Workloads of Emergency Call Types in Active-Duty Firefighters
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Phase 1
2.2.2. Phase 2
2.2.3. Data Processing
2.3. Statistical Analysis
3. Results
3.1. Participant Description
3.2. External Load
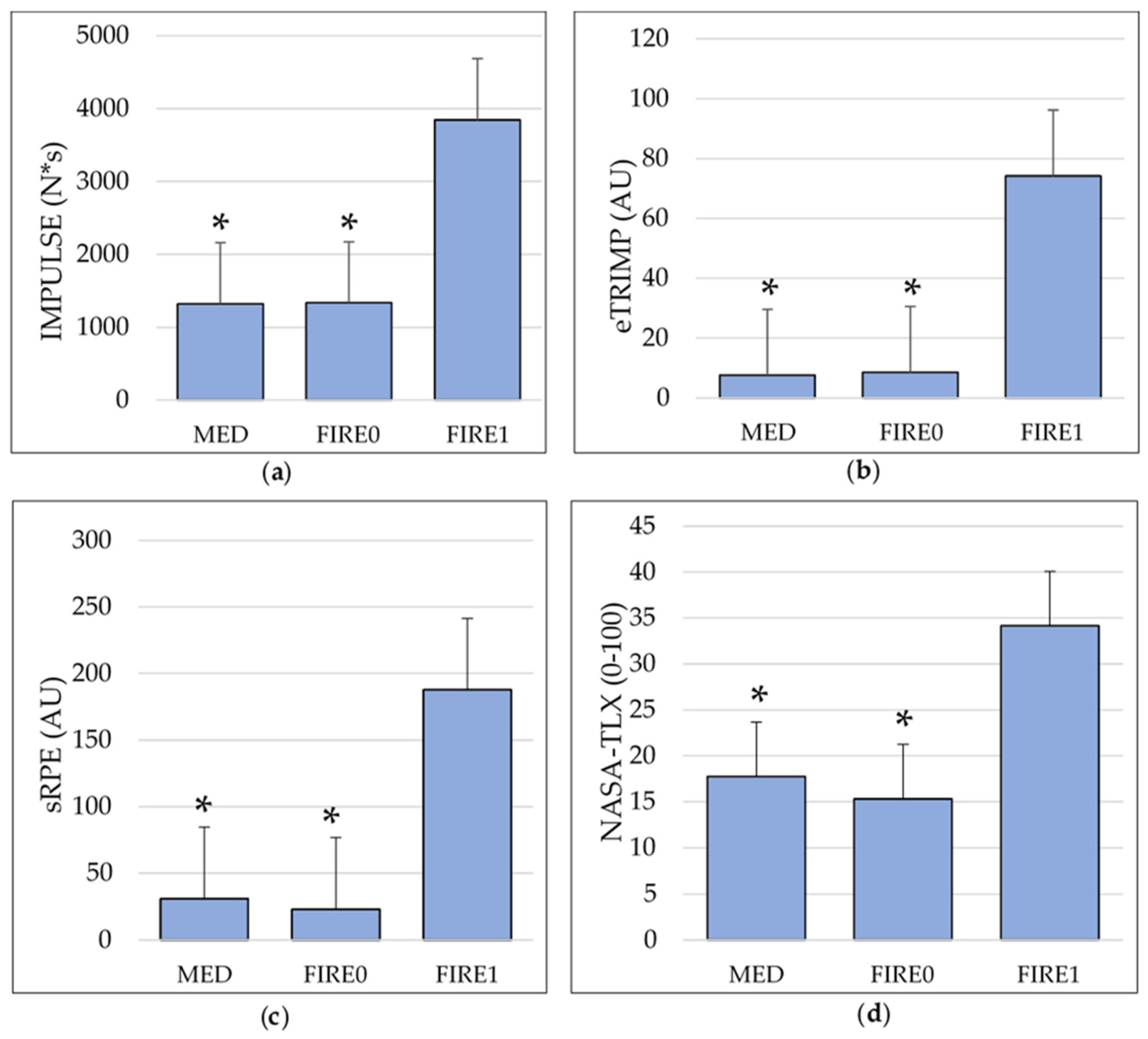
Impulse Load
3.3. Internal Load
3.3.1. Edwards’ Training Impulse
3.3.2. Foster’s Session Rating of Perceived Exertion
3.3.3. NASA-Task Load Index
4. Discussion
4.1. External Load
4.2. Internal Load
4.2.1. Edwards’ Training Impulse
4.2.2. Foster’s Session Rating of Perceived Exertion
4.2.3. NASA Task Load Index
4.3. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Fire Protection Association. NFPA 1582 Standard on Comprehensive Occupational Medical Program for Fire Departments. Available online: https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=1582 (accessed on 28 November 2023).
- Marciniak, R.A.; Tesch, C.J.; Ebersole, K.T. Heart rate response to alarm tones in firefighters. Int. Arch. Occup. Env. Health 2021, 94, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Kaikkonen, P.; Lindholm, H.; Lusa, S. Physiological load and psychological stress during a 24-hour work shift among Finnish firefighters. J. Occup. Env. Med. 2017, 59, 41–46. [Google Scholar] [CrossRef]
- Horn, G.P.; Blevins, S.; Fernhall, B.; Smith, D.L. Core temperature and heart rate response to repeated bouts of firefighting activities. Ergonomics 2013, 56, 1465–1473. [Google Scholar] [CrossRef]
- Smith, D.L.; Petruzzello, S.J.; Kramer, J.M.; Misner, J.E. The effects of different thermal environments on the physiological and psychological responses of firefighters to a training drill. Ergonomics 1997, 40, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.S.; Ong, C.N.; Phoon, W.O. Work stress of firemen as measured by heart rate and catecholamine. J. Hum. Ergol. 1987, 16, 209–218. [Google Scholar] [CrossRef]
- Barnes, B.H. The experience of traumatic stress among urban firefighters. Aust. J. Emerg. Manag. 2000, 14, 59–60. [Google Scholar]
- Billings, J.; Focht, W. Firefighter shift schedules affect sleep quality. J. Occup. Env. Med. 2016, 58, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Watkins, S.L.; Shannon, M.A.; Hurtado, D.A.; Shea, S.A.; Bowles, N.P. Interactions between home, work, and sleep among firefighters. Am. J. Ind. Med. 2021, 64, 137–148. [Google Scholar] [CrossRef]
- Blackwell, K.C.; Vaughn Becker, D.; Adams, G. Hot cognition: Exploring the relationship between excessive call volume and cognitive fatigue. FireFighter Health Saf. 2011, 7, 88–93. [Google Scholar]
- Gabbett, T.J.; Nassis, G.P.; Oetter, E.; Pretorius, J.; Johnston, N.; Medina, D.; Rodas, G.; Myslinski, T.; Howells, D.; Beard, A.; et al. The athlete monitoring cycle: A practical guide to interpreting and applying training monitoring data. Br. J. Sports Med. 2017, 51, 1451–1452. [Google Scholar] [CrossRef]
- Gabbett, T.J.; Ullah, S. Relationship between running loads and soft-tissue injury in elite team sport athletes. J. Strength Cond. Res. 2012, 26, 953–960. [Google Scholar] [CrossRef]
- Gabbett, T.J.; Whyte, D.G.; Hartwig, T.B.; Wescombe, H.; Naughton, G.A. The relationship between workloads, physical performance, injury and illness in adolescent male football players. Sports Med. 2014, 44, 989–1003. [Google Scholar] [CrossRef]
- Bourdon, P.C.; Cardinale, M.; Murray, A.; Gastin, P.; Kellmann, M.; Varley, M.C.; Gabbett, T.J.; Coutts, A.J.; Burgess, D.J.; Gregson, W.; et al. Monitoring athlete training loads: Consensus statement. Int. J. Sports Physiol. Perform 2017, 12, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.M.; Griffiths, P.C.; Mellalieu, S.D. Training Load and Fatigue Marker Associations with Injury and Illness: A Systematic Review of Longitudinal Studies. Sports Med. 2017, 47, 943–974. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, F.M.; Marcora, S.M.; Coutts, A.J. Internal and external training load: 15 years on. Int. J. Sports Physiol. Perform. 2019, 14, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Webb, H.E.; McMinn, D.R.; Garten, R.S.; Beckman, J.L.; Kamimori, G.H.; Acevedo, E.O. Cardiorespiratory responses of firefighters to a computerized fire strategies and tactics drill during physical activity. Appl. Erg. 2010, 41, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Marcel-Millet, P.; Ravier, G.; Groslambert, A. Effect of protective equipment on firefighters’ external and internal workloads during a simulated rescue intervention. J. Strength. Cond. Res. 2020, 36, 2291–2297. [Google Scholar] [CrossRef] [PubMed]
- Bouzigon, R.; Ravier, G.; Paulin, P.; Grappe, F. The use of two different methods of workload quantification in firefighters. Sci. Sports 2015, 30, 169–172. [Google Scholar] [CrossRef]
- Gentles, J.A.; Coniglio, C.L.; Besemer, M.M.; Morgan, J.M.; Mahnken, M.T. The demands of a women’s college soccer season. Sports 2018, 6, 16. [Google Scholar] [CrossRef] [PubMed]
- Edwards, S. The Heart Rate Monitor Book; Polar Electro Oy: New York, NY, USA, 1993; ISBN 0963463306. [Google Scholar]
- Foster, C. Monitoring training in athletes with reference to overtraining syndrome. Med. Sci. Sports Exerc. 1998, 30, 1164–1168. [Google Scholar] [CrossRef]
- Gawron, V.J. NASA Task Load Index. In Human Performance Measures Handbook; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2000; pp. 130–135. ISBN 0-8058-3701-9. [Google Scholar]
- Gómez-Carmona, C.D.; Pino-Ortega, J.; Sánchez-Ureña, B.; Ibáñez, S.J.; Rojas-Valverde, D. Accelerometry-based external load indicators in sport: Too many options, same practical outcome? Int. J. Env. Res. Public Health 2019, 16, 5101. [Google Scholar] [CrossRef]
- Johnstone, J.A.; Ford, P.A.; Hughes, G.; Watson, T.; Garrett, A.T. BioharnessTM multivariable monitoring device. Part I: Validity. J. Sports Sci. Med. 2012, 11, 400–408. [Google Scholar]
- Johnstone, J.A.; Ford, P.A.; Hughes, G.; Watson, T.; Garrett, A.T. BioharnessTM multivariable monitoring device. Part II: Reliability. J. Sports Sci. Med. 2012, 11, 409–417. [Google Scholar] [PubMed]
- Johnstone, J.A.; Ford, P.A.; Hughes, G.; Watson, T.; Mitchell, A.C.S.; Garrett, A.T. Field based reliability and validity of the bioharnessTM multivariable monitoring device. J. Sports Sci. Med. 2012, 11, 643–652. [Google Scholar]
- Zadeh, A.; Taylor, D.; Bertsos, M.; Tillman, T.; Nosoudi, N.; Bruce, S. Predicting sports injuries with wearable technology and data analysis. Inf. Syst. Front. 2020, 23, 1023–1037. [Google Scholar] [CrossRef]
- Sanders, D.; Abt, G.; Hesselink, M.K.C.; Myers, T.; Akubat, I. Methods of monitoring training load and their relationships to changes in fitness and performance in competitive road cyclists. Int. J. Sports Physiol. Perform 2017, 12, 668–675. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Hart, S.G.; Staveland, L.E. Development of NASA-TLX (Task load index): Results of empirical and theoretical research. In Human Mental Workload; Hancock, P.A., Meshkati, N., Eds.; Elsevier: Amsterdam, NL, USA, 1988; pp. 139–178. [Google Scholar]
- Hart, S.G. Nasa-task load index (NASA-TLX); 20 years later. Proc. Hum. Factors Ergon. Soc. 50th Annu. Meet. 2006, 50, 904–908. [Google Scholar] [CrossRef]
- Huck, S.W. Two-way analyses of variance. In Reading Statistics and Research, 6th ed.; Pearson: London, UK, 2012; pp. 276–311. ISBN 978-0132178631. [Google Scholar]
- Fahy, R.; Evarts, B.; Stein, G.P. U.S. Fire Department Profile. 2020. Available online: https://www.nfpa.org/education-and-research/research/nfpa-research/fire-statistical-reports/us-fire-department-profile?l=0 (accessed on 28 November 2023).
- Sainani, K.L. Dealing with missing data. PMR 2015, 7, 990–994. [Google Scholar] [CrossRef]
- United States Fire Administration. Fire Department Overall Run Profile as Reported to the National Fire Incident Reporting System (2020). Available online: https://www.usfa.fema.gov/downloads/pdf/statistics/v22i1-fire-department-run-profile.pdf (accessed on 28 November 2023).
- Coniglio, C.L.; Smith, A.; Bursais, A.; Kirkpatrick, J.; Justin, T. Training loads of a Division I conference volleyball tournament. In Proceedings of the East Tennessee State University College and Sport Science College Proceedings, Johnson City, TN, USA, 30 November–1 December 2018. [Google Scholar]
- Gledhill, N.; Jamnik, V.K. Characterization of the physical demands of firefighting. Can. J. Sport. Sci. 1992, 17, 207–213. [Google Scholar]
- Tibana, R.A.; de Sousa, N.M.F.; Cuhna, G.V.; Prestes, J.; Fett, C.; Gabbett, T.J.; Voltarelli, F.A. Validity of session rating perceived exertion method for quantifying internal training load during high-intensity functional training. Sports 2018, 6, 68. [Google Scholar] [CrossRef] [PubMed]
- Casamichana, D.; Castellano, J.; Calleja-Gonzalez, J.; Roman, J.S.; Castagna, C. Relationship between indicators of training load in soccer players. J. Strength. Cond. Res. 2013, 27, 369–374. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Rampinini, E.; Coutts, A.J.; Sassi, A.; Marcora, S.M. Use of RPE-based training load in soccer. Med. Sci. Sports Exerc. 2004, 36, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.J.; Sanders, D.; Myers, T.; Abt, G.; Taylor, C.A.; Akubat, I. The dose-response relationship between training load and aerobic fitness in academy rugby union players. Int. J. Sports Physiol. Perform 2018, 13, 163–169. [Google Scholar] [CrossRef]
- Smith, D.L.; DeBlois, J.P.; Kales, S.N.; Horn, G.P. Cardiovascular strain of firefighting and the risk of sudden cardiac events. Exerc. Sport. Sci. Rev. 2016, 44, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Kesler, R.M.; Ensari, I.; Bollaert, R.E.; Motl, R.W.; Hsiao-Wecksler, E.T.; Rosengren, K.S.; Fernhall, B.; Smith, D.L.; Horn, G.P. Physiological response to firefighting activities of various work cycles using extended duration and prototype SCBA. Ergonomics 2018, 61, 390–403. [Google Scholar] [CrossRef]
- Colburn, D.; Suyama, J.; Reis, S.E.; Morley, J.L.; Goss, F.L.; Chen, Y.; Moore, C.G.; Hostler, D. A comparison of cooling techniques in firefighters after a live burn evolution. Prehosp Emerg. Care 2011, 15, 226–232. [Google Scholar] [CrossRef]
- Smith, D.L.; Petruzzello, S.J.; Chludzinski, M.A.; Reed, J.J.; Woods, J.A. Selected hormonal and immunological reponses to strenuous live-fire firefighting drills. Ergonomics 2005, 48, 55–65. [Google Scholar] [CrossRef]
- Sothmann, M.S.; Saupe, K.; Jasenof, D.; Blaney, J. Heart rate response of firefighters to actual emergencies. Implications for cardiorespiratory fitness. J. Occup. Med. 1992, 34, 797–800. [Google Scholar] [CrossRef]
- Enes, A.; Oneda, G.; Alves, D.L.; de Palumbo, P.D.; Cruz, R.; Moiano Junior, J.V.M.; Novack, L.F.; Osieki, R. Determinant factors of the match-based internal load in elite soccer players. Res. Q. Exerc. Sport 2021, 92, 63–70. [Google Scholar] [CrossRef]
- Borg, G.A.V. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.L.; Petruzzello, S.J.; Kramer, J.M.; Misner, J.E. Physiological, psychophysical, and psychological responses of firefighters to training drills. Aviat. Space Env. Med. 1996, 67, 1063–1068. [Google Scholar]
- Alaimo, A.; Esposito, A.; Orlando, C.; Simoncini, A. Aircraft pilots workload analysis: Heart rate variability objective measures and NASA-Task Load Index subjective evaluation. Aerospace 2020, 7, 137. [Google Scholar] [CrossRef]
- Mansikka, H.; Virtanen, K.; Harris, D. Comparison of NASA-TLX scale, modified Cooper–Harper scale and mean inter-beat interval as measures of pilot mental workload during simulated flight tasks. Ergonomics 2019, 62, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Kesisoglou, A.; Nicolò, A.; Passfield, L. Cycling performance and training load: Effects of intensity and duration. Int. J. Sports Physiol. Perform. 2021, 16, 535–543. [Google Scholar] [CrossRef] [PubMed]
| Description | |
|---|---|
| Mental Demand | How much mental and perceptual activity was required (e.g., thinking, deciding, calculating, remembering, looking, searching, etc.)? Was the task easy or demanding, simple or complex, exacting or forgiving? |
| Physical Demand | How much physical activity was required (e.g., pushing, pulling, turning, controlling, activating, etc.)? Was the task easy or demanding, slow or brisk, slack or strenuous, restful or laborious? |
| Temporal Demand | How much time pressure did you feel due to the rate of pace at which the tasks or task elements occurred? Was the pace slow and leisurely or rapid and frantic? |
| Performance | How successful do you think you were in accomplishing the goals of the task? How satisfied were you with your performance in accomplishing these goals? |
| Effort | How hard did you have to work (mentally and physically) to accomplish your level of performance? |
| Frustration Level | How insecure, discouraged, irritated, stressed, and annoyed versus secure, gratified, content, relaxed, and complacent did you feel during the task? |
| MED | FIRE0 | FIRE1 | RM MANOVA Sample | |
|---|---|---|---|---|
| IMPULSE | 38 | 37 | 38 | 37 |
| eTRIMP | 38 | 37 | 38 | 37 |
| sRPE | 38 | 22 | 37 | 21 |
| NASA-TLX | 38 | 22 | 37 | 21 |
| Component | MED | FIRE0 | FIRE1 |
|---|---|---|---|
| Call Duration (min) | 21.15 ± 3.42 | 14.30 ± 5.86 | 42.75 ± 23.67 |
| RPE (AU) | 1.06 ± 0.84 | 1.38 ± 0.85 | 3.53 ± 1.22 |
| Heart Rate Zones (Total Time Per Call, min) | |||
| ZONE1 | 4.63 ± 3.31 | 3.94 ± 2.75 | 8.51 ± 6.98 |
| ZONE2 | 1.15 ± 1.25 | 1.45 ± 1.53 | 8.58 ± 7.31 |
| ZONE3 | 0.21 ± 0.30 | 0.46 ± 0.76 | 6.23 ± 5.23 |
| ZONE4 | 0.03 ± 0.05 | 0.08 ± 0.16 | 4.38 ± 4.86 |
| ZONE5 | 0.01 ± 0.02 | 0.01 ± 0.03 | 2.47 ± 4.43 |
| Heart Rate Zones (Percent of Call Duration, %) | |||
| ZONE1 | 21.89 ± 15.65 | 27.55 ± 19.23 | 19.91 ± 16.33 |
| ZONE2 | 5.44 ± 5.91 | 10.14 ± 10.70 | 20.07 ± 17.10 |
| ZONE3 | 0.99 ± 1.42 | 3.22 ± 5.31 | 14.57 ± 12.23 |
| ZONE4 | 0.14 ± 0.24 | 0.56 ± 1.12 | 10.25 ± 11.37 |
| ZONE5 | 0.00 ± 0.00 | 0.00 ± 0.21 | 5.78 ± 10.36 |
| NASA-TLX Raw Scores (0–100) | |||
| Mental Demand | 16.95 ± 15.97 | 12.89 ± 8.22 | 38.20 ± 23.71 |
| Physical Demand | 11.10 ± 12.21 | 12.18 ± 7.92 | 43.69 ± 23.31 |
| Temporal Demand | 14.57 ± 18.04 | 11.70 ± 8.37 | 39.28 ± 22.81 |
| Performance | 22.32 ± 31.14 | 20.46 ± 31.52 | 24.63 ± 29.14 |
| Effort | 13.86 ± 13.11 | 13.75 ± 9.55 | 40.72 ± 22.84 |
| Frustration | 12.84 ± 13.85 | 6.42 ± 5.26 | 16.02 ± 10.48 |
| NASA-TLX Weighted Contribution (%) | |||
| Mental Demand | 27.88 ± 17.40 | 22.92 ± 13.81 | 20.55 ± 14.16 |
| Physical Demand | 7.79 ± 10.26 | 13.20 ± 12.62 | 23.57 ± 13.44 |
| Temporal Demand | 14.88 ± 12.20 | 20.58 ± 12.80 | 21.69 ± 12.72 |
| Performance | 21.80 ± 22.56 | 17.84 ± 15.12 | 12.20 ± 13.53 |
| Effort | 14.30 ± 9.48 | 18.30 ± 9.99 | 18.99 ± 9.44 |
| Frustration | 13.35 ± 13.69 | 7.15 ± 8.92 | 3.00 ± 4.89 |
| Omnibus Test Results | Call Type (Mean ± SD) | |||
|---|---|---|---|---|
| Wilks’ Lambda | ||||
| F Value | MED | FIRE0 | FIRE1 | |
| Impulse (N*s) | ||||
| 21.17 * | 1320.81 ± 221.05 | 1330.42 ± 375.76 | 3857.54 ± 2442.62 ab | |
| eTRIMP (AU) | ||||
| 31.84 * | 7.67 ± 6.31 | 8.48 ± 7.28 | 74.33 ± 59.84 ab | |
| sRPE (AU) | ||||
| 14.46 * | 31.02 ± 37.15 | 23.11 ± 16.01 | 187.80 ± 141.06 ab | |
| NASA-TLX (0–100) | ||||
| 24.70 * | 17.77 ± 16.08 | 15.33 ± 10.42 | 34.17 ± 15.74 ab | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marciniak, R.A.; Cornell, D.J.; Meyer, B.B.; Azen, R.; Laiosa, M.D.; Ebersole, K.T. Workloads of Emergency Call Types in Active-Duty Firefighters. Merits 2024, 4, 1-18. https://doi.org/10.3390/merits4010001
Marciniak RA, Cornell DJ, Meyer BB, Azen R, Laiosa MD, Ebersole KT. Workloads of Emergency Call Types in Active-Duty Firefighters. Merits. 2024; 4(1):1-18. https://doi.org/10.3390/merits4010001
Chicago/Turabian StyleMarciniak, Rudi A., David J. Cornell, Barbara B. Meyer, Razia Azen, Michael D. Laiosa, and Kyle T. Ebersole. 2024. "Workloads of Emergency Call Types in Active-Duty Firefighters" Merits 4, no. 1: 1-18. https://doi.org/10.3390/merits4010001
APA StyleMarciniak, R. A., Cornell, D. J., Meyer, B. B., Azen, R., Laiosa, M. D., & Ebersole, K. T. (2024). Workloads of Emergency Call Types in Active-Duty Firefighters. Merits, 4(1), 1-18. https://doi.org/10.3390/merits4010001









