Enhancing Function, Fun and Participation with Assistive Devices, Adaptive Positioning, and Augmented Mobility for Young Children with Infantile-Onset Spinal Muscular Atrophy: A Scoping Review and Illustrative Case Report
Abstract
:1. Introduction
2. Methods
- Pediatric Evaluation of Disability Inventory (PEDI) caregiver assistance scale [28] was selected to describe Tom’s level of independence in self-care and functional mobility;
- Power mobility or driving skill measures also primarily fall under the Activity domain and were used to describe power mobility skill development over time;
- Assessment of Learning Powered Mobility (ALP) measures the power mobility skill process and is suitable for all ages, motor and cognitive abilities [29];
- Power Mobility Program (PMP) [30] measures abilities to complete a list of 34 power mobility tasks ranging from basic mobility to integrated skills in structured and unstructured environments;
- Power Mobility Training Tool (PMTT) [31] was developed to guide power mobility training for children at the very beginning stages of learning;
- One included measure is considered to address primarily the domain of Participation;
- Wheelchair Outcome Measure for Young People (WhOM-YP) [32] is an individualized, client-centered measure developed for children or young people who use wheeled mobility.
3. Results
3.1. Case Introduction and History
3.2. Current Functional Description
3.3. Postural Management
3.3.1. Lying or Night-Time Positioning
3.3.2. Seating
3.3.3. Standing
3.3.4. Orthotics
3.4. Mobility
3.4.1. Manual Mobility
3.4.2. Power Mobility
3.4.3. Gait Trainers and Dynamic Mobility Devices
3.4.4. Tricycle
3.5. Assistive Technologies
3.5.1. Augmentative and Alternative Communication
3.5.2. Arm Assists
4. Discussion
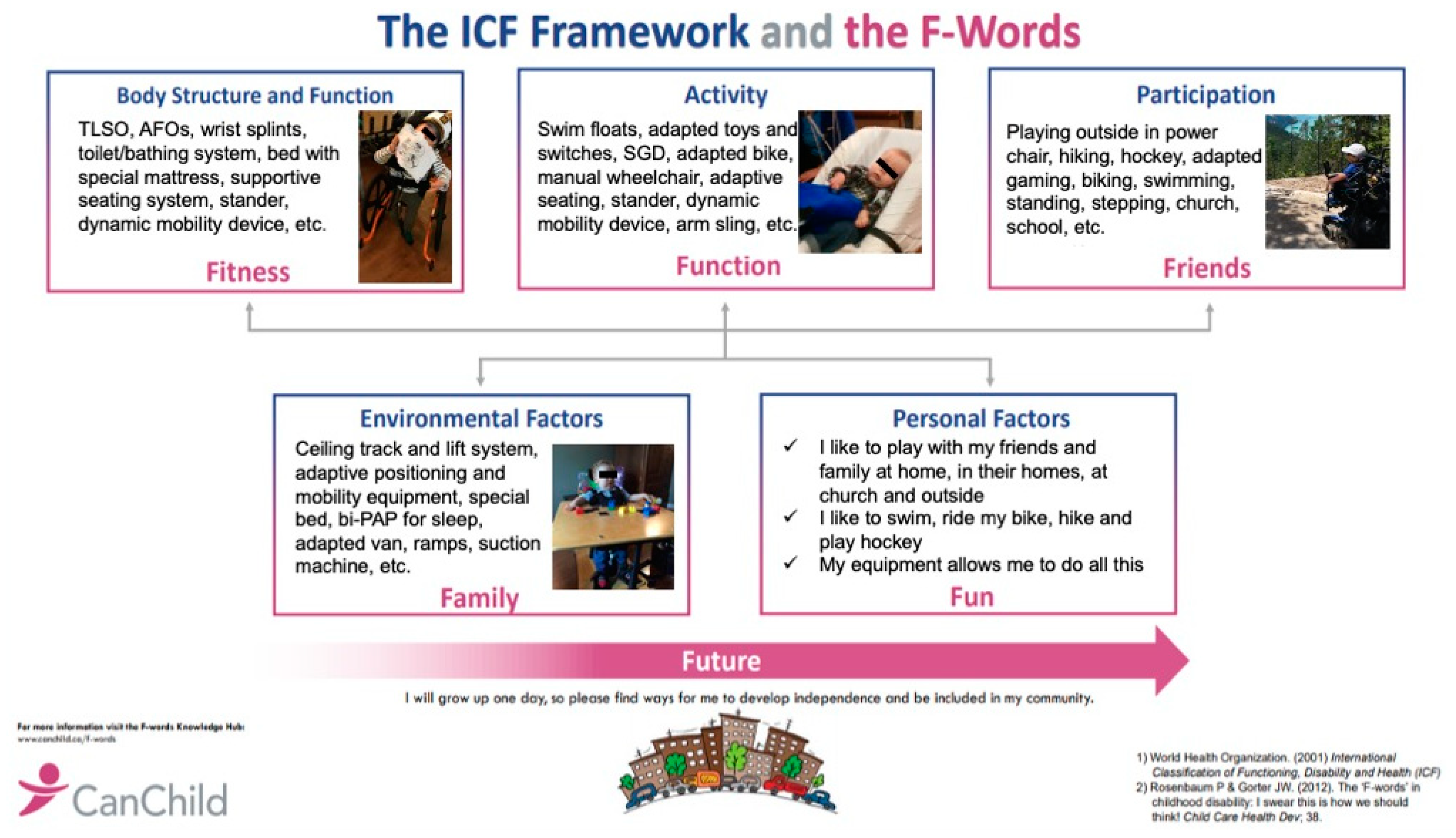
4.1. Fitness
4.2. Function
4.3. Friends
4.4. Family
4.5. Fun
4.6. Future
4.7. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Measures Included in Case Report
- Pediatric Evaluation of Disability Inventory (PEDI) caregiver assistance scale [28] describes the amount of assistance children require in activities of daily living, mobility and social skills. Items may be reported on a 6-point ordinal scale. Independent indicates the child can do the task alone; Supervision indicates verbal supervision is needed; Minimal indicates caregiver may need to provide a small amount of physical assistance, Moderate indicates the caregiver may complete up to half the task; Maximal indicates the caregiver does more than half the task but the child may provide a small amount of meaningful assistance; and Total indicates the child is completely dependent. The PEDI has demonstrated reliability and validity in multiple studies [38,65].
- Assessment of Learning Powered Mobility (ALP) measures the power mobility skill process and is suitable for all ages, motor and cognitive abilities [29]. It includes eight phases from novice (ALP 1) to expert (ALP 8). At phases 1 or 2 children are just beginning to explore effects of the switch or joystick and by phase 3 they establish cause-effect. At phases 4 and 5 children explore different effects and directional control. Basic steering control is demonstrated at phase 6 and at phase 7 they can use the power mobility device to participate in other activities. The ALP has established validity for a wide range of ages and abilities and inter-rater reliability has recently been established between experienced professionals (ICC2,1 0.83) [66] and between professionals and relatives or assistants (κw 0.85) [67].
- Power Mobility Program (PMP) [30] measures abilities to complete a list of 34 power mobility tasks ranging from basic mobility to integrated skills in structured and unstructured environments. It is scored on a 6-point ordinal scale depending on amount of assistance required from 1 (maximal assistance) to 5 (age-appropriate supervision). Maximum raw score is 170 and, where all items can be scored, total score can be divided by 34 for a summary score of 1–5 describing average assistance required. Good inter-rater reliability (κw 0.87) and fair intra-rater reliability (κw 0.52) was reported from repeated assessment of 9 children with physical disabilities in the original study [30]. Recently other researchers reported excellent intra-rater (ICC2,1 0.97/0.98) and good to excellent inter-rater reliability (ICC2,1 0.93/0.87) from assessment of 30 children over two occasions [66]. It has been widely used in paediatric power mobility research although concerns remain regarding its structure and content [54]. To illustrate sections more challenging to score in community settings (and with very young children with significant disabilities) we reported scoring separately from each section within the tool. Basic mobility skills include three sections: beginning skills (including ability to turn the wheelchair on/off); directional control; and speed control. Integration of basic skills in structured environments also has three sections: functional skills (doorways, hallways and curving paths); negotiating ramps; and negotiating sidewalks. The final section is integration of basic skills for functional mobility in unstructured environments and includes community mobility skills.
- Power Mobility Training Tool (PMTT) [31] was developed to guide power mobility training for children at the very beginning stages of learning. Content validity was established through multiple methods including review by an international expert panel. It includes non-motor, motor and driving skills subscales and items are scored on a 5-point ordinal scale for a maximum score of 48. A score of 1 indicates that the task can only be completed with assistance, 2 indicates independent demonstration less than 50%, 3 indicates independent demonstration more than 50% and a score of 4 means the child completes the task independently more than 90% of the time.
- Excellent Spearman correlations (0.83–0.92, p < 0.001) have been measured between PMTT, PMP and ALP scores [26].
- Wheelchair Outcome Measure for Young People (WhOM-YP) [32] is an individualized, client-centred measure developed for children or young people who use wheeled mobility. Depending on the child’s age or abilities, importance and satisfaction of meaningful participation-focused outcomes related to use of a wheeled mobility device may be rated either by the child or parent proxy. It is scored on an 11-point ordinal scale and has evidence of face and content validity with ability to discriminate known groups and good association between parent and child ratings. Test-retest reliability for parent proxy ratings is excellent (ICC2,1 0.85–0.90) and minimal detectible change (MDD95) has been estimated as 1.8 [32].
References
- Mercuri, E.; Finkel, R.S.; Muntoni, F.; Wirth, B.; Montes, J.; Main, M.; Mazzone, E.S.; Vitale, M.; Snyder, B.; Quijano-Roy, S.; et al. Diagnosis and management of spinal muscular atrophy: Part 1: Recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscul. Disord. 2018, 28, 103–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, C.H.; Finkel, R.S.; Bertini, E.S.; Schroth, M.; Simonds, A.; Wong, B.; Aloysius, A.; Morrison, L.; Main, M.; Crawford, T.O.; et al. Consensus statement for standard of care in spinal muscular atrophy. J. Child Neurol. 2007, 22, 1027–1049. [Google Scholar] [CrossRef] [PubMed]
- Oskoui, M.; Levy, G.; Garland, C.J.; Gray, J.M.; O’Hagen, J.; De Vivo, D.C.; Kaufmann, P. The changing natural history of spinal muscular atrophy type 1. Neurology 2007, 69, 1931–1936. [Google Scholar] [CrossRef] [PubMed]
- Kariyawasam, D.; Carey, K.A.; Jones, K.J.; Farrar, M.A. New and developing therapies in spinal muscular atrophy. Paediatr. Respir. Rev. 2018, 28, 3–10. [Google Scholar] [CrossRef]
- Finkel, R.S.; Mercuri, E.; Meyer, O.H.; Simonds, A.K.; Schroth, M.K.; Graham, R.J.; Kirschner, J.; Iannaccone, S.T.; Crawford, T.O.; Woods, S.; et al. Diagnosis and management of spinal muscular atrophy: Part 2: Pulmonary and acute care; medications, supplements and immunizations; other organ systems; and ethics. Neuromuscul. Disord. 2018, 28, 197–207. [Google Scholar] [CrossRef] [Green Version]
- Paganoni, S. Evidence-based physiatry: Pediatric neuromuscular rehabilitation in the era of precision medicine. Am. J. Phys. Med. Rehabil. 2018, 97, 920. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability and Health—Children and Youth; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Palisano, R.J.; Chiarello, L.A.; King, G.A.; Novak, I.; Stoner, T.; Fiss, A. Participation-based therapy for children with physical disabilities. Disabil. Rehabil. 2011, 34, 1041–1052. [Google Scholar] [CrossRef]
- Rosenbaum, P.; Gorter, J.W. The ‘F-words’ in childhood disability: I swear this is how we should think! Child Care Health Dev. 2012, 38, 457–463. [Google Scholar] [CrossRef]
- Humphreys, G.; King, T.; Jex, J.; Rogers, M.; Blake, S.; Thompson-Coon, J.; Morris, C. Sleep positioning systems for children and adults with a neurodisability: A systematic review. Br. J. Occup. Ther. 2018, 82, 5–14. [Google Scholar] [CrossRef]
- Ryan, S.E. An overview of systematic reviews of adaptive seating interventions for children with cerebral palsy: Where do we go from here? Disabil. Rehabil. Assist. Technol. 2011, 7, 104–111. [Google Scholar] [CrossRef]
- Angsupaisal, M.; Maathuis, C.G.B.; Hadders-Algra, M. Adaptive seating systems in children with severe cerebral palsy across International Classification of Functioning, Disability and Health for Children and Youth version domains: A systematic review. Dev. Med. Child Neurol. 2015, 57, 919–930. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.; Hilderman, C.; Wilson, G.; Misovic, R. Effectiveness of stretch interventions for children with neuromuscular disabilities: Evidence-based recommendations. Pediatr. Phys. Ther. 2016, 28, 262–275. [Google Scholar] [CrossRef] [PubMed]
- Paleg, G.; Smith, B.A.; Glickman, L.B. Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs. Pediatr. Phys. Ther. 2013, 25, 232–247. [Google Scholar] [CrossRef] [PubMed]
- Bray, N.; Kolehmainen, N.; McAnuff, J.; Tanner, L.; Tuersley, L.; Beyer, F.; Grayston, A.; Wilson, D.; Edwards, R.T.; Noyes, J.; et al. Powered mobility interventions for very young children with mobility limitations to aid participation and positive development: The EMPoWER evidence synthesis. Health Technol. Assess. 2020, 24, 1–194. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, R.W.; Field, D. Systematic review of power mobility outcomes for infants, children and adolescents with mobility limitations. Clin. Rehabil. 2014, 28, 954–964. [Google Scholar] [CrossRef]
- Livingstone, R.W.; Field, D. The child and family experience of power mobility: A qualitative synthesis. Dev. Med. Child Neurol. 2014, 57, 317–327. [Google Scholar] [CrossRef]
- Paleg, G.; Livingstone, R.W. Outcomes of gait trainer use in home and school settings for children with motor impairments: A systematic review. Clin. Rehabil. 2015, 29, 1077–1091. [Google Scholar] [CrossRef]
- Finkel, R.S.; Mercuri, E.; Darras, B.T.; Connolly, A.M.; Kuntz, N.L.; Kirschner, J.; Chiriboga, C.A.; Saito, K.; Servais, L.; Tizzano, E.; et al. Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N. Engl. J. Med. 2017, 377, 1723–1732. [Google Scholar] [CrossRef] [Green Version]
- Meylemans, A.; De Bleecker, J. Current evidence for treatment with Nusinersen for spinal muscular atrophy: A systematic review. Acta Neurol. Belg. 2019, 119, 523–533. [Google Scholar] [CrossRef] [Green Version]
- Aragon-Gawinska, K.; Seferian, A.M.; Daron, A.; Gargaun, E.; Vuillerot, C.; Cances, C.; Ropars, J.; Chouchane, M.; Cuppen, I.; Hughes, I.; et al. Nusinersen in patients older than 7 months with spinal muscular atrophy type 1. Neurology 2018, 91, e1312–e1318. [Google Scholar] [CrossRef]
- Dabbous, O.; Maru, B.; Jansen, J.P.; Lorenzi, M.; Cloutier, M.; Guérin, A.; Pivneva, I.; Wu, E.Q.; Arjunji, R.; Feltner, D.; et al. Survival, motor function, and motor milestones: Comparison of Avxs-101 relative to Nusinersen for the treatment of infants with spinal muscular atrophy type 1. Adv. Ther. 2019, 36, 1164–1176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations Human Rights. Convention on the Rights of the Child. Available online: https://www.ohchr.org/en/professionalinterest/pages/crc.aspx (accessed on 24 November 2020).
- Livingstone, R.W.; Bone, J.N.; Field, D.A. Beginning power mobility: An exploration of factors associated with child use of early power mobility devices and parent device preference. J. Rehabil. Assist. Technol. Eng. 2020, 7, 1–12. [Google Scholar] [CrossRef]
- Livingstone, R.W.; Field, D.A. Exploring change in young children’s power mobility skill following several months’ experience. Disabil. Rehabil. Assist. Technol. 2020, 1–10. [Google Scholar] [CrossRef]
- Livingstone, R.W.; Field, D.A. Exploring young children’s activity and participation change following 6 months’ power mobility experience. Br. J. Occup. Ther. 2020, 1–10. [Google Scholar] [CrossRef]
- Haley, S.; Coster, W.; Ludlow, L. Pediatric Evaluation of Disability Inventory: Development, Standardization and Administration Manual; New England Medical Center Publications: Boston, MA, USA, 1992. [Google Scholar]
- Nilsson, L.; Durkin, J. Assessment of learning powered mobility use—Applying grounded theory to occupational performance. J. Rehabil. Res. Dev. 2014, 51, 963–974. [Google Scholar] [CrossRef]
- Furumasu, J.; Guerette, P.; Tefft, D. The development of a powered wheelchair mobility program for young children. Technol. Disabil. 1996, 5, 41–48. [Google Scholar] [CrossRef]
- Kenyon, L.K.; Farris, J.P.; Cain, B.; King, E.; Vandenberg, A. Development and content validation of the power mobility training tool. Disabil. Rehabil. Assist. Technol. 2017, 13, 10–24. [Google Scholar] [CrossRef]
- Field, D.A.; Miller, W. The Wheelchair Outcome Measure for Young People (WhOM-YP): Modification and metrics for children and youth with mobility limitations. Disabil. Rehabil. Assist. Technol. 2020, 1–9. [Google Scholar] [CrossRef]
- Ball, L.; Chavez, S.; Perez, G.F.; Bharucha-Goebel, D.; Smart, K.; Kundrat, K.; Carruthers, L.; Brady, C.; Leach, M.; Evans, S. Communication skills among children with spinal muscular atrophy type 1: A parent survey. Assist. Technol. 2019, 2019, 1–11. [Google Scholar] [CrossRef]
- Dunaway, S.; Montes, J.; O’Hagen, J.; Sproule, D.M.; De Vivo, D.C.; Kaufmann, P. Independent mobility after early introduction of a power wheelchair in spinal muscular atrophy. J. Child Neurol. 2013, 28, 576–582. [Google Scholar] [CrossRef]
- Fujak, A.; Kopschina, C.; Forst, R.; Mueller, L.A.; Forst, J. Use of orthoses and orthopaedic technical devices in proximal spinal muscular atrophy. Results of survey in 194 SMA patients. Disabil. Rehabil. Assist. Technol. 2010, 6, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Paguinto, S.-G.; Kasparian, N.A.; Bray, P.; Farrar, M. “It’s not just the wheelchair, it’s everything else”: Australian parents’ perspectives of wheelchair prescription for children with neuromuscular disorders. Disabil. Rehabil. 2020, 42, 3457–3466. [Google Scholar] [CrossRef] [PubMed]
- Townsend, E.L.; Simeone, S.D.; Krosschell, K.J.; Zhang, R.Z.; Swoboda, K.J. Stander use in spinal muscular atrophy: Results from a large natural history database. Pediatr. Phys. Ther. 2020, 32, 235–241. [Google Scholar] [CrossRef]
- Jones, M.A.; McEwen, I.R.; Hansen, L. Use of power mobility for a young child with spinal muscular atrophy. Phys. Ther. 2003, 83, 253–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flodin, E. Interactive Design—The desire for autonomous upright mobility: A longitudinal case study. Technol. Disabil. 2008, 19, 213–224. [Google Scholar] [CrossRef]
- Gudgeon, S.; Kirk, S. Living with a powered wheelchair: Exploring children’s and young people’s experiences. Disabil. Rehabil. Assist. Technol. 2013, 10, 118–125. [Google Scholar] [CrossRef]
- Mandy, A.; Sims, T.; Stew, G.; Onions, D. Manual feeding device experiences of people with a neurodisability. Am. J. Occup. Ther. 2018, 72. [Google Scholar] [CrossRef]
- Sonday, A.; Gretschel, P. Empowered to play: A case study describing the impact of powered mobility on the exploratory play of disabled children. Occup. Ther. Int. 2016, 23, 11–18. [Google Scholar] [CrossRef]
- Rahman, T.; Sample, W.; Seliktar, R.; Scavina, M.T.; Clark, A.L.; Moran, K.; Alexander, M.A. Design and testing of a functional arm orthosis in patients with neuromuscular diseases. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 244–251. [Google Scholar] [CrossRef]
- Collange, L.; Rodini, C.; Juliano, Y.; Misao, M.H.; Isola, A.M.; Almeida, S.B. Influence of wheelchair positioning aids on the respiratory function of patients with type II spinal muscular atrophy. Fisioter Pesqui. 2009, 16, 229–232. [Google Scholar] [CrossRef] [Green Version]
- Rahman, T.; Sample, W.; Seliktar, R.; Alexander, M.; Scavina, M. A body-powered functional upper limb orthosis. J. Rehabil. Res. Dev. 2001, 37, 675–680. [Google Scholar]
- Paguinto, S.-G.; Kasparian, N.A.; Bray, P.; Farrar, M. Parents’ perceptions of power wheelchair prescription for children with a neuromuscular disorder: A scoping review. Disabil. Rehabil. 2018, 41, 2750–2757. [Google Scholar] [CrossRef]
- May, M.; Rugg, S. Electrically powered indoor/outdoor wheelchairs: Recipients’ views of their effects on occupational performance and quality of life. Br. J. Occup. Ther. 2010, 73, 2–12. [Google Scholar] [CrossRef]
- Butler, C.; Okamoto, G.A.; McKay, T.M. Powered mobility for very young disabled children. Dev. Med. Child Neurol. 2008, 25, 472–474. [Google Scholar] [CrossRef]
- Evans, N.; Baines, R. Trends, goals and outcomes for children and families using early powered mobility in a charitable loan scheme. J. Enabling Technol. 2017, 11, 138–147. [Google Scholar] [CrossRef]
- Everard, L. The wheelchair toddler. Health Visit. 1984, 57, 241–242. [Google Scholar]
- Livingstone, R.W.; Field, D.A.; Sanderson, C.; Pineau, N.; Zwicker, J.G. Beginning power mobility: Parent and therapist perspectives. Disabil. Rehabil. 2020, 1–10. [Google Scholar] [CrossRef]
- Bora, G.; Subaşı-Yıldız, Ş.; Yeşbek-Kaymaz, A.; Bulut, N.; Alemdaroğlu, I.; Tunca-Yılmaz, Ö.; Topaloğlu, H.; Karaduman, A.A.; Erdem-Yurter, H. Effects of arm cycling exercise in spinal muscular atrophy type II patients: A pilot study. J. Child Neurol. 2018, 33, 209–215. [Google Scholar] [CrossRef]
- Haumont, T.; Rahman, T.; Sample, W.; King, M.M.; Church, C.; Henley, J.; Jayakumar, S. Wilmington robotic exoskeleton: A novel device to maintain arm improvement in muscular disease. J. Pediatr. Orthop. 2011, 31, e44–e49. [Google Scholar] [CrossRef]
- Field, D.A.; Livingstone, R.W. Power mobility skill progression for children and adolescents: A systematic review of measures and their clinical application. Dev. Med. Child Neurol. 2018, 60, 997–1011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bottos, M.; Bolcati, C.; Sciuto, L.; Ruggeri, C.; Feliciangeli, A. Powered wheelchairs and independence in young children with tetraplegia. Dev. Med. Child Neurol. 2007, 43, 769–777. [Google Scholar] [CrossRef]
- Rosenberg, L.; Maeir, A.; Gilboa, Y. Feasibility study of a therapeutic mobility summer camp for children with severe cerebral palsy: Power fun. Phys. Occup. Ther. Pediatr. 2019, 40, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Zuluaga-Sanchez, S.; Teynor, M.; Knight, C.; Thompson, R.; Lundqvist, T.; Ekelund, M.; Forsmark, A.; Vickers, A.D.; Lloyd, A.J. Cost effectiveness of Nusinersen in the treatment of patients with infantile-onset and later-onset spinal muscular atrophy in Sweden. Pharmacoeconomics 2019, 37, 845–865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De, S.; Coomer, W.; Gerk, A.; Kwok, A.; Zhaoxing, P.; Oleszek, J.; Stratton, A.; Chang, F. Progression of hip instability in children with spinal muscular atrophy. Dev. Med. Child. Neurol. 2020, 62, 4–134. [Google Scholar]
- Hägglund, G.; Andersson, S.; Düppe, H.; Lauge-Pedersen, H.; Nordmark, E.; Westbom, L. Prevention of dislocation of the hip in children with cerebral palsy: 20 Year results of a population-based prevention programme. J. Bone Jt. Surgery. Br. Vol. 2005, 87, 95–101. [Google Scholar] [CrossRef] [Green Version]
- Ágústsson, A.; Sveinsson, T.; Pope, P.; Rodby-Bousquet, E. Preferred posture in lying and its association with scoliosis and windswept hips in adults with cerebral palsy. Disabil. Rehabil. 2019, 41, 3198–3202. [Google Scholar] [CrossRef]
- Pettersson, K.; Rodby-Bousquet, E. Prevalence and goal attainment with spinal orthoses for children with cerebral palsy. J. Pediatr. Rehabil. Med. 2019, 12, 197–203. [Google Scholar] [CrossRef] [Green Version]
- Ryan, S.E.; Sophianopoulos, M.-B. Measurement of assistive technology outcomes associated with computer-based writing interventions for children and youth with disabilities. Technologies 2017, 5, 19. [Google Scholar] [CrossRef] [Green Version]
- Hung, Y.-C.; Spingarn, A.; Friel, K.M.; Gordon, A.M. Intensive unimanual training leads to better reaching and head control than bimanual training in children with unilateral cerebral palsy. Phys. Occup. Ther. Pediatr. 2020, 40, 491–505. [Google Scholar] [CrossRef]
- Thokala, P.; Stevenson, M.; Kumar, V.M.; Ren, S.; Ellis, A.G.; Chapman, R.H. Cost effectiveness of Nusinersen for patients with infantile-onset spinal muscular atrophy in US. Cost Eff. Resour. Alloc. 2020, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.A.; McEwen, I.R.; Neas, B.R. Effects of power wheelchairs on the development and function of young children with severe motor impairments. Pediatr. Phys. Ther. 2012, 24, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Gefen, N.; Rigbi, A.; Weiss, P.L. (Tamar) Reliability and validity of pediatric powered mobility outcome measures. Disabil. Rehabil. Assist. Technol. 2020, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Svensson, E.; Nilsson, L. Inter-rater reliability of the assessment of learning powered mobility use, version 2.0, when applied with children and adults engaged in Driving to Learn in a powered wheelchair. Aust. Occup. Ther. J. 2020. [Google Scholar] [CrossRef] [PubMed]



| Citation | Design | Participants | N SMA-1 | Devices | Results |
|---|---|---|---|---|---|
| Ball et al., 2019 [33] | Internet-based survey | Parents of children diagnosed SMA-1 | 32 parents of individuals aged 6 months–30 years | Speech Generating Devices (SGD) | 12/32 used SGDs 13 used eye-gaze, 3 direct finger access and 4 switch access |
| Dunaway et al., 2013 [34] | Descriptive case-series | 6 children (5 SMA, 1 CMD) | 1 aged 34 months at PWC delivery | Power mobility | SMA-1 achieved basic skills in 260 days, directional control and doorway/corridor navigation in 458 days |
| Fujak et al., 2011 [35] | Descriptive retrospective cohort | 194 children and adults with SMA types 1–4, recruited from one specialized clinic | 14 aged 1.7–36.9 years | Orthotics Power mobility Manual mobility Standing frames | Use by SMA-1 (mean age at prescription ± SD) AFO—1 (4.7 years) TLSO—10 (6.0 years ± 4.9) PWC—6 (7.0 years: ± 3.9) Stroller—8 (ND) Stander—2 (ND) |
| Paguinto et al., 2019 [36] | Qualitative | Parents of 14 children with neuromuscular disorders aged 1–17 years | Parents of two children: SMA-1 aged 1 year and SMA1-2 aged 3.5 years | Manual or Power mobility | PWC recommendation offered hope, increased independence and participation. Child with SMA-1-2 prescribed PWC at 14 months. Child with SMA-1 provided early power mobility trial between 9 and 12 months. |
| Townsend et al., 2020 [37] | Descriptive retrospective multi-center cohort | 397 children SMA-1 and SMA-2 enrolled in natural history study 2004–2015 | 152 aged 0–4.5 years at enrolment who survived >9 months | Standing frames | 20 SMA-1 stood regularly ≥3 times a week Stander use from 6 months of age |
| Months | 9–12 | 13–15 | 16–18 | 19–21 | 22–24 | 25–27 | 28–30 | 31–33 | 34–36 | 37–39 | 40–42 | 43–45 | 46–48 | 49–51 | 52–54 | 55–57 | 58–60 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Night-time positioning | Air-filled mattress section. Positioned 3/4 prone with roll under top leg. | ||||||||||||||||||||
| Memory foam mattress. Side-lying or 3/4 prone with roll under top leg | |||||||||||||||||||||
| Seating | Reclined foam seat | ||||||||||||||||||||
| Custom seating with curved trunk laterals, medial and lateral pelvic and thigh supports and custom arm supports. | |||||||||||||||||||||
| Wooden tilt floor base | |||||||||||||||||||||
| Standing | Floor level supine stander. Stands in 10 degrees tilt 1 h twice daily | High level transfer supine stander. Stands fully upright 1 h twice daily | |||||||||||||||||||
| Orthotics | Solid AFO’s used 2 h daily in stander initially—progressed to using 10 h a day in wheelchairs, standing and other positions. Not in walker as weight limits leg movement. | ||||||||||||||||||||
| TLSO used for floor sitting, in floor level mobility device, manual wheelchair and in tricycle | |||||||||||||||||||||
| Custom wrist splints used at night-time to maintain ROM. Some daytime use to enhance function | |||||||||||||||||||||
| Manual mobility | Infant stroller | ||||||||||||||||||||
| Special needs stroller with full tilt and recline | |||||||||||||||||||||
| Home-made self-propelled floor level manual mobility device | |||||||||||||||||||||
| Microlite wheelchair with soft backrest and cushion. | Lightweight rigid wheelchair with cushion and curved backrest. | ||||||||||||||||||||
| Power mobility | Switch-adapted cart | ||||||||||||||||||||
| MPW with tilt and sensitive finger joystick | Pediatric power wheelchair with tilt and seat elevate. Accessed with micro extremity joystick | Pediatric power wheelchair with tilt and seat elevate. Accessed with mini proportional joystick | |||||||||||||||||||
| Dynamic mobility device | Hands-free device trial | Using 30 min daily | |||||||||||||||||||
| Tricycle | Special needs tricycle with high backrest, pelvic and chest harness and shoe holders. | ||||||||||||||||||||
| Other assistive technologies | Custom suspension arm support | ||||||||||||||||||||
| Tablet-based augmentative communication software | |||||||||||||||||||||
| 11 Months | 14 Months | 16 Months | 17 Months | 20 Months | 22 Months | |
|---|---|---|---|---|---|---|
| ALP | 1 | 2 | 3 | 6 | 7 | 7 |
| PMTT non-motor | 5/16 | 9/16 | 12/16 | 16/16 | 16/16 | 16/16 |
| PMTT motor | 4/12 | 5/12 | 6/12 | 12/12 | 12/12 | 12/12 |
| PMTT driving | 3/20 | 8/20 | 10/20 | 20/20 | 20/20 | 20/20 |
| PMP beginning | 4/30 | 8/30 | 9/30 | 25/30 | 25/30 | 25/30 |
| PMP directional | 2/35 | 4/35 | 5/35 | 30/35 | 30/35 | 30/35 |
| PMP speed control | 0/20 | 0/20 | 0/20 | 0/20 | 10/20 | 10/20 |
| PMP functional | 0/15 | 0/15 | 0/15 | 0/15 | 15/15 | 15/15 |
| PMP ramps | 0/30 | 0/30 | 0/30 | 0/30 | 5/30 | 18/30 |
| PMP sidewalks | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 |
| PMP community | 0/30 | 0/30 | 0/30 | 0/30 | 0/30 | 12/30 |
| Equipment | |
|---|---|
| Item | Cost in USD (website source where available) |
| Power wheelchair | USD 12,000–30,000 replacement every 5 years |
| Custom adaptive seating | USD 2000–4000 replacement at least every 2 years |
| Supine standing frame | USD 2000–4000 replacement every 5 years (www.adaptivemall.com) |
| Manual wheelchair | USD 2–6000 replacement every 5 years |
| Gait Trainer/Dynamic Mobility Device | USD 2000–4000 replacement every 5 years (www.adaptivemall.com) |
| AFO’s | USD 2000–4000 replacement every 1–2 years |
| TLSO | USD 2000–4000 replacement every 1–2 years |
| Wrist splints | USD 50–100 replacement every 1–2 years |
| Bath/Toilet Chair | USD 500–2000 (www.adaptivemall.com) |
| Ceiling Track lift system | USD 3500 |
| Adapted wheelchair van | USD 60–80,000 |
| Ramp for home accessibility | USD 400–2000 |
| Special-needs adapted tricycle | USD 600–2500 (www.adaptivemall.com) |
| SGD and communication software | USD 2000–10,000 depending on model and features |
| Car support harness | USD 200 (www.especialneeds.com) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Livingstone, R.; Paleg, G. Enhancing Function, Fun and Participation with Assistive Devices, Adaptive Positioning, and Augmented Mobility for Young Children with Infantile-Onset Spinal Muscular Atrophy: A Scoping Review and Illustrative Case Report. Disabilities 2021, 1, 1-22. https://doi.org/10.3390/disabilities1010001
Livingstone R, Paleg G. Enhancing Function, Fun and Participation with Assistive Devices, Adaptive Positioning, and Augmented Mobility for Young Children with Infantile-Onset Spinal Muscular Atrophy: A Scoping Review and Illustrative Case Report. Disabilities. 2021; 1(1):1-22. https://doi.org/10.3390/disabilities1010001
Chicago/Turabian StyleLivingstone, Roslyn, and Ginny Paleg. 2021. "Enhancing Function, Fun and Participation with Assistive Devices, Adaptive Positioning, and Augmented Mobility for Young Children with Infantile-Onset Spinal Muscular Atrophy: A Scoping Review and Illustrative Case Report" Disabilities 1, no. 1: 1-22. https://doi.org/10.3390/disabilities1010001
APA StyleLivingstone, R., & Paleg, G. (2021). Enhancing Function, Fun and Participation with Assistive Devices, Adaptive Positioning, and Augmented Mobility for Young Children with Infantile-Onset Spinal Muscular Atrophy: A Scoping Review and Illustrative Case Report. Disabilities, 1(1), 1-22. https://doi.org/10.3390/disabilities1010001





