Power Mobility, Supported Standing and Stepping Device Use in the First Two Years of Life: A Case Report of Twins Functioning at GMFCS V
Abstract
:1. Introduction
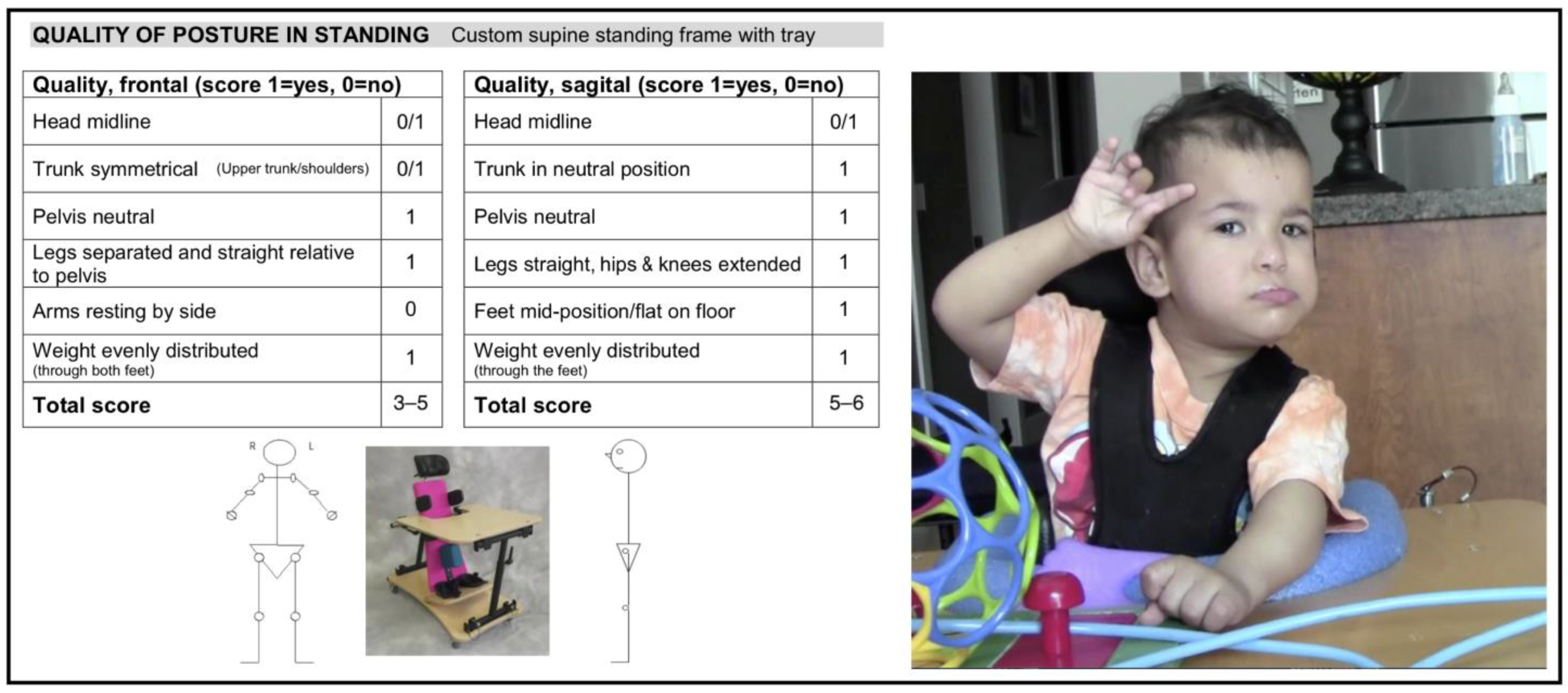
2. Materials and Methods
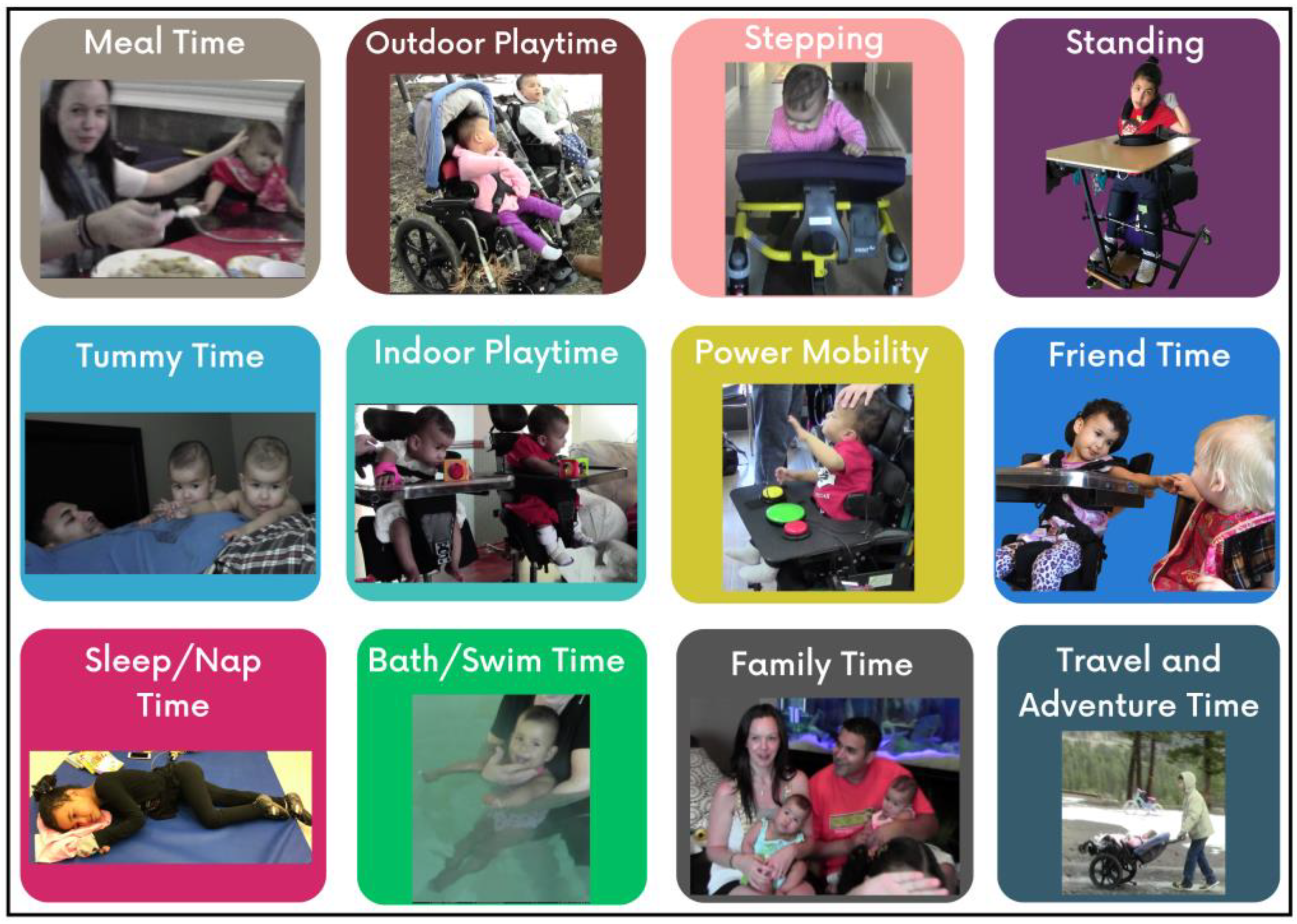
3. Description of Feasibility and Use of Assistive Devices in the First 2 Years
3.1. Initial Assessment
3.2. Equipment Trials and Introduction of Positioning and Mobility Devices
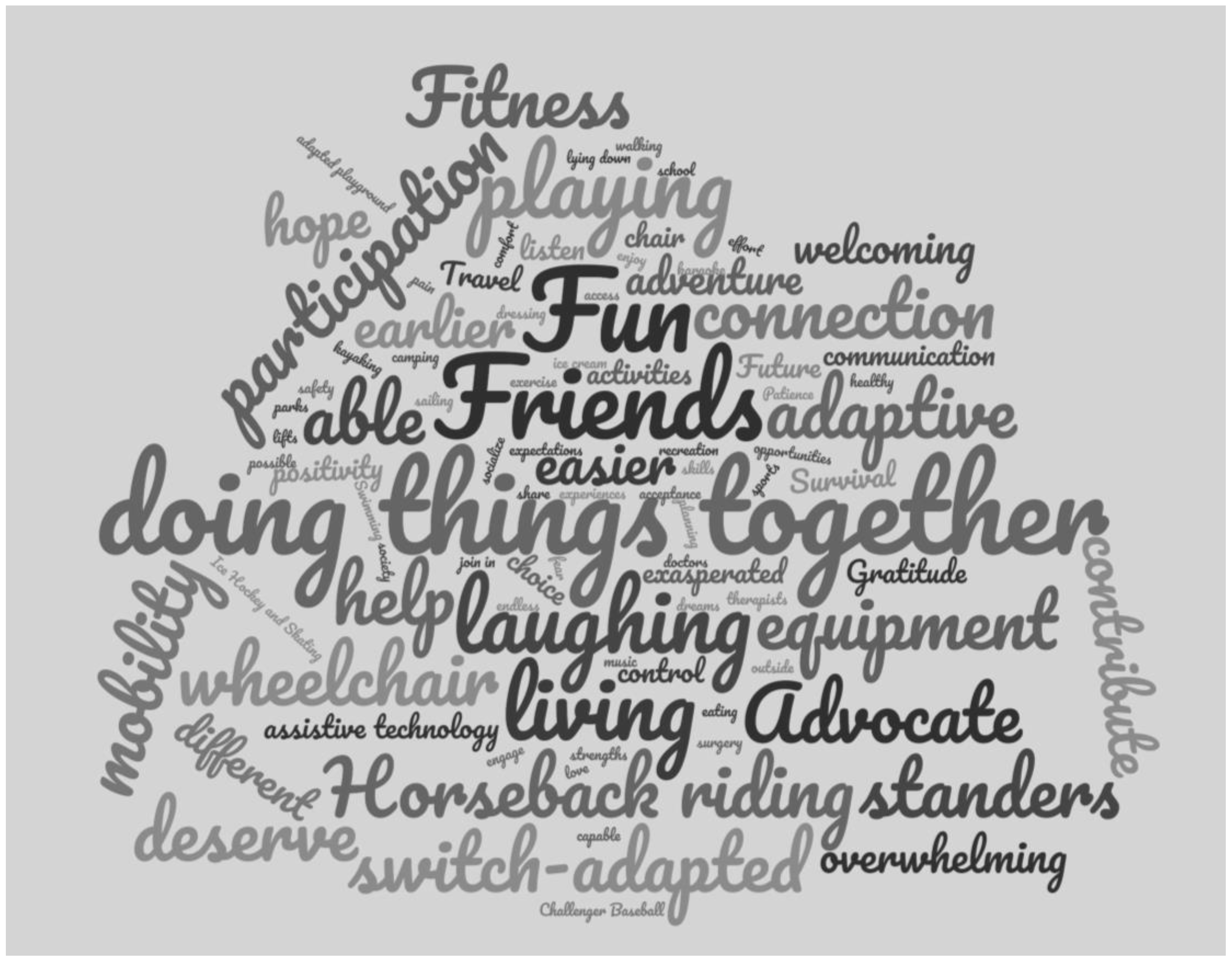
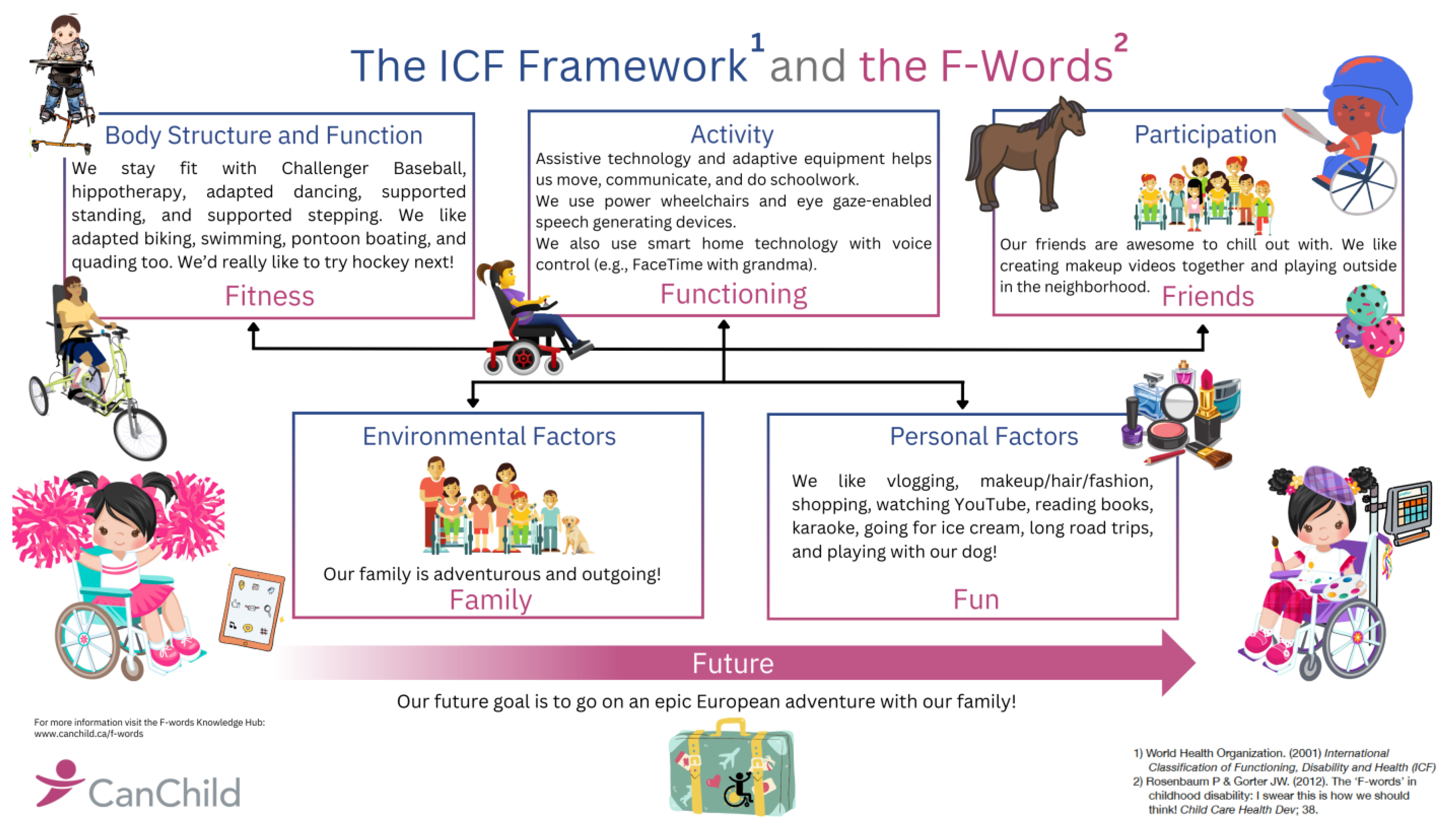
3.3. Family’s Lived Experience Reflected in the F-Words
- How did adaptive equipment help with the girls’ early development and functioning?
- Mom:
- I think seeing the world not laying down…as soon as you got them up in the feeding chairs, that allowed full participation in eating…communicating, and learning how to socialize, and other equipment…I guess it’s more for fun, playing like typical [kids]… to be experimental with speed and direction…like the GoBot, spinning in a circle…or going in the mini-car and being able to control that.
- How did adaptive equipment help the girls engage and participate in family life and routines?
- Mom:
- Like in every aspect … like being able to move, being able to go out, and being able to eat safely, and being able to play, and engage, and socialize. And experience life. Everything!
- How has adaptive equipment helped the girls with fitness?
- Sister:
- There’s standing frames
- Dad:
- And keeping the body in proper form, right? Like spines, hips, arms, legs, neck, everything right? Like it’s been huge.
- Does your equipment help you with making friends?
- Mom:
- you had your standing frame at school and you participated differently with gym. You have had some fun with your power wheelchair with your friends.
- Dad:
- I think kids think it’s cool… their power wheelchair where it can go as almost as high as me, which is six feet. Yeah, it’s cool. I think it brings in a crowd, especially if it’s out in public.
- Mom:
- And having assistive technology for eye gaze and stuff. Because other kids have their laptops at school now and they have their own systems. That’s really important.
- How has having this equipment impacted family life and the girls’ future?
- Dad:
- [without it] We wouldn’t be able to go anywhere, right? …The pros far outweigh the cons… it’s definitely worth it, because without it we’d just be, honestly, I don’t know. I can’t fathom life without it.
- Sister:
- The girls have more opportunities
- Mom:
- So, if you look back at ten years of say, them laying on the couch without support, or laying on the ground, or not being able to sit upright, or … experience different fun … equipment, along with friends and peers, and being able to be out in the world—well, then you’ve got two completely different kids right now. They would look a lot different. They would act a lot different. They wouldn’t have any speech or quality of life.
- Dad:
- you can see how much it has affected their lives and how much it’s made our lives better.
- What advice would you give to other families in a similar situation?
- Mom:
- Try not to compare your children to others around you …Also to keep on fighting for what your child and you deserve.
- Dad:
- Advocate…Stay positive… because there’s always something around the bend that you’re gonna have to deal with. Right? So, staying positive, Number one. But number two, surround yourself with good support—and that means friends, family, therapists…
- Mom:
- it was really overwhelming and stuff, right? But…what would it be like…if we didn’t start earlier? I believed in everybody around us, I guess. And then just to try and live every day the best you can. Because you’re going to have lots of bad days.
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- MacLennan, A.H.; Lewis, S.; Moreno-De-Luca, A.; Fahey, M.; Leventer, R.J.; McIntyre, S.; Ben-Pazi, H.; Corbett, M.; Wang, X.; Baynam, G.; et al. Genetic or other causation should not change the clinical diagnosis of cerebral palsy. J. Child Neurol. 2019, 34, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Kwong, A.K.L.; Fitzgerald, T.L.; Doyle, L.W.; Cheong, J.L.Y.; Spittle, A.J. Predictive validity of spontaneous early infant movement for later cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2018, 60, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Romeo, D.M.; Ricci, D.; Brogna, C.; Mercuri, E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: A critical review of the literature. Dev. Med. Child Neurol. 2016, 58, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.; Romeo, D.M.; Chorna, O.; Novak, I.; Galea, C.; Del Secco, S.; Guzzetta, A. The Pooled Diagnostic Accuracy of Neuroimaging, General Movements, and Neurological Examination for Diagnosing Cerebral Palsy Early in High-Risk Infants: A Case Control Study. J. Clin. Med. 2019, 8, 1879. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Palisano, R.J.; Rosenbaum, P.; Bartlett, D.; Livingston, M.H. Content validity of the expanded and revised Gross Motor Function Classification System. Dev. Med. Child Neurol. 2008, 50, 744–750. [Google Scholar] [CrossRef]
- Gorter, J.W.; Ketelaar, M.; Rosenbaum, P.; Helders, P.J.M.; Palisano, R. Use of the GMFCS in infants with CP: The need for reclassification at age 2 years or older. Dev. Med. Child Neurol. 2009, 51, 46–52. [Google Scholar] [CrossRef]
- Palisano, R.J.; Cameron, D.; Rosenbaum, P.L.; Walter, S.D.; Russell, D. Stability of the Gross Motor Function Classification System. Dev. Med. Child Neurol. 2006, 48, 424–428. [Google Scholar] [CrossRef]
- Williams, S.; Stott, N.; Wilson, N.; Sorhage, A.; Battin, M.; Hogan, A.; Mackey, A. “It should have been given sooner, and we shouldn’t have to fight for it”: Understanding the family experience of the diagnosis of cerebral palsy. Dev. Med. Child Neurol. 2019, 61, 75–223. [Google Scholar] [CrossRef]
- Bailes, A.F.; Gannotti, M.; Bellows, D.M.; Shusterman, M.; Lyman, J.; Horn, S.D. Caregiver knowledge and preferences for gross motor function information in cerebral palsy. Dev. Med. Child Neurol. 2018, 60, 1264–1270. [Google Scholar] [CrossRef]
- Einspieler, C.; Marschik, P.B.; Pansy, J.; Scheuchenegger, A.; Krieber, M.; Yang, H.; Kornacka, M.K.; Rowinska, E.; Soloveichick, M.; Bos, A.F. The general movement optimality score: A detailed assessment of general movements during preterm and term age. Dev. Med. Child Neurol. 2016, 58, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Einspieler, C.; Bos, A.F.; Krieber-Tomantschger, M.; Alvarado, E.; Barbosa, V.M.; Bertoncelli, N.; Burger, M.; Chorna, O.; Del Secco, S.; DeRegnier, R.-A.; et al. Cerebral Palsy: Early Markers of Clinical Phenotype and Functional Outcome. J. Clin. Med. 2019, 8, 1616. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.A.; Mackey, A.; Sorhage, A.; Battin, M.; Wilson, N.; Spittle, A.; Stott, N.S. Clinical practice of health professionals working in early detection for infants with or at risk of cerebral palsy across New Zealand. J. Paediatr. Child Health 2021, 57, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Merino-Andrés, J.; Hidalgo-Robles, Á.; Pérez-Nombela, S.; Williams, S.A.; Paleg, G.; Fernández-Rego, F.J. Tool Use for Early Detection of Cerebral Palsy: A Survey of Spanish Pediatric Physical Therapists. Pediatr. Phys. Ther. 2022, 34, 202–210. [Google Scholar] [CrossRef]
- de Campos, A.C.; Hidalgo Robles, A.; Longo, E.; Shrader, C.; Paleg, G. Scoping review of early interventions for young children classified as Gross Motor Function Classification System (GMFCS) IV and V. Dev. Med. Child Neurol, 2023; Online ahead of print. [Google Scholar]
- te Velde, A.; Morgan, C.; Novak, I.; Tantsis, E.; Badawi, N. Early Diagnosis and Classification of Cerebral Palsy: An Historical Perspective and Barriers to an Early Diagnosis. J. Clin. Med. 2019, 8, 1599. [Google Scholar] [CrossRef]
- Sun, D.; Wang, Q.; Hou, M.; Li, Y.; Yu, R.; Zhao, J.; Wang, K. Clinical characteristics and functional status of children with different subtypes of dyskinetic cerebral palsy. Medicine 2018, 97, e10817. [Google Scholar] [CrossRef]
- Miao, H.; Mathur, A.M.; Aravamuthan, B.R. Spasticity and Dystonia are Underidentified in Young Children at High Risk for Cerebral Palsy. J. Child Neurol. 2022, 37, 105–111. [Google Scholar] [CrossRef]
- Knights, S.; Datoo, N.; Kawamura, A.; Switzer, L.; Fehlings, D. Further evaluation of the scoring, reliability, and validity of the hypertonia assessment tool (HAT). J. Child Neurol. 2014, 29, 500–504. [Google Scholar] [CrossRef]
- Barry, M.J.; VanSwearingen, J.; Albright, A. Reliability and responsiveness of the Barry–Albright Dystonia Scale. Dev. Med. Child Neurol. 1999, 41, 404–411. [Google Scholar] [CrossRef]
- Rice, J.; Skuza, P.; Baker, F.; Russo, R.; Fehlings, D. Identification and measurement of dystonia in cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 1249–1255. [Google Scholar] [CrossRef]
- Marsico, P.; Frontzek-Weps, V.; Balzer, J.; Van Hedel, H.J.A. Hypertonia Assessment Tool: Reliability and Validity in Children with Neuromotor Disorders. J. Child Neurol. 2017, 32, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Monbaliu, E.; Ortibus, E.; Roelens, F.; Desloovere, K.; Deklerck, J.; Prinzie, P.; De Cock, P.; Feys, H. Rating scales for dystonia in cerebral palsy: Reliability and validity. Dev. Med. Child Neurol. 2010, 52, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Dar, H.; Stewart, K.; McIntyre, S.; Paget, S. Multiple motor disorders in cerebral palsy. Dev. Med. Child Neurol. 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Casey, J.; Rosenblad, A.; Rodby-Bousquet, E. Postural asymmetries, pain, and ability to change position of children with cerebral palsy in sitting and supine: A cross-sectional study. Disabil. Rehabil. 2022, 44, 2363–2371. [Google Scholar] [CrossRef]
- Lobo, M.A.; Harbourne, R.T.; Dusing, S.C.; McCoy, S.W. Grounding early intervention: Physical therapy cannot just be about motor skills anymore. Phys. Ther. 2013, 93, 94–103. [Google Scholar] [CrossRef] [PubMed]
- McLean, L.; Paleg, G.; Livingstone, R. Supported-standing interventions for children and young adults with non-ambulant cerebral palsy: A scoping review. Dev. Med. Child Neurol. 2023, 65, 754–772. [Google Scholar] [CrossRef]
- Livingstone, R.W.; Paleg, G.S. Use of overground supported-stepping devices for non-ambulant children, adolescents, and adults with cerebral palsy: A scoping review. Disabilities 2023, 3, 20012. [Google Scholar] [CrossRef]
- Livingstone, R.; Paleg, G. Practice considerations for the introduction and use of power mobility for children. Dev. Med. Child Neurol. 2014, 56, 210–221. [Google Scholar] [CrossRef]
- Rosen, L.; Plummer, T.; Sabet, A.; Lange, M.L.; Livingstone, R. RESNA position on the application of power mobility devices for pediatric users. Assist. Technol. 2023, 35, 14–22. [Google Scholar] [CrossRef]
- Bornstein, M.H.; Hahn, C.-S.; Suwalsky, J.T.D. Physically developed and exploratory young infants contribute to their own long-term academic achievement. Psychol. Sci. 2013, 24, 1906–1917. [Google Scholar] [CrossRef]
- Farran, E.K.; Critten, V.; Courbois, Y.; Campbell, E.; Messer, D. Spatial cognition in children with physical disability; What is the impact of restricted independent exploration? Front. Hum. Neurosci. 2021, 15, 669034. [Google Scholar] [CrossRef]
- Sabet, A.; Feldner, H.; Tucker, J.; Logan, S.W.; Galloway, J.C. ON Time Mobility: Advocating for Mobility Equity. Pediatr. Phys. Ther. 2022, 34, 546–550. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Gorter, J.W. The “F-words” in childhood disability: I swear this is how we should think! Child Care Health Dev. 2012, 38, 457–463. [Google Scholar] [CrossRef]
- Rosenbaum, P. The F-words for child development: Functioning, family, fitness, fun, friends and future. Dev. Med. Child Neurol. 2022, 64, 141–142. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability & Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Livingstone, R.; Field, D. Systematic review of power mobility outcomes for infants, children and adolescents with mobility limitations. Clin. Rehabil. 2014, 28, 954–964. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, A.; Ullenhag, A.; Wahlström, U.; Krumlinde-Sundholm, L. Mini-MACS: Development of the Manual Ability Classification System for children younger than 4 years of age with signs of cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 72–78. [Google Scholar] [CrossRef]
- Hidecker, M.J.C.; Paneth, N.; Rosenbaum, P.L.; Kent, R.D.; Lillie, J.; Eulenberg, J.B.; Chester, K., Jr.; Johnson, B.; Michalsen, L.; Evatt, M.; et al. Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev. Med. Child Neurol. 2011, 53, 704–710. [Google Scholar] [CrossRef]
- Baranello, G.; Signorini, S.; Tinelli, F.; Guzzetta, A.; Pagliano, E.; Rossi, A.; Foscan, M.; Tramacere, I.; Romeo, D.M.M.; Ricci, D.; et al. Visual Function Classification System for children with cerebral palsy: Development and validation. Dev. Med. Child Neurol. 2020, 62, 104–110. [Google Scholar] [CrossRef]
- Sellers, D.; Pennington, L.; Bryant, E.; Benfer, K.; Weir, K.; Aboagye, S.; Morris, C. Mini-EDACS: Development of the Eating and Drinking Ability Classification System for young children with cerebral palsy. Dev. Med. Child Neurol. 2022, 64, 897–906. [Google Scholar] [CrossRef]
- Fife, S.E.; Roxborough, L.A.; Armstrong, R.W.; Harris, S.R.; Gregson, J.L.; Field, D. Development of a clinical measure of postural control for assessment of adaptive seating in children with neuromotor disabilities. Phys. Ther. 1991, 71, 981–993. [Google Scholar] [CrossRef]
- Rodby-Bousquet, E.; Persson-Bunke, M.; Czuba, T. Psychometric evaluation of the Posture and Postural Ability Scale for children with cerebral palsy. Clin. Rehabil. 2016, 30, 697–704. [Google Scholar] [CrossRef]
- Rodby-Bousquet, E.; Ágústsson, A.; Jónsdóttir, G.; Czuba, T.; Johansson, A.C.; Hägglund, G. Interrater reliability and construct validity of the Posture and Postural Ability Scale in adults with cerebral palsy in supine, prone, sitting and standing positions. Clin. Rehabil. 2014, 28, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Stewart, K.; Harvey, A.; Johnston, L.M. A systematic review of scales to measure dystonia and choreoathetosis in children with dyskinetic cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 786–795. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, L.; Durkin, J. Assessment of learning powered mobility use–Applying grounded theory to occupational performance. J. Rehabil. Res. Dev. 2014, 51, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Svensson, E.; Nilsson, L. Inter-rater reliability of the Assessment of Learning Powered mobility use, version 2.0, when applied with children and adults engaged in Driving to Learn in a powered wheelchair. Aust. Occup. Ther. J. 2021, 68, 115–123. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Farris, J.P.; Cain, B.; King, E.; VandenBerg, A. Development and content validation of the Power Mobility Training Tool. Disabil. Rehabil. Assist. Technol. 2018, 13, 10–24. [Google Scholar] [CrossRef]
- Lisbeth Nilsson––Universal ALP Tool. Available online: https://www.lisbethnilsson.se/en/alp-tool/ (accessed on 7 September 2023).
- Larnert, P.; Risto, O.; Hägglund, G.; Wagner, P. Hip displacement in relation to age and gross motor function in children with cerebral palsy. J. Child Orthop. 2014, 8, 129–134. [Google Scholar] [CrossRef]
- Fulford, G.; Brown, J. Position as a cause of deformity in children with cerebral palsy. Dev. Med. Child Neurol. 1976, 18, 305–314. [Google Scholar] [CrossRef]
- Porter, D.; Michael, S.; Kirkwood, C. Patterns of postural deformity in non-ambulant people with cerebral palsy: Scoliosis, pelvic obliquity, windswept hips and hip dislocation. Clin. Rehab. 2007, 21, 1087–1096. [Google Scholar] [CrossRef]
- Casey, J.; Agustsson, A.; Rosenblad, A.; Rodby-Bousquet, E. Relationship between scoliosis, windswept hips and contractures with pain and asymmetries in sitting and supine in 2450 children with cerebral palsy. Disabil. Rehabil. 2022, 44, 6738–6743. [Google Scholar] [CrossRef]
- Paleg, G.; Livingstone, R. Evidence-informed clinical perspectives on postural management for hip health in children and adults with non-ambulant cerebral palsy. J. Pediatr. Rehabil. Med. 2022, 15, 39–48. [Google Scholar] [CrossRef]
- Morgan, C.; Darrah, J.; Gordon, A.M.; Harbourne, R.; Spittle, A.; Johnson, R.; Fetters, L. Effectiveness of motor interventions in infants with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2016, 58, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Gimeno, H.; Adlam, T. Protocol: Using single-case experimental design to evaluate whole-body dynamic seating on activity, participation, and quality of life in dystonic cerebral palsy. Healthcare 2020, 8, 11. [Google Scholar] [CrossRef]
- Lange, M.L.; Crane, B.; Diamond, F.J.; Eason, S.; Presperin Pedersen, J.; Peek, G. RESNA position on the application of dynamic seating. Assist. Technol. 2021, 30, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lange, M.L. Clinical changes as a result of dynamic seating in a young adult with cerebral palsy. Disabil. Rehabil. Assist. Technol. 2021, 21, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Cimolin, V.; Piccinini, L.; Avellis, M.; Cazzaniga, A.; Turconi, A.C.; Crivellini, M.; Galli, M. 3D-Quantitative evaluation of a rigid seating system and dynamic seating system using 3D movement analysis in individuals with dystonic tetraparesis. Disabil. Rehabil. Assist. Technol. 2009, 4, 422–428. [Google Scholar] [CrossRef]
- Hahn, M.; Simkins, S.; Gardner, J.; Kaushik, G. A Dynamic Seating System for Children with Cerebral Palsy. J. Musculoskelet. Res. 2009, 12, 21–30. [Google Scholar] [CrossRef]
- Harniess, P.A.; Basu, A.P.; Bezemer, J.; Gibbs, D. How do parents frame their engagement experience in early intervention? A grounded theory study. Disabil. Rehabil. 2023, 31, 1–10. [Google Scholar] [CrossRef]
- George, C.; Levin, W.; Ryan, J.M. The use and perception of support walkers for children with disabilities: A United Kingdom survey. BMC Pediatr. 2020, 20, 528. [Google Scholar] [CrossRef]
- Low, S.A.; McCoy, S.W.; Beling, J.; Adams, J. Pediatric physical therapists’ use of support walkers for children with disabilities: A nationwide survey. Pediatr. Phys. Ther. 2011, 23, 381–389. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Jones, M.; Livingstone, R.; Breaux, B.; Tsotsoros, J.; Williams, K.M. Power mobility for children: A survey study of American and Canadian therapists’ perspectives and practices. Dev. Med. Child Neurol. 2018, 60, 1018–1025. [Google Scholar] [CrossRef]
- Angsupaisal; Maathuis, C.G.B.; Hadders-Algra, M. Adaptive seating systems in children with severe cerebral palsy across International Classification of Functioning, Disability and Health for Children and Youth version domains: A systematic review. Dev. Med. Child Neurol. 2015, 57, 919–930. [Google Scholar] [CrossRef] [PubMed]
- Hospodar, C.M.; Feldner, H.A.; Logan, S.W. Active mobility, active participation: A systematic review of modified ride-on car use by children with disabilities. Disabil. Rehabil. Assist. Technol. 2023, 18, 974–988. [Google Scholar] [CrossRef] [PubMed]
- Feldner, H.A.; Gaebler-Spira, D.; Awasthi, V.; Bjornson, K. Supportive mobility device use across the life span by individuals with cerebral palsy: A qualitative study. Dev. Med. Child Neurol. 2022, 64, 1392–1401. [Google Scholar] [CrossRef]
- Sloane, B.M.; Kenyon, L.K.; Logan, S.W.; Feldner, H.A. Caregiver perspectives on powered mobility devices and participation for children with cerebral palsy in Gross Motor Function Classification System level V. Dev. Med. Child Neurol. 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Verschuren, O.; Hulst, R.Y.; Voorman, J.; Pillen, S.; Luitwieler, N.; Dudink, J.; Gorter, J.W. 24-Hour activity for children with cerebral palsy: A clinical practice guide. Dev. Med. Child Neurol. 2020, 63, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Verschuren, O.; Peterson, M.; Balemans, A.C.J.; Hurvitz, E.A. Exercise and physical activity recommendations for people with cerebral palsy. Dev. Med. Child Neurol. 2016, 58, 798–808. [Google Scholar] [CrossRef] [PubMed]
- Ostensjø, S.; Carlberg, E.B.; Vøllestad, N. The use and impact of assistive devices and other environmental modifications on everyday activities and care in young children with cerebral palsy. Disabil. Rehabil. 2005, 27, 849–861. [Google Scholar] [CrossRef]
- Moen, R.D.; Østensjø, S. Understanding the use and benefits of assistive devices among young children with cerebral palsy and their families in Norway: A cross-sectional population-based registry study. Disabil. Rehabil. Assist. Technol. 2023, 7, 1–9. [Google Scholar] [CrossRef]



| Measure | Description |
|---|---|
| Gross Motor Function Classification System (GMFCS) [5,6] | Five-point ordinal scale classifying gross motor and mobility function in children and youth with CP. Abilities range from I (walks without restrictions in the community by school-age to V (requires support to sit and primarily uses wheelchair mobility) |
| Mini Manual Abilities Classification System (mini-MACS) [38] | Five-point ordinal scale classifying manual abilities in children with CP under 4 years of age. Manual abilities range from I (handles objects easily and successfully) to V (does not handle objects) |
| Communication Function Classification System (CFCS) [39] | Five-point ordinal scale classifying abilities of children with disabilities to send and receive communication. Communication abilities range from I (sends and receives with familiar and unfamiliar partners effectively and efficiently) to V (seldom effectively sends or receives, even with familiar partners) |
| Visual Function Classification System (VFCS) [40] | Five-point ordinal scale classifying how toddlers, children and youth with CP use visual function in daily life. Visual function ranges from I (uses visual function easily and successfully in vision-related activities) to V (does not use visual function even in very adapted environments) |
| Mini Eating and Drinking Abilities Classification System (mini-EDACS) [41] | Five-point ordinal scale classifying eating and drinking functional abilities in children with CP under 36 months of age. Eating and drinking abilities range from I (eats and drinks safely and efficiently) to V (unable to eat or drink safely—tube feeding may be considered to provide nutrition) |
| Level of Sitting Scale (LSS) [42] | Eight-point ordinal scale classifying postural abilities of children with disabilities to maintain bench sitting with feet unsupported. Abilities range from 1 (unable to be supported in upright sitting by one adult for 30 s) to 8 (able to move in and out of the seated position in all directions) |
| Posture and Postural Abilities Scale (PPAS) [43,44] | Seven-point ordinal scale classifying postural abilities plus a detailed description of posture from the front and the side in supine and prone lying, bench sitting with feet supported and standing positions. Postural abilities range from 1 (unable to maintain position without support) to 7 (able to move in and out of position). The PPAS is valid and reliable for use with children and adults with CP and can be used as an outcome measure to record change in posture following provision of adaptive seating, lying or standing devices. |
| Barry-Albright Dystonia Scale (BADS) [20] | Five-point criterion-based, ordinal scale from 0 (no dystonia) to 4 (severe dystonia) in eyes, mouth, neck, trunk and limbs for a maximum score of 32 points. BADS is considered to have moderate construct validity, limited content validity and moderate concurrent or predictive validity [45]. |
| Assessment of Learning Powered mobility use (ALP-tool 2.0) [46] | Eight-point ordinal scale describing the power mobility learning process from 1 (novice) to 8 (Expert). It is validated for all ages and cognitive levels. Very good inter-rater reliability has been established between professionals and family members or caregivers [47] |
| Power Mobility Training Tool (PMTT) [48] | Five-point ordinal scale describing non-motor, motor and driving skills from 0 (not attempted) to 4 (able to complete independently >90% of the time) for a total score of 48. It was developed to guide power mobility training for young children. |
| Universal Assessment of Learning Process (Universal ALP-tool) [49] | Modified from the ALP-tool 2.0 to describe the learning process for all tools and assistive devices. For devices activated through physical or body movements such as a stepping device: in stage 1 (phases 1–3), individuals can exert force and learn what the device is used for; in stage 2 (phases 4 and 5), they can grade force and begin searching to find a working pattern for functional use; and at stage 3 (phases 6–8), they can direct force and begin to use the device to attain a functional outcome or achieve a self-selected goal. Phase 3 represents basic use of tool functions, phase 6 is competent use, and phase 8 represents expert tool use integrated into everyday life. |
| Classification | Functional Level at 2 Years of Age |
|---|---|
| Gross Motor Function Classification System (GMFCS) | V (has difficulty controlling head and trunk posture in most positions; uses adaptive seating to maintain position comfortably; usually lifted by another person to move about indoors) |
| Mini Manual Abilities Classification System (mini-MACS) | V (does not handle objects; can touch, press, hold onto or handle a few objects with constant adult assistance) |
| Communication Function Classification System (CFCS) | IV (inconsistent sender and receiver with familiar communication partners) |
| Visual Function Classification System (VFCS) | I (uses visual function easily and successfully in vision-related activities) |
| Mini Eating and Drinking Abilities Classification System (mini-EDACS) | IV (eats and drinks with close attention to food texture, fluid consistency and the way in which food is offered; supplementary gastrostomy tube feeds were considered and added by age 3) |
| Level of Sitting Scale (LSS) | 2 (requires support from the head down when placed in bench sitting with feet unsupported) |
| 5–8 Months | 9–11 Months | 12–14 Months | 15–18 Months | 19–24 Months | |
|---|---|---|---|---|---|
| Adaptive Seating | Commercial contoured foam seat | Custom wrap around seat in highchair | Custom saddle seat with tray on high-low base for feeding and play at home | ||
| Supported Standing | Equipment trials | Loan program—supine standing frame | |||
| Supported Stepping | Equipment trials | Anterior support stepping device with custom foam tray | |||
| Power Mobility | Specialized early power mobility device | Switch-adapted ride-on toys outdoors at home | Mini power wheelchair in therapy sessions | ||
| Manual Mobility | Standard twin stroller—reclined positioning | Loan program—dynamic manual wheelchair with custom adaptive seating | |||
| Jayde | Skyla | |||||||
| Age in Months | 12 | 15 | 18 | 24 | 12 | 15 | 18 | 24 |
| ALP | 1 | 2 | 3 | 3 | 1 | 2 | 3 | 3 |
| PMTT Non-Motor Skills | ||||||||
| Cause–effect: movement | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 |
| Cause–effect: direction | 0 | 0 | 1 | 2 | 0 | 0 | 1 | 2 |
| Stop and go | 1 | 2 | 3 | 3 | 1 | 2 | 3 | 3 |
| Visual skills | 3 | 4 | 4 | 4 | 3 | 4 | 4 | 4 |
| PMTT Motor Skills | ||||||||
| Activate | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 2 |
| Release | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 |
| Sustain > 5 s | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 |
| PMTT Driving Skills | ||||||||
| Forward 5 feet | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| Turn right | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 |
| Turn left | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 |
| Reverse | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maneuver | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| PMTT Total | 9/48 | 12/48 | 17/48 | 21/48 | 9/48 | 12/48 | 19/48 | 23/48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Livingstone, R.W.; Chin, A.J.; Paleg, G.S. Power Mobility, Supported Standing and Stepping Device Use in the First Two Years of Life: A Case Report of Twins Functioning at GMFCS V. Disabilities 2023, 3, 507-524. https://doi.org/10.3390/disabilities3040032
Livingstone RW, Chin AJ, Paleg GS. Power Mobility, Supported Standing and Stepping Device Use in the First Two Years of Life: A Case Report of Twins Functioning at GMFCS V. Disabilities. 2023; 3(4):507-524. https://doi.org/10.3390/disabilities3040032
Chicago/Turabian StyleLivingstone, Roslyn W., Angela J. Chin, and Ginny S. Paleg. 2023. "Power Mobility, Supported Standing and Stepping Device Use in the First Two Years of Life: A Case Report of Twins Functioning at GMFCS V" Disabilities 3, no. 4: 507-524. https://doi.org/10.3390/disabilities3040032
APA StyleLivingstone, R. W., Chin, A. J., & Paleg, G. S. (2023). Power Mobility, Supported Standing and Stepping Device Use in the First Two Years of Life: A Case Report of Twins Functioning at GMFCS V. Disabilities, 3(4), 507-524. https://doi.org/10.3390/disabilities3040032








