The effect of weather conditions on respiratory diseases is one of the most critical factors indicated by researchers. Respiratory diseases are widespread globally and are the third cause of non-communicable mortality [
5]. Many studies have confirmed positive connections between public health and weather indicators, such as temperature, humidity, or wind speed [
6,
7]. One crucial question during the COVID-19 pandemic is whether there is a connection between weather conditions and the COVID-19 virus spread. This study tries to answer that question. Determining this connection could help governments make more informed policy decisions and become more prepared for the next waves and next pandemics.
Some previous studies have shown that seasonal and geographic climatic change could affect the spread of respiratory diseases, the concentrations of those studies were mostly on influenza, SARS, and MERS-COV but not COVID-19, which is distinctive from other recognized viruses in its spread and pathogenicity. From another angle, there are several studies about government policy and its effects on controlling respiratory diseases. A close relationship between government and society is not inevitable during abnormal conditions like the COVID-19 pandemic. This study also tries to identify the effect of government regulations on controlling COVID-19 transmissions.
Second, the generalized additive model (GAM) was applied to answer the research question. The GAM was selected for this study because it can work with many distributions, such as gamma, normal, and Poisson, and the distribution of dependent variables in this study is Poisson.
This study, which focuses on South Korea’s initial regulation period, innovates by merging climate data with an analysis of the consequences of public policy on COVID-19 transmission. Our work incorporates these components to give a comprehensive picture of their combined impact on virus distribution, in contrast to other research that frequently separates climate factors or policy effects. This study provides an improved method for simulating COVID-19 transmission by utilizing the generalized additive model (GAM), which takes into account a variety of distributions and incorporates nonlinear interactions. Together with an analysis of South Korea’s early intervention tactics, this methodological development offers fresh perspectives on the policy-driven and environmental aspects of pandemic management. Compared to previous studies, this research uses more features that can affect the spread of the COVID-19 virus. This study is different since it tries to connect two different literature angles by applying climate indicators and government regulation in the same regression as right-hand-side variables. The Infectious Disease Alert level 4 (red) policy caused a decrease in mobility of more than 10% for the whole country; this policy can help control the mobility effect in this study since the city-level mobility data for South Korea are not available. Other contributions of this study include finding reliable predictive models for daily COVID-19 positive cases in countries with the most advanced health care systems and forecasting numbers of infections by applying the GAM. By addressing the gap in understanding the interaction between climate and policy, this study not only enhances current knowledge but also provides a framework applicable to other pandemic scenarios, paving the way for more informed and effective public health strategies globally.
1.1. Literature Review
Coronaviruses (CoVs) belong to the Coronaviridae family, a group of enveloped, positive-sensed, single-stranded RNA viruses [
11]. These types of viruses are named CoVs due to their crown shape [
12]. Coronaviruses are a widespread group of viruses that are prevalent among animals. Zoonotic transmission, in which viruses travel from animals to humans, has played a crucial role in recent pandemics, including COVID-19, which was initially discovered on 31 December 2019, in Wuhan, China. According to research conducted in China and South Korea, personal contact is the predominant mechanism of COVID-19 transmission. This highlights the need of understanding both environmental and behavioral factors that influence disease spread [
13].
Since 31 December 2019, when the first positive case of COVID-19 was detected in Wuhan, China, people worldwide have struggled with this disease [
14]. Based on recent studies, COVID-19 transmission has been mostly happening through physical contact; for example, a study in China reported that 41% of patient infections were due to person-to-person hospital visits [
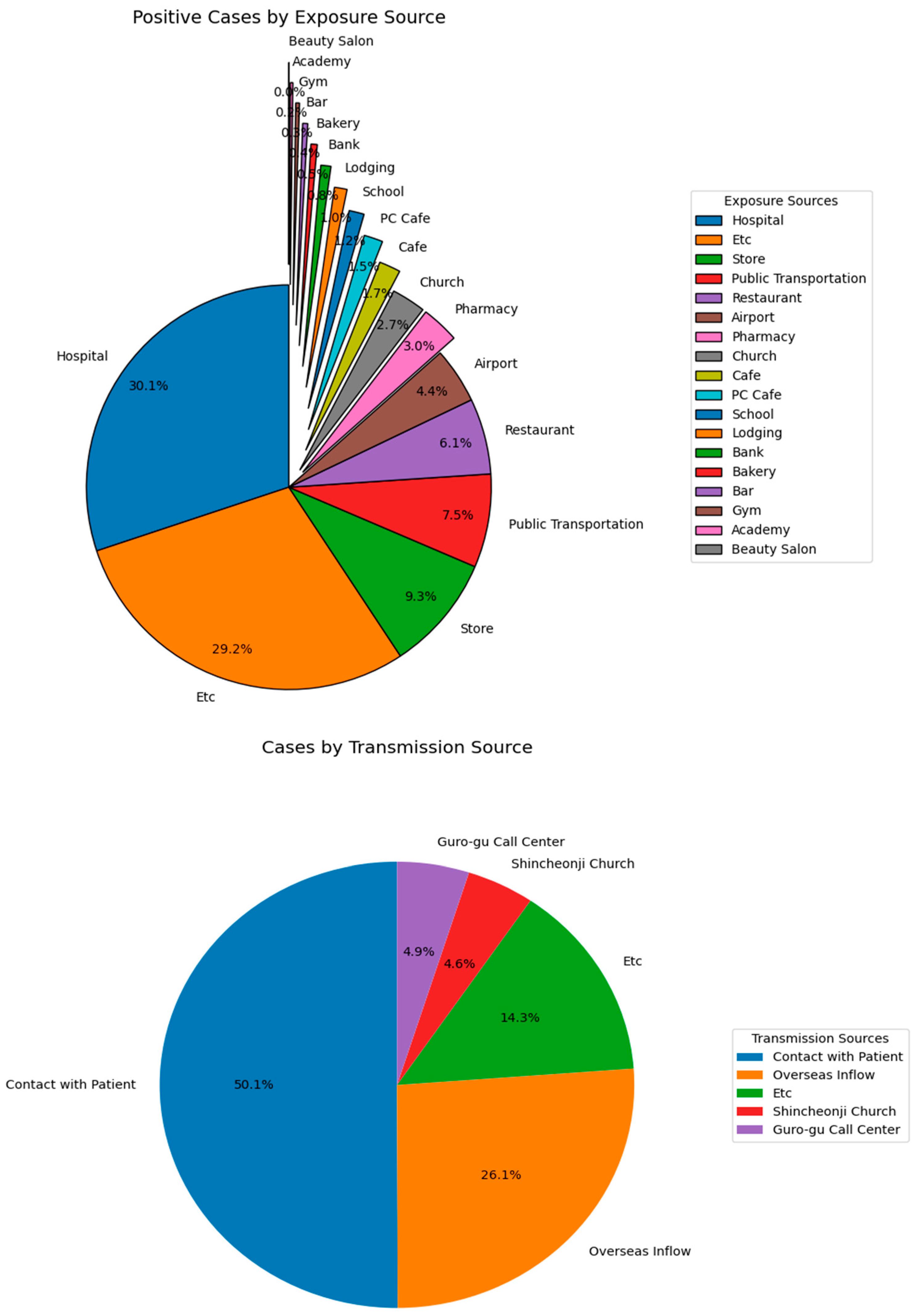
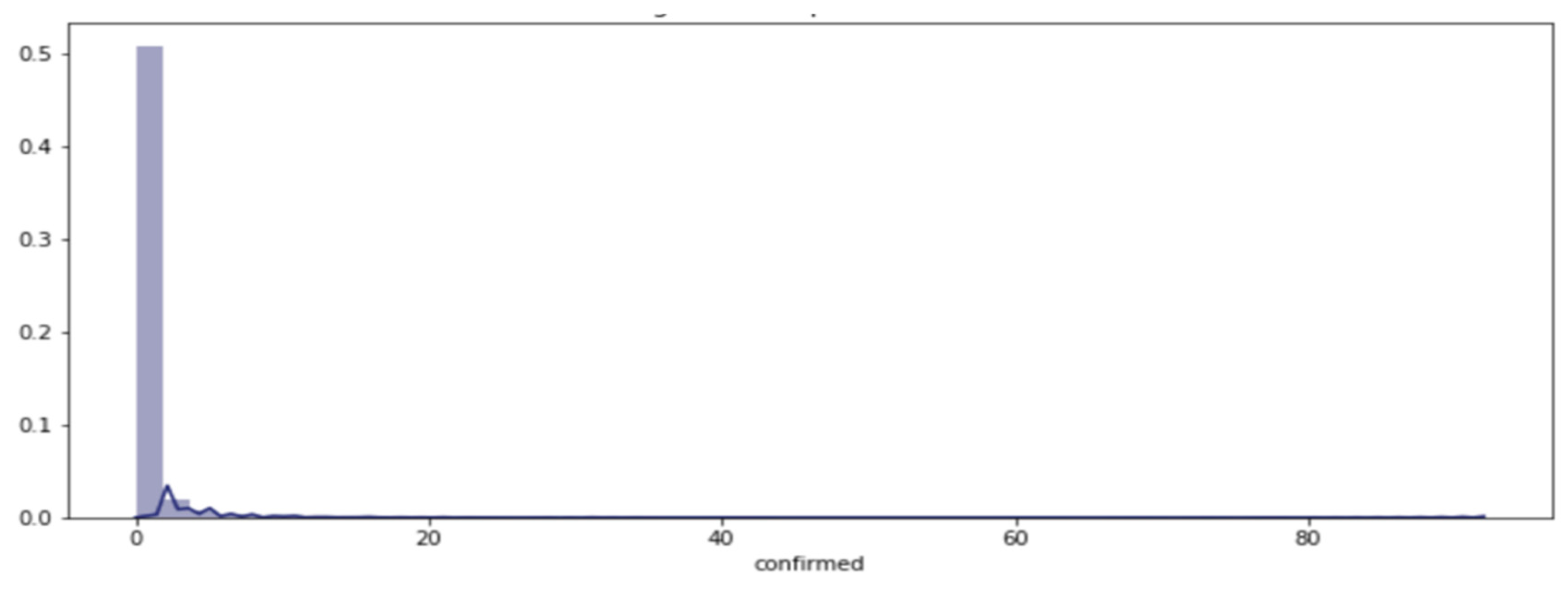
15]. Furthermore, our results are consistent with this fact in the case of South Korea during the timeline of this study (
Figure 1).
The literature has two strands: disease spread patterns and weather connection and public policy. First, let us focus on the literature on the relationship between weather conditions and respiratory disease. Epidemiological and laboratory research has recognized a connection between weather conditions and respiratory diseases [
8,
16]. Weather conditions have an essential role in human health. A study was performed by Cheng et al. [
17] in the five most populated Australian cities (Sydney, Melbourne, Brisbane, Adelaide, and Perth) from 2000 to 2009, which analyzed the relationship between mortality rate and temperature variability. The results show that any significant temperature change can be associated with a higher mortality rate.
The risk of transmission can differ based on weather conditions related to respiratory diseases’ durability on various surfaces [
18,
19]. There is extensive literature about patterns between weather conditions and virus mortality.
In 2003, Bi et al. [
20] tried to estimate how weather conditions could change the speed of spread by applying data for a daily number of positive SARS cases in Beijing and Hong Kong during the 2003 pandemic. This study indicated that higher temperatures could decrease infection; air pressure, however, was positively correlated with the number of positive SARS cases. Likewise, a study in South Korea showed that the number of positive influenza cases increased significantly on days with lower temperatures and relative humidity [
21].
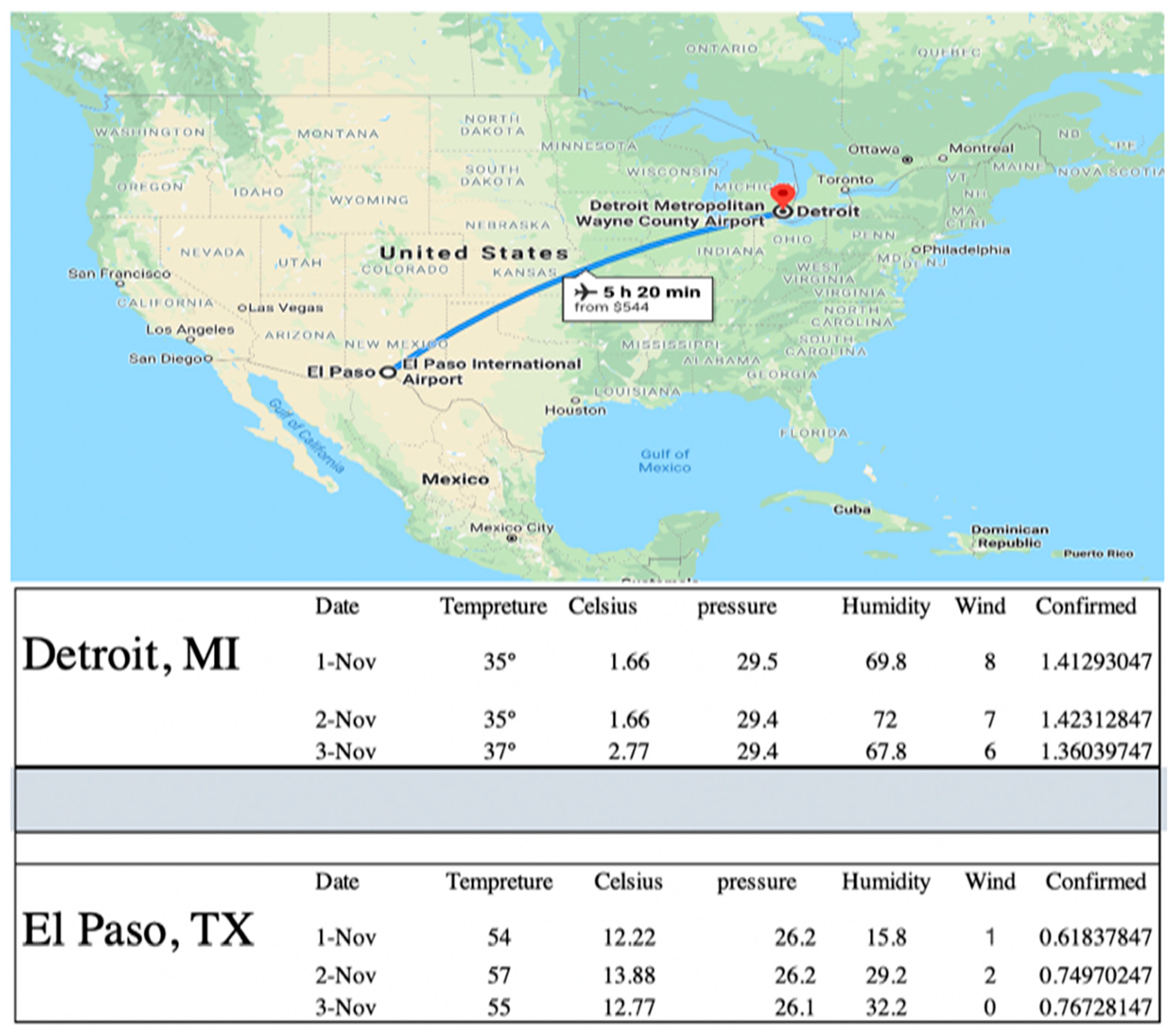
In 2020, Bashir [
22] conducted a study to analyze the relationship between weather indicators and the COVID-19 mortality rate in New York City. The weather condition variables in this study included average temperature, minimum temperature, maximum temperature, rainfall, average humidity, wind speed, and air quality. The outcome indicated that average temperature, minimum temperature, and air quality were significantly associated with the COVID-19 pandemic. Existing literature reveals a complex relationship between weather conditions and respiratory diseases. Research, such as that by Cheng et al. [
17], has shown that temperature variability can influence mortality rates. However, studies specifically connecting weather conditions to COVID-19 transmission are still emerging. For example, Bashir [
22] explored the impact of various weather indicators on COVID-19 mortality in New York City, while Hossain et al. [
23] examined similar factors across South Asia, highlighting the role of climate indicators like rainfall and air pollution. These studies point to a significant association between climate factors and the spread of respiratory diseases, yet the precise mechanisms remain unclear. This research aims to bridge this gap by investigating how climate conditions interact with social behaviors to affect COVID-19 transmission.
In 2021, Hossain et al. [
23] aimed to investigate the effect of weather-condition factors on the number of COVID-19 infected cases in South Asian countries—India, Afghanistan, Pakistan, Bangladesh, and Sri Lanka—from the day of the first infection case to 31 August 2020 in each country. The climate indicators in this study included aggregate rainfall, relative humidity, surface pressure, maximum and minimum temperature (in °C), maximum air pollutants, and maximum wind velocity (m/s). The autoregressive integrated moving average with explanatory variables (ARIMAX) model was applied as an estimator model. The outcomes show that aggregated rainfall, air pollution, and maximum wind velocity play an essential role in spreading coronavirus in these countries.
In 2021, Zhang et al. [
24] tried to estimate the effect of temperature and humidity on COVID-19 infection numbers for 1236 areas worldwide. The weather data were collected from a large-scale satellite, and the results indicate that temperature and relative humidity have a negative relationship with the global spread of COVID-19.
Most previous research in this section has indicated that temperature and humidity negatively affect respiratory disease infections [
25,
26]. The mucus produced in cold weather, however, is especially concentrated and dense, which can lead to obstructions in the respiratory system and raise the likelihood of catching a cold or other respiratory diseases [
2].
There is another relevant strand of respiratory disease literature. There are several studies on government policy and its effects on controlling respiratory diseases [
27,
28]. For example, Nidhi and Jayaraman [
29] tried to estimate the effect of Indian government regulations on the amount of carbon dioxide released by factories. They used the information of people who had been hospitalized for respiratory illnesses in seven Delhi hospitals between 1998 and 2004. For the patient population, they applied the Poisson regression model. Their results indicate that the regulations caused a notable reduction in the monthly average density of sulfur dioxide; the monthly average density of nitrogen dioxide, however, increased by 2%. These changes in air quality reduced the number of respiratory patients significantly, by about 12%.
A study in Vietnam examined the effectiveness of government policy during the coronavirus pandemic. The study’s timeline was divided into four periods based on four principal government regulations: emergency responses, border and entry control measures, social isolation, and financial support. The findings show that the Vietnamese policy system responded quickly, proactively, and virtually at multiple authority levels [
30]. Another research by Wielechowski et al. [
31] in 2020 tried to determine how government lockdown regulations in Poland affected mobility and the spread of COVID-19 between 2 March and 19 July 2020. The results indicated that lockdown decreased the number of positive COVID-19 cases in Poland but that social distance regulations were more effective than lockdown. In addition to environmental factors, government policies and social behaviors play crucial roles in disease spread. Research on government regulations, such as those by Nidhi and Jayaraman [
29] and Wielechowski et al. [
31], demonstrates the impact of policy interventions on respiratory diseases and COVID-19. However, the interaction between these policies and environmental factors, particularly in the context of a pandemic, requires further exploration.
This study seeks to integrate these diverse strands of research by examining how climate variables, social activities, and public policies interact to influence COVID-19 transmission. By focusing on both climatic conditions and social behaviors and employing advanced statistical methods like the Generalized Additive Model (GAM), this research aims to provide a comprehensive understanding of the factors affecting pandemic dynamics. This approach addresses gaps in current literature and offers actionable insights for future public health strategies.
1.2. Data Set Description
The data set includes 11,000 observations, including all the confirmed positive coronavirus cases. The South Korean data set is a reliable source because of the country’s aggressive testing protocol and sizable testing capacity. During this study’s timeline, around 500,000 individuals were tested—1% of South Korea’s population. Sub-national level data and spatial variation in weather within the country were used. We collected daily COVID-19 confirmed case data from the official website of the KCDC (the Korea Centers for Disease Control and Prevention, which is South Korea’s main public health agency responsible for managing disease outbreaks and collecting health data) and daily weather data from NASA’s website. City-level panel data analysis was used for this research. The data covered the information of nine provinces as well as 95 cities in South Korea (
Figure 2).
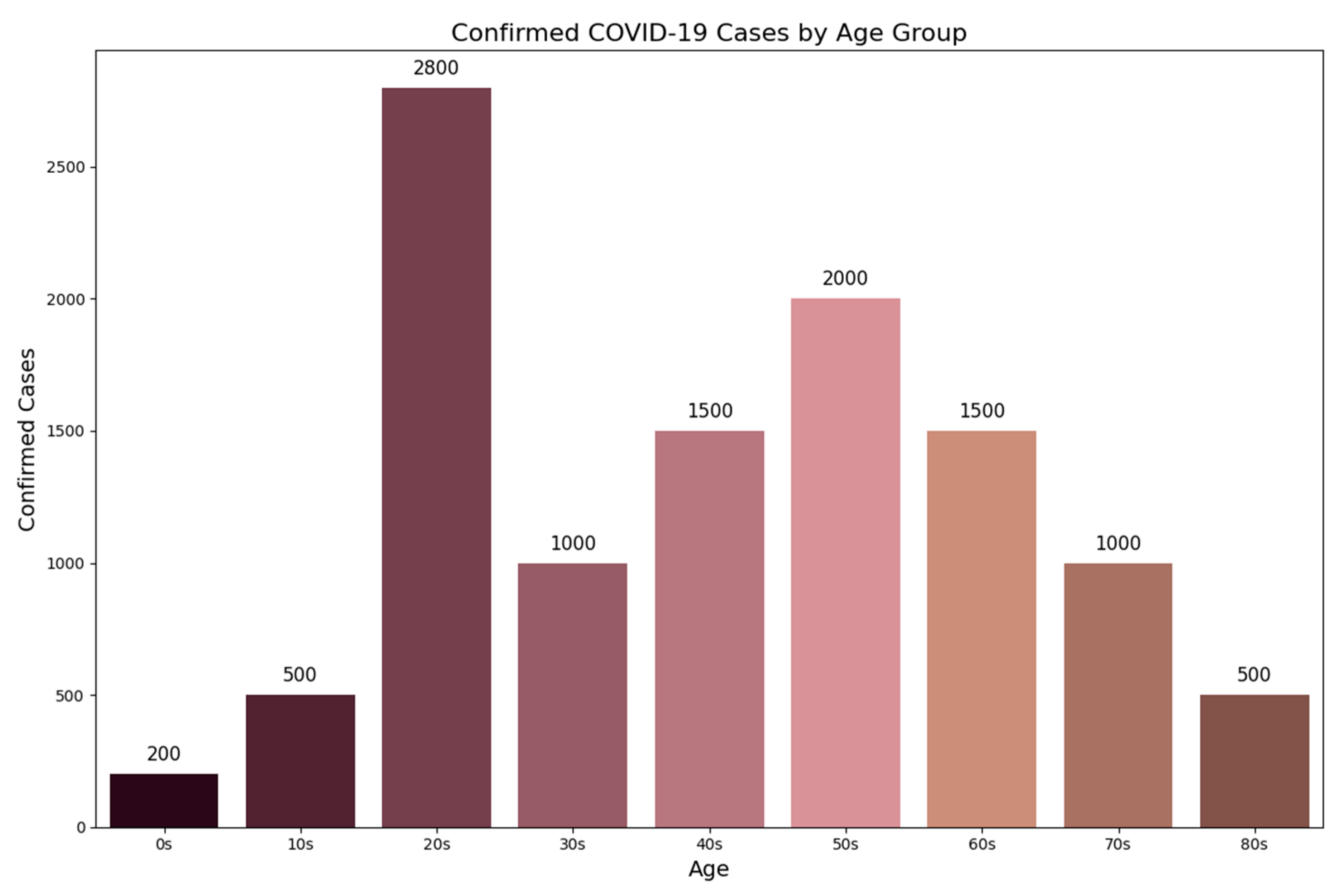
The COVID-19 data set consists of the following three categories: patient data, policy data, and local data. The patient data category includes per-patient symptom onset date, confirmed date, and state deceased. The symptom onset date is when each patient first displayed symptoms of COVID-19, and the confirmed date is the date that the patient was diagnosed. An age-specific number of patients was also indicated in this category. As shown in
Figure 3, people in their twenties have the highest infection rate, but the lowest rate belongs to infants and kids.
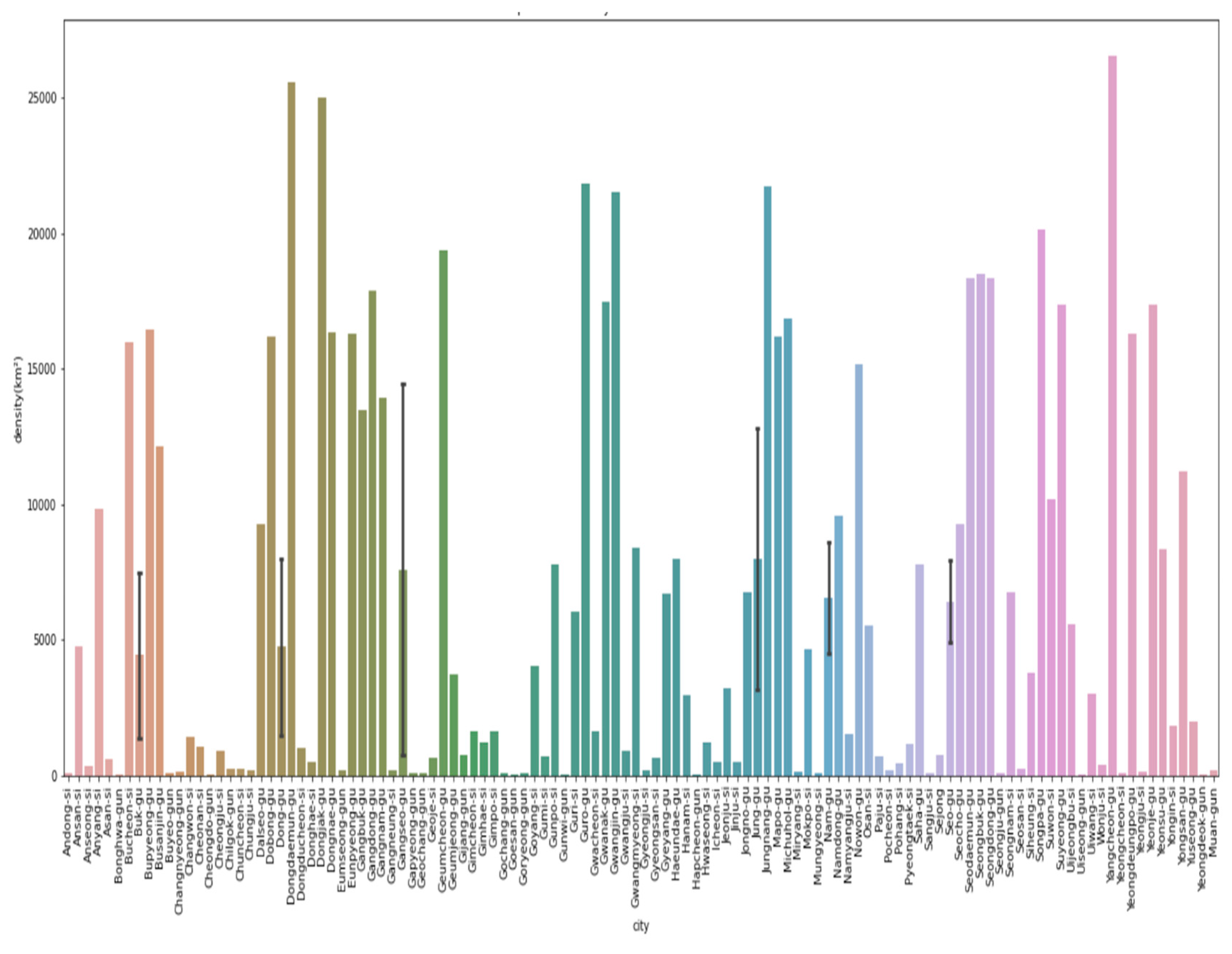
The second category is regional data, which includes number of screening centers, land size, and population of each province. It also includes 178 cities in 17 South Korean provinces (126.30–129.47° east longitude and 33.45–38.19° north latitude).
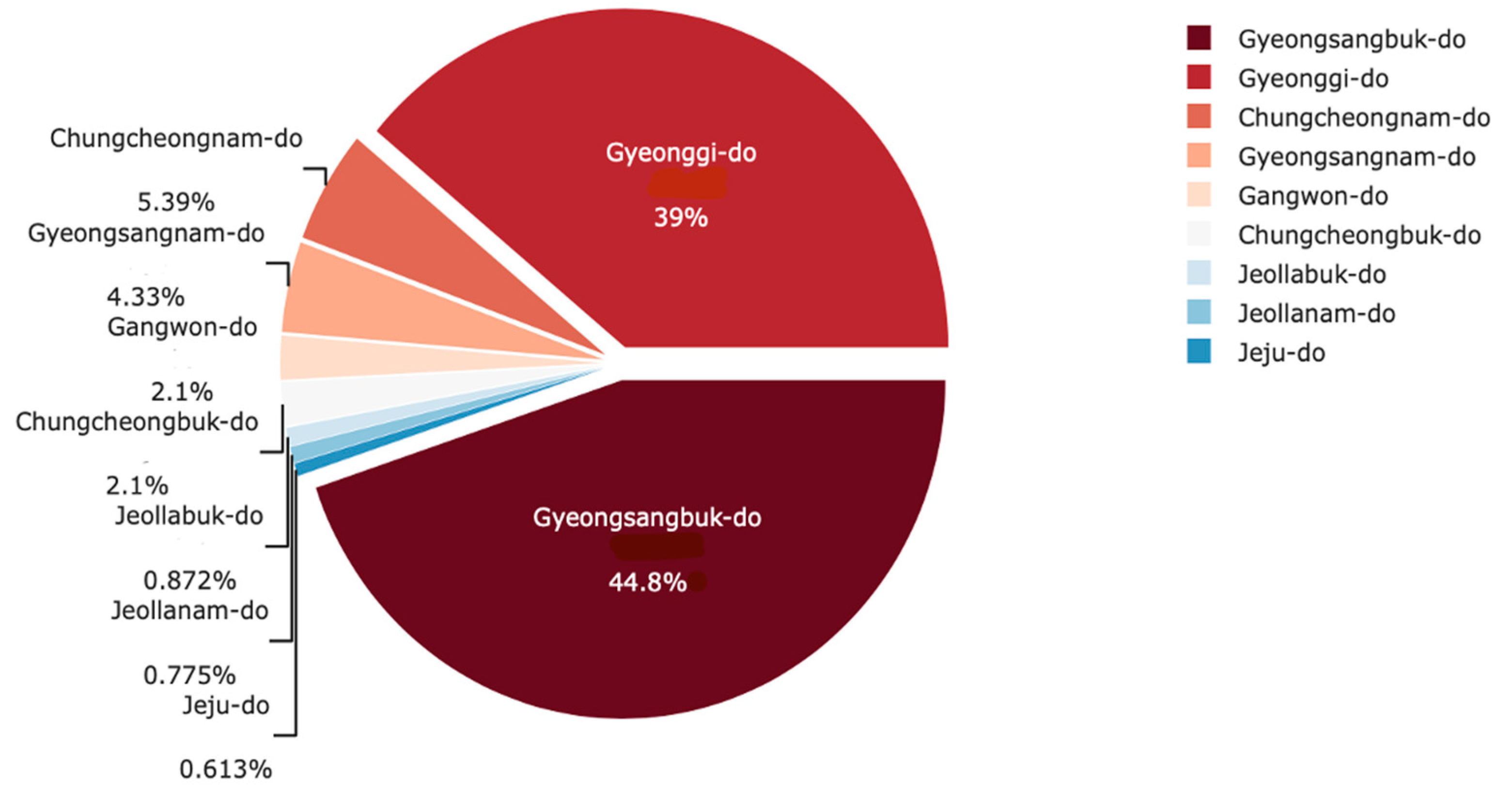
Among these 15 provinces, Gyeongsangbuk-do had the highest COVID-19 spread rate (35.2% of all cases detected during that study period), and the first COVID-19 case was seen in this province.
Figure 4 shows more details about this.
Lastly, policy data include descriptions and the start and end dates of eight preventative policies enacted by the Korean government [
28]. These eight policies include a broad range of policies, such as social, educational, and immigration policies. To help understand the policies’ effectiveness, the cumulative number of confirmed patients is appended as part of the data set.
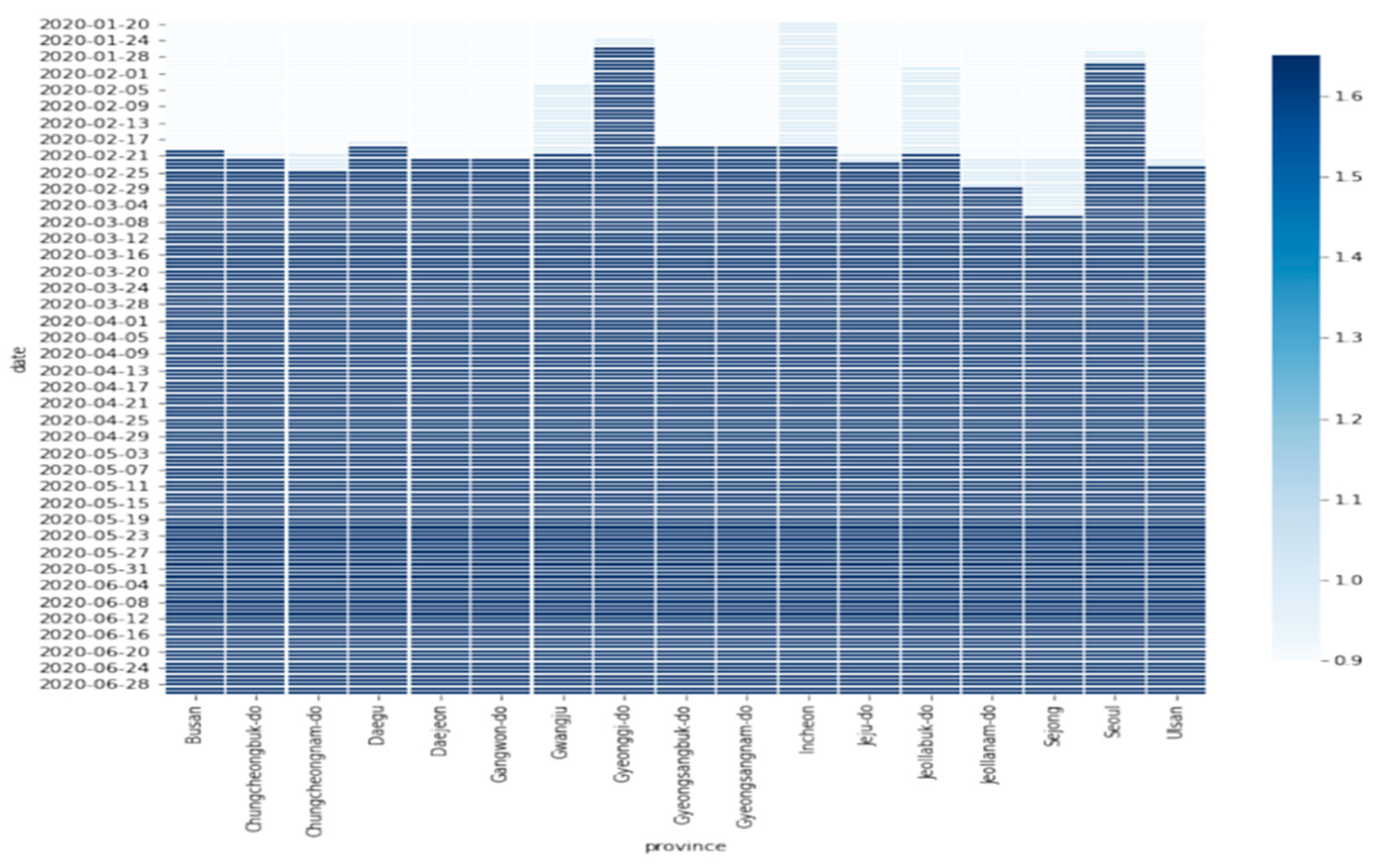
The timeline of this study is 20 January to 28 June 2020; during the timeline of this study, from 19 May to 12 June 2020, South Korea faced the highest number of infections in almost all provinces, as shown in
Figure 5.
The model also controlled for population density, the number of hospitals per 1000 people, the elderly population ratio, social distance order, the day of the week, and the young population ratio.
Table 1 shows summary statistics of selected variables in this study.
Although other weather condition variables applied in the regression are useful for explaining the relationship between weather conditions and the number of positive coronavirus cases, the minimum temperature is the variable of interest for this study for the following reasons. Firstly, among all explanatory variables, it has the highest correlation with the independent variable.
Secondly, there is a strong correlation between temperature and health, as critical temperatures can jeopardize health conditions by affecting the body’s ability to control its internal temperature [
25,
26]. There are also strong relationships between extreme temperature and cardiovascular disease, respiratory disease, cerebrovascular disease, and diabetes-related conditions [
32].
Lastly, since temperature varies by season, it is more predictable than other climate variables [
25,
26]. Hence, governments can be more prepared and face an issue more effectively based on temperature data. Furthermore, this study’s dependent variable is count data, which is reflected in the number of occurrences of behavior in a fixed period, such as the number of positive COVID-19 cases [
33]. A proper model, then, is required to work with this type of data, which will be explained in more detail in the
Section 2.3.1.
This research innovatively combines weather conditions with COVID-19 transmission dynamics to analyze the impact of temperature and humidity on virus spread. It highlights how higher temperatures and humidity can reduce transmission and examines the effectiveness of South Korea’s initial regulatory measures. This dual-focus approach enhances our understanding of both environmental factors and policy responses in managing the pandemic [
27,
28].