski, S.; Liu, R.; McLoughlin, G.M.; Steinberg, L.G.; Walk, A.M. Visceral Adiposity and Diet Quality Are Differentially Associated with Cognitive Abilities and Early Academic Skills Among Preschool-Age Children. Front. Pediatr. 2020, 7, 548. [Google Scholar] [CrossRef]
- Nistal, M.T.F.; Bertrán, A.M.T.; de la Paz Ross Argüelles, G. Un Estudio Normativo de los Ítems Evolutivos del Test del Dibujo de la Figura Humana en Niñs Indígenas Yaquis. Rev. Iberoam. Diagnóstico. Y Evaluación Psicológica 2015, 39, 77–90. [Google Scholar]
- Ortiz-Andrellucchi, A.; Peña-Quintana, L.; Saavedra-Santana, P.; Albino-Beñacar, A.; Monckeberg-Barros, F.; Serra-Majem, L. Facing malnutrition and poverty: Evaluating the CONIN experience. Nutr. Rev. 2009, 67 (Suppl. S1), S47–S55. [Google Scholar] [CrossRef]
| Indicators | Cut-Off Point | Measurement Date | ||||
|---|---|---|---|---|---|---|
| 3 March 2020 (%) | 26 April 2022 (Mean ± SD) | 3 March 2020 (%) | 26 April 2022 (Mean ± SD) | p | ||
| Anthropometric | ||||||
| LGD (cm) | Height-for-age (HAZ-Score ≤ −1) | 35.0 | −1.60 ± 0.26 | 38.8 | −1.52 ± 0.31 | 0.660 |
| Stunting (cm) | Height-for-age (Z-Score ≤ −2) | 43.8 | −2.95 ± 2.81 | 37.5 | −2.67 ± 0.74 | 0.472 |
| Undernutrition (cm) | LGD + Stunting | 78.8 | −2.35 ± 2.21 | 76.3 | −2.10 ± 0.80 | 0.733 |
| Excess of body weight (kg/m2) | BMI-for–age (percentile) | 24.1 | 93.0 ± 5.20 | 31.1 | 94.0 ± 4.60 | 0.342 |
| DBM (cm + kg/m2) | HAZ ≤ −2 SD + BMI-for–age (≥85th percentile) | 7.50 | −2.29 ± 0.27 89.40 ± 4.80 | 3.75 | −2.21 ± 0.24 93.70 ± 5.6 | 0.371 |
| Adiposity markers | ||||||
| Body fat mass (%) | Body fat mass (boys > 20); (girls > 25) | 2.50 | 24.10 ± 9.05 NA | 16.3 | 24.62 ± 6.53 27.14 ± 3.49 | 0.001 |
| Central obesity (cm) | Waist circumference (≥75th percentile) | 16.5 | 85.20 ± 7.50 | 26.3 | 87.30 ± 6.70 | 0.168 |
| Excess of adiposity (mm/mm2) | Tricipital skinfold (≥85th percentile) | 7.60 | 90.11 ± 4.30 | 11.3 | 90.16 ± 4.60 | 0.629 |
| Arm fat area (>85th percentile) | 7.60 | 93.40 ± 4.88 | 20.0 | 93.03 ± 4.60 | 0.024 | |
| Excess of fat mass (kg/m2) | Fat Mass Index (according to sex and age) | 5.10 | 5.42 ± 2.66 | 16.3 | 6.60 ± 2.87 | 0.011 |
| Cardiometabolic risk factors | ||||||
| High blood pressure (mmHg) | Systolic blood pressure (≥90th percentile) | 22.5 | 94.40 ± 3.20 | 16.3 | 93.90 ± 3.00 | 0.284 |
| Waist-to-height ratio | Waist-to-height ratio (≥0.5) | 24.1 | 0.54 ± 0.05 | 32.5 | 0.56 ± 0.06 | 0.210 |
| Cognitive ability | Cognitive score (<80) | 13.8 | 60.00 ± 20.00 | 21.3 | 58.00 ± 22.00 | 0.264 |
| Indicators | Boys | Girls | ||||
|---|---|---|---|---|---|---|
| 3 March 2020 (n = 39) | 26 April 2022 (n = 39) | p | 3 March 2020 (n = 41) | 26 April 2022 (n = 41) | p | |
| Height-for-age (Z-score) | −1.87 ± 0.89 | −1.78 ± 0.93 | 1 × 10−4 | −1.63 ± 0.76 | −1.52 ± 0.92 | 1 × 10−4 |
| BMI-for-age (kg/m2) | 17.30 ± 2.91 | 18.70 ± 3.71 | 1 × 10−4 | 17.50 ± 2.24 | 19.60 ± 3.65 | 1 × 10−4 |
| Body fat mass (%) | 8.15 ± 5.15 | 13.30 ± 7.04 | 1 × 10−4 | 14.83 ± 2.60 | 16.60 ± 4.91 | 1 × 10−4 |
| Waist circumference (cm) | 57.80 ± 7.78 | 65.60 ± 9.0 | 1 × 10−4 | 58.60 ± 9.80 | 67.40 ± 8.80 | 1 × 10−4 |
| Tricipital skinfold (mm) | 9.30 ± 4.19 | 11.52 ± 7.15 | 1 × 10−4 | 11.36 ± 3.30 | 13.30 ± 5.50 | 3 × 10−3 |
| Arm fat area (mm3) | 8.52 ± 5.21 | 12.26 ± 10.0 | 2 × 10−3 | 10.39 ± 4.03 | 14.18 ± 8.08 | 1 × 10−4 |
| Fat Mass Index (kg/m2) | 1.53 ± 1.50 | 2.70 ± 2.37 | 1 × 10−4 | 2.63 ± 0.77 | 3.40 ± 1.77 | 1 × 10−4 |
| Systolic blood pressure (mmHg) | 100 ± 9 | 102 ± 8 | 0.32 | 98 ± 12 | 102 ± 9 | 0.01 |
| Waist-to-height (ratio) | 0.47 ± 0.07 | 0.49 ± 0.06 | 1 × 10−4 | 0.47 ± 0.08 | 0.49 ± 0.06 | 1 × 10−3 |
| Cognitive ability (score) | 83.00 ± 4.00 | 79.00 ± 14.00 | 1 × 10−4 | 77.00 ± 15.00 | 76.00 ± 15.00 | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbosa-Martín, E.; Pena-Espinoza, B.; Escalante-Sosa, R.; May-Kim, S.; Sánchez-Pozos, K.; Ortiz-López, M.G.; Torre-Horta, E.; Menjivar, M. The Harmful Impact of COVID-19 on Adiposity Markers and Cognitive Development in Maya Children. COVID 2025, 5, 164. https://doi.org/10.3390/covid5100164
Barbosa-Martín E, Pena-Espinoza B, Escalante-Sosa R, May-Kim S, Sánchez-Pozos K, Ortiz-López MG, Torre-Horta E, Menjivar M. The Harmful Impact of COVID-19 on Adiposity Markers and Cognitive Development in Maya Children. COVID. 2025; 5(10):164. https://doi.org/10.3390/covid5100164
Chicago/Turabian StyleBarbosa-Martín, Enrique, Barbara Pena-Espinoza, Rachel Escalante-Sosa, Shérlin May-Kim, Katy Sánchez-Pozos, María Guadalupe Ortiz-López, Emmanuel Torre-Horta, and Marta Menjivar. 2025. "The Harmful Impact of COVID-19 on Adiposity Markers and Cognitive Development in Maya Children" COVID 5, no. 10: 164. https://doi.org/10.3390/covid5100164
APA StyleBarbosa-Martín, E., Pena-Espinoza, B., Escalante-Sosa, R., May-Kim, S., Sánchez-Pozos, K., Ortiz-López, M. G., Torre-Horta, E., & Menjivar, M. (2025). The Harmful Impact of COVID-19 on Adiposity Markers and Cognitive Development in Maya Children. COVID, 5(10), 164. https://doi.org/10.3390/covid5100164






