Abstract
Many surgical practices closed at the onset of the COVID-19 pandemic. We implemented operational changes to safely continue treating patients with cutaneous tumors during the pandemic. This study seeks to evaluate the impact of pandemic-based operational changes on safety, access, and treatment. Here, we report results from a retrospective study from a single academic office-based surgical practice that provided treatment to patients with skin cancer between November 2019 and September 2020. Time to treatment, tumor area, and upstaging after treatment were compared among patients seen “pre-pandemic” (November 2019 to March 2020), during the “pause” (March 2020 to June 2020), and in the “reopening” (June 2020 to September 2020). One-way ANOVA or Fisher Exact analyses were performed, and p < 0.05 was considered significant. Our study included 691 patients (22–101 years old) with a total of 912 tumors. No cases of COVID-19 transmission occurred during the study period. The time from consultation to treatment was reduced during the pause and reopening periods relative to pre-pandemic (p ≤ 0.002), and the average Mohs post-operative defect size remained unchanged throughout the study period (p = 0.75). Consistent with the prioritization of higher-risk tumors in the pandemic peak, a significant reduction in the treatment of basal cell carcinoma tumors was noted during the pause (p = 0.01), and cutaneous squamous cell carcinoma tumors were upstaged more frequently after treatment (p < 0.001). Our findings demonstrate that practice modifications can permit essential surgical care to be delivered safely to patients with high-risk skin cancers during a pandemic.
1. Introduction
COVID-19 has placed tremendous strain on healthcare systems globally. The fear and uncertainty experienced during the early pandemic led to emergency declarations suspending non-essential care. Such recommendations aimed to mitigate the risk of virus transmission by altering patient volumes and staffing patterns, triaging hospital bed and ventilator capacity, and preserving personal protective equipment (PPE). As a result, many elective procedures and office visits were postponed, and some practices temporarily shut down [1].
The relative urgency of skin (and other) cancer screening and treatment came under scrutiny in early efforts to triage healthcare resources. Many countries suspended national skin cancer screening programs, resulting in decreased skin cancer diagnoses and referrals [2,3,4,5]. Specifically, a recent study from the Netherlands reported a 60% decline in skin cancer diagnoses over the first 1.5 months of the pandemic when nationwide screening was halted [2]. Similarly, Andrew et al. reported a 68.61% decrease in skin cancer diagnoses during the first 3 months of the pandemic in the UK [5]. Recognizing that some skin cancers have fairly indolent courses [6], while others exhibit more aggressive features or arise in a compromised host and have the potential to threaten life or function [7,8,9,10,11,12], risk stratification algorithms defining acceptable timeframes for postponing skin exams and cancer treatment were developed [13,14,15,16,17,18,19,20,21,22].
The full consequences of delays in skin cancer diagnosis and treatment are likely not yet realized, but several studies have already documented patients presenting with thicker or larger tumors after lockdowns were lifted [2,3,5]. For example, an Italian study found that patients presented with thicker melanomas in the period immediately following their country’s lockdown [3]. Moreover, established associations between tumor size or depth, staging, and disease-specific mortality for more aggressive cutaneous malignancies raise concerns that delays in skin cancer diagnosis and treatment may lead to poorer outcomes for some patients [23].
In the US, dermatologic surgery is often performed in an outpatient setting under local anesthesia. As such, it does not tie up pandemic mission-critical resources, such as ventilators. If cases are appropriately triaged, the overall impact on the supply chain is minimal. Rather than closing during the early pandemic, the Dermatologic Surgery Unit at New York University remained open with modified operations to continue to provide safe care for patients with cutaneous tumors. We implemented several operational changes to ensure continued care for patients with skin tumors, including (1) modified scheduling, staffing, and rooming; (2) COVID-19 symptom screening and testing where appropriate; (3) adequate PPE for patients and staff (such as N95 respirators and face shields); (4) triage based on tumor acuity; (5) same-day or video consultation; and (6) increased utilization of same-day biopsy and surgery for suspicious lesions. Here, we studied the impact of these changes on safety, access, and treatment.
2. Materials and Methods
We conducted a single-center retrospective study in an academic office-based dermatological surgical practice. All patients were referred for the treatment of skin cancer between November 2019 and September 2020 and consented to inclusion in research. Patients were divided into three groups: those seen pre-pandemic (1 November 2019 to 21 March 2020), patients seen during the mandated pause (22 March 2020 to 8 June 2020), and patients seen during the early reopening (9 June 2020 to 30 September 2020). We evaluated time to treatment, tumor area, and tumor upstaging using analysis of variance (ANOVA, continuous variables) or Fisher Exact (nominal variables) analysis. Here, p < 0.05 was considered to indicate statistically significant results.
3. Results
Study results are summarized in Table 1. Our study population included 912 tumors from 691 patients ranging in age from 22 to 100.8 years, and a slight male predominance (564 males vs. 348 females) was observed. Despite continuing to provide care, our unit experienced a significant decrease in volume during the pandemic pause, which had largely recovered by the reopening period (Figure 1). No cases of COVID-19 transmission were attributable to maintained operations that occurred during the study period. The proportion of patients taking immunosuppressive medications was enriched (p = 0.03) during the pause (16.9%) relative to the pre-pandemic (7%) or reopening (4.2%) phases.

Table 1.
Characteristics of patients and tumors treated in the pre-pandemic, pause, and reopening phases of the COVID-19 pandemic.
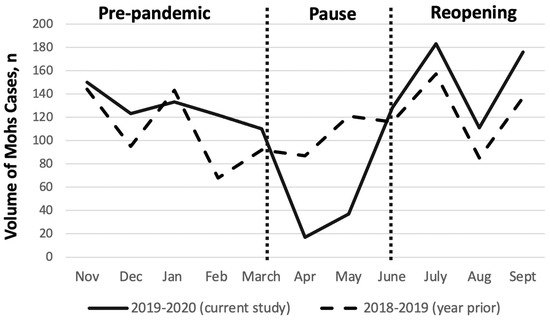
Figure 1.
Mohs case volumes at the NYU Dermatologic Surgery unit in the period from2019 to2020 (solid black line, current study) and from 2018 to2019 (dashed black line, year prior).
The time from biopsy to treatment was unchanged during the pause (56 days vs. 66 days, p = 0.7), but tumors were treated within 8 days of consultation during the pause, compared with 28 days during the pre-pandemic period (p = 0.002). This trend toward more rapid access to care persisted into the reopening phase (p = 0.001). During the pause, a significant reduction in the treatment of basal cell carcinoma (BCC, p = 0.01) was noted as these tumors are generally considered to represent a lower overall risk. Specifically, BCC tumors represented 50.4% and 49.5% of all cutaneous tumors treated during the pre-pandemic and reopening phases, respectively. In contrast, BCC tumors comprised 32.8% of skin tumors treated during the pause. Correspondingly, a relative shift toward treatment of higher-risk tumors, such as squamous cell carcinoma (SCC), malignant melanoma (MM), and other rare tumors, was observed. In total, 50.0% of all cutaneous tumors treated during the pause were SCC, representing an increase compared with percentages observed during the pre-pandemic (39.6%) and reopening (44.65%) periods. Similar trends were noted for MM given that these lesions represented 4.2% of cases during the pre-pandemic period compared with 8.6% during the pause; however, the difference was not statistically significant.
Regarding treatment modality, the majority of tumors were treated with Mohs surgery (n = 804, 88.2%). However, standard excisions (n = 81, 8.9%), staged excisions (n = 10, 1.1%), and electrodessication and curettage (n = 16, 1.75%) were also performed as appropriate throughout the study period.
We found no difference in the post-operative defect size for all surgical procedures (p = 0.54) or Mohs cases (p = 0.75) across all groups.
We detected a significant increase in the percent of SCC tumors that were upstaged during the pause (p < 0.001). Specifically, 51.7% of SCC tumors were upstaged during the pause period. Fewer SCC tumors were upstaged during the pre-pandemic (17.3%) and reopening phases (15.2%), and the rates observed during these periods did not statistically differ (p = 0.66) (Figure 2).
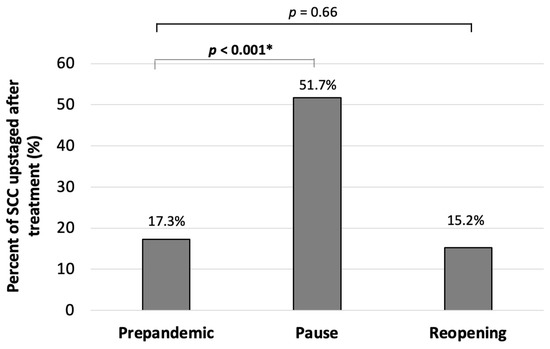
Figure 2.
Upstaging of cutaneous squamous cell carcinoma tumors during the pre-pandemic, pause, and reopening phases. Statistically significant comparisons are indicated in bold with an *.
4. Discussion
Our findings show that throughout the height of the COVID-19 pandemic, our unit was able to safely continue caring for our patients. During this period, we employed various operational measures to ensure continued care for patients with skin tumors, including modified scheduling, staffing, and rooming; COVID-19 symptom screening and testing where appropriate; adequate PPE for patients and staff; triage by tumor acuity; and same-day or video consultation. In addition, we also increased the utilization of same-day biopsy and surgery for suspicious lesions (Table 1). Here, we assessed the impact of these changes on three critical measures of patient care: safety, access, and treatment.
Regarding safety, no cases of COVID-19 transmission attributed to maintained operations were noted during the pause (Table 1). Although delayed presentation for healthcare services was encountered across all medical specialties throughout the pandemic [24], we were unable to detect delays in care for patients referred to our practice.
To ascertain the effects of the measure implemented at our practice to maintain care during the pandemic, we reviewed the average time to treatment as a measure of patient access to care. During normal operations, the average time from consultation to treatment was slightly less than one month, corresponding to an approximately 2-month time period from biopsy to treatment. During the pause, the 2-month time from biopsy to treatment was retained, but patients received treatment for tumors approximately one week after consultation. These trends of more rapid access to care persisted into the reopening.
We found no difference in the time from referring providers for biopsy to consultation during the pandemic. However, a significant reduction in the time from initial consultation to definitive treatment was observed. The more rapid access to care likely reflects initial decreases in overall volume as well as practice modifications implemented to minimize the risk of COVID-19 exposure for patients and staff (tumor triage, same-day consultation and surgery, and same-day frozen section biopsy with treatment). These practice modifications also increase practice efficiency. Several other studies from units that remained open during the pandemic also noted decreased skin cancer referrals and more rapid access to care for patients [5,25,26]. While some reports describe patients presenting with larger tumors or thicker melanomas as a consequence of pandemic lockdowns [3,27], our department did not observe any increase in the size of tumors treated during the pause or reopening (Table 1). This finding offers reassurance that by maintaining access to surgical services, the unit continued to treat malignancies in a timely manner.
We examined whether post-operative defects might be larger due to potential delayed care. Interestingly, post-operative defects for all surgical procedures and Mohs cases were similar to normal operations in the pause and reopening (Figure 2). This finding suggests that overall, tumor size was not affected by changes in operations or patient avoidance related to the COVID-19 pandemic.
Consistent with advisory statements recommending triage of the highest risk cases and the results of other studies [4,28], we treated proportionally fewer BCC tumors and more SCC, MM, and other rare tumors during the pandemic pause. To evaluate the acuity of tumors treated during the different phases, we evaluated the upstaging of SCC tumors after treatment. Consistent with our intention to prioritize treatment of higher-risk tumors during the peak of the pandemic, we detected a significant increase in the number of SCC that were upstaged during the pause. We also noted that the number of tumors upstaged was similar in pre- and reopening. This finding suggests that access was not significantly delayed.
Organ transplant recipients as well as patients on immunosuppressive medications or with underlying immunomodulating medical conditions are at risk for aggressive tumors. A higher percentage of our patients treated during the pandemic pause were on immunosuppressive medications for organ transplant or inflammatory diseases, compared with those treated pre-pandemic or during the reopening. Increased skin cancer incidence, awareness, and established relationships with dermatology providers among these patient populations may have contributed to this observation [29,30,31]. Although these patients may be at elevated risk of suffering poor outcomes from COVID-19 [23], they are also more likely to suffer poor outcomes from aggressive cutaneous malignancies [32]. Thus, with our modified operations in place, we did not feel it was appropriate to postpone their care.
We conclude that practice modifications can permit essential surgical care to be delivered safely to patients with high-risk skin cancers during a pandemic. Maintaining outpatient dermatological surgery services during a pandemic prevents backlog accumulation and has the potential to improve long-term patient outcomes by treating lesions before they have a chance to progress. The limitations of this study should be noted. Selection bias potentially affected our results as patients were required to have consented to inclusion in research. Further, the pandemic is ongoing given the emergence of variants, and our work does not capture data for patients who have delayed care beyond the study period. Extended follow-up will be required to gauge the full consequences of the COVID-19 pandemic on skin cancer diagnosis, treatment, and patient outcomes.
Author Contributions
Conceptualization, J.A.C. and M.L.S.; formal analysis, S.R.J.C.; data curation, A.C. and N.A.D.; writing—original draft preparation, S.R.J.C.; writing—review and editing, N.A.D., J.A.C. and M.L.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of NYU School of Medicine (i18-01209, approved on 10/5/2018).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of this study.
Data Availability Statement
Data used in this study are available from the author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Meredith, J.W.; High, K.P.; Freischlag, J.A. Preserving Elective Surgeries in the COVID-19 Pandemic and the Future. JAMA 2020, 324, 1725. [Google Scholar] [CrossRef]
- Dinmohamed, A.G.; Visser, O.; Verhoeven, R.H.A.; Louwman, M.W.J.; van Nederveen, F.H.; Willems, S.M.; Merkx, M.A.W.; Lemmens, V.E.P.P.; Nagtegaal, I.D.; Siesling, S. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020, 21, 750–751. [Google Scholar] [CrossRef]
- Ricci, F.; Fania, L.; Paradisi, A.; Di Lella, G.; Pallotta, S.; Sobrino, L.; Panebianco, A.; Annessi, G.; Abeni, D. Delayed melanoma diagnosis in the COVID-19 era: Increased breslow thickness in primary melanomas seen after the COVID-19 lockdown. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e778–e779. [Google Scholar] [CrossRef]
- Nolan, G.S.; Dunne, J.A.; Kiely, A.L.; Jones, R.O.P.; Gardiner, M.; Jain, A.; Abdelaty, M. The effect of the COVID-19 pandemic on skin cancer surgery in the United Kingdom: A national, multi-centre, prospective cohort study and survey of Plastic Surgeons. Br. J. Surg. 2020, 107, e598–e600. [Google Scholar]
- Andrew, T.W.; Alrawi, M.; Lovat, P. Reduction in skin cancer diagnoses in the UK during the COVID-19 pandemic. Clin. Exp. Dermatol. 2020, 46, 145–146. [Google Scholar] [CrossRef]
- Wehner, M.; Dalma, N.; Landefeld, C.; Pare-Anastasiadou, A.; Koutelidas, I.; Chren, M.; Aji, N.; Teng, C.; Koenig, B.; Tang, J.; et al. Natural history of lesions suspicious for basal cell carcinoma in older adults in Ikaria, Greece. Br. J. Dermatol. 2018, 179, 767–768. [Google Scholar] [CrossRef]
- Fields, R.C.; Busam, K.J.; Chou, J.F.; Panageas, K.S.; Pulitzer, M.P.; Allen, P.J.; Kraus, D.H.; Brady, M.S.; Coit, D.G. Five Hundred Patients with Merkel Cell Carcinoma Evaluated at a Single Institution. Ann. Surg. 2011, 254, 465–475. [Google Scholar] [CrossRef]
- Heenan, P.J.; Holman, C.D. Nodular malignant melanoma: A distinct entity or a common end stage? Am. J. Dermatopathol. 1982, 4, 477–478. [Google Scholar]
- Lattanzi, M.; Lee, Y.; Simpson, D.; Moran, U.; Darvishian, F.; Kim, R.; Hernando, E.; Polsky, D.; Hanniford, D.; Shapiro, R.; et al. Primary Melanoma Histologic Subtype: Impact on Survival and Response to Therapy. Gynecol. Oncol. 2018, 111, 180–188. [Google Scholar] [CrossRef]
- Eigentler, T.K.; Leiter, U.; Häfner, H.-M.; Garbe, C.; Röcken, M.; Breuninger, H. Survival of Patients with Cutaneous Squamous Cell Carcinoma: Results of a Prospective Cohort Study. J. Investig. Dermatol. 2017, 137, 2309–2315. [Google Scholar] [CrossRef]
- Thompson, A.K.; Kelley, B.F.; Prokop, L.J.; Murad, M.H.; Baum, C.L. Risk Factors for Cutaneous Squamous Cell Carcinoma Recurrence, Metastasis, and Disease-Specific Death: A Systematic Review and Meta-analysis. JAMA Dermatol. 2016, 152, 419–428. [Google Scholar] [CrossRef]
- Ruiz, E.S.; Karia, P.S.; Besaw, R.; Schmults, C.D. Performance of the American Joint Committee on Cancer Staging Manual, 8th Edition vs. the Brigham and Women’s Hospital Tumor Classification System for Cutaneous Squamous Cell Carcinoma. JAMA Dermatol. 2019, 155, 819–825. [Google Scholar] [CrossRef]
- Pavia, G.; Gargiulo, L.; Valenti, M.; Facheris, P.; Nucca, O.; Narcisi, A.; Borroni, R.G.; Costanzo, A. Skin cancers: How to balance the risks and benefits of surgery during COVID-19 pandemic (a Northern Italy single-center experience). Int. J. Dermatol. 2020, 59, 1287–1289. [Google Scholar] [CrossRef]
- NCCN. National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology: Advisory Statement for Non-Melanoma Skin Cancer Care during the COVID-19 Pandemic. 2020. Available online: https://www.nccn.org/covid-19/pdf/NCCN-NMSC.pdf (accessed on 1 June 2021).
- Surgery AcoM. American College of Mohs Surgery: COVID-19 (Coronavirus) Preparedness. 2020. Available online: https://www.mohscollege.org/UserFiles/AM20/Member%20Alert/COVIDAlert3March20.pdf (accessed on 1 June 2021).
- NCCN. National Comprehensive Cancer Network (NCCN): NCCN Short-Term Recommendations for Cutaneous Melanoma Management during COVID-19 Pandemic. 2020. Available online: https://www.nccn.org/covid-19/pdf/melanoma.pdf (accessed on 1 June 2021).
- British Association of Dermatologists BSfDS. COVID-19 Skin Cancer Surgery Guidance. 2020. Available online: http://www.bad.org.uk/healthcare-professionals/covid-19 (accessed on 1 June 2021).
- Tee, M.W.; Stewart, C.; Aliessa, S.; Polansky, M.; Shah, K.; Petukhova, T.; Rossi, A.; Lipner, S.R.; Minkis, K. Dermatologic surgery during the COVID-19 pandemic: Experience of a large academic center. J. Am. Acad. Dermatol. 2020, 84, 1094–1096. [Google Scholar] [CrossRef]
- Brochez, L.; Baurain, J.; Del Marmol, V.; Nikkels, A.; Kruse, V.; Sales, F.; Stas, M.; Van Laethem, A.; Garmyn, M. Recommendations for skin cancer consultation and surgery during COVID-19 pandemic. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1876–1878. [Google Scholar] [CrossRef]
- Geskin, L.J.; Trager, M.H.; Aasi, S.Z.; Bickers, D.R.; Carvajal, R.D.; Nghiem, P.; Taback, B.; Zeitouni, N.C.; Samie, F.H. Perspectives on the recommendations for skin cancer management during the COVID-19 pandemic. J. Am. Acad. Dermatol. 2020, 83, 295–296. [Google Scholar] [CrossRef]
- Miranda, B.H.; Hughes, W.R.M.; Pinto-Lopes, R.; Mathur, B.S.; Ramakrishnan, V.V.; Sood, M.K. St Andrew’s COVID-19 surgery safety (StACS) study: Elective plastic surgery, trauma & burns. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 211–222. [Google Scholar]
- Alam, M. Struggling with COVID: Every cancer patient is unique and needs their own plan. J. Am. Acad. Dermatol. 2020, 83, 297–298. [Google Scholar] [CrossRef]
- Baumann, B.C.; MacArthur, K.M.; Brewer, J.D.; Mendenhall, W.M.; Barker, C.A.; Etzkorn, J.R.; Jellinek, N.J.; Scott, J.F.; Gay, H.A.; Baumann, J.C.; et al. Management of primary skin cancer during a pandemic: Multidisciplinary recommendations. Cancer 2020, 126, 3900–3906. [Google Scholar] [CrossRef]
- Rosenbaum, L. The Untold Toll—The Pandemic’s Effects on Patients without Covid-19. N. Engl. J. Med. 2020, 382, 2368–2371. [Google Scholar] [CrossRef]
- Rich, H.; Jones, B.; Malin, I.; Hemington-Gorse, S.J.; Cubitt, J.J. Plastic surgical management of skin cancer patients during the COVID-19 pandemic. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 666–668. [Google Scholar] [CrossRef] [PubMed]
- Rich, H.; O’Neill, T. Major fall in urgent skin cancer referrals during the COVID-19 outbreak. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 670–671. [Google Scholar] [CrossRef]
- Shannon, A.B.; Sharon, C.E.; Straker, R.J., 3rd; Miura, J.T.; Ming, M.E.; Chu, E.Y.; Karakousis, G.C. The impact of the COVID-19 pandemic on the presentation status of newly diagnosed melanoma: A single institution experience. J. Am. Acad. Dermatol. 2021, 84, 1096–1098. [Google Scholar] [CrossRef] [PubMed]
- Capitelli-McMahon, H.; Hurley, A.; Pinder, R.; Matteucci, P.; Totty, J. Characterising non-melanoma skin cancer undergoing surgical management during the COVID-19 pandemic. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 668–670. [Google Scholar] [CrossRef] [PubMed]
- Beyaert, R.; Beaugerie, L.; Van Assche, G.; Brochez, L.; Renauld, J.-C.; Viguier, M.; Cocquyt, V.; Jerusalem, G.; Machiels, J.-P.; Prenen, H.; et al. Cancer risk in immune-mediated inflammatory diseases (IMID). Mol. Cancer 2013, 12, 98. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.-W.; Fung, K.; Austin, P.C.; Kim, S.J.; Singer, L.G.; Baxter, N.N.; Alhusayen, R.; Rochon, P.A. Improved keratinocyte carcinoma outcomes with annual dermatology assessment after solid organ transplantation: Population-based cohort study. Am. J. Transplant. 2018, 19, 522–531. [Google Scholar] [CrossRef]
- Acuna, S.A.; Huang, J.W.; Scott, A.L.; Micic, S.; Daly, C.; Brezden-Masley, C.; Kim, S.J.; Baxter, N.N. Cancer Screening Recommendations for Solid Organ Transplant Recipients: A Systematic Review of Clinical Practice Guidelines. Am. J. Transplant. 2016, 17, 103–114. [Google Scholar] [CrossRef]
- Collins, L.; Quinn, A.; Stasko, T. Skin Cancer and Immunosuppression. Dermatol. Clin. 2018, 37, 83–94. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).