Development and Validation of a Methodology to Measure Exhaled Carbon Dioxide (CO2) and Control Indoor Air Renewal
Abstract
:1. Introduction
2. Materials and Methods
2.1. Measurement of Metabolic CO2
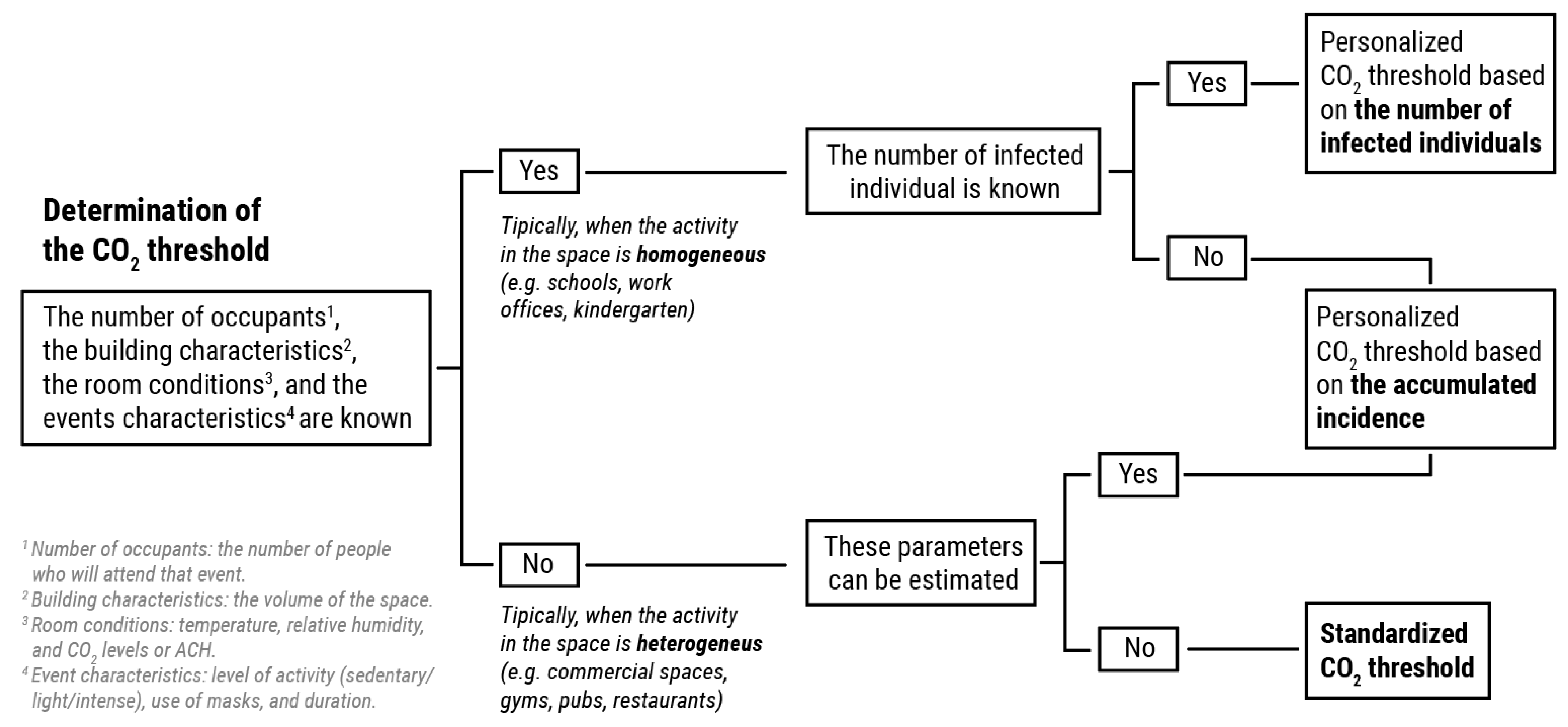
2.2. General Description of the Methodology
2.2.1. Analysis Phase
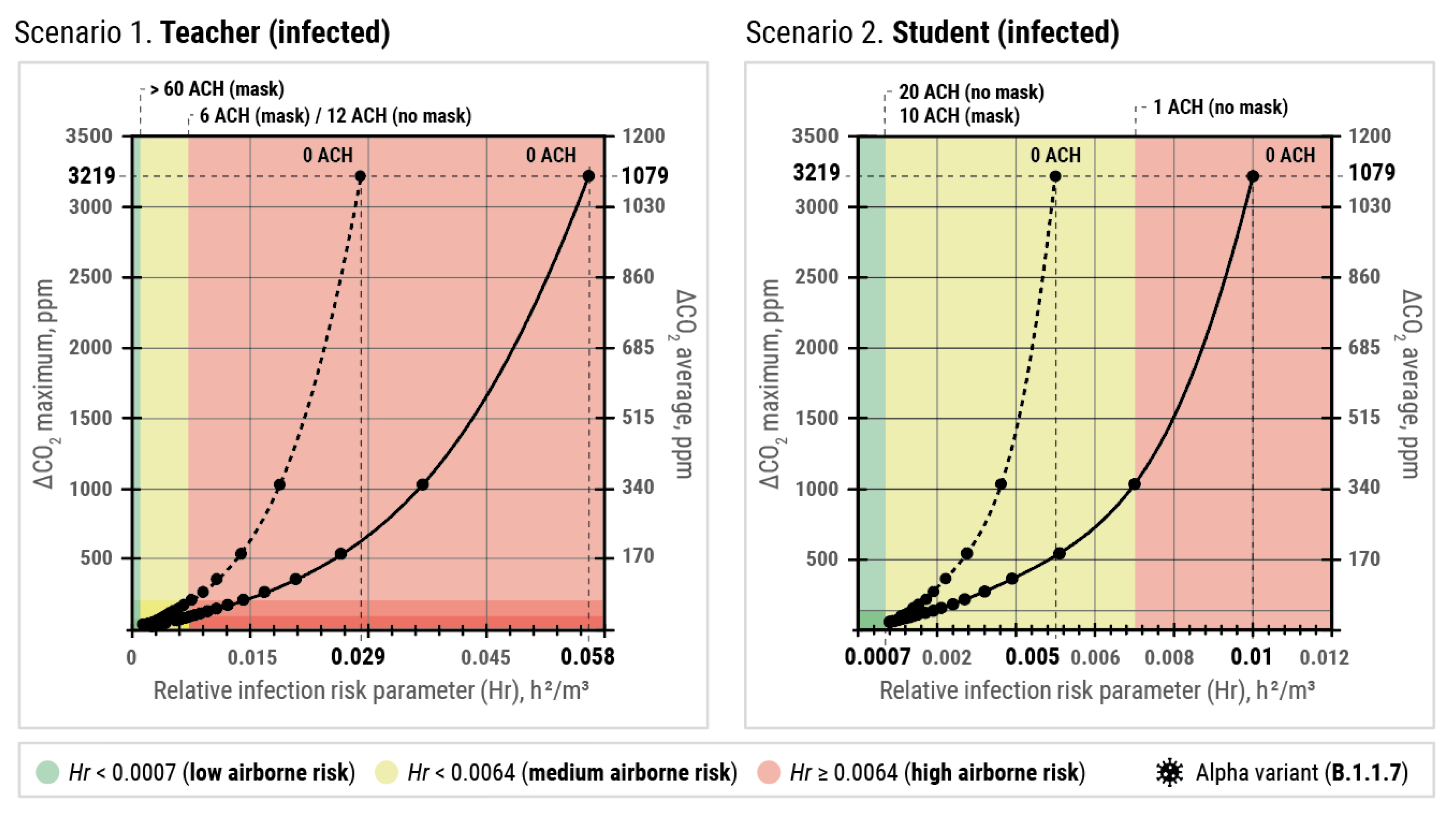
- Scenario 1a. The infected person is the teacher (40 years old) and everyone wears a surgical mask.
- Scenario 1b. The infected person is the teacher (40 years old) and no one wears a mask.
- Scenario 2a. The infected person is a student (18 years old) and everyone wears a surgical mask.
- Scenario 2b. The infected person is a student (18 years old) and no one wears a mask.
- To carry out the statistical estimation, Alpha (B.1.1.7) has been considered the predominant variant. In scenario 1, it has been assumed that the teacher performs a sedentary activity, speaking and emitting aerosols in the 75% percentile of viral exhalation rate from the mean value of 2.0 q·h−1 (~259 quanta/h). In scenario 2, the student performs a sedentary activity, with oral breathing and emitting aerosols in the 75% percentile of viral exhalation rate from the mean value of 2.0 q·h−1 (~49 quanta/h). In both scenarios, the efficiency of surgical masks against aerosol retention has been close to 32.5% (in the exhalation of the infected individual) and 25% (in the inhalation of susceptible individuals).
2.2.2. Diagnosis
2.2.3. Correction
2.2.4. Monitoring, Control, and Surveillance (MCS)
2.3. Description of First Case Space (Cultural Building)
2.4. Description of Second Case Spaces (Commercial Spaces)
3. Results
3.1. First Case: Cultural Building
3.1.1. Analysis: Determining Personalized CO2 Thresholds
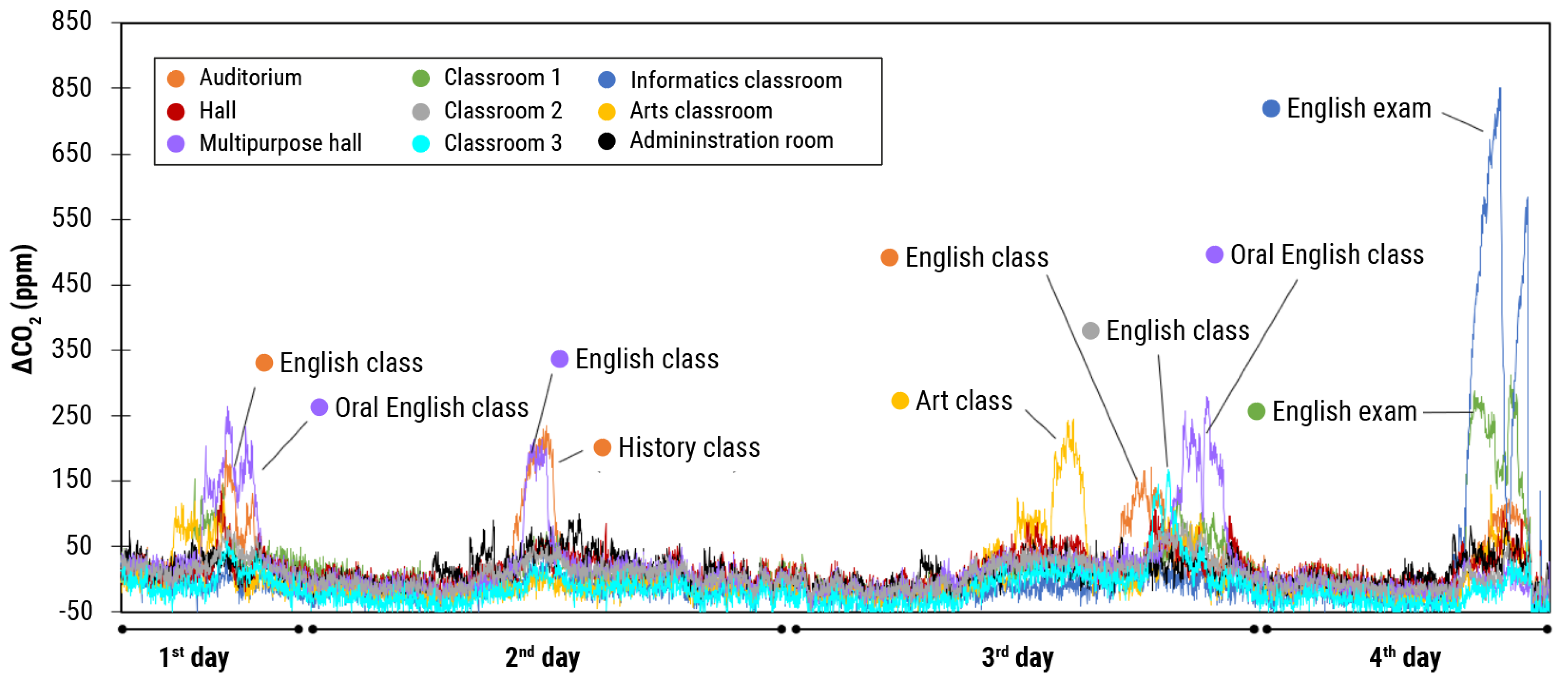
3.1.2. Diagnostic Phase of the Space
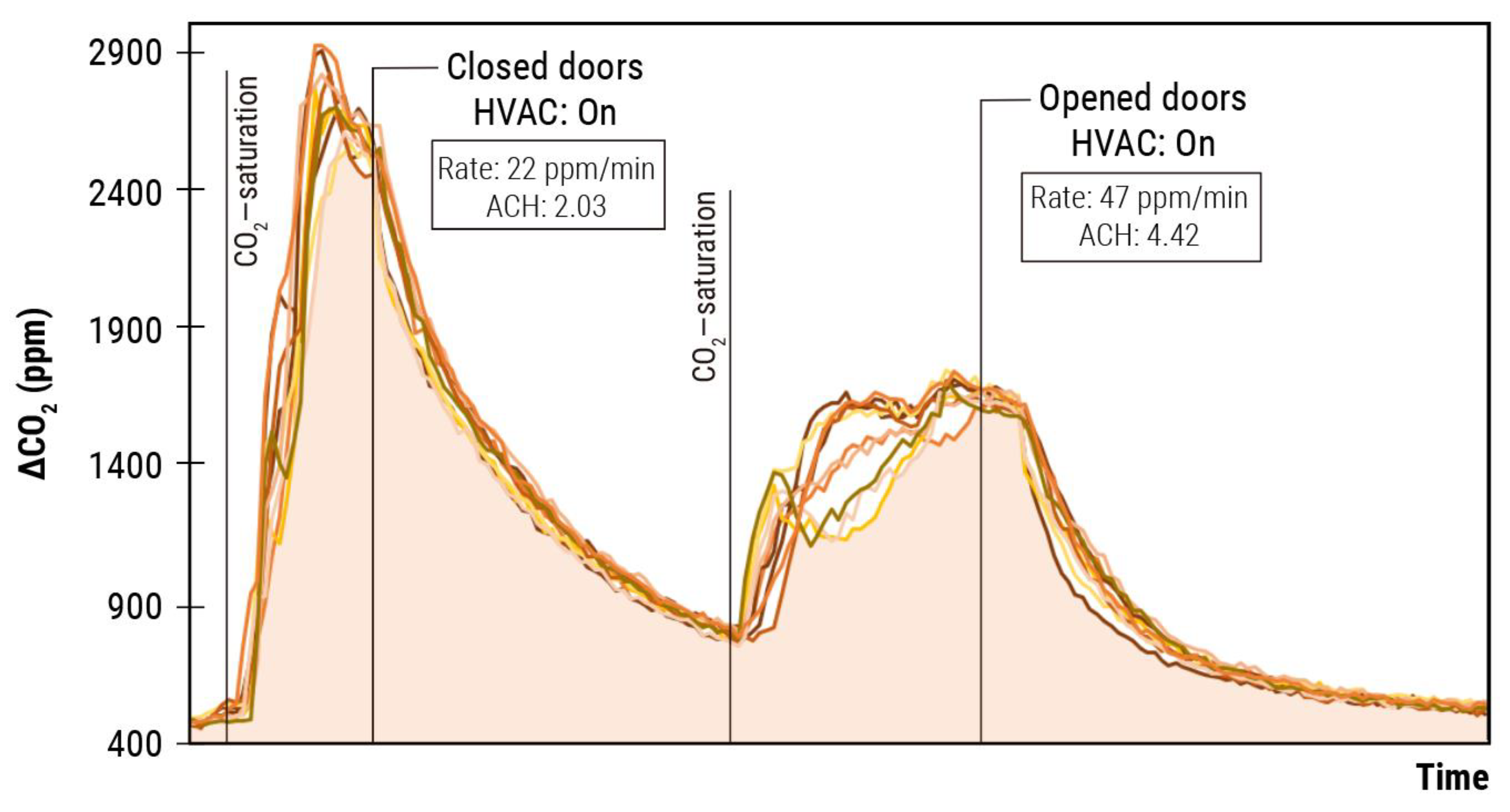
3.1.3. Correction Phase: Improving Ventilation Patterns
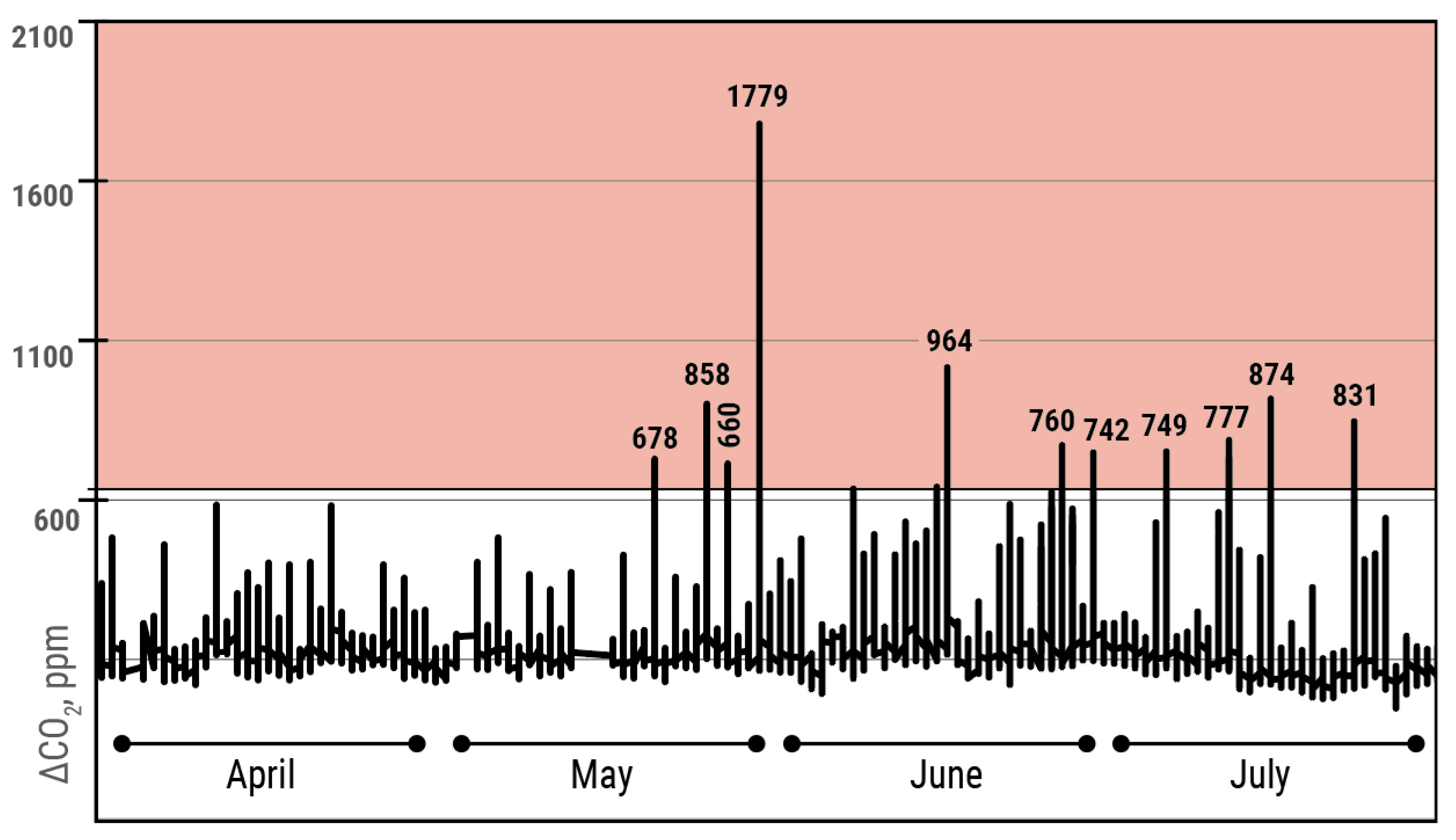
3.1.4. MCS: Monitoring, Control, and Surveillance
3.2. Second Case: Commercial Spaces
3.2.1. Analysis: Determining Standard CO2 Thresholds
3.2.2. Analysis: Determining Standard CO2 Thresholds
3.2.3. Corrective Measure Implementation
3.2.4. MCS Phase and Corrective Measure Validation
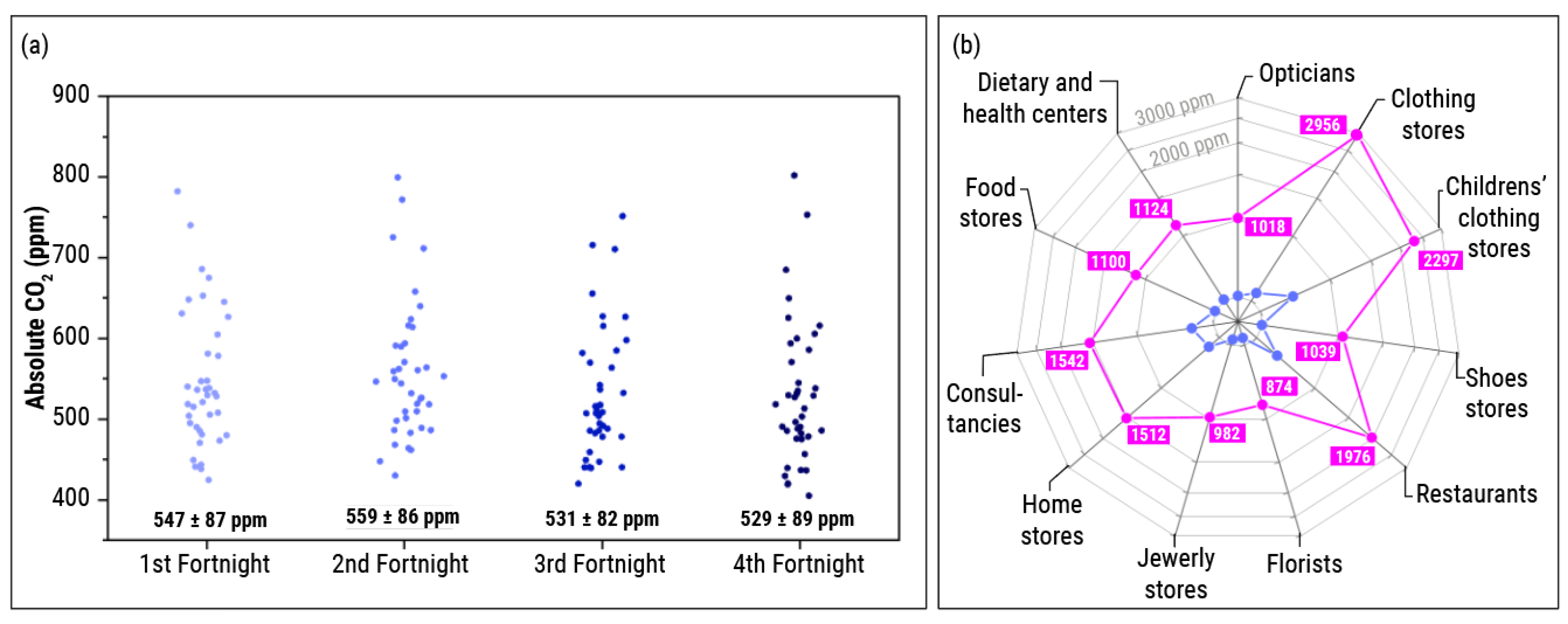
- Retail stores with good starting air quality. Initially, 17 shops showed a renewal of the air appropriate to the architecture of the space and the type of activity carried out. Three cases are shown below as an example.
- (Example 1) In a shoe store, the limit of 800 ppm was not exceeded during the recorded period (Figure 10a). Specifically, it obtained an average CO2 value of 441 ± 42 ppm, reaching a maximum value of 776 ppm.
- (Example 2) A food store was kept below 800 ppm (Figure 10b). Despite the large influx of customers, the levels maintained an average of 454 ± 39 ppm, reaching a maximum value of 782 ppm
- (Example 3) In one of the clothing stores, the maximum established by the scientific community of 800 ppm was not exceeded (Figure 10c). On average, it reached a value of 469 ± 33 ppm, reaching a maximum value of 783 ppm.
- Businesses with improvable air quality that did not implement corrective actions. Of the 23 stores that showed levels above 800 ppm during the first week, only 15 of them did so continuously and with values above 900 ppm. The remaining eight stores were recommended to maximize the frequency of opening doors and windows. This section shows the evolution of CO2 in a business that refused to establish the proposed corrective measures.
- (Example 1) On average, a clothing store reached a value of 709 ± 295 ppm, reaching a maximum of 2956 ppm (Figure 10d).
- (Example 2) A restaurant establishment reached an average value of 589 ± 139 ppm, reaching a maximum value of 1976 ppm (Figure 10e).
- (Example 3) The mean of CO2 in a children’s clothing store was 762 ± 229 ppm, reaching a maximum of 2297 ppm (Figure 10f).
- Spaces with improvable air quality that implemented corrective actions. After implementing the prevention measures (especially the reinforcement of natural ventilation), the reduction of CO2 in the establishments was substantial. Three cases are described below. The values of the first weeks concerning the final weeks are comparable, given that similar trends and averages are observed in the previous section.
- (Example 1) In a clothing shop, the mean of CO2 was reduced from 605 ± 78 ppm (maximum of 1100 ppm) to 529 ± 78 ppm (745 ppm) after trying different measures. The increase in the frequency of door opening (Figure 10g) was more effective in the fourth fortnight. In this period, no values over 800 ppm were registered.
- (Example 2) CO2 levels on average were reduced from 536 ± 89 ppm (maximum of 1001 ppm) to 485 ± 51 ppm (714 ppm) from the third fortnight in a food store, as shown in Figure 10h.
- (Example 3) In a shoe store, the mean of CO2 was reduced from 528 ± 67 ppm (maximum of 946 ppm) to 473 ± 45 ppm (764 ppm). Although, at one point, 800 ppm was exceeded (Figure 10i).
4. Discussion
- Analyzing. In this phase, acceptable CO2 thresholds will be established to reach areas of low risk of transmission. If the activity is homogeneous and the fundamental variables are known, it is possible to approximate the CO2 threshold following the Wells–Riley model [67] modified by Peng and Jimenez [7] to determine the risk of the space. In spaces with heterogeneous activities and/or unknown variables, it will be necessary to apply threshold values that could guarantee reasonable air renewal. Typically, CO2 thresholds have been established in a standard manner, without considering the variables related to the outbreak, the airborne pathogen, the parameters of the event, and the building [71]. However, as proposed in this methodology, the detailed study of the CO2 results can be crucial to interpret the event and the risk of transmission [62,70,76].
- Diagnosing. After training the responsible person, the diagnostic phase was carried out. A first assessment of the shared space is made by placing CO2 meters for a time interval long enough to address the maximum possible casuistry. Usually, 3 or 4 activity days are enough. Ideally, placing more than one CO2 meter will let us know if the measurement represents the space. Additionally, it will bring preliminary, but not definitive, information about how the air renewal occurs in the shared space. After an in-depth analysis of the evolution of CO2 levels in the diagnosis phase, it is necessary to follow up in subsequent days (typically 6 or 7 days) to ensure that the diagnosis is representative of the space. Analyzing ventilation patterns under different boundary conditions can be key to establishing effective measures [56,77,78,79].
- Correcting. Poor air renewal must be identified once an exhaustive analysis of the space has been carried out. After detecting these incidences (CO2 levels exceeding the established threshold), it is necessary to look for the cause of the problem. It is helpful to raise possible hypotheses and try to rule them out to propose efficient corrective measures. Ideally, these proposed measures can be validated by conducting experiments (e.g., saturating with CO2 and analyzing the advantage of each one) or carrying out a detailed follow-up in the monitoring phase. Note that this phase can be performed linearly (e.g., after diagnosis), or it can also be implemented during monitoring if necessary. The results obtained from the validation in 40 retail stores in the center of Zaragoza (Spain) suggest that it is possible to quickly implement measures that favor the renewal of shared air. In this work, opening doors and windows was one of the most straightforward and immediate methods applied in almost any situation, according to previous reports [80,81]. In this sense, other authors suggest that continuous and cross-ventilation is effective to maintain an adequate ventilation in school classrooms [77]. Considering the ease of adopting these measures, it is necessary to start establishing definitive strategies to improve ventilation in indoor spaces.
- MCS. A monitoring and follow-up phase is crucial to warn of any incident where the CO2 limit is exceeded. It is the only strategy that ensures good indoor air quality. It is possible that, in spaces where natural ventilation influences the space air renewal, the CO2 concentration fluctuates depending on the weather. In these cases, it may be necessary to re-implement the correction phase to maintain adequate air renewal. Ideally, an alert system can be valuable for the monitored center, allowing it to prevent the accumulation of CO2 or modulate the capacity and, ultimately, correct the situation.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lewis, B.D. Why the WHO Took Two Years to Say COVID Is Airborne. Nature 2022, 604, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Ruiz de Adana, M.; Jiménez, E.; Jiménez, J.L.; Cruz Minguillon, M.; Ballester, J.; Querol, X.; Grupo de Trabajo Multidisciplinar. Informe Del GTM: Equipos Autónomos Para La Limpieza Del Aire y Sensores Para El Control de La Transmisión de SARS-CoV-2 Por Aerosoles; Ministerio de Ciencia e Innovación: Madrid, Spain, 2021; Available online: https://digital.csic.es/handle/10261/242479 (accessed on 16 December 2022).
- Baselga, M.; Alba, J.J.; Schuhmacher, A.J. Impact of Needle-Point Bipolar Ionization System in the Reduction of Bioaerosols in Collective Transport. Sci. Total Environ. 2023, 855, 158965. [Google Scholar] [CrossRef] [PubMed]
- Licht, S.; Hehir, A.; Trent, S.; Dunlap, D.; Borumand, K.; Wilson, M.; Smith, K. Use of Bipolar Ionization for Disinfection within Airplanes; Boeing: Chicago, IL, USA, 2021. [Google Scholar]
- Liu, D.T.; Philips, K.M.; Speth, M.M.; Besser, G.; Mueller, C.A.; Sedaghat, A.R. Portable HEPA Purifiers to Eliminate Airborne SARS-CoV-2: A Systematic Review. Otolaryngol. Head Neck Surg. 2021, 166, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.; Palop, M.L.; Seseña, S.; Rodríguez, A. Are the Portable Air Cleaners (PAC) Really Effective to Terminate Airborne SARS-CoV-2? Sci. Total Environ. 2021, 785, 147300. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Jimenez, J.L. Exhaled CO2 as a COVID-19 Infection Risk Proxy for Different Indoor Environments and Activities. Environ. Sci. Technol. Lett. 2021, 8, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Rudnick, S.; Milton, D. Risk of Indoor Airborne Infection Transmission Estimated from Carbon Dioxide Concentration. Indoor Air 2003, 13, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Kappelt, N.; Russell, H.S.; Kwiatkowski, S.; Afshari, A.; Johnson, M.S. Correlation of Respiratory Aerosols and Metabolic Carbon Dioxide. Sustainability 2021, 13, 12203. [Google Scholar] [CrossRef]
- Shao, S.; Zhou, D.; He, R.; Li, J.; Zou, S.; Mallery, K.; Kumar, S.; Yang, S.; Hong, J. Risk Assessment of Airborne Transmission of COVID-19 by Asymptomatic Individuals under Different Practical Settings. J. Aerosol Sci. 2021, 151, 105661. [Google Scholar] [CrossRef]
- Fabian, P.; Brain, J.; Houseman, E.; Gern, J.; Milton, D. Origin of Exhaled Breath Particles from Healthy and Human Rhinovirus-Infected Subjects. J. Aerosol Med. Pulm. Drug Deliv. 2011, 24, 137–147. [Google Scholar] [CrossRef]
- Wang, C.C.; Prather, K.A.; Sznitman, J.; Jimenez, J.L.; Lakdawala, S.S.; Tufekci, Z.; Marr, L.C. Airborne Transmission of Respiratory Viruses. Science 2021, 373, eabd9149. [Google Scholar] [CrossRef]
- Johnson, G.R.; Morawska, L.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Chao, C.Y.H.; Wan, M.P.; Li, Y.; Xie, X.; Katoshevski, D.; et al. Modality of Human Expired Aerosol Size Distributions. J. Aerosol Sci. 2011, 42, 839–851. [Google Scholar] [CrossRef]
- Colegio Ingenieros Industriales de Aragón y la Rioja; Ayuntamiento de Zaragoza. Guía de Referencia COVID. 2021. Available online: https://www.zaragoza.es/contenidos/coronavirus/guia-referencia-covid.pdf (accessed on 13 December 2022).
- Cheng, S.Y.; Wang, C.J.; Shen, A.C.T.; Chang, S.C. How to Safely Reopen Colleges and Universities During COVID-19: Experiences From Taiwan. Ann. Intern. Med. 2020, 173, 638–641. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, P.; Zupin, L.; Licen, S.; Torboli, V.; Semeraro, S.; Cozzutto, S.; Palmisani, J.; Di Gilio, A.; de Gennaro, G.; Fontana, F.; et al. Molecular Detection of SARS-CoV-2 from Indoor Air Samples in Environmental Monitoring Needs Adequate Temporal Coverage and Infectivity Assessment. Environ. Res. 2021, 198, 111200. [Google Scholar] [CrossRef] [PubMed]
- Baselga, M.; Güemes, A.; Alba, J.J.; Schuhmacher, A.J. SARS-CoV-2 Droplet and Airborne Transmission Heterogeneity. J. Clin. Med. 2022, 11, 2607. [Google Scholar] [CrossRef] [PubMed]
- Chan, V.W.M.; So, S.Y.C.; Chen, J.H.K.; Yip, C.C.Y.; Chan, K.H.; Chu, H.; Chung, T.W.H.; Sridhar, S.; To, K.K.W.; Chan, J.F.W.; et al. Air and Environmental Sampling for SARS-CoV-2 around Hospitalized Patients with Coronavirus Disease 2019 (COVID-19). Infect. Control. Hosp. Epidemiol. 2020, 41, 1258–1265. [Google Scholar]
- Chia, P.Y.; Coleman, K.K.; Tan, Y.K.; Ong, S.W.X.; Gum, M.; Lau, S.K.; Lim, X.F.; Lim, A.S.; Sutjipto, S.; Lee, P.H.; et al. Detection of Air and Surface Contamination by SARS-CoV-2 in Hospital Rooms of Infected Patients. Nat. Commun. 2020, 11, 2800. [Google Scholar] [CrossRef]
- Department of Infectious Disease, Imperial College London (London, UK). Evaluation of Sars-Cov-2 Air Contamination in Hospitals with Coriolis Air Sampler. 2020. Available online: https://www.bertin-instruments.com/wp-content/uploads/2020/08/CORM-026-039-B-SARS-CoV-2-in-hospitals-1.pdf (accessed on 13 December 2023).
- Ding, Z.; Qian, H.; Xu, B.; Huang, Y.; Miao, T.; Yen, H.L.; Xiao, S.; Cui, L.; Wu, X.; Shao, W.; et al. Toilets Dominate Environmental Detection of Severe Acute Respiratory Syndrome Coronavirus 2 in a Hospital. Sci. Total Environ. 2021, 753, 141710. [Google Scholar] [CrossRef]
- Dumont-Leblond, N.; Veillette, M.; Mubareka, S.; Yip, L.; Longtin, Y.; Jouvet, P.; Paquet Bolduc, B.; Godbout, S.; Kobinger, G.; McGeer, A.; et al. Low Incidence of Airborne SARS-CoV-2 in Acute Care Hospital Rooms with Optimized Ventilation. Emerg. Microbes Infect. 2020, 9, 2597–2605. [Google Scholar] [CrossRef]
- Gomes, P.; Gonçalves, J.; Isabel, A.; Lopes, B.; Esteves, N.A.; Emanuel, G.; Bamba, E.; Maria, S.; Branco, P.T.B.S.; Soares, R.R.G.; et al. Evidence of Air and Surface Contamination with SARS-CoV-2 in a Major Hospital in Portugal. Int. J. Environ. Res. Public Health 2022, 19, 525. [Google Scholar]
- Kenarkoohi, A.; Noorimotlagh, Z.; Falahi, S.; Amarloei, A.; Abbas, S. Hospital Indoor Air Quality Monitoring for the Detection of SARS-CoV-2 (COVID-19) Virus. Sci. Total Envion. 2020, 748, 141324. [Google Scholar] [CrossRef]
- Lednicky, J.A.; Shankar, S.N.; Elbadry, M.A.; Gibson, J.C.; Alam, M.M.; Stephenson, C.J.; Eiguren-Fernandez, A.; Glenn Morris, J.; Mavian, C.N.; Salemi, M.; et al. Collection of SARS-CoV-2 Virus from the Air of a Clinic within a University Student Health Care Center and Analyses of the Viral Genomic Sequence. Aerosol Air Qual. Res. 2020, 20, 1167–1171. [Google Scholar] [CrossRef] [PubMed]
- Mallach, G.; Kasloff, S.B.; Kovesi, T.; Kumar, A.; Kulka, R.; Krishnan, J.; Robert, B.; McGuinty, M.; den Otter-Moore, S.; Yazji, B.; et al. Aerosol SARS-CoV-2 in Hospitals and Long-Term Care Homes during the COVID-19 Pandemic. PLoS ONE 2021, 16, e0258151. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.; Rickard, H.; Stevenson, D.; Aranega-Bou, P.; Pitman, J.; Crook, A.; Davies, K.; Spencer, A.; Burton, C.; Easterbrook, L.; et al. Detection of SARS-CoV-2 within the Healthcare Environment: A Multi-Centre Study Conducted during the First Wave of the COVID-19 Outbreak in England. J. Hosp. Infect. 2021, 108, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Nissen, K.; Krambrich, J.; Akaberi, D.; Hoffman, T.; Ling, J.; Lundkvist, Å.; Svensson, L.; Salaneck, E. Long-Distance Airborne Dispersal of SARS-CoV-2 in COVID-19 Wards. Sci. Rep. 2020, 10, 19589. [Google Scholar] [CrossRef] [PubMed]
- Santarpia, J.L.; Rivera, D.N.; Herrera, V.L.; Morwitzer, M.J.; Creager, H.M.; Santarpia, G.W.; Crown, K.K.; Brett-Major, D.M.; Schnaubelt, E.R.; Broadhurst, M.J.; et al. Aerosol and Surface Contamination of SARS-CoV-2 Observed in Quarantine and Isolation Care. Sci. Rep. 2020, 10, 12732. [Google Scholar] [CrossRef] [PubMed]
- Winslow, R.L.; Zhou, J.; Windle, E.F.; Nur, I.; Lall, R.; Ji, C.; Millar, J.E.; Dark, P.; Naisbitt, J.; Simonds, A.; et al. SARS-CoV-2 Environmental Contamination from Hospitalised COVID-19 Patients Receiving Aerosol Generating Procedures. Thorax 2021, 77, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic Analysis of SARS-CoV-2 in Two Wuhan Hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef]
- Stern, R.A.; Koutrakis, P.; Martins, M.A.G.; Lemos, B.; Dowd, S.E.; Sunderland, E.M.; Garshick, E. Characterization of Hospital Airborne SARS-CoV-2. Respir. Res. 2021, 22, 1–8. [Google Scholar] [CrossRef]
- Ma, J.; Qi, X.; Chen, H.; Li, X.; Zhang, Z.; Wang, H.; Sun, L.; Zhang, L.; Guo, J.; Morawska, L.; et al. Exhaled Breath Is a Significant Source of SARS-CoV-2 Emission. medRxiv 2020, arXiv:2020.05.31.20115154. [Google Scholar] [CrossRef]
- Styczynski, A.; Hemlock, C.; Hoque, K.I.; Verma, R.; LeBoa, C.; Bhuiyan, M.O.F.; Nag, A.; Harun, M.G.D.; Amin, M.B.; Andrews, J.R. Ventilation and Detection of Airborne SARS-CoV-2: Elucidating High-Risk Spaces in Naturally Ventilated Healthcare Settings. medRxiv 2021, arXiv:2021.06.30.21258984. [Google Scholar]
- Song, Z.G.; Chen, Y.M.; Wu, F.; Xu, L.; Wang, B.F.; Shi, L.; Chen, X.; Dai, F.H.; She, J.L.; Chen, J.M.; et al. Identifying the Risk of SARS-CoV-2 Infection and Environmental Monitoring in Airborne Infectious Isolation Rooms (AIIRs). Virol. Sin. 2020, 35, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Moreno, T.; Pintó, R.M.; Bosch, A.; Moreno, N.; Alastuey, A.; Minguillón, M.C.; Anfruns-Estrada, E.; Guix, S.; Fuentes, C.; Buonanno, G.; et al. Tracing Surface and Airborne SARS-CoV-2 RNA inside Public Buses and Subway Trains. Environ. Int. 2021, 147, 106326. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.G.; Branco, P.T.B.S.; Soares, R.R.G.; Mesquita, J.R.; Sousa, S.I.V. SARS-CoV-2 air sampling: A systematic review on the methodologies for detection and infectivity. Indoor Air 2022, 32, e13083. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.M.; Ji, J.J.; Jiang, S.; Xiao, Y.Q.; Zhang, R.L.; Huang, D.N.; Liu, H.; Yu, S.Y. Detecting Environmental Contamination of Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in Isolation Wards and Fever Clinics*. Biomed. Environ. Sci. 2020, 33, 943–947. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.J.; Otter, J.A.; Price, J.R.; Cimpeanu, C.; Garcia, M.; Kinross, J.; Boshier, P.R.; Mason, S.; Bolt, F.; Alison, H.; et al. Investigating SARS-CoV-2 Surface and Air Contamination in an Acute Healthcare 2 Setting during the Peak of the COVID-19 Pandemic in London. medRxiv 2020, arXiv:2020.05. 24.20110346. [Google Scholar]
- Lei, H.; Ye, F.; Liu, X.; Huang, Z.; Ling, S.; Jiang, Z.; Cheng, J.; Huang, X.; Wu, Q.; Wu, S.; et al. SARS-CoV-2 Environmental Contamination Associated with Persistently Infected COVID-19 Patients. Influenza Other Respir. Viruses 2020, 14, 688–699. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Scientific Brief: SARS-CoV-2 Transmission. Available online: https://stacks.cdc.gov/view/cdc/105949 (accessed on 13 December 2022).
- Shim, E.; Tariq, A.; Choi, W.; Lee, Y.; Chowell, G. Transmission Potential and Severity of COVID-19 in South Korea. Int. J. Infect. Dis. 2020, 93, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kim, Y.M.; Yi, S.; Lee, S.; Na, B.J.; Kim, C.B.; Kim, J.; Kim, H.S.; Kim, Y.B.; Park, Y.; et al. Coronavirus Disease Outbreak in Call Center, South Korea. Emerg. Infect. Dis. 2020, 26, 1666–1670. [Google Scholar] [CrossRef]
- Fontanet, A.; Tondeur, L.; Madec, Y.; Grant, R.; Besombes, C.; Jolly, N.; Pellerin, S.F.; Ungeheuer, M.-N.; Cailleau, I.; Kuhmel, L.; et al. Cluster of COVID-19 in Northern France: A Retrospective Closed Cohort Study. SSRN Electron. J. 2020, 1–22. [Google Scholar] [CrossRef]
- MOH News Highlights. 2020. Available online: http://web.archive.org/web/20200420074230/https://www.moh.gov.sg/news-highlights/details/16-more-cases-discharged-35-new-cases-of-covid-19-infection-confirmed (accessed on 13 December 2023).
- Cai, J.; Sun, W.; Huang, J.; Gamber, M.; Wu, J.; He, G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg. Infect. Dis. 2020, 26, 1343–1345. [Google Scholar] [CrossRef]
- Chu, J.; Yang, N.; Wei, Y.; Yue, H.; Zhang, F.; Zhao, J.; He, L.; Sheng, G.; Chen, P.; Li, G.; et al. Clinical Characteristics of 54 Medical Staff with COVID-19: A Retrospective Study in a Single Center in Wuhan, China. J. Med. Virol. 2020, 92, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Sim, W. The Straits Times. Japan Identifies 15 Clusters as COVID-19 Cases. 2020. Available online: http://web.archive.org/web/20200420073241/https://www.straitstimes.com/asia/east-asia/japan-identifies-15-clusters-as-covid-19-cases-mount (accessed on 13 December 2023).
- Aljazeera after One Infected 16 at Berlin Nightclub, Coronavirus Fears Grow. 2020. Available online: http://web.archive.org/web/20200420071353/https://www.aljazeera.com/news/2020/03/infected-16-berlin-nightclub-coronavirus-fears-grow-200310132859234.html (accessed on 13 December 2023).
- Marcelo, P.; O’brien, M. Cluster of Coronavirus Cases Tied to U.S. Biotech Meeting. 2020. Available online: http://web.archive.org/web/20200401222019/https://time.com/5801554/coronavirus-cluster-biotech-biogen-boston-mbridge/ (accessed on 13 December 2023).
- Orban, A. 26 Passengers Tested Positive for COVID-19 on an Emirates Flight to Hong Kong. Aviation 24 Website. 2020. Available online: https://www.aviation24.be/airlines/emirates-airline/26-passengers-tested-positive-on-an-emirates-flight-to-hong-kong/ (accessed on 13 December 2023).
- Shen, Y.; Li, C.; Dong, H.; Wang, Z.; Martinez, L.; Sun, Z.; Handel, A.; Chen, Z.; Chen, E.; Ebell, M.H.; et al. Community Outbreak Investigation of SARS-CoV-2 Transmission among Bus Riders in Eastern China. JAMA Intern. Med. 2020, 180, 1665–1671. [Google Scholar] [CrossRef] [PubMed]
- Zauzmer, J. ‘Take It Very Seriously’: Pastor at Arkansas Church Where 34 People Came down with Coronavirus Sends a Warning. The Washington Pos. 2020. Available online: http://web.archive.org/web/20200420073657/https://www.washingtonpost.com/religion/2020/03/24/pastor-arkansas-church-coronavirus-warning-greers-ferry/ (accessed on 13 December 2023).
- McKie, R. Did Singing Together Spread Coronavirus to Four Choirs? The Observer. 2020. Available online: https://www.theguardian.com/world/2020/may/17/did-singing-together-spread-coronavirus-to-four-choirs (accessed on 13 December 2023).
- Singapore Upcode Academy. Dashboard of the COVID-19 Virus Outbreak in Singapore. 2021. Available online: http://web.archive.org/web/20200420073524/https://www.againstcovid19.com/singapore?start=21-01-2020&end=20-04-2020 (accessed on 13 December 2023).
- Adam, D.C.; Wu, P.; Wong, J.Y.; Lau, E.H.Y.; Tsang, T.K.; Cauchemez, S.; Leung, G.M.; Cowling, B.J. Clustering and Superspreading Potential of SARS-CoV-2 Infections in Hong Kong. Nat. Med. 2020, 26, 1714–1719. [Google Scholar] [CrossRef] [PubMed]
- DW News. Coronavirus: German Slaughterhouse Outbreak Crosses. 2020. Available online: https://www.dw.com/en/coronavirus-german-slaughterhouse-outbreak-crosses-1000/a-53883372 (accessed on 13 December 2023).
- Cannon, A. Spike in COVID-19 Cases in Iowa Packing Plants a Big Part of 389 New Cases, State’s Largest Single-Day Increase. Des Moines Register. 2020. Available online: https://eu.desmoinesregister.com/story/news/2020/04/19/coronavirus-iowa-largest-single-day-increase-iowa-covid-19-cases-tied-meatpacking-plants/5162127002/ (accessed on 13 December 2023).
- Adebayo, B. A Worker Infected 533 Others with Coronavirus at a Factory in Ghana, President Says. 2020. Available online: https://edition.cnn.com/2020/05/11/africa/ghana-factory-coronavirus-infection-intl/index.html (accessed on 13 December 2023).
- Halliday, J. Over 450 COVID-19 Cases Reported at Food Factories in England and Wales. The Guardian. 2020. Available online: https://www.theguardian.com/uk-news/2020/jun/25/over-450-covid-19-cases-reported-at-food-factories-in-england-and-wales (accessed on 13 December 2023).
- Sneppen, K.; Taylor, R.J.; Simonsen, L. Impact of Superspreaders on Dissemination and Mitigation of COVID-19. medRxiv 2020, arXiv:2020.05.17.2010474. [Google Scholar]
- Querol, X.; Alastuey, A.; Moreno, N.; Minguillón, M.C.; Moreno, T.; Karanasiou, A.; Jimenez, J.L.; Li, Y.; Morguí, J.A.; Felisi, J.M. How Can Ventilation Be Improved on Public Transportation Buses? Insights from CO2 Measurements. Environ. Res. 2022, 205, 112451. [Google Scholar] [CrossRef]
- Woodward, H.; Fan, S.; Bhagat, R.K.; Dadonau, M.; Wykes, M.D.; Martin, E.; Hama, S.; Tiwari, A.; Dalziel, S.B.; Jones, R.L.; et al. Air Flow Experiments on a Train Carriage—Towards Understanding the Risk of Airborne Transmission. Atmosphere 2021, 12, 1267. [Google Scholar] [CrossRef]
- Salthammer, T.; Fauck, C.; Omelan, A.; Wientzek, S.; Uhde, E. Time and Spatially Resolved Tracking of the Air Quality in Local Public Transport. Sci. Rep. 2022, 12, 3262. [Google Scholar] [CrossRef]
- Baselga, M.; Alba, J.J.; Schuhmacher, A.J. The Control of Metabolic CO2 in Public Transport as a Strategy to Reduce the Transmission of Respiratory Infectious Diseases. Int. J. Environ. Res. Public Health 2022, 19, 6605. [Google Scholar] [CrossRef]
- Bazant, M.Z.; Kodio, O.; Cohen, A.E.; Khan, K.; Gu, Z.; Bush, J.W.M. Monitoring Carbon Dioxide to Quantify the Risk of Indoor Airborne Transmission of COVID-19. Flow 2021, 1, E10. [Google Scholar] [CrossRef]
- Chillon, S.A.; Millan, M.; Aramendia, I.; Fernandez-Gamiz, U.; Zulueta, E.; Mendaza-Sagastizabal, X. Natural Ventilation Characterization in a Classroom under Different Scenarios. Int. J. Environ. Res. Public Health 2021, 18, 5425. [Google Scholar] [CrossRef]
- Zhang, D.; Ding, E.; Bluyssen, P.M. Guidance to Assess Ventilation Performance of a Classroom Based on CO2 Monitoring. Indoor Built Environ. 2022, 31, 1107–1126. [Google Scholar] [CrossRef]
- McNeill, V.F.; Corsi, R.; Huffman, J.A.; King, C.; Klein, R.; Lamore, M.; Maeng, D.Y.; Miller, S.L.; Lee Ng, N.; Olsiewski, P.; et al. Room-Level Ventilation in Schools and Universities. Atmos. Environ. X 2022, 13, 100152. [Google Scholar] [CrossRef] [PubMed]
- Avella, F.; Gupta, A.; Peretti, C.; Fulici, G.; Verdi, L.; Belleri, A.; Babich, F. Low-Invasive CO2-Based Visual Alerting Systems to Manage Natural Ventilation and Improve IAQ in Historic School Buildings. Heritage 2021, 4, 3442–3468. [Google Scholar] [CrossRef]
- Zivelonghi, A.; Lai, M. Mitigating Aerosol Infection Risk in School Buildings: The Role of Natural Ventilation, Volume, Occupancy and CO2 Monitoring. Build. Environ. 2021, 204, 108139. [Google Scholar] [CrossRef]
- GOV.UK. All Schools to Receive Carbon Dioxide Monitors. Available online: https://www.gov.uk/government/news/allschools-to-receive-carbon-dioxide-monitors (accessed on 13 December 2023).
- Dutch News. All Classrooms to Get a CO2 Meter as Part of Ventilation Package. 2022. Available online: https://www.dutchnews.nl/news/2022/02/all-classrooms-to-get-aco2-meter-as-part-of-ventilation-package/ (accessed on 13 December 2023).
- The White House. Biden Administration Launches Effort to Improve Ventilation and Reduce the Spread of COVID-19 in Buildings. Available online: https://www.whitehouse.gov/briefing-room/statements-releases/2022/03/17/fact-sheet-biden-administration-launches-effort-to-improve-ventilation-and-reduce-the-spread-of-covid-19-in-buildings/#:~:text=Today%20the%20Administration%20is%20launching,their%20buildings%20and%20reduce%20the (accessed on 13 December 2023).
- Aireamos. Aireamos. Available online: https://www.aireamos.org/ (accessed on 13 December 2023).
- Campano-Laborda, M.A.; Domínguez-Amarillo, D.; Acosta-García, J.; Fernández-Agüera, J.; Bustamante-Rojas, P.; Sendra-Salas, J.; Jiménez-Palacios, J.L.; Velarde-Rodríguez, I.; Acosta-García, I.; Bustamante-Rojas, P. COVID Risk Airborne; Universidad de Sevilla: Sevilla, Spain, 2021. [Google Scholar]
- Wells, W.F. Airborne Contagion and Air Hygiene: An Ecological Study of Droplet Infections; Commonwealth Fund: New York, NY, USA, 1955. [Google Scholar]
- Buonanno, G.; Morawska, L.; Stabile, L. Quantitative Assessment of the Risk of Airborne Transmission of SARS-CoV-2 Infection: Prospective and Retrospective Applications. Environ. Int. 2020, 145, 106112. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Rojas, A.L.P.; Kropff, E.; Bahnfleth, W.; Buonanno, G.; Dancer, S.J.; Kurnitski, J.; Li, Y.; Loomans, M.G.L.C.; Marr, L.C.; et al. Practical Indicators for Risk of Airborne Transmission in Shared Indoor Environments and Their Application to COVID-19 Outbreaks. Environ. Sci. Technol. 2022, 56, 1125–1137. [Google Scholar] [CrossRef]
- Rodríguez, D.; Urbieta, I.R.; Velasco, Á.; Campano-Laborda, M.Á.; Jiménez, E. Assessment of Indoor Air Quality and Risk of COVID-19 Infection in Spanish Secondary School and University Classrooms. Build. Environ. 2022, 226, 109717. [Google Scholar] [CrossRef]
- Ahmed Abdul–Wahab, S.A.; En, S.C.F.; Elkamel, A.; Ahmadi, L.; Yetilmezsoy, K. A Review of Standards and Guidelines Set by International Bodies for the Parameters of Indoor Air Quality. Atmos. Pollut. Res. 2015, 6, 751–767. [Google Scholar] [CrossRef]




| Characteristics | Aranet 4 Pro | Signos (SiO2) |
|---|---|---|
| CO2 measurement | <9999 ppm (±50 ppm) | <5000 ppm (±50 ppm) |
| Temperature measurement | 0–50 °C (±0.3 °C) | −60–80 °C (±0.2 °C) |
| Humidity measurement | 0–85% (±3%) | 0–95% (±2%) |
| Atmospheric pressure | 0.3–1.1 atm (±0.003 atm) | 0.3–1.1 atm (±0.003 atm) |
| Sensor | N-DIR | N-DIR |
| Sampling frequency | 1 min | 11 min |
| Transmission | Bluetooth (−12–4 dBm) | LoRa |
| Dimensions/weight | 70 × 70 × 24 mm/104 g | 100 × 100 × 23 mm/170 g |
| (a) Estimation Considering that One Occupant is Infected | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixedvariables | Hypothetical Variables | Calculated Variables | |||||||||
| Scenario 1: Teacher (Infected) | Scenario 2: Student (Infected) | ||||||||||
| Location | Occupants, pax | Duration min | Scenario | ∆CO2 mean -max., ppm | AR, % | H, h2·pax/m3 | Hr, h2/m3 | ∆CO2 mean -max., ppm | AR, % | H, h2·pax/m3 | Hr, h2/m3 |
| Classroom 1 (330 m3) | 5 | 90 | (a) Surgical masks | 90–196 | 2.8 | 0.0175 | 0.0064 | 180–540 | 0.9 | 0.0055 | 0.006 |
| (b) No masks | 38–65 | 2.8 | 0.0174 | 0.0064 | 180–540 | 1.8 | 0.0110 | 0.0064 | |||
| 5 | 180 | (a) Surgical masks | 38–60 | 2.8 | 0.0174 | 0.0063 | 359–1073 | 4.4 | 0.0152 | 0.0055 | |
| (b) No masks | 17–26 | 2.8 | 0.0172 | 0.0064 | 105–273 | 4.9 | 0.0172 | 0.0063 | |||
| 10 | 90 | (a) Surgical masks | 181–393 | 2.8 | 0.0395 | 0.0064 | 361–1081 | 0.9 | 0.0124 | 0.002 | |
| (b) No masks | 77–131 | 2.8 | 0.0390 | 0.0064 | 361–1081 | 1.8 | 0.0248 | 0.004 | |||
| 10 | 180 | (a) Surgical masks | 76–121 | 2.8 | 0.0392 | 0.0063 | 719–2146 | 2.8 | 0.0342 | 0.0055 | |
| (b) No masks | 36–55 | 2.8 | 0.0402 | 0.0064 | 294–588 | 2.8 | 0.0400 | 0.0065 | |||
| 15 | 90 | (a) Surgical masks | 272–590 | 2.8 | 0.0614 | 0.0064 | 542–1621 | 0.9 | 0.0193 | 0.002 | |
| (b) No masks | 119–205 | 2.8 | 0.0628 | 0.0065 | 542–1621 | 1.8 | 0.0386 | 0.004 | |||
| 15 | 180 | (a) Surgical masks | 114–181 | 2.8 | 0.0610 | 0.0064 | 1079 -3219 | 1.0 | 0.0532 | 0.0055 | |
| (b) No masks | 52–80 | 2.8 | 0.0600 | 0.0063 | 241–882 | 1.9 | 0.0623 | 0.0065 | |||
| (b) Estimation Considering the Cumulative Incidence (434 Persons per 100,000 Citizens) | |||||||||||
| Fixed variables | Hypothetical Variables | Calculated Variables | |||||||||
| Scenario 1: Teacher (Infected) | Scenario 2: Student (Infected) | ||||||||||
| Location | Occupants, pax | Duration min | Scenario | ∆CO2 mean -max., ppm | AR, % | H, h2·pax/m3 | Hr, h2/m3 | ∆CO2 mean -max., ppm | AR, % | H, h2·pax/m3 | Hr, h2/m3 |
| Classroom 1 (330 m3) | 5 | 90 | (a) Surgical masks | 90–196 | 0.1 | 0.0218 | 0.0064 | 180–540 | 0.1 | 0.0069 | 0.0064 |
| (b) No masks | 38–66 | 0.1 | 0.0218 | 0.0064 | 180–540 | 0.1 | 0.0137 | 0.0064 | |||
| 5 | 180 | (a) Surgical masks | 38–60 | 0.1 | 0.0218 | 0.0064 | 359–1073 | 0.1 | 0.0189 | 0.0064 | |
| (b) No masks | 18–27 | 0.1 | 0.0335 | 0.0064 | 105–273 | 0.1 | 0.0214 | 0.0063 | |||
| 10 | 90 | (a) Surgical masks | 181–393 | 0.1 | 0.0437 | 0.0064 | 361–1081 | 0.1 | 0.0138 | 0.0002 | |
| (b) No masks | 77–131 | 0.1 | 0.0428 | 0.0064 | 361–1081 | 0.1 | 0.0275 | 0.0004 | |||
| 10 | 180 | (a) Surgical masks | 76–121 | 0.1 | 0.0433 | 0.0064 | 719–2146 | 0.1 | 0.0379 | 0.0055 | |
| (b) No masks | 36–55 | 0.1 | 0.0440 | 0.0064 | 294–588 | 0.1 | 0.0443 | 0.0064 | |||
| 15 | 90 | (a) Surgical masks | 272–590 | 0.2 | 0.0655 | 0.0064 | 114–181 | 0.2 | 0.0650 | 0.0064 | |
| (b) No masks | 119–201 | 0.2 | 0.0661 | 0.0065 | 54–83 | 0.2 | 0.0667 | 0.0063 | |||
| 15 | 180 | (a) Surgical masks | 114–181 | 0.2 | 0.0206 | 0.0020 | 1079–3219 | 0.2 | 0.0568 | 0.0055 | |
| (b) No masks | 54–83 | 0.2 | 0.0412 | 0.0040 | 418–820 | 0.2 | 0.0642 | 0.0063 | |||
| Known Variables | Calculated Variables | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scenario 1: Teacher (Infected) | Scenario 2: Student (Infected) | ||||||||||||
| Location | Occupants, pax | Duration, min | Mean ∆CO2, ppm | Max. ∆CO2, ppm | Ta, °C | RH, % | Scenario | AR, % | H, h2·pax/m3 | Hr, h2/m3 | AR, % | H, h2·pax/m3 | Hr, h2/m3 |
| Classroom 1 (330 m3) | 10 | 90 | 89 ± 18 | 153 | 23.9 ± 0.7 | 42 ± 2 | (a) Surgical masks | 1.6 | 0.0221 | 0.0036 | 0.3 | 0.0042 | 0.0006 |
| (b) No masks | 3.1 | 0.0437 | 0.0071 | 0.6 | 0.0083 | 0.0013 | |||||||
| 8 | 120 | 76 ± 22 | 140 | 24.0 ± 0.8 | 44 ± 2 | (a) Surgical masks | 2.2 | 0.0236 | 0.0049 | 0.4 | 0.0045 | 0.0009 | |
| (b) No masks | 4.3 | 0.0467 | 0.0098 | 0.8 | 0.0089 | 0.0018 | |||||||
| 18 | 150 | 219 ± 52 | 312 | 23.0 ± 1.3 | 43 ± 4 | (a) Surgical masks | 3.2 | 0.0851 | 0.0073 | 0.6 | 0.0162 | 0.0014 | |
| (b) No masks | 6.2 | 0.1682 | 0.0145 | 1.2 | 0.032 | 0.0027 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baselga, M.; Alba, J.J.; Schuhmacher, A.J. Development and Validation of a Methodology to Measure Exhaled Carbon Dioxide (CO2) and Control Indoor Air Renewal. COVID 2023, 3, 1797-1817. https://doi.org/10.3390/covid3120124
Baselga M, Alba JJ, Schuhmacher AJ. Development and Validation of a Methodology to Measure Exhaled Carbon Dioxide (CO2) and Control Indoor Air Renewal. COVID. 2023; 3(12):1797-1817. https://doi.org/10.3390/covid3120124
Chicago/Turabian StyleBaselga, Marta, Juan J. Alba, and Alberto J. Schuhmacher. 2023. "Development and Validation of a Methodology to Measure Exhaled Carbon Dioxide (CO2) and Control Indoor Air Renewal" COVID 3, no. 12: 1797-1817. https://doi.org/10.3390/covid3120124
APA StyleBaselga, M., Alba, J. J., & Schuhmacher, A. J. (2023). Development and Validation of a Methodology to Measure Exhaled Carbon Dioxide (CO2) and Control Indoor Air Renewal. COVID, 3(12), 1797-1817. https://doi.org/10.3390/covid3120124








