The Two Sides of the COVID-19 Pandemic
Abstract
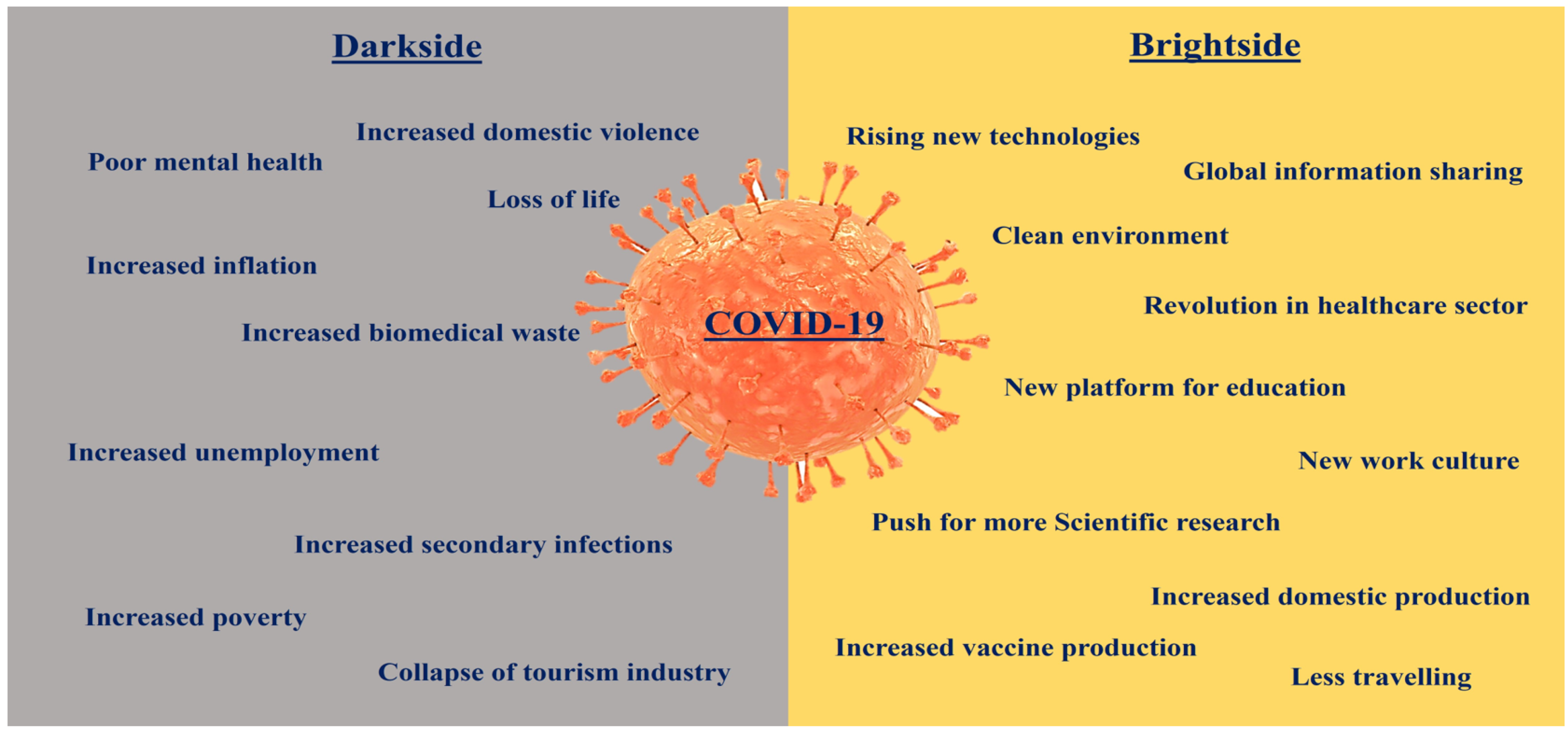
:1. Introduction
2. The Darkside of the COVID-19 Pandemic
3. COVID-19 Impact in Developing Countries and Resources Disparities
4. The Impact of the Pandemic on Healthcare Workers (HCW)
5. The Impact on the Healthcare Sector
5.1. The Arrival of mRNA-Based Vaccine Technology
5.2. Boost for Telemedicine
5.3. Increased Production Capacity of Vaccines
5.4. Increased Production of PPE
5.5. Development of an International Program for Vaccine Development and Production
5.6. Increased Testing Capacity
5.7. More Focus on Improving and Developing Healthcare Infrastructure
6. AI-Based Health Screen, Tracking, and Monitoring
7. New Dimension in Education
8. Cleaner Environment
9. Work-from-Home, a New Work Culture Normal
10. World Sharing of Information Is the Key
11. The World Working Together
12. Learning and Preparedness for Future Pandemics
13. Major Concerns
14. Measures to Prevent or Prepare for Future Pandemics
- Set up more testing facilities throughout the country.
- Set up more local PPE production units.
- Associated authorities should keep stocks of PPE and common medicines.
- Year-round surveillance, monitoring, and prediction (using AI technology) of microbial infections locally and globally.
- Concerned authorities should be made more accountable and transparent.
- States or governments should be forced to share data on microbial infection more accurately, rapidly and in real-time.
- More investment in research related to microbial infection.
- Set up more oxygen-generation plants and increase the number of beds and ventilators.
- Include topics like microbial diseases or infections and ways to prevent infection in primary education to equip the population with the correct information.
- Lifesaving medicines or vaccines should be made accessible to everyone.
- Develop facilities for better distribution and storage of medicine and vaccines.
- Establish more vaccine production facilities spread throughout the world.
- Strict guidelines and procedures to contain the spread of disease; all states and nations should abide by them without exception.
- Use of daily health screening and contact tracing in day-to-day life.
- Facilities for quarantine or self-isolation should be developed and maintained.
- With more strict guidelines for international travel, airlines should ask travelers to provide medical history (infectious diseases) up to the last three months from the journey date.
- International travelers should complete a health screening before leaving the airport.
- More facilities for self-isolation.
- More focus on telemedicine.
- More online education activities.
- More focus on mental health management.
- Better distribution system for food and other life essentials.
- More awareness about zoonotic diseases.
- Teaching healthy habits of hygiene and cleanliness.
15. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. What is a pandemic? J. Infect. Dis. 2009, 200, 1018–1021. [Google Scholar] [CrossRef] [PubMed]
- Piret, J.; Boivin, G. Pandemics Throughout History. Front. Microbiol. 2021, 11, 631736. [Google Scholar] [CrossRef] [PubMed]
- Sampath, S.; Khedr, A.; Qamar, S.; Tekin, A.; Singh, R.; Green, R.; Kashyap, R. Pandemics Throughout the History. Cureus 2021, 13, e18136. [Google Scholar] [CrossRef] [PubMed]
- Ciotti, M.; Ciccozzi, M.; Terrinoni, A.; Jiang, W.C.; Wang, C.B.; Bernardini, S. The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 2020, 57, 365–388. [Google Scholar] [CrossRef] [PubMed]
- Brazeau, N.F.; Verity, R.; Jenks, S.; Fu, H.; Whittaker, C.; Winskill, P.; Dorigatti, I.; Walker, P.G.T.; Riley, S.; Schnekenberg, R.P.; et al. Estimating the COVID-19 infection fatality ratio accounting for seroreversion using statistical modelling. Commun. Med. 2022, 2, 54. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A. Infection fatality rate of COVID-19 inferred from seroprevalence data. Bull. World Health Organ. 2021, 99, 19–33F. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.B.; Cisewski, J.A.; Xu, J.; Anderson, R.N. COVID-19 Mortality Update—United States, 2022. Morb. Mortal. Wkly. Rep. 2023, 72, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Wolff, D.; Nee, S.; Hickey, N.S.; Marschollek, M. Risk factors for COVID-19 severity and fatality: A structured literature review. Infection 2021, 49, 15–28. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Bacon, S.; Evans, S.J.; Bates, C.J.; Rentsch, C.T.; MacKenna, B.; Tomlinson, L.; Walker, A.J.; Schultze, A.; Morton, C.E.; et al. Factors associated with deaths due to COVID-19 versus other causes: Population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg. Health Eur. 2021, 6, 100109. [Google Scholar] [CrossRef]
- Pijls, B.G.; Jolani, S.; Atherley, A.; Derckx, R.T.; Dijkstra, J.I.R.; Franssen, G.H.L.; Hendriks, S.; Richters, A.; Venemans-Jellema, A.; Zalpuri, S.; et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: A meta-analysis of 59 studies. BMJ Open 2021, 11, e044640. [Google Scholar] [CrossRef]
- Chen, Y.; Klein, S.L.; Garibaldi, B.T.; Li, H.; Wu, C.; Osevala, N.M.; Li, T.; Margolick, J.B.; Pawelec, G.; Leng, S.X. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res. Rev. 2021, 65, 101205. [Google Scholar] [CrossRef]
- Shahid, Z.; Kalayanamitra, R.; McClafferty, B.; Kepko, D.; Ramgobin, D.; Patel, R.; Aggarwal, C.S.; Vunnam, R.; Sahu, N.; Bhatt, D.; et al. COVID-19 and Older Adults: What We Know. J. Am. Geriatr. Soc. 2020, 68, 926–929. [Google Scholar] [CrossRef] [PubMed]
- Wise, J. COVID-19: WHO declares end of global health emergency. BMJ 2023, 381, 1041. [Google Scholar] [CrossRef] [PubMed]
- V’kovski, P.; Kratzel, A.; Steiner, S.; Stalder, H.; Thiel, V. Coronavirus biology and replication: Implications for SARS-CoV-2. Nat. Rev. Microbiol. 2021, 19, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.Y.; Zhao, R.; Gao, L.J.; Gao, X.F.; Wang, D.P.; Cao, J.M. SARS-CoV-2: Structure, Biology, and Structure-Based Therapeutics Development. Front. Cell. Infect. Microbiol. 2020, 10, 587269. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.J. Pathogenesis of COVID-19 from a cell biology perspective. Eur. Respir. J. 2020, 55, 2000607. [Google Scholar] [CrossRef]
- Bayati, A.; Kumar, R.; Francis, V.; McPherson, P.S. SARS-CoV-2 infects cells after viral entry via clathrin-mediated endocytosis. J. Biol. Chem. 2021, 296, 100306. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Diana Beltekian, D.; Esteban Ortiz-Ospina, E.; et al. Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 22 November 2023).
- The Lancet Infectious Diseases. COVID-19 vaccine equity and booster doses. Lancet Infect. Dis. 2021, 21, 1193. [Google Scholar] [CrossRef]
- Mallapaty, S. The coronavirus is most deadly if you are older and male—New data reveal the risks. Nature 2020, 585, 16–17. [Google Scholar] [CrossRef]
- Bartik, A.W.; Bertrand, M.; Cullen, Z.; Glaeser, E.L.; Luca, M.; Stanton, C. The impact of COVID-19 on small business outcomes and expectations. Proc. Natl. Acad. Sci. USA 2020, 117, 17656–17666. [Google Scholar] [CrossRef]
- Jain, U. Effect of COVID-19 on the Organs. Cureus 2020, 12, e9540. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Xu, E.; Al-Aly, Z. Risks of mental health outcomes in people with COVID-19: Cohort study. BMJ 2022, 376, e068993. [Google Scholar] [CrossRef] [PubMed]
- Penninx, B.W.J.H.; Benros, M.E.; Klein, R.S.; Vinkers, C.H. How COVID-19 shaped mental health: From infection to pandemic effects. Nat. Med. 2022, 28, 2027–2037. [Google Scholar] [CrossRef] [PubMed]
- Bengoechea, J.A.; Bamford, C.G. SARS-CoV-2, bacterial co-infections, and AMR: The deadly trio in COVID-19? EMBO Mol. Med. 2020, 12, e12560. [Google Scholar] [CrossRef] [PubMed]
- Bahceci, I.; Yildiz, I.E.; Duran, O.F.; Soztanaci, U.S.; Kirdi Harbawi, Z.; Senol, F.F.; Demiral, G. Secondary Bacterial Infection Rates among Patients with COVID-19. Cureus 2022, 14, e22363. [Google Scholar] [CrossRef] [PubMed]
- Hoenigl, M.; Seidel, D.; Sprute, R.; Cunha, C.; Oliverio, M.; Goldman, G.H.; Ibrahim, A.S.; Carvalho, A. COVID-19-associated fungal infections. Nat. Microbiol. 2022, 7, 1127–1140. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, V.; Ahmad, A. New perspective towards therapeutic regimen against SARS-CoV-2 infection. J. Infect. Public Health 2021, 14, 852–862. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Srivastava, V. Application of anti-fungal vaccines as a tool against emerging anti-fungal resistance. Front. Fungal Biol. 2023, 4, 1241539. [Google Scholar] [CrossRef]
- Kawohl, W.; Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 2020, 7, 389–390. [Google Scholar] [CrossRef]
- Gadermann, A.C.; Thomson, K.C.; Richardson, C.G.; Gagné, M.; McAuliffe, C.; Hirani, S.; Jenkins, E. Examining the impacts of the COVID-19 pandemic on family mental health in Canada: Findings from a national cross-sectional study. BMJ Open 2021, 11, e042871. [Google Scholar] [CrossRef]
- Zhang, H. The Influence of the Ongoing COVID-19 Pandemic on Family Violence in China. J. Fam. Violence 2022, 37, 733–743. [Google Scholar] [CrossRef] [PubMed]
- A Look at the Economic Effects of the Pandemic for Children. Available online:https://www.kff.org/coronavirus-covid-19/issue-brief/a-look-at-the-economic-effects-of-the-pandemic-for-children/ (accessed on 15 September 2023).
- Available online: https://www.imf.org/en/Publications/WP/Issues/2022/12/09/Here-Comes-the-Change-The-Role-of-Global-and-Domestic-Factors-in-Post-Pandemic-Inflation-in-525754 (accessed on 15 September 2023).
- Ismail, H.; Marshall, V.D.; Patel, M.; Tariq, M.; Mohammad, R.A. The impact of the COVID-19 pandemic on medical conditions and medication adherence in people with chronic diseases. J. Am. Pharm. Assoc. 2022, 62, 834–839.e1. [Google Scholar] [CrossRef] [PubMed]
- Abbas, J.; Mubeen, R.; Iorember, P.T.; Raza, S.; Mamirkulova, G. Exploring the impact of COVID-19 on tourism: Transformational potential and implications for a sustainable recovery of the travel and leisure industry. Curr. Res. Behav. Sci. 2021, 2, 100033. [Google Scholar] [CrossRef]
- You, S.; Sonne, C.; Ok, Y.S. COVID-19’s unsustainable waste management. Science 2020, 368, 1438. [Google Scholar] [CrossRef] [PubMed]
- Ngoc, S.V.; Nguyen, M.A.; Nguyen, T.L.; Thi, H.V.; Dao, T.L.; Bui, T.M.P.; Hoang, V.T.; Chu, D.T. COVID-19 and environmental health: A systematic analysis for the global burden of biomedical waste by this epidemic. Case Stud. Chem. Environ. Eng. 2022, 6, 100245. [Google Scholar] [CrossRef] [PubMed]
- Jayasinghe, P.A.; Jalilzadeh, H.; Hettiaratchi, P. The Impact of COVID-19 on Waste Infrastructure: Lessons Learned and Opportunities for a Sustainable Future. Int. J. Environ. Res. Public Health 2023, 20, 4310. [Google Scholar] [CrossRef]
- Moosavi, J.; Fathollahi-Fard, A.M.; Dulebenets, M.A. Supply chain disruption during the COVID-19 pandemic: Recognizing potential disruption management strategies. Int. J. Disaster Risk Reduct. 2022, 75, 102983. [Google Scholar] [CrossRef]
- Ndlovu, M.; Matipano, G.; Miliyasi, R. An analysis of the effect of COVID-19 pandemic on wildlife protection in protected areas of Zimbabwe in 2020. Sci. Afr. 2021, 14, e01031. [Google Scholar] [CrossRef]
- Rana, M.S.; Usman, M.M.; Ikram, A.; Salman, M.; Zaidi, S.S.Z.; Umair, M. The negative impact of the COVID-19 Pandemic on immunization and the positive impact on Polio eradication in Pakistan and Afghanistan. J. Infect. 2022, 85, 174–211. [Google Scholar] [CrossRef]
- Available online: https://www.un.org/nl/desa/un-report-finds-covid-19-reversing-decades-progress-poverty-healthcare-and (accessed on 5 October 2023).
- Moyer, J.D.; Verhagen, W.; Mapes, B.; Bohl, D.K.; Xiong, Y.; Yang, V.; McNeil, K.; Solórzano, J.; Irfan, M.; Carter, C.; et al. How many people is the COVID-19 pandemic pushing into poverty? A long-term forecast to 2050 with alternative scenarios. PLoS ONE 2022, 17, e0270846. [Google Scholar] [CrossRef]
- Available online: https://www.unicef.org/press-releases/covid-19-may-push-millions-more-children-child-labour-ilo-and-unicef (accessed on 5 October 2023).
- Karunathilake, K. Positive and negative impacts of COVID-19, an analysis with special reference to challenges on the supply chain in South Asian countries. J. Soc. Econ. Dev. 2021, 23 (Suppl. S3), 568–581. [Google Scholar] [CrossRef] [PubMed]
- Paremoer, L.; Nandi, S.; Serag, H.; Baum, F. COVID-19 pandemic and the social determinants of health. BMJ 2021, 372, n129. [Google Scholar] [CrossRef] [PubMed]
- Romano, S.D.; Blackstock, A.J.; Taylor, E.V.; El Burai Felix, S.; Adjei, S.; Singleton, C.M.; Fuld, J.; Bruce, B.B.; Boehmer, T.K. Trends in Racial and Ethnic Disparities in COVID-19 Hospitalizations, by Region—United States, March-December 2020. Morb. Mortal. Wkly. Rep. 2021, 70, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Etienne, C.F. COVID-19 has revealed a pandemic of inequality. Nat. Med. 2022, 28, 17. [Google Scholar] [CrossRef]
- Younis, I.; Longsheng, C.; Zulfiqar, M.I.; Imran, M.; Shah, S.A.A.; Hussain, M.; Solangi, Y.A. Regional disparities in Preventive measures of COVID-19 pandemic in China. A study from international students’ prior knowledge, perception and vulnerabilities. Environ. Sci. Pollut. Res. Int. 2021, 28, 40355–40370. [Google Scholar] [CrossRef]
- Yang, K.; Qi, H. Research on Health Disparities Related to the COVID-19 Pandemic: A Bibliometric Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1220. [Google Scholar] [CrossRef]
- Arsenault, C.; Gage, A.; Kim, M.K.; Kapoor, N.R.; Akweongo, P.; Amponsah, F.; Aryal, A.; Asai, D.; Awoonor-Williams, J.K.; Ayele, W.; et al. COVID-19 and resilience of healthcare systems in ten countries. Nat. Med. 2022, 28, 1314–1324. [Google Scholar] [CrossRef]
- Boro, E.; Stoll, B. Barriers to COVID-19 Health Products in Low-and Middle-Income Countries during the COVID-19 Pandemic: A Rapid Systematic Review and Evidence Synthesis. Front. Public Health 2022, 10, 928065. [Google Scholar] [CrossRef]
- McMahon, D.E.; Peters, G.A.; Ivers, L.C.; Freeman, E.E. Global resource shortages during COVID-19: Bad news for low-income countries. PLoS Negl. Trop. Dis. 2020, 14, e0008412. [Google Scholar] [CrossRef]
- Burki, T. Global shortage of personal protective equipment. Lancet Infect. Dis. 2020, 20, 785–786. [Google Scholar] [CrossRef]
- Available online: https://www.who.int/news/item/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed on 21 November 2023).
- Alshamrani, M.M.; El-Saed, A.; Al Zunitan, M.; Almulhem, R.; Almohrij, S. Risk of COVID-19 morbidity and mortality among healthcare workers working in a Large Tertiary Care Hospital. Int. J. Infect. Dis. 2021, 109, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Deng, X.; Ryan, I.; Zhang, K.; Zhang, W.; Oghaghare, E.; Gayle, D.B.; Shaw, B. COVID-19 Symptoms and Deaths among Healthcare Workers, United States. Emerg. Infect. Dis. 2022, 28, 1624–1641. [Google Scholar] [CrossRef] [PubMed]
- Vera-Alanis, Y.; Aranda-Sanchez, D.; Cano-Verdugo, G.; Gonzalez-Angulo, P.; Rueda-Sanchez, C.B.; Rojas-Martinez, A. Nursing Staff Mortality during the COVID-19 Pandemic, Scoping Review. SAGE Open Nurs. 2022, 8, 23779608221119130. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zhao, Z.; Zhang, H.; Zhu, Y.; Xi, Z.; Xiang, K. Workplace violence against healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2023, 30, 74838–74852. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Dhamija, S.; Patil, J.; Chaudhari, B. Impact of COVID-19 pandemic on healthcare workers. Ind. Psychiatry J. 2021, 30 (Suppl. S1), S282–S284. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Machado, F.; Kwizera, A.; Papazian, L.; Moss, M.; Azoulay, É.; Herridge, M. COVID-19: A heavy toll on health-care workers. Lancet Respir. Med. 2021, 9, 226–228. [Google Scholar] [CrossRef]
- Hall, H. The effect of the COVID-19 pandemic on healthcare workers’ mental health. JAAPA 2020, 33, 45–48. [Google Scholar] [CrossRef]
- Shaukat, N.; Ali, D.M.; Razzak, J. Physical and mental health impacts of COVID-19 on healthcare workers: A scoping review. Int. J. Emerg. Med. 2020, 13, 40. [Google Scholar] [CrossRef]
- Pardi, N.; Hogan, M.J.; Porter, F.W.; Weissman, D. mRNA vaccines—A new era in vaccinology. Nat. Rev. Drug Discov. 2018, 17, 261–279. [Google Scholar] [CrossRef]
- Van Norman, G.A. Drugs, Devices, and the FDA: Part 1: An Overview of Approval Processes for Drugs. JACC Basic Transl. Sci. 2016, 1, 170–179. [Google Scholar] [CrossRef]
- Miao, L.; Zhang, Y.; Huang, L. mRNA vaccine for cancer immunotherapy. Mol. Cancer 2021, 20, 41. [Google Scholar] [CrossRef]
- Lorentzen, C.L.; Haanen, J.B.; Met, Ö.; Svane, I.M. Clinical advances and ongoing trials on mRNA vaccines for cancer treatment. Lancet Oncol. 2022, 23, e450–e458. [Google Scholar] [CrossRef] [PubMed]
- Tamandjou Tchuem, C.R.; Auvigne, V.; Vaux, S.; Montagnat, C.; Paireau, J.; Monnier Besnard, S.; Gabet, A.; Benhajkassen, N.; Le Strat, Y.; Parent Du Chatelet, I.; et al. Vaccine effectiveness and duration of protection of COVID-19 mRNA vaccines against Delta and Omicron BA.1 symptomatic and severe COVID-19 outcomes in adults aged 50 years and over in France. Vaccine 2023, 41, 2280–2288. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Srivastava, V.; Baindara, P.; Ahmad, A. Thermostable vaccines: An innovative concept in vaccine development. Expert Rev. Vaccines 2022, 21, 811–824. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.Y.; Mehrotra, A.; Huskamp, H.A.; Uscher-Pines, L.; Ganguli, I.; Barnett, M.L. Trends in Outpatient Care Delivery and Telemedicine during the COVID-19 Pandemic in the US. JAMA Intern. Med. 2021, 181, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Hjelm, N.M. Benefits and drawbacks of telemedicine. J. Telemed. Telecare 2005, 11, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Lamptey, E.; Senkyire, E.K.; Dorcas, S.; Benita, D.A.; Boakye, E.O.; Ikome, T.; Asamoah, A. Exploring the myths surrounding the COVID-19 vaccines in Africa: The study to investigate their impacts on acceptance using online survey and social media. Clin. Exp. Vaccine Res. 2022, 11, 193–208. [Google Scholar] [CrossRef]
- Bajaj, S.S.; Maki, L.; Stanford, F.C. Vaccine apartheid: Global cooperation and equity. Lancet 2022, 399, 1452–1453. [Google Scholar] [CrossRef]
- Martonosi, S.E.; Behzad, B.; Cummings, K. Pricing the COVID-19 vaccine: A mathematical approach. Omega 2021, 103, 102451. [Google Scholar] [CrossRef]
- Xue, Q.C.; Ouellette, L.L. Innovation policy and the market for vaccines. J. Law Biosci. 2020, 7, lsaa026. [Google Scholar] [CrossRef]
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical Supply Shortages—The Need for Ventilators and Personal Protective Equipment during the COVID-19 Pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef] [PubMed]
- Bown, C.P. How COVID-19 Medical Supply Shortages Led to Extraordinary Trade and Industrial Policy. Asian Econ. Policy Rev. 2022, 17, 114–135. [Google Scholar] [CrossRef]
- Rannan-Eliya, R.P.; Wijemunige, N.; Gunawardana, J.R.N.A.; Amarasinghe, S.N.; Sivagnanam, I.; Fonseka, S.; Kapuge, Y.; Sigera, C.P. Increased Intensity of PCR Testing Reduced COVID-19 Transmission within Countries during the First Pandemic Wave. Health Aff. 2021, 40, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Tromberg, B.J.; Schwetz, T.A.; Pérez-Stable, E.J.; Hodes, R.J.; Woychik, R.P.; Bright, R.A.; Fleurence, R.L.; Collins, F.S. Rapid Scaling up of COVID-19 Diagnostic Testing in the United States—The NIH RADx Initiative. N. Engl. J. Med. 2020, 383, 1071–1077. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.J.R.D.; Pena, L. Collapse of the public health system and the emergence of new variants during the second wave of the COVID-19 pandemic in Brazil. One Health 2021, 13, 100287. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.A. Fragility and challenges of health systems in pandemic: Lessons from India’s second wave of coronavirus disease 2019 (COVID-19). Glob. Health J. 2022, 6, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Santini, A.; Messina, A.; Costantini, E.; Protti, A.; Cecconi, M. COVID-19: Dealing with ventilator shortage. Curr. Opin. Crit. Care 2022, 28, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, D.; Fowler, E.J.; Abrams, M.; Collins, S.R. COVID-19—Implications for the Health Care System. N. Engl. J. Med. 2020, 383, 1483–1488. [Google Scholar] [CrossRef]
- Kretzschmar, M.E.; Rozhnova, G.; Bootsma, M.C.J.; van Boven, M.; van de Wijgert, J.H.H.M.; Bonten, M.J.M. Impact of delays on effectiveness of contact tracing strategies for COVID-19: A modelling study. Lancet Public Health 2020, 5, e452–e459. [Google Scholar] [CrossRef]
- Martin, A.; Nateqi, J.; Gruarin, S.; Munsch, N.; Abdarahmane, I.; Zobel, M.; Knapp, B. An artificial intelligence-based first-line defence against COVID-19: Digitally screening citizens for risks via a chatbot. Sci. Rep. 2020, 10, 19012. [Google Scholar] [CrossRef]
- Wang, B.; Jin, S.; Yan, Q.; Xu, H.; Luo, C.; Wei, L.; Zhao, W.; Hou, X.; Ma, W.; Xu, Z.; et al. AI-assisted CT imaging analysis for COVID-19 screening: Building and deploying a medical AI system. Appl. Soft Comput. 2021, 98, 106897. [Google Scholar] [CrossRef] [PubMed]
- Soltan, A.A.S.; Yang, J.; Pattanshetty, R.; Novak, A.; Yang, Y.; Rohanian, O.; Beer, S.; Soltan, M.A.; Thickett, D.R.; Fairhead, R.; et al. Real-world evaluation of rapid and laboratory-free COVID-19 triage for emergency care: External validation and pilot deployment of artificial intelligence driven screening. Lancet Digit. Health 2022, 4, e266–e278. [Google Scholar] [CrossRef] [PubMed]
- Patricia Aguilera-Hermida, A. College students’ use and acceptance of emergency online learning due to COVID-19. Int. J. Educ. Res. Open 2020, 1, 100011. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Yang, H.; Thompson, J.R.; Li, J.; Loiselle, S.; Duan, H. COVID-19 lockdown improved river water quality in China. Sci. Total Environ. 2022, 802, 149585. [Google Scholar] [CrossRef]
- Khan, I.; Shah, D.; Shah, S.S. COVID-19 pandemic and its positive impacts on environment: An updated review. Int. J. Environ. Sci. Technol. 2021, 18, 521–530. [Google Scholar] [CrossRef]
- Jha, D.K.; Yashvardhini, N.; Samiksha Kumar, A. Rejuvenating impact of COVID-19 lockdown on major environmental parameters: An Indian perspective. Spat. Inf. Res. 2023, 31, 301–313. [Google Scholar] [CrossRef]
- Sarmadi, M.; Rahimi, S.; Rezaei, M.; Sanaei, D.; Dianatinasab, M. Air quality index variation before and after the onset of COVID-19 pandemic: A comprehensive study on 87 capital, industrial and polluted cities of the world. Environ. Sci. Eur. 2021, 33, 134. [Google Scholar] [CrossRef]
- Kotnala, G.; Mandal, T.K.; Sharma, S.K.; Kotnala, R.K. Emergence of Blue Sky Over Delhi Due to Coronavirus Disease (COVID-19) Lockdown Implications. Aerosol. Sci. Eng. 2020, 4, 228–238. [Google Scholar] [CrossRef]
- Abd Rabou, A. How Is the COVID-19 Outbreak Affecting Wildlife around the World? Open J. Ecol. 2020, 10, 497–517. [Google Scholar] [CrossRef]
- Bloom, N.; Liang, J.; Roberts, J.; Ying, Z.J. Does Working from Homework? Evidence from a Chinese Experiment. Q. J. Econ. 2015, 130, 165–218. [Google Scholar] [CrossRef]
- de Lucas Ancillo, A.; Gavrila Gavrila, S.; Del Val Núñez, M.T. Workplace change within the COVID-19 context: The new (next) normal. Technol. Forecast. Soc. Chang. 2023, 194, 122673. [Google Scholar] [CrossRef] [PubMed]
- Vyas, L. “New normal” at work in a post-COVID world: Work–life balance and labor markets. Policy Soc. 2022, 41, 155–167. [Google Scholar] [CrossRef]
- Al-Habaibeh, A.; Watkins, M.; Waried, K.; Javareshk, M.B. Challenges and opportunities of remotely working from home during COVID-19 pandemic. Glob. Transit. 2021, 3, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Zhang, A.; Xiao, X.; Das, S.; Zhang, Y. Work from home in the post-COVID world. Case Stud. Transp. Policy 2022, 10, 1118–1131. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.un.org/en/uncoronavirus-communications-team/un-tackling-%E2 %80 %98infodemic%E2 %80 %99-misifomation-and-cybercrime-covid-19 (accessed on 22 November 2023).
- Available online: http://blogs.bmj.com/bmj/2020/01/31/is-reporting-of-the-coronavirus-producing-viral-panic/ (accessed on 22 November 2023).
- Lencucha, R.; Bandara, S. Trust, risk, and the challenge of information sharing during a health emergency. Glob. Health 2021, 17, 21. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.business-standard.com/article/current-affairs/india-received-help-from-52-countries-during-second-wave-of-covid-govt-121073000100_1.html (accessed on 22 November 2023).
- Sharun, K.; Dhama, K. India’s role in COVID-19 vaccine diplomacy. J. Travel Med. 2021, 28, taab064. [Google Scholar] [CrossRef]
- Available online: https://www.cnbc.com/2020/06/30/billionaires-confirmed-to-have-given-money-to-covid-19-fight-wealth-x.html (accessed on 22 November 2023).
- Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/donate (accessed on 22 November 2023).
- COVID-19 Funds in Response to the Pandemic. Available online: https://www.imf.org/en/Publications/SPROLLs/covid19-special-notes (accessed on 22 November 2023).
- Saqr, M.; Wasson, B. COVID-19: Lost opportunities and lessons for the future. Int. J. Health Sci. 2020, 14, 4–6. [Google Scholar]
- Türe, Z.; Alp, E. Future pandemics: How can we be ready? Turk. J. Med. Sci. 2022, 52, 1400–1403. [Google Scholar] [CrossRef]
- Auerbach, J.D.; Forsyth, A.D.; Davey, C.; Hargreaves, J.R.; Group for lessons from pandemic HIV prevention for the COVID-19 response. Living with COVID-19 and preparing for future pandemics: Revisiting lessons from the HIV pandemic. Lancet HIV 2023, 10, e62–e68. [Google Scholar] [CrossRef]
- Besançon, L.; Peiffer-Smadja, N.; Segalas, C.; Jiang, H.; Masuzzo, P.; Smout, C.; Billy, E.; Deforet, M.; Leyrat, C. Open science saves lives: Lessons from the COVID-19 pandemic. BMC Med. Res. Methodol. 2021, 21, 117. [Google Scholar] [CrossRef]
- Quan, N.K.; Anh, N.L.M.; Taylor-Robinson, A.W. The global COVID-19 vaccine surplus: Tackling expiring stockpiles. Infect. Dis. Poverty 2023, 12, 21. [Google Scholar] [CrossRef]
- Tatar, M.; Shoorekchali, J.M.; Faraji, M.R.; Seyyedkolaee, M.A.; Pagán, J.A.; Wilson, F.A. COVID-19 vaccine inequality: A global perspective. J. Glob. Health 2022, 12, 03072. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Abdool Karim, S.S.; Baden, L.R.; Farrar, J.J.; Hamel, M.B.; Longo, D.L.; Morrissey, S.; Rubin, E.J. Addressing Vaccine Inequity—COVID-19 Vaccines as a Global Public Good. N. Engl. J. Med. 2022, 386, 1176–1179. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://reliefweb.int/report/world/pfizer-biontech-and-moderna-making-1000-profit-every-second-while-world-s-poorest (accessed on 22 November 2023).
- Okereke, M. Towards vaccine equity: Should big pharma waive intellectual property rights for COVID-19 vaccines? Public Health Pract. 2021, 2, 100165. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Srivastava, V.; Baindara, P.; Ahmad, A. Response to: “immunization in state of siege: The importance of thermostable vaccines for Ukraine and other war-torn countries and territories”. Expert Rev. Vaccines 2022, 21, 1009–1010. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Kharbikar, B.N. Lyophilized yeast powder for adjuvant free thermostable vaccine delivery. Appl. Microbiol. Biotechnol. 2021, 105, 3131–3143. [Google Scholar] [CrossRef] [PubMed]
- Björkman, A.; Gisslén, M.; Gullberg, M.; Ludvigsson, J. The Swedish COVID-19 approach: A scientific dialogue on mitigation policies. Front. Public Health 2023, 11, 1206732. [Google Scholar] [CrossRef]
- Available online: https://www.who.int/news/item/26-04-2023-who-launches-new-initiative-to-improve-pandemic-preparedness (accessed on 22 November 2023).
- Available online: https://www.nature.com/articles/d41586-022-03362-8 (accessed on 22 November 2023).
- Recommended Actions before, during and after a Pandemic. In Pandemic Influenza Preparedness and Response: A WHO Guidance Document; World Health Organization: Geneva, Switzerland, 2009; Chapter 5. Available online: https://www.ncbi.nlm.nih.gov/books/NBK143063/ (accessed on 22 November 2023).
- Available online: https://www.thehindu.com/sci-tech/health/a-report-highlights-11-ways-to-prepare-for-future-pandemics/article65936941.ece (accessed on 22 November 2023).
- Available online: https://wellcome.org/news/how-prevent-another-major-pandemic (accessed on 22 November 2023).
- Available online: https://ww1.odu.edu/content/dam/odu/offices/mun/docs/unss-future-pandemics---2.pdf (accessed on 22 November 2023).
- Daszak, P.; Olival, K.J.; Li, H. A strategy to prevent future epidemics similar to the 2019-nCoV outbreak. Biosaf. Health 2020, 2, 6–8. [Google Scholar] [CrossRef]
- Tangye, S.G. COVID Human Genetic Effort consortium. Impact of SARS-CoV-2 infection and COVID-19 on patients with inborn errors of immunity. J. Allergy Clin. Immunol. 2023, 151, 818–831. [Google Scholar] [CrossRef]
- Zhang, Q.; Bastard, P.; COVID Human Genetic Effort; Cobat, A.; Casanova, J.L. Human genetic and immunological determinants of critical COVID-19 pneumonia. Nature 2022, 603, 587–598. [Google Scholar] [CrossRef]
- Biancolella, M.; Colona, V.L.; Luzzatto, L.; Watt, J.L.; Mattiuz, G.; Conticello, S.G.; Kaminski, N.; Mehrian-Shai, R.; Ko, A.I.; Gonsalves, G.S.; et al. COVID-19 annual update: A narrative review. Hum. Genom. 2023, 17, 68. [Google Scholar] [CrossRef] [PubMed]
| Disease (Nature) | mRNA | Protein | Company/Sponsor | Status | Reference |
|---|---|---|---|---|---|
| Coronavirus (viral) | mRNA | Spike protein | Pfizer, Moderna | In public use | |
| Zika virus (viral) | mRNA-1893 | NCT03375047 | Moderna | Phase-II clinical trials completed | NCT04917861 |
| Respiratory syncytial virus (viral) | mRNA-1345 | Prefusion F glycoprotein | Moderna | Phase-III clinical trials | NCT05330975 |
| Rabies (viral) | CV7202 | Rabies virus glycoprotein | CureVac | Phase-I clinical trials completed | NCT03713086 |
| Chikungunya (viral) | mRNA-1944 | Anti-CK virus mAb | Moderna | Phase-I clinical trials completed | NCT03829384 |
| Melanoma (cancer) | BNT111 | TAAs (NY-ESO-1, MAGE-A3, tyrosinase, and TPTE) | BioNTech SE | Phase-II clinical trials | NCT04526899 |
| Cystic fibrosis (genetic disorder) | MRT5005 | CFTR protein | Translate Bio, Inc. | Phase-II clinical trials completed | NCT03375047 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumar, R.; Srivastava, V.; Nand, K.N. The Two Sides of the COVID-19 Pandemic. COVID 2023, 3, 1746-1760. https://doi.org/10.3390/covid3120121
Kumar R, Srivastava V, Nand KN. The Two Sides of the COVID-19 Pandemic. COVID. 2023; 3(12):1746-1760. https://doi.org/10.3390/covid3120121
Chicago/Turabian StyleKumar, Ravinder, Vartika Srivastava, and Kripa N. Nand. 2023. "The Two Sides of the COVID-19 Pandemic" COVID 3, no. 12: 1746-1760. https://doi.org/10.3390/covid3120121
APA StyleKumar, R., Srivastava, V., & Nand, K. N. (2023). The Two Sides of the COVID-19 Pandemic. COVID, 3(12), 1746-1760. https://doi.org/10.3390/covid3120121








