The Development of a Real-Time PCR Assay for Specific Detection of the NISKHI Sheep Pox Vaccine Virus Strain DNA
Abstract
1. Introduction
2. Materials and Methods
2.1. Samples and Viruses
2.2. DNA Extraction
2.3. Primer Design and PCR Protocol
2.4. Assay Validation on Clinical Samples
2.5. Assessment of Limit of Detection
2.6. Assessment of Competitiveness
2.7. Statistical Analysis
3. Results
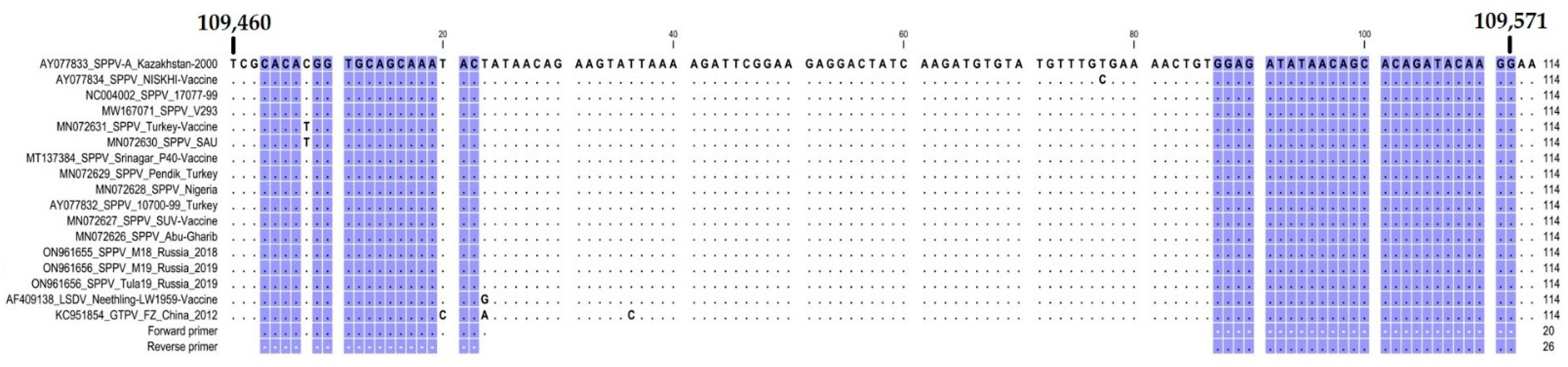
3.1. Assay Design
3.2. Performance of the HRM Assay on Clinical Samples
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; Zsak, L.; Sur, J.H.; Sandybaev, N.T.; Kerembekova, U.Z.; Zaitsev, V.L.; Kutish, G.F.; Rock, D.L. The genomes of sheeppox and goatpox viruses. J. Virol. 2002, 76, 6054–6061. [Google Scholar] [CrossRef]
- Dao, T.D.; Tran, L.H.; Nguyen, H.D.; Hoang, T.T.; Nguyen, G.H.; Tran, K.V.D.; Nguyen, H.X.; Van Dong, H.; Bui, A.N.; Bui, V.N. Characterization of Lumpy skin disease virus isolated from a giraffe in Vietnam. Transbound. Emerg. Dis. 2022, 69, e3268–e3272. [Google Scholar] [CrossRef] [PubMed]
- Tuppurainen, E.S.M.; Venter, E.H.; Shisler, J.L.; Gari, G.; Mekonnen, G.A.; Juleff, N.; Lyons, N.A.; De Clercq, K.; Upton, C.; Bowden, T.R.; et al. Review: Capripoxvirus Diseases: Current Status and Opportunities for Control. Transbound. Emerg. Dis. 2017, 64, 729–745. [Google Scholar] [CrossRef] [PubMed]
- Babiuk, S.; Bowden, T.R.; Boyle, D.B.; Wallace, D.B.; Kitching, R.P. Capripoxviruses: An emerging worldwide threat to sheep, goats and cattle. Transbound. Emerg. Dis. 2008, 55, 263–272. [Google Scholar] [CrossRef] [PubMed]
- OIE Terrestrial Manual 2008: Sheep Pox and Goat Pox, Office International Des Epizooties Paris. Chapter 2.7.14. pp. 1058–1068. Available online: https://www.woah.org/fileadmin/Home/eng/Animal_Health_in_the_World/docs/pdf/Disease_cards/SHEEP_GOAT_POX.pdf (accessed on 18 October 2022).
- CFSPH. The Center for Food Security Public Health, Lowa State University, College of Veterinary Medicine and Institution of International Cooperation in Animal Biologics, an OIE Collaborating Center. 2008. Available online: https://www.cfsph.iastate.edu/diseaseinfo/disease/?disease=sheep-pox-and-goat-pox&lang=en (accessed on 18 October 2022).
- World Organisation for Animal Health. WAHIS. Available online: https://wahis.woah.org/#/event-management (accessed on 30 October 2022).
- World Organisation for Animal Health. OIE Terrestrial Manual: Lumpy Skin Disease [Internet]; World Organisation for Animal Health: Paris, France, 2018; Available online: https://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.0 (accessed on 27 December 2020).
- Chibssa, T.R.; Settypalli, T.B.K.; Berguido, F.J.; Grabherr, R.; Loitsch, A.; Tuppurainen, E.; Nwankpa, N.; Tounkara, K.; Madani, H.; Omani, A.; et al. An HRM Assay to Differentiate Sheeppox Virus Vaccine Strains from Sheeppox Virus Field Isolates and other Capripoxvirus Species. Sci. Rep. 2019, 9, 6646. [Google Scholar] [CrossRef] [PubMed]
- Uzar, S.; Sarac, F.; Gulyaz, V.; Enul, H.; Yılmaz, H.; Turan, N. Comparison and efficacy of two different sheep pox vaccines prepared from the Bakırköy strain against lumpy skin disease in cattle. Clin. Exp. Vaccine Res. 2022, 11, 1–11. [Google Scholar] [CrossRef]
- Kurchenko, F.P.; Ivanyushchenkov, B.N.; Ufimtsev, K.P.; Alyokhin, A.F.; Gononov, Y.M.; Seitkassymov, B.K.; Kutumbetov, L.B.; Safonov, G.A.; Tatarintsev, N.T. Effectiveness of the cultural virus vaccine based on NISKhI strain against sheep pox. Veterinariya 1991, 10, 21–23. (In Russian) [Google Scholar]
- Sambrook, J.; Russell, D.W. Molecular Cloning Laboratory Manual; Science Press: Beijing, China, 2002; pp. 69–71. [Google Scholar]
- Bustin, S.A.; Benes, V.; Garson, J.A.; Hellemans, J.; Huggett, J.; Kubista, M.; Mueller, R.; Nolan, T.; Pfaffl, M.W.; Shipley, G.L.; et al. The MIQE guidelines: Minimum information for publication of quantitative real-time PCR experiments. Clin. Chem. 2009, 55, 611–622. [Google Scholar] [CrossRef]
- Singh, A. Modern Vaccines with Diva Capability: An Overview. RRJology 2015, 5, 1–12. [Google Scholar]
- Wolff, J.; Moritz, T.; Schlottau, K.; Hoffmann, D.; Beer, M.; Hoffmann, B. Development of a Safe and Highly Efficient Inactivated Vaccine Candidate against Lumpy Skin Disease Virus. Vaccines 2020, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Wondimu, A.; Tassew, H.; Gelaye, E.; Hagos, Y.; Belay, A.; Teshome, Y.; Laiju, S.; Asebe, G. Outbreak Investigation and Molecular Detection of Pox Virus Circulating in Sheep and Goats in Selected Districts of West Gojjam and Awi Zones Northwest, Ethiopia. Vet. Med. 2021, 12, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Kali, K.; Kardjadj, M.; Touaghit, N.; Yahiaoui, F.; Ben-Mahdi, M.H. Understanding the epidemiology of sheep-pox outbreaks among vaccinated Algerian sheep and post vaccination evaluation of the antibodies kinetics of the commercially used vaccine. Comp. Immunol. Microbiol. Infect. Dis. 2019, 65, 128–131. [Google Scholar] [CrossRef] [PubMed]
- Krotova, A.; Shalina, K.; Mazloum, A.; Kwon, D.; Van Schalkwyk, A.; Byadovskaya, O.; Sprygin, A. Genetic characterization of sheeppox virus strains from outbreaks in Central Russia in 2018–2019. Transbound. Emerg. Dis. 2022, 1–6. [Google Scholar] [CrossRef]
- Haegeman, A.; Zro, K.; Sammin, D.; Vandenbussche, F.; Ennaji, M.M.; De Clercq, K. Investigation of a Possible Link Between Vaccination and the 2010 Sheep Pox Epizootic in Morocco. Transbound. Emerg. Dis. 2016, 63, e278–e287. [Google Scholar] [CrossRef] [PubMed]
- Hanley, K.A. The double-edged sword: How evolution can make or break a live-attenuated virus vaccine. Evolution 2011, 4, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Bull, J.J. Evolutionary reversion of live viral vaccines: Can genetic engineering subdue it? Virus Evol. 2015, 1, vev005. [Google Scholar] [CrossRef] [PubMed]
- Sprygin, A.; Pestova, Y.; Bjadovskaya, O.; Prutnikov, P.; Zinyakov, N.; Kononova, S.; Ruchnova, O.; Lozovoy, D.; Chvala, I.; Kononov, A. Evidence of recombination of vaccine strains of lumpy skin disease virus with field strains, causing disease. PLoS ONE 2020, 15, e0232584. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, S.S.; Pandey, K.D.; Singh, R.P.; Verma, P.C.; Gupta, P.K. A vero cell derived combined vaccine against sheep pox and Peste des Petits ruminants for sheep. Vaccine 2009, 27, 2548–2553. [Google Scholar] [CrossRef] [PubMed]
- Abutarbush, S.M.; Tuppurainen, E. Serological and clinical evaluation of the Yugoslavian RM65 sheep pox strain vaccine use in cattle against lumpy skin disease. Transbound. Emerg. Dis. 2018, 65, 1657–1663. [Google Scholar] [CrossRef] [PubMed]

| Isolate/Strain | Region | Isolation Year | Type of Material | GenBank Accession Number |
|---|---|---|---|---|
| Amur | Amurskaya oblast | 2018 | Scabs | Not applicable |
| Moscow 2018 (M18) | Moscow region | 2018 | Scabs | ON961655 |
| Tula | Tula region | 2018 | Scabs | ON961657 |
| Pskov | Pskov region | 2019 | Scabs | Not applicable |
| Moscow 2019 (M19) | Moscow region | 2019 | Scabs | ON961656 |
| Tver | Tver region | 2019 | Scabs | Not applicable |
| Kaluga | Kaluga Region | 2020 | Scabs | Not applicable |
| Dagestan | Republic of Dagestan | 2022 | Scabs | Not applicable |
| ARRIAH | “NISKHI” | 1996 | Cell culture | AY077834 |
| Name | Sequence (5′->3′) | Template Strand | Calculated Tm (°C) | Length |
|---|---|---|---|---|
| Forward primer | CACACGGTGCAGCAAATACT | Plus | 60.6 | 20 |
| Reverse primer | CCTTGTATCTGTGCTGTTATATCTCC | Minus | 59.6 | 26 |
| Isolate/Strain | Original Sample (200 ng) | Dilution 10−1 | Dilution 10−2 | Dilution 10−3 | Dilution 10−4 | GM/SD | GM/SD |
|---|---|---|---|---|---|---|---|
| (M/SD) | (M/SD) | (M/SD) | (M/SD) | (M/SD) | |||
| NISKHI (ARRIAH) | 76.44 ± 0.07 | 76.57 ± 0.11 | 76.66 ± 0.2 | 76.41 ± 0.02 | 76.225 ± 0.21 | 76.46 ± 0.12 | 76.46 ± 0.12 |
| Amur | 75.44 ± 0.04 | 75.79 ± 0.04 | 75.77 ± 0.02 | 75.62 ± 0.04 | 75.43 ± 0.096 | 75.61 ± 0.05 | 75.65 ± 0.04 |
| Pskov | 75.81 ± 0.01 | 75.78 ± 0.02 | 75.75 ± 0.02 | 75.63 ± 0.04 | 75.41 ± 0.06 | 75.68 ± 0.03 | |
| Kaluga | 75.71 ± 0.01 | 75.69 ± 0.02 | 75.65 ± 0.05 | 75.59 ± 0.01 | ND | 75.66 ± 0.02 | |
| Tula | 75.32 ± 0.03 | 75.67 ± 0.03 | 75.62 ± 0.07 | 75.57 ± 0.03 | 75.18± 0.09 | 75.47 ± 0.04 | |
| M19 | 75.74 ± 0.04 | 75.68 ± 0.02 | 75.67 ± 0.02 | 75.59 ± 0.03 | 75.51 ± 0.01 | 75.64 ± 0.02 | |
| Tver | 75.66 ± 0.05 | 75.72 ± 0.03 | 75.73 ± 0.04 | 75.57 ± 0.04 | 75.56 ± 0.02 | 75.65 ± 0.04 | |
| Dagestan | 75.5 ± 0.07 | 75.79 ± 0.04 | 75.84 ± 0.04 | 75.68 ± 0.04 | 75.62 ± 0.09 | 75.69 ± 0.06 | |
| M18 | 75.89 ± 0.1 | 75.9 ± 0.07 | 75.88 ± 0.08 | 75.78 ± 0.06 | ND | 75.86 ± 0.08 |
| Field Isolate (Constant)/Vaccine Strain (Variable) | M/SD | M/SD |
|---|---|---|
| 01:01 | 75.64/0.14 | 76.17/0.08 |
| 1:10−1 | 75.58/0.01 | Neg |
| 1:10−2 | 75.52/0.12 | neg |
| 1:10−3 | 75.4/0.03 | neg |
| 1:10−4 | 75.43/0.07 | neg |
| Vaccine strain (Constant)/Field | M/SD | M/SD |
| Isolate (Variable) | ||
| 01:01 | 76.4/0.04 | 75.61/0.03 |
| 1:10−1 | 76.43/0.01 | neg |
| 1:10−2 | 76.27/0.03 | neg |
| 1:10−3 | 76.08/0.06 | neg |
| 1:10−4 | 76.71/0.01 | neg |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sprygin, A.; Mazloum, A.; Van Schalkwyk, A.; Krotova, A.; Shalina, K.; Dmitric, M.; Byadovskaya, O.; Prokhvatilova, L.; Chvala, I. The Development of a Real-Time PCR Assay for Specific Detection of the NISKHI Sheep Pox Vaccine Virus Strain DNA. Appl. Microbiol. 2022, 2, 956-964. https://doi.org/10.3390/applmicrobiol2040073
Sprygin A, Mazloum A, Van Schalkwyk A, Krotova A, Shalina K, Dmitric M, Byadovskaya O, Prokhvatilova L, Chvala I. The Development of a Real-Time PCR Assay for Specific Detection of the NISKHI Sheep Pox Vaccine Virus Strain DNA. Applied Microbiology. 2022; 2(4):956-964. https://doi.org/10.3390/applmicrobiol2040073
Chicago/Turabian StyleSprygin, Alexander, Ali Mazloum, Antoinette Van Schalkwyk, Alena Krotova, Kseniya Shalina, Marko Dmitric, Olga Byadovskaya, Larisa Prokhvatilova, and Ilya Chvala. 2022. "The Development of a Real-Time PCR Assay for Specific Detection of the NISKHI Sheep Pox Vaccine Virus Strain DNA" Applied Microbiology 2, no. 4: 956-964. https://doi.org/10.3390/applmicrobiol2040073
APA StyleSprygin, A., Mazloum, A., Van Schalkwyk, A., Krotova, A., Shalina, K., Dmitric, M., Byadovskaya, O., Prokhvatilova, L., & Chvala, I. (2022). The Development of a Real-Time PCR Assay for Specific Detection of the NISKHI Sheep Pox Vaccine Virus Strain DNA. Applied Microbiology, 2(4), 956-964. https://doi.org/10.3390/applmicrobiol2040073





