Applying the Analytic Hierarchy Process (AHP) to Accessible Housing: A Multi-Disability Perspective
Abstract
1. Introduction
Previous Research and Conceptual Framework
2. Materials and Methods
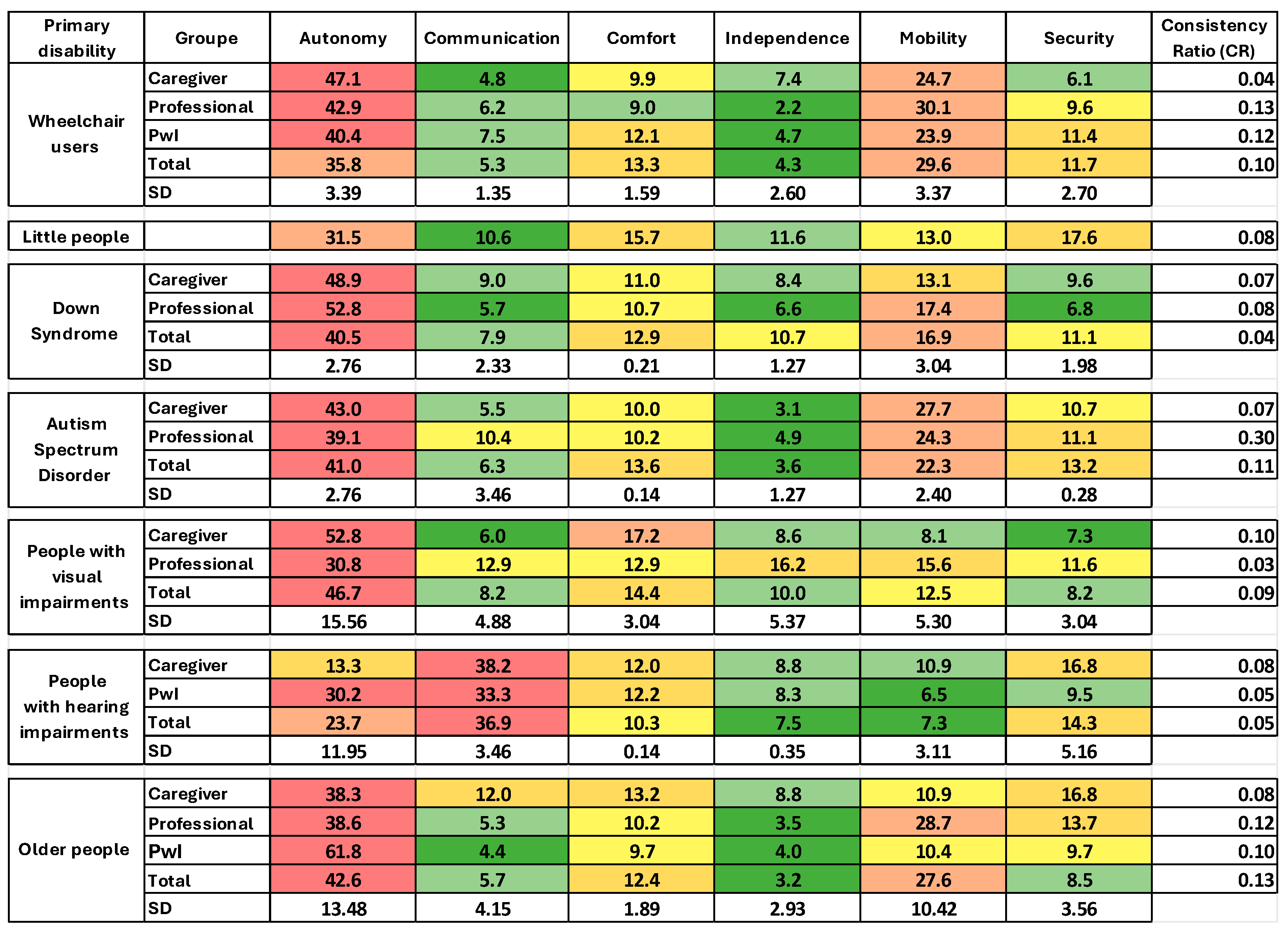
2.1. Quantitative Analysis: AHP Method
- Preference Scale: Participants rated the relative importance of each criterion using a 1 to 9 scale, based on the intensity of preference, ranging from “extremely preferable” to “equally important”.
- Pairwise Comparison Matrix: Based on the ratings, a square matrix was constructed, where each element represented the relationship between two criteria. The Consistency Index (CI) was calculated to ensure internal consistency.
- Calculation of Relative Weights: The weights for each criterion were derived from the matrix analysis, determining their priority in the habitability assessment.
- Consistency Ratio (CR): The rationality of judgments was evaluated, with values below 0.10 considered acceptable, those between 0.10 and 0.20 moderately consistent, and values above 0.20 indicating the need to adjust initial judgment.
2.2. Participant Selection
- Professionals: researchers or professionals working in the field of disability, contributing a technical perspective.
- Caregivers: individuals directly assisting people with disabilities, offering practical insights into necessary adaptations.
- People with disabilities: end-users of housing spaces whose feedback was essential in evaluating the effectiveness of the proposed criteria.
2.3. Qualitative Analysis
2.4. Validation and Results
2.5. Ethical Considerations
2.6. Background on Accessibility Types and Housing-Related Issues
2.6.1. Physical Disability
Wheelchair Users
Person with Size Alteration (Achondroplasia)
2.6.2. Cognitive Impairment
Down Syndrome
Autism Spectrum Disorder (ASD)
2.6.3. Sensory Disability
People with Visual Impairments
Primary Causes of Visual Impairments
- Macular Degeneration: Affects the macula, the central part of the retina, causing progressive loss of central vision. Individuals with macular degeneration experience difficulties perceiving details, as their vision becomes blurred by a central blind spot, impacting tasks such as reading, facial recognition, and food preparation. These individuals require increased lighting in their living spaces and adjustments to contrast levels to aid in night vision and color perception [51]
- Glaucoma: Damages the optic nerve, leading to blind spots in peripheral vision, with central vision remaining intact. Individuals with glaucoma struggle to detect objects in their periphery, making activities such as driving or navigating spaces safely more challenging [52].
- Retinal Detachment: Occurs when fluid accumulates beneath the retina, causing separation from its underlying tissue. Vision loss varies depending on the location of detachment, often leaving individuals with only partial vision in one eye, severely affecting their ability to perceive their environment cohesively [53].
- Cataracts: Characterized by clouding of the eye’s lens, resulting in blurred, hazy, or dim vision. Individuals with cataracts have trouble seeing at night, increased light sensitivity, and require brighter lighting for reading or household tasks [54].
People with Hearing Problems
2.6.4. Diminished Capacities in Older People
Alzheimer’s Disease
Older People Self-Sufficient
3. Results
3.1. Presentation Axis from ICF
- Functioning and Disability (health or disability status of the individual and its impact on body functions and structures, activities, and participation).
- Body functions are related to the physiological or psychological systems of the body, such as sensory, muscular, and mental, among others. Body structures are the anatomical parts of the human body, such as organs, limbs, and related structures.
- Activities relate to the execution of tasks or actions by an individual, such as self-care, mobility, communication, and other daily routine tasks. Participation is the possibility of involvement in daily life, such as work activities, education, social interactions, or community activities.
- 2.
- Contextual factors (environmental and personal circumstances that may influence the person’s functioning and disability are composed of environmental and personal components).
- Environmental components correspond to the physical, social, and attitudinal aspects of the individual’s environment, such as the built environment, the social support network, the attitude of other individuals, and the accessibility of services. These components can, therefore, facilitate or hinder human functioning.
- The personal component delivers the individual’s demographic characteristics, educational level or cultural background, although the ICF does not classify them specifically due to their diversity.
3.2. Prioritization of the Axes of Accessibility and Habitability According to the AHP Method
3.3. Prioritization of Indicators in Each of the Axes
3.3.1. Autonomy Axis
3.3.2. Communication Axis
3.3.3. Comfort Axis
3.3.4. Independence Axis
3.3.5. Mobility Axis
3.3.6. Safety Axis
- S01—Window and balcony sill height, selected by 25% of the Autism Spectrum Disorder group, 67% of wheelchair users, and 31% of older adults.
- S03—Grab bars and handrails, selected by 25% of the Autism Spectrum Disorder group (in hallways), 83% of wheelchair users (in bathtub and toilet), and 94% of older people (in bathtub, toilet, stairs, and hallways).
- S05—The height and location of the gas stopcock, in addition to being hidden and safe, were chosen by 25% of caregivers and professionals in the group of children with Autism Spectrum Disorder, 50% of wheelchair users (for reach issues), and 31% of older people.
- S02—Height and strength of railings at exterior openings, chosen by 33% of wheelchair users and 18% of older people.
- S07—Night lighting in the bedroom and on the way to the bathroom, selected by 50% of wheelchair users and 63% of older people.
- S08—Protection on windows and balconies (or terraces), selected by 25% of the surveyed Autism Spectrum Disorder group and 100% of the Down syndrome group.
- S10—The type of flooring on stairs is indicated by 25% of the Autism Spectrum Disorder group and older people.
- S11—The existence of smoke or carbon monoxide alarms was chosen by 68% of older people and 50% of the Down syndrome group.
4. Discussion
4.1. On the Use of AHP
4.2. About the Results
4.3. Importance of the Study in Public Policy
4.4. Limitations
5. Conclusions
Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Capasso, L.; D’Alessandro, D. Housing and Health: Here We Go Again. Int. J. Environ. Res. Public Health 2021, 18, 12060. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Disability. Key Facts; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Watson, N.; Vehmas, S. Routledge Handbook of Disability Studies, 2nd ed.; Series: Routledge international handbooks, Revised edition of Routledge handbook of disability studies; Watson, N., Vehmas, S., Eds.; Routledge: New York, NY, USA, 2020; ISBN 9780429430817. [Google Scholar]
- Valderrama-Ulloa, C.; Ferrada, X.; Rouault, F. A Tool for Universal Accessibility Assessment in the Interior of Dwellings. Inf. Constr. 2023, 75, e491. [Google Scholar] [CrossRef]
- Imrie, R. Universalism, Universal Design and Equitable Access to the Built Environment. Disabil. Rehabil. 2012, 34, 873–882. [Google Scholar] [CrossRef]
- Steinfeld, E.; Maisel, J. Universal Design: Creating Inlcusive Environments; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- Heylighen, A.; Van der Linden, V.; Van Steenwinkel, I. Ten Questions Concerning Inclusive Design of the Built Environment. Build. Environ. 2017, 114, 507–517. [Google Scholar] [CrossRef]
- Badland, H.; Whitzman, C.; Lowe, M.; Davern, M.; Aye, L.; Butterworth, I.; Hes, D.; Giles-Corti, B. Urban Liveability: Emerging Lessons from Australia for Exploring the Potential for Indicators to Measure the Social Determinants of Health. Soc. Sci. Med. 2014, 111, 64–73. [Google Scholar] [CrossRef]
- Kim, M.K.; Kim, M.J. Affordable Modular Housing for College Students Emphasizing Habitability. J. Asian Archit. Build. Eng. 2016, 15, 49–56. [Google Scholar] [CrossRef]
- Mansoori, M.; Gulnaz; Khan, M.A. Evaluating the Effectiveness of Universal Design Principles in Architecture Design Studio. ShodhKosh J. Vis. Perform. Arts 2024, 4, 151–160. [Google Scholar] [CrossRef]
- Ormerod, M.G.; Newton, R.A. Moving Beyond Accessibility: The Principles of Universal (Inclusive) Design as a Dimension in ND Modelling of the Built Environment. Archit. Eng. Des. Manag. 2005, 1, 103–110. [Google Scholar] [CrossRef]
- Machado, L.; de Oliveira, U. Analysis of Failures in the Accessibility of University Buildings. J. Build. Eng. 2021, 33, 101654. [Google Scholar] [CrossRef]
- Harper, K.; McAuliffe, K.; Parsons, D. Barriers and Facilitating Factors Influencing Implementation of Occupational Therapy Home Assessment Recommendations: A Mixed Methods Systematic Review. Aust. Occup. Ther. J. 2022, 69, 599–624. [Google Scholar] [CrossRef]
- Padilla-Muñoz, A. Discapacidad: Contexto, Concepto y Modelos. Int. Law Rev. Colomb. Derecho Int. 2010, 8, 381–414. [Google Scholar]
- Zhou, W.; Lyu, X.; Huang, Y.; Jiang, B.; Jiang, J. A Comparative Bibliometric Analysis of Global Research on Adaptation Interventions for Healthy Aging at Home. Sage Open 2025, 15, 1–17. [Google Scholar] [CrossRef]
- Cho, H.; MacLachlan, M.; Clarke, M.; Mannan, H. Accessible Home Environments for People with Functional Limitations: A Systematic Review. Int. J. Environ. Res. Public Health 2016, 13, 826. [Google Scholar] [CrossRef]
- Valderrama-Ulloa, C.; Ferrada, X.; Herrera, F. Breaking Down Barriers: Findings from a Literature Review on Housing for People with Disabilities in Latin America. Int. J. Environ. Res. Public Health 2023, 20, 4972. [Google Scholar] [CrossRef]
- Lindsay, S.; Ragunathan, S.; Fuentes, K.; Li, Y. Barriers and Facilitators to Obtaining Accessible Housing among Children, Youth and Young Adults with Disabilities and Their Families: A Scoping Review. Disabil. Rehabil. 2024, 46, 3266–3285. [Google Scholar] [CrossRef]
- Struckmeyer, L.; Morgan-Daniel, J.; Ahrentzen, S.; Ellison, C. Home Modification Assessments for Accessibility and Aesthetics: A Rapid Review. Health Environ. Res. Des. J. 2021, 14, 313–327. [Google Scholar] [CrossRef] [PubMed]
- Muñoz Cordones, J.-P. Revisión Sistemática de Iniciativas Que Promueven La Accesibilidad Universal. Rev. Esp. Discapac. 2024, 12, 185–214. [Google Scholar] [CrossRef]
- Saaty, T.; De Paola, P. Rethinking Design and Urban Planning for the Cities of the Future. Buildings 2017, 7, 76. [Google Scholar] [CrossRef]
- Goepel, K. Implementation of an Online Software Tool for the Analytic Hierarchy Process (AHP-OS). Int. J. Anal. Hierarchy Process 2018, 10, 471–487. [Google Scholar] [CrossRef]
- Taherdoost, H.; Madanchian, M. Multi-Criteria Decision Making (MCDM) Methods and Concepts. Encyclopedia 2023, 3, 77–87. [Google Scholar] [CrossRef]
- Valderrama-Ulloa, C.; Schmitt, C.; Marchetti, J.-P.; Bucarey, V. Design Criteria Recommendation to Achieve Accessibility in House to Different Users. Int. J. Archit. Environ. Eng. 2024, 18, 83–88. [Google Scholar]
- Valderrama-Ulloa, C.; Schmitt, C.; Ortiz Velosa, E.; Marchetti, J.-P.; Bucarey, V. Condiciones de Habitabilidad de Viviendas Para Personas Mayores. Revisión de Criterios de Diseño. Inf. Constr. 2024, 76, 6623. [Google Scholar] [CrossRef]
- Valderrama-Ulloa, C.; Bucarey, V.; Marchetti, J.-P. Architectural Needs in Housing for People with Disabilities. Salud Cienc. Tecnol. 2023, 3, 693. [Google Scholar] [CrossRef]
- Hernández Sampieri, R.; Fernández Collado, C.; Baptista Lucio, P. Fundamentos de Metodología de La Investigación, 6th ed.; McGraw-Hill: New York, NY, USA, 2005. [Google Scholar]
- World Health Organization. Towards a Common Language for Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Saaty, T. The Analytic Hierarchy Process: Planning, Priority Setting, Resource Allocation; McGraw-Hill: New York, NY, USA, 1980. [Google Scholar]
- Muhr, T. ATLAS.ti, Scientific Software Development GmbH. Available online: https://atlasti.com/ (accessed on 9 December 2024).
- World Health Organization. Assistive Technology; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Servicio Nacional de la Discapacidad (SENADIS) III Estudio; Nacional de La Discapacidad En Chile: Iquique, Chile, 2023.
- Ferrada, X.; Valderrama, C.; Fuentes-Contreras, C. Economic and Technical Analysis of Universal Accessibility in Social and Private Housing in Chile. IOP Conf. Ser. Earth Environ. Sci. 2020, 503, 012003. [Google Scholar] [CrossRef]
- de Brito Prado, B.; Frascareli Lelis, V.; Katayama, E.; Magagnin, R. Spatial Accessibility for Elderly in a Multi Residential Condominium in Brazil. In Proceedings of the 14th International Conference on Mobility and Transport for Elderly and Disabled Persons (TRANSED), Lisbon, Portugal, 28–31 July 2015. [Google Scholar]
- Pauli, R. Achondroplasia: A Comprehensive Clinical Review. Orphanet J. Rare Dis. 2019, 14, 1. [Google Scholar] [CrossRef] [PubMed]
- Collett-Solberg, P.F.; Ambler, G.; Backeljauw, P.F.; Bidlingmaier, M.; Biller, B.M.K.; Boguszewski, M.C.S.; Cheung, P.T.; Choong, C.S.Y.; Cohen, L.E.; Cohen, P.; et al. Diagnosis, Genetics, and Therapy of Short Stature in Children: A Growth Hormone Research Society International Perspective. Horm. Res. Paediatr. 2019, 92, 1–14. [Google Scholar] [CrossRef]
- Achondroplasia. Available online: https://medlineplus.gov/genetics/condition/achondroplasia/ (accessed on 9 December 2024).
- Parisi, B.; Matos e Silva, C.; Oliveira, K.; Araújo, R. Acessibilidade e Inclusão Social Da Pessoa Com Nanismo: Da Legislação à Realidade. Rev. Bras. Assuntos Reg. Urbanos 2021, 7, 19–29. [Google Scholar] [CrossRef]
- Tavares, A.; Cardoso, R.; Santos, J.; Sampaio, G. Acessibilidade Para Pessoas Com Deficiência: Algunas Dificuldades Em Projetar Para Indivíduos Com Nanismo. In Proceedings of the VI Encontro Nacional de Ergonomía do Ambiente Construido (ENEAC ANO 10), Recife, Brazil, 23–25 May 2016. [Google Scholar]
- Brusilovsky, B. Modelo para Diseñar Espacios Accesibles. Espectro Cognitivo. Available online: http://riberdis.cedid.es/bitstream/handle/11181/5484/Modelo_para_dise%c3%b1ar_espacios_accesibles.pdf?sequence=1&rd=0031103474977893 (accessed on 9 December 2024).
- Chen, L.; Wang, L.; Wang, Y.; Hu, H.; Zhan, Y.; Zeng, Z.; Liu, L. Global, Regional, and National Burden and Trends of Down Syndrome From 1990 to 2019. Front. Genet. 2022, 13, 908482. [Google Scholar] [CrossRef]
- Nazer, H.J.; Aguila, R.A.; Cifuentes, O.L. Vigilancia Epidemiológica Del Síndrome de Down En Chile, 1972 a 2005. Rev. Medica Chile 2006, 134, 1549–1557. [Google Scholar] [CrossRef]
- Cumella, S.; Heslam, S. Supported Housing for People with Down’s Syndrome. Br. J. Learn. Disabil. 2014, 42, 251–256. [Google Scholar] [CrossRef]
- World Health Organization. Autismo Datos y Cifras; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- World Health Organization. Autismo; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Zeidan, J.; Fombonne, E.; Scorah, J.; Ibrahim, A.; Durkin, M.; Saxena, S.; Yusuf, A.; Shih, A.; Elsabbagh, M. Global Prevalence of Autism: A Systematic Review Update. Autism Res. 2022, 15, 778–790. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, M. An Architecture for Autism: Concepts of Design Intervention for Autistic User. Int. J. Archit. Res. 2008, 2, 189–211. [Google Scholar]
- Boey, D.; Fitzmaurice, K.; Tse, T.; Chan, M.; Carey, L. Classifying Types of Visual Loss Linked with Function to Inform Referral to Vision Rehabilitation for Older Adults in Singapore. Gerontol. Geriatr. Med. 2022, 8, 1–18. [Google Scholar] [CrossRef]
- World Health Organization. Blindness and Vision Impairment; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Steinmetz, J.; Bourne, R.; Briant, P.S.; Flaxman, S.R.; Taylor, H.R.B.; Jonas, J.B.; Abdoli, A.A.; Abrha, W.A.; Abualhasan, A.; Abu-Gharbieh, E.G.; et al. Causes of Blindness and Vision Impairment in 2020 and Trends over 30 Years, and Prevalence of Avoidable Blindness in Relation to VISION 2020: The Right to Sight: An Analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, 144–160. [Google Scholar] [CrossRef]
- Centro Oftalmológico de Barcelona. Degeneración Macular Asociada a La Edad; Centro Oftalmológico de Barcelona: Barcelona, Spain, 2023. [Google Scholar]
- American Academy of Ophthalmology. Understanding Glaucoma: Symptoms, Causes, Diagnosis, Treatment; American Academy of Ophthalmology: San Francisco, CA, USA, 2024. [Google Scholar]
- National Eye Institute. A Simple Vista: Desprendimiento de La Retina; National Eye Institute: Bethesda, MD, USA, 2024. [Google Scholar]
- National Eye Institute. A Simple Vista: Cataratas; National Eye Institute: Bethesda, MD, USA, 2024. [Google Scholar]
- Guerry, E.; Caumon, C.; Bécheras, E.; Zissis, G. Influence of Chromatic and Lighting on the Visual Environment of the Elderly: A Critical Literature Review. Color Res. Appl. 2021, 46, 117–124. [Google Scholar] [CrossRef]
- Haile, L.; Kamenov, K.; Briant, P.S.; Orji, A.U.; Steinmetz, J.D.; Abdoli, A. Hearing Loss Prevalence and Years Lived with Disability, 1990–2019: Findings from the Global Burden of Disease Study 2019. Lancet 2021, 397, 996–1009. [Google Scholar] [CrossRef] [PubMed]
- Sowden, J.; Kros, C.; Sirimanna, T.; Pagarkar, W.; Oluonye, N.; Henderson, R. Impact of Sight and Hearing Loss in Patients with Norrie Disease: Advantages of Dual Sensory Clinics in Patient Care. BMJ Paediatr. Open 2020, 4, e000781. [Google Scholar] [CrossRef] [PubMed]
- Organización Panamericana de la Salud Demencia. Available online: https://www.paho.org/es/temas/demencia (accessed on 9 December 2024).
- Li, X.; Feng, X.; Sun, X.; Hou, N.; Han, F.; Liu, Y. Global, Regional, and National Burden of Alzheimer’s Disease and Other Dementias, 1990–2019. Front. Aging Neurosci. 2022, 14, 937486. [Google Scholar] [CrossRef]
- Klaassen, P.G.; Werlinger, E.E.; Contreras, E.L.; González, B.A.; Vera, C.A.; Juica, A.S.; Fuentealba, S.M. Calidad de Vida En Demencia Alzheimer: Un Nuevo Desafío. Rev. Chil. Neuropsiquiatr. 2021, 59, 361–367. [Google Scholar] [CrossRef]
- Dias de Azevedo, M.-C.; Charchat-Fichman, H.; Damazio Vera, M.-M. Environmental Interventions to Support Orientation and Social Engagement of People with Alzheimer’s Disease. Dement. Neuropsychol. 2021, 15, 510–523. [Google Scholar] [CrossRef]
- World Health Organization. Ageing and Health. Keys Fact; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- Ministerio de Desarrollo Social. Gobierno de Chile Encuesta de Caracterización Socioeconómica Nacional; Ministerio de Desarrollo Social: Santiago, Chile, 2022. [Google Scholar]
- Glasinovic Peña, A. Prevención de Caídas y Ayudas Técnicas En El Adulto Mayor, Enfoque Para La Atención Primaria Chilena. Rev. Chil. Med. Fam. 2020, 14, 1–8. [Google Scholar]
- Lord, S.; Menz, H.; Sherrington, C. Home Environment Risk Factors for Falls in Older People and the Efficacy of Home Modifications. Age Ageing 2006, 35, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Pizzi, M.; Chalmers, J.; Bunout, D.; Osorio, P.; Fernández, V.; Cusato, M.; Avendaño, V.; Rivera, K. Physical Barriers and Risks in Basic Activities of Daily Living Performance Evaluation in State Housing for Older People in Chile. Hous. Care Support 2013, 16, 23–31. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Impairments, Disabilities, and Handicaps. A Manual of Classification Relating to the Consequences of Disease; World Health Organization: Geneva, Switzerland, 1980. [Google Scholar]
- Darko, A.; Chan, A.; Ameyaw, E.; Owusu, E.; Pärn, E.; Edwards, D. Review of Application of Analytic Hierarchy Process (AHP) in Construction. Int. J. Constr. Manag. 2019, 19, 436–452. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, Y.; Wang, L. A Study on the Quality Evaluation Index System of Smart Home Care for Older Adults in the Community—Based on Delphi and AHP. BMC Public Health 2023, 23, 411. [Google Scholar] [CrossRef]
- Bender, A.; Din, A.; Hoesli, M.; Brocher, S. Environmental Preferences of Homeowners. J. Prop. Invest. Financ. 2000, 18, 445–455. [Google Scholar] [CrossRef]
- Wu, F. Housing Environment Preference of Young Consumers in Guangzhou, China. Prop. Manag. 2010, 28, 174–192. [Google Scholar] [CrossRef]
- Goodwin, I.; Davis, E.; Winkler, D.; Douglas, J.; Wellecke, C.; D’Cruz, K.; Mulherin, P.; Liddicoat, S. Making Homes More Accessible for People with Mobility Impairment: A Lived Experience Perspective. Aust. J. Social. Issues 2022, 57, 956–969. [Google Scholar] [CrossRef]
- Slaug, B.; Chiatti, C.; Oswald, F.; Kaspar, R.; Schmidt, S. Improved Housing Accessibility for Older People in Sweden and Germany: Short Term Costs and Long-Term Gains. Int. J. Environ. Res. Public Health 2017, 14, 964. [Google Scholar] [CrossRef]
- Slaug, B.; Granbom, M.; Iwarsson, S. An Aging Population and an Aging Housing Stock—Housing Accessibility Problems in Typical Swedish Dwellings. J. Aging Environ. 2020, 34, 156–174. [Google Scholar] [CrossRef]
- Kuboshima, Y.; McIntosh, J. Housing Design That Improves the Independence and Safety for Older Adults Using a Walker. Appl. Ergon. 2021, 97, 103539. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, K.; Brod, M.; Smith, A.; Gianettoni, J.; Viuff, D.; Ota, S.; Charlton, R. Assessing Physical Symptoms, Daily Functioning, and Well-being in Children with Achondroplasia. Am. J. Med. Genet. A 2021, 185, 33–45. [Google Scholar] [CrossRef]
- Ireland, P.; Pacey, V.; Zankl, A.; Edwards, P.; Johnson, L.; Savarirayan, R. Optimal Management of Complications Associated with Achondroplasia. Appl. Clin. Genet. 2014, 7, 117–125. [Google Scholar] [CrossRef]
- Shediac, R.; Moshkovich, O.; Gerould, H.; Ballinger, R.; Williams, A.; Bellenger, M.; Quinn, J.; Hoover-Fong, J.; Mohnike, K.; Savarirayan, R.; et al. Experiences of Children and Adolescents Living with Achondroplasia and Their Caregivers. Mol. Genet. Genom. Med. 2022, 10, e1891. [Google Scholar] [CrossRef]
- Rooney, C.; Hadjri, K.; Mcallister, K.; Rooney, M.; Faith, V.; Craig, C. Experiencing Visual Impairment in a Lifetime Home: An Interpretative Phenomenological Inquiry. J. Hous. Built Environ. 2018, 33, 45–67. [Google Scholar] [CrossRef]
- Riazi, A.; Ying Boon, M.; Bridge, C.; Dain, S.J. Home Modification Guidelines as Recommended by Visually Impaired People. J. Assist. Technol. 2012, 6, 270–284. [Google Scholar] [CrossRef]
- Brugnaro, B.; Fernandes, G.; De Campos, A.; Pavão, S.; Pfeifer, L.; Kraus de Camargo, O.; Hlyva, O.; Rocha, N. Home Participation and Personal and Environmental Factors in Children and Adolescents with Down Syndrome. Dev. Med. Child Neurol. 2024, 66, 1031–1044. [Google Scholar] [CrossRef]
- Sood, D.; LaVesser, P.; Schranz, C. Influence of Home Environment on Participation in Home Activities of Children with an Autism Spectrum Disorder. Open J. Occup. Ther. 2014, 2, 2. [Google Scholar] [CrossRef]
- Lee, Y.; Park, J.; Jang, M. Perceived Effects of Home Renovation on Independence of Physically Disabled Koreans Living at Home. Disabil. Rehabil. 2018, 40, 2380–2387. [Google Scholar] [CrossRef]
- Jiménez-Arberas, E.; Varela, G.R.; Ordoñez Fernández, F.; Méndez Fernández, M.-I. Development of the Home Environmental Scale of Accessibility Instrument for Spain. Clin. Pract. 2024, 14, 1123–1136. [Google Scholar] [CrossRef]

| Variable | Frequency | % | |
|---|---|---|---|
| Sex | Male | 11 | 29% |
| Female | 26 | 71% | |
| Age | <30 years | 6 | 17% |
| 31–40 years | 11 | 29% | |
| 41–50 years | 10 | 28% | |
| 51–60 years | 5 | 13% | |
| >60 years | 5 | 13% | |
| Group | Professionals | 16 | 43% |
| Caregivers (mothers and daughters) | 14 | 37% | |
| People with disabilities | 7 | 20% | |
| Primary disability | Wheelchair users | 6 | 17% |
| Little people (achondroplasia) | 2 | 5% | |
| Down Syndrome | 2 | 5% | |
| Autism Spectrum Disorder | 4 | 11% | |
| People with visual impairments | 2 | 5% | |
| People with hearing impairments | 4 | 11% | |
| People with Alzheimer’s disease * | 1 | 3% | |
| Older people (>60 years) | 16 | 43% | |
| Total | 37 | 100% | |
| Autonomy | Communication | Comfort (Indoor Quality) | Independence | Mobility | Safety |
|---|---|---|---|---|---|
| A01—Height of bathroom accessories (soap dish, towel rack, toilet paper, etc.) | C01—Type of doorbell and/or buzzer (sound, light and audible in several places) | IQ01—Access to natural lighting in most areas | I01—Height of hardware (door and window handles and locks) | M01—Ample space to avoid obstacles in its route | S01—Window and balcony sill heights |
| A02—Height of sanitary fixtures (toilet, sink) | C02—Location of artificial light | IQ02—Sound insulation from outside in all areas | I02—Hardware type (door and window handles and locks) | M02—Door characteristics | S02—Height and strength of railings at all openings to the exterior |
| A03—Height and placement of faucets (kitchen and bathroom) | C03—Strategic location of windows (optimization v/s glare) | IQ03—Quantity of artificial lighting | I03—Window characteristics | M03—Clear width of doors (in access, bathroom, bedroom, kitchen) | S03—Support bars and/or handrails |
| A04—Clear transfer areas in the bathroom | C04- Use of appropriate colors in furniture (contrast with floor) | IQ04—Indoor temperature control system | I04—Type of door opening (in access, bathroom, bedroom, kitchen) | M04—Staircase characteristics | S04—Emergency button in bathroom |
| A05—Shower or bathtub seat | C05—Use of separate exhaust fan switch (bathroom or other) | IQ5—On/off control of fixed heating (radiators or air-conditioning) | I05—Height of adaptable lighting fixtures | M05—Existence of slopes | S05—Height and location of gas stopcock |
| A06—Closet dimensions (or fixed furniture: height and depth) | C06—Control of natural light in enclosures (glare) | IQ6—On/off control of fixed heating (radiators or air-conditioning) | I06—Number of sockets | M06—Existence of stairs | S06—Protection under the stairs (to avoid knocks) |
| A07—Kitchen appliance dimensions (height and depth) | IQ07—Existence of ventilation (natural or exhaust) | I07—Number of switches | M07—Size of spaces (bathroom, kitchen, bedroom) | S07—Night lighting in the bedroom and on the way to the bathroom | |
| A08—Sink dimension | I08—Type and color of switch buttons | M08—Type of flooring | S08—Protection on windows and balcony | ||
| A09—Bathroom furniture dimension | I09—Location and height of sockets | M09—Corridor characteristics (dimension and trajectory) | S09—Type of kitchen appliances (sound and automatic shut-off) | ||
| A10—Kitchen furniture dimension | I10—Location and height of switches | S10—Type of staircase flooring | |||
| A11—Shower or bathtub dimensions | I11—Color and illumination of switch boxes and sockets to locate them | S11—Existence of alarms (smoke or carbon monoxide) | |||
| A12—Bathtub type (bathtub, shower tray, or floor-level access) | I12—Type of furniture (fixed) | S12—Electrical outlet protection | |||
| A13—Faucet type (bathroom and kitchen) | I13—Organization and characteristics of spaces | ||||
| A14—Countertop dimension |
| Indicator | Wheelchair Users | Little Person | Professionals and Caregivers of Children with | Visual Impairments | Hearing Impairments | Older People | |
|---|---|---|---|---|---|---|---|
| Down Syndrome | Autism Spectrum Disorder | ||||||
| A01—Height of bathroom accessories (soap dish, towel rack, toilet paper, etc.) | 100% | ||||||
| A02—Height of sanitary fixtures (toilet, sink) | 67% | 100% | |||||
| A03—Height and placement of Faucets (kitchen and bathroom) | 100% | 100% | 88% | ||||
| A04—Clear transfer areas in the bathroom | 67% | ||||||
| A05—Shower or bathtub seat | 63% | ||||||
| A06—Closet dimensions (or fixed furniture: height and depth) | 50% | 50% | 18% | ||||
| A07—Kitchen appliance dimensions (height and depth) | 50% | ||||||
| A08—Sink dimension | 50% | 50% | |||||
| A09—Bathroom furniture dimension | 67% | 50% | 56% | ||||
| A10—Kitchen furniture dimension | 50% | 50% | 50% | ||||
| A11—Shower or Bathtub Dimensions | 67% | ||||||
| A12—Bathtub type (bathtub, shower tray or floor-level access) | 67% | 100% | 75% | ||||
| A13—Faucet Type (bathroom and kitchen) | 67% | 50% | 25% | 18% | |||
| A14—Countertop dimension | 25% | 50% | 25% | ||||
| Indicator | Wheelchair Users | Little Person | Professionals and Caregivers of Children with | Visual Impairments | Hearing Impairments | Older People | |
|---|---|---|---|---|---|---|---|
| Down Syndrome | Autism Spectrum Disorder | ||||||
| I01—Height of hardware (door and window handles and locks) | 50% | 25% | |||||
| I02—Hardware type (door and window handles and locks) | 50% | 100% | 75% | 44% | |||
| I03—Window characteristics | 33% | 100% | 50% | 38% | |||
| I04—Type of door opening (in access, bathroom, bedroom, kitchen) | 75% | 50% | 68% | ||||
| I05—Height of adaptable lighting fixtures | 18% | ||||||
| I06—Number of sockets | 13% | ||||||
| I07—Number of switches | 13% | ||||||
| I08—Type and color of switch buttons | 31% | ||||||
| I09—Location and height of sockets | 50% | 50% | 44% | ||||
| I10—Location and height of switches | 50% | 100% | 44% | ||||
| I11—Color and illumination of switch boxes and sockets to locate them | 100% | ||||||
| I12—Type of furniture (fixed) | 25% | 56% | |||||
| I13—Organization and characteristics of spaces | 50% | 100% | 50% | ||||
| Indicator | Wheelchair Users | Little Person | Professionals and Caregivers of Children with | Visual Impairments | Older People | |
|---|---|---|---|---|---|---|
| Down Syndrome | Autism Spectrum Disorder | |||||
| M01—Ample space to avoid obstacles in its route | 67% | 50% | 63% | |||
| M02—Door characteristics | 100% | 18% | ||||
| M03—Clear width of doors (in access, bathroom, bedroom, kitchen) | 83% | 75% | ||||
| M04—Staircase characteristics | 100% | 50% | 100% | 50% | ||
| M05—Existence of slopes | 67% | 63% | ||||
| M06—Existence of stairs | 50% | 38% | ||||
| M07—Size of spaces (bathroom, kitchen, bedroom) | 50% | 50% | ||||
| M08—Type of flooring | 50% | 100% | 44% | |||
| M09—Corridor characteristics (dimension and trajectory) | 67% | |||||
| Primary Disability/AXIS | Autonomy (n = 14) | Communication (n = 6) | Comfort (n = 7) | Independence (n = 13) | Mobility (n = 9) | Safety (n = 12) | Total (n = 61) |
|---|---|---|---|---|---|---|---|
| Wheelchair users | 83%—10 | 16%—1 | 14%—1 | 46%—6 | 77%—7 | 50%—6 | 51%—31 |
| Little people (achondroplasia) | 64%—9 | 0 | 0 | 8%—1 | 11%—1 | 0 | 18%—11 |
| Children with Down syndrome (professionals and caregivers) | 7%—1 | 0 | 14%—1 | 31%—4 | 11%—1 | 25%—3 | 16%—10 |
| Children with Autism Spectrum Disorder (professionals and caregivers) | 14%—2 | 0 | 71%—5 | 31%—4 | 11%—1 | 50%—6 | 30%—18 |
| People with visual impairments | 7%—1 | 64%—4 | 28%—2 | 8%—2 | 33%—3 | 8%—1 | 21%—13 |
| People with hearing impairments | 7%—1 | 32%—2 | 43%—3 | 8%—1 | 0 | 8%—1 | 13%—8 |
| Older people | 50%—7 | 16%—1 | 56%—4 | 85%—11 | 88%—8 | 75%—9 | 66%—40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valderrama-Ulloa, C.; Ferrada, X.; Herrera, F. Applying the Analytic Hierarchy Process (AHP) to Accessible Housing: A Multi-Disability Perspective. Disabilities 2025, 5, 48. https://doi.org/10.3390/disabilities5020048
Valderrama-Ulloa C, Ferrada X, Herrera F. Applying the Analytic Hierarchy Process (AHP) to Accessible Housing: A Multi-Disability Perspective. Disabilities. 2025; 5(2):48. https://doi.org/10.3390/disabilities5020048
Chicago/Turabian StyleValderrama-Ulloa, Claudia, Ximena Ferrada, and Felipe Herrera. 2025. "Applying the Analytic Hierarchy Process (AHP) to Accessible Housing: A Multi-Disability Perspective" Disabilities 5, no. 2: 48. https://doi.org/10.3390/disabilities5020048
APA StyleValderrama-Ulloa, C., Ferrada, X., & Herrera, F. (2025). Applying the Analytic Hierarchy Process (AHP) to Accessible Housing: A Multi-Disability Perspective. Disabilities, 5(2), 48. https://doi.org/10.3390/disabilities5020048






