Perspectives Matter: Insecure Residency Status Accounts for Aggressive Emotions in Adolescent Refugees
Abstract
1. Introduction
- Adolescent refugees with insecure residency status will show higher levels of psychological distress, aggressive emotions, and PTSD symptoms compared to individuals with secure residency status.
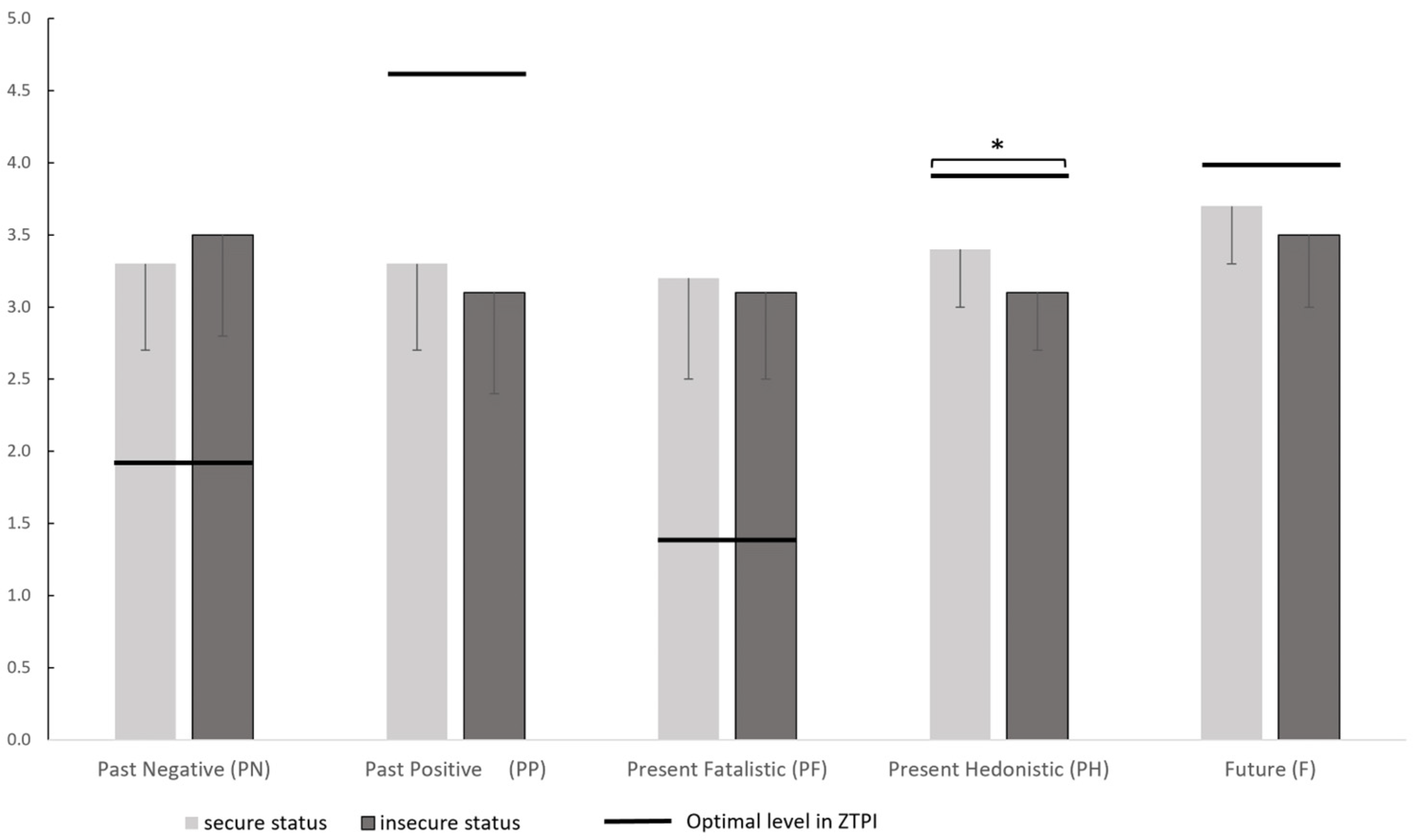
- Adolescent refugees with insecure residency status will exhibit lower orientation to F and lower orientation to PH compared to refugees with secure residency status.
- Compared to adolescent refugees with secure residency status, individuals with insecure residency status will show higher levels of aggressive emotions.
2. Materials and Methods
2.1. Participants and Procedure
2.2. Ethics Statement
2.3. Measures
2.3.1. Time Perspective Inventory (ZTPI)
2.3.2. Impact of Event Scale (IES-R)
2.3.3. Brief Symptom Checklist (BSCL)
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Time Perspectives
3.3. Psychological Distress, PTSD Symptoms and Aggressive Emotions
4. Discussion
4.1. Limitations
4.2. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations High Commissioner for Refugees. Global Trends, Forced Displacement in 2022. June 2023. Available online: https://www.unhcr.org/global-trends-report-2022 (accessed on 20 December 2023).
- Bradby, H.; Humphris, R.; Newall, D.; Philimore, J. Health Evidence Network Synthesis Report 44, Public Health Aspects of Migrant Health: A Review of the Evidence on Health Status for Refugees and Asylum Seekers in the European Region; World Health Organization: Copenhagen, Denmark, 2015. [Google Scholar]
- Schubert, S.; Kluge, U.; Klapprott, F.; Ringeisen, T. German’s awareness of refugees’ information barriers regarding health care access: A cross sectional study. BMC Health Serv. Res. 2023, 23, 221. [Google Scholar] [CrossRef] [PubMed]
- Reis, R.; Crone, M.R.; Berckmoes, L.H. Unpacking context and culture in mental health pathways of child and adolescent refugees. In Child, Adolescent and Family Refugee Mental Health, a Global Perspective; Song, S.J., Ventevogel, P., Eds.; Springer: Cham, Switzerland, 2020; pp. 37–51. [Google Scholar]
- Sam, D.L.; Berry, J.W. Acculturation: When individuals and groups of different cultural backgrounds meet. Perspect. Psychol. Sci. 2010, 5, 472–481. [Google Scholar] [CrossRef]
- Phinney, J.S. Acculturation is not an independent variable: Approaches to studying acculturation as a complex process. In Acculturation and Parent Child Relationships, Measurement and Development; Bornstein, M.H., Cote, M.H.L., Eds.; Routledge: New York, NY, USA, 2006; pp. 79–95. [Google Scholar]
- Ward, C.; Kus, L. Back to and beyond Berry’s basics: The conceptualization, operationalization and classification of acculturation. Int. J. Intercult. Relat. 2012, 36, 472–485. [Google Scholar] [CrossRef]
- Batista Pinto Wiese, E.; Burhorst, I. The mental health of asylum-seeking and refugee children and adolescents attending a clinic in the Netherlands. Transcult. Psychiatry 2007, 44, 596–613. [Google Scholar] [CrossRef] [PubMed]
- Müller, L.R.; Büter, K.P.; Rosner, R.; Unterhitzenberger, J. Mental health and associated stress factors in accompanied and unaccompanied refugee minors resettled in Germany: A cross-sectional study. Child Adolesc. Psychiatry Ment. Health 2019, 13, 8. [Google Scholar] [CrossRef]
- Ruf, M.; Schauer, M.; Elbert, T. Prevalence of traumatic stress and mental health problems in children of asylum-seekers in Germany. Z. Für Klin. Psychol. Und Psychother. 2010, 39, 151–160. [Google Scholar] [CrossRef]
- Kien, C.; Sommer, I.; Faustmann, A.; Gibson, L.; Schneider, M.; Krczal, E.; Jank, R.; Klerings, I.; Szelag, M.; Kerschner, B.; et al. Prevalence of mental disorders in young refugees and asylum seekers in European Countries: A systematic review. Eur. Child Adolesc. Psychiatry 2019, 28, 1295–1310. [Google Scholar] [CrossRef]
- Daniel-Calveras, A.; Baldaquí, N.; Baeza, I. Mental health of unaccompanied refugee minors in Europe: A systematic review. Child Abus. Negl. 2022, 133, 105864. [Google Scholar] [CrossRef]
- Walg, M.; Fink, E.; Großmeier, M.; Hapfelmeier, G. The proportion of unaccompanied refugee minors suffering from psychiatric disorders in Germany. Z. Für Kinder-Und Jugendpsychiatrie Und Psychother. 2016, 45, 58–68. [Google Scholar] [CrossRef]
- Höhne, E.; Banaschewski, T.; Bajbouj, M.; Böge, K.; Sukale, T.; Kamp-Becker, I. Prevalences of mental distress and its associated factors in unaccompanied refugee minors in Germany. Eur. Child Adolesc. Psychiatry 2023, 32, 1211–1217. [Google Scholar] [CrossRef]
- Witt, A.; Rassenhofer, M.; Fegert, J.M.; Plener, P.L. Demand for help and provision of services in the care of unaccompanied refugee minors: A systematic review. Kindh. Und Entwickl. 2015, 24, 209–224. [Google Scholar] [CrossRef]
- Hargasser, B. Unbegleitete Minderjährige Flüchtlinge, Sequentielle Traumatisierungsprozesse und Die Aufgaben der Jugendhilfe; Brandes & Apsel: Frankfurt am Main, Germany, 2014. [Google Scholar]
- United Nations High Commissioner for Refugees. Refugee and Migrant Children in Europe Accompanied, Unaccompanied and Separated, Overview of Trends January to December 2021. July 2022. Available online: https://data.unhcr.org/en/documents/details/94351 (accessed on 20 December 2023).
- United Nations High Commissioner for Refugees. Desperate Journeys, Refugees and Migrants Arriving in Europe and at Europe’s Borders, January–December 2018. January 2019. Available online: https://www.unhcr.org/desperatejourneys/ (accessed on 20 December 2023).
- Huemer, J.; Karnik, N.S.; Voelkl-Kernstock, S.; Granditsch, E.; Dervic, K.; Friedrich, M.H.; Steiner, H. Mental health issues in unaccompanied refugee minors. Child Adolesc. Psychiatry Ment. Health 2009, 3, 13. [Google Scholar] [CrossRef] [PubMed]
- Jensen, T.K.; Fjermestad, K.W.; Granly, L.; Wilhelmsen, N.H. Stressful life experiences and mental health problems among unaccompanied asylum-seeking children. Clin. Child Psychol. Psychiatry 2015, 20, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Zimbardo, P.; Sword, R.; Sword, R. The Time Cure: Overcoming PTSD with the New Psychology of Time Perspective Therapy; John Wiley & Sons: New York, NY, USA, 2012. [Google Scholar]
- Zimbardo, P.G.; Boyd, J.N. Putting time in perspective: A valid, reliable individual-differences metric. In Time Perspective Theory: Review, Research and Application: Essays in Honor of Philip G. Zimbardo; Stolarski, M., Fieulaine, N., van Beek, W., Eds.; Springer: Cham, Switzerland, 2015; pp. 17–56. [Google Scholar]
- Zimbardo, P.G.; Boyd, J.N. The Time Paradox: The New Psychology of Time That Will Change Your Life; Free Press, Simon & Schuster: New York, NY, USA, 2008. [Google Scholar]
- Stolarski, M.; Wiberg, B.; Osin, E. Assessing temporal harmony: The issue of a balanced time perspective. In Time Perspective Theory: Review, Research and Application: Essays in Honor of Philip G. Zimbardo; Stolarski, M., Fieulaine, N., van Beek, W., Eds.; Springer: Cham, Switzerland, 2015; pp. 57–71. [Google Scholar]
- Van Beek, W.; Berghuis, H.; Kerkhof, A.; Beekman, A. Time perspective, personality and psychopathology: Zimbardo’s time perspective inventory in psychiatry. Time Soc. 2010, 20, 364–374. [Google Scholar] [CrossRef]
- Tomich, P.L.; Tolich, A.; DeMalio, I. Strive for balance: Deviation from a balanced time perspective mediates the relationship between lifetime trauma exposure and PTSD symptoms. Curr. Psychol. 2022, 41, 8103–8111. [Google Scholar] [CrossRef]
- Wang, Y.; Hu, X.; Han, J.; Scalabrini, A.; Hu, Y.; Hu, Z.; Tan, Z.; Zhang, J.; Northoff, G. Time is of essence—Abnormal time perspectives mediate the impact of childhood trauma on depression severity. J. Psychiatr. Res. 2021, 137, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Walg, M.; Eder, L.L.; Martin, A.; Hapfelmeier, G. Distorted time perspective in adolescent Afghan and Syrian refugees is associated with psychological distress. J. Nerv. Ment. Dis. 2020, 208, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Papastamatelou, J.; Unger, A.; Zachariadis, A. Time perspectives and proneness to PTSD among Syrian refugees in Greece. J. Loss Trauma 2021, 26, 375–388. [Google Scholar] [CrossRef]
- Stolarski, M.; Zajenkowski, M.; Zajenkowska, A. Aggressive? From time to time… uncovering the complex associations between time perspectives and aggression. Curr. Psychol. 2016, 35, 506–515. [Google Scholar] [CrossRef]
- Walg, M.; Löwer, F.; Bender, S.; Hapfelmeier, G. Domain-specific discrepancies between self- and caseworkers’ proxy-reports of emotional and behavioral difficulties in unaccompanied refugees. Emot. Behav. Difficulties 2022, 27, 163–177. [Google Scholar] [CrossRef]
- Grimm, T.; Georgiadou, E.; Silbermann, A.; Junker, K.; Nisslbeck, W.; Erim, Y. Distress, main burdens, engagement motivators and needs of full-time and volunteer refugee aid workers. Psychother. Psychosom. Med. Psychol. 2017, 67, 345–351. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Wachington, DC, USA, 2013. [Google Scholar]
- Bègue, L.; Nguyen, D.; Vezirian, K.; Zerhouni, O.; Bricout, V. Psychological distress mediates the connection between sleep deprivation and physical fighting in adolescents. Aggress. Behav. 2022, 48, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.E.; Rasmussen, A. The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiol. Psychiatr. Sci. 2017, 26, 129–138. [Google Scholar] [CrossRef]
- Scharpf, F.; Kaltenbach, E.; Nickerson, A.; Hecker, T. A systematic review of socio-ecological factors contributing to risk and protection of the mental health of refugee children and adolescents. Clin. Psychol. Rev. 2021, 83, 101930. [Google Scholar] [CrossRef] [PubMed]
- Carswell, K.; Blackburn, P.; Barker, C. The relationship between trauma, post-migration problems and the psychological well-being of refugees and asylum seekers. Int. J. Soc. Psychiatry 2011, 57, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Vromans, L.; Schweitzer, R.D.; Brough, M.; Kobe, M.A.; Correa-Velez, I.; Farrell, L.; Murray, K.; Lenette, C.; Sagar, V. Persistent psychological distress in resettled refugee women-at-risk at one-year follow-up: Contributions of trauma, post-migration problems, loss, and trust. Transcult. Psychiatry 2021, 58, 157–171. [Google Scholar] [CrossRef] [PubMed]
- Hajak, V.L.; Sardana, S.; Verdeli, H.; Grimm, S. A systematic review of factors affecting mental health and well-being of asylum seekers and refugees in Germany. Front. Psychiatry 2021, 12, 643704. [Google Scholar] [CrossRef]
- Walther, L.; Fuchs, L.M.; Schupp, J.; von Scheve, C. Living conditions and the mental health and well-being of refugees: Evidence from a large-scale German survey. J. Immigr. Minor. Health 2020, 22, 903–913. [Google Scholar] [CrossRef]
- Laban, C.J.; Gernaat, H.B.; Komproe, I.H.; Schreuders, B.A.; De Jong, J.T. Impact of a long asylum procedure on the prevalence of psychiatric disorders in Iraqi asylum seekers in The Netherlands. J. Nerv. Ment. Dis. 2004, 192, 843–851. [Google Scholar] [CrossRef]
- Brune, M.; Eiroà-Orosa, F.J.; Fischer-Ortman, J.; Haasen, C. Effectiveness of psychotherapy for traumatized refugees without a secure residency status. Int. J. Migr. Health Soc. Care 2014, 10, 52–59. [Google Scholar] [CrossRef]
- Müller, L.R.; Gossmann, K.; Hartmann, F.; Büter, K.P.; Rosner, R.; Unterhitzenberger, J. 1-year follow-up of the mental health and stress factors in asylum-seeking children and adolescents resettled in Germany. BMC Public Health 2019, 19, 908. [Google Scholar] [CrossRef] [PubMed]
- Li, S.S.; Liddell, B.J.; Nickerson, A. The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Curr. Psychiatry Rep. 2016, 18, 82. [Google Scholar] [CrossRef] [PubMed]
- Hornfeck, F.; Sowade, C.; Bovenschen, I. Effects of the asylum process on the mental health of unaccompanied young refugees—A scoping review. Child. Youth Serv. Rev. 2022, 137, 106490. [Google Scholar] [CrossRef]
- Leerkes, A.; Engbersen, G.; Snel, E.; de Boom, J. Civic stratification and crime: A comparison of asylum migrants with different legal statuses. Crime Law Soc. Chang. 2018, 69, 41–66. [Google Scholar] [CrossRef]
- Bundesamt für Migration und Flüchtlinge. (2023, January). Schlüsselzahlen Asyl 1. Halbjahr 2023. July 2023. Available online: https://www.bamf.de/SharedDocs/Anlagen/DE/Statistik/SchluesselzahlenAsyl/flyer-schluesselzahlen-asyl-HJ01-2023.html (accessed on 20 December 2023).
- Deutscher Bundestag. Bericht der Bundesregierung über die Evaluation des Gesetzes zur Verbesserung der Unterbringung, Versorgung und Betreuung Ausländischer Kinder und Jugendlicher und über die Situation Unbegleiteter Ausländischer Minderjähriger in Deutschland. July 2021. Available online: https://b-umf.de/src/wp-content/uploads/2023/02/bericht-der-bundesregierung-2021.pdf (accessed on 20 December 2023).
- Zimbardo, P.G.; Boyd, J. Putting time in perspective: A valid, reliable individual differences metric. J. Personal. Soc. Psychol. 1999, 77, 1271–1288. [Google Scholar] [CrossRef]
- Weiss, D.S.; Marmar, C.R. The impact of event scale—Revised. In Assessing Psychological Trauma and PTSD; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 399–411. [Google Scholar]
- Franke, G.H. BSCL-Brief-Symptom-Checklist; Hogrefe: Göttingen, Germany, 2017. [Google Scholar]
- Davey, C.; Heard, R.; Lennings, C. Development of the Arabic versions of the Impact of Events Scale-Revised and the posttraumatic growth inventory to assess trauma and growth in middle eastern refugees in Australia. Clin. Psychol. 2014, 19, 131–139. [Google Scholar] [CrossRef]
- Guillemin, F.; Bombardier, C.; Beaton, D. Cross-Cultural Adaptation of Health-Related Quality of Life Measures: Literature Review and Proposed Guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef]
- Zimbardo, P.; Sword, R.; Sword, R. Die Zeitperspektiven-Therapie, Posttraumatische Belastungsstörungen Behandeln; Huber: Bern, Switzerland, 2013. [Google Scholar]
- Sircova, A.; van de Vijver, F.J.; Osin, E.; Milfont, T.L.; Fieulaine, N.; Kislali-Erginbilgic, A.; Zimbardo, P.G.; Djarallah, S.; Chorfi, M.S.; Leite, U.; et al. A global look at time: A 24-country study of the equivalence of the Zimbardo Time Perspective Inventory. SAGE Open 2014, 4. [Google Scholar] [CrossRef]
- Danner, D.; Treiber, L.; Bosnjak, M. Development and psychometric evaluation of a short version of the time perspective inventory. Eur. J. Psychol. Assess. 2019, 35, 172–181. [Google Scholar] [CrossRef]
- Maercker, A.; Schützwohl, M. Erfassung von psychischen Belastungsfolgen: Die Impact of Event Skala-revidierte Version. Diagnostica 1998, 44, 130–141. [Google Scholar]
- Beck, J.G.; Grant, D.M.; Read, J.P.; Clapp, J.D.; Coffey, S.F.; Miller, L.M.; Palyo, S.A. The impact of event scale -revised: Psychometric properties in a sample of motor vehicle accident survivors. J. Anxiety Disord. 2008, 22, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Morina, N.; Ehring, T.; Priebe, S. Diagnostic utility of the impact of event scale-revised in two samples of survivors of war. PLoS ONE 2013, 8, e83916. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R. The SCL-90-R: Administration, Scoring and Procedures Manual, 3rd ed.; National Computer Systems: Minneapolis, MN, USA, 1994. [Google Scholar]
- Boniwell, I.; Osin, E.; Linley, P.A.; Ivanchenko, G.V. A question of balance: Time perspective and well-being in British and Russian samples. J. Posit. Psychol. 2010, 5, 24–40. [Google Scholar] [CrossRef]
- Carelli, M.G.; Wiberg, B.; Wiberg, M. Development and construct validation of the Swedish Zimbardo Time Perspective Inventory. Eur. J. Psychol. Assess. 2011, 27, 220–227. [Google Scholar] [CrossRef]
- Choy, B.; Arunachalam, K.; Gupta, S.; Taylor, M.; Lee, A. Systematic review: Acculturation strategies and their impact on the mental health of migrant populations. Public Health Pract. 2021, 2, 100069. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, N.; Rodgers, R.F.; Bui, E.; Pirlot, G.; Chabrol, H. Relations between acculturation orientations and antisocial behavior in adolescents and young adults from immigrant families. Int. J. Cult. Ment. Health 2012, 7, 68–82. [Google Scholar] [CrossRef]
- Phillimore, J. Refugees, acculturation strategies, stress and integration. J. Soc. Policy 2011, 40, 575–593. [Google Scholar] [CrossRef]
- Mairean, C.; Diaconu-Gherasim, L.R. The relation between time perspective and posttraumatic stress symptoms: The mediating role of traffic locus of control. Personal. Individ. Differ. 2022, 192, 111586. [Google Scholar] [CrossRef]
- Bamford, J.; Fletcher, M.; Leavey, G. Mental health outcomes of unaccompanied refugee minors: A rapid review of recent research. Curr. Psychiatry Rep. 2021, 23, 46. [Google Scholar] [CrossRef]
- Mohwinkel, L.-M.; Nowak, A.C.; Kasper, A.; Razum, O. Gender differences in the mental health of unaccompanied refugee minors in Europe: A systematic review. BMJ Open 2018, 8, e022389. [Google Scholar] [CrossRef]
- Hanewald, B.; Knipper, M.; Fleck, W.; Pons-Kühnemann, J.; Hahn, E.; Ta, T.M.T.; Brosig, B.; Gallhofer, B.; Mulert, C.; Stingl, M. Different patterns of mental health problems in unaccompanied refugee minors (URM): A sequential mixed method study. Front. Psychiatry 2020, 11, 324. [Google Scholar] [CrossRef] [PubMed]
- Worell, F.C.; Temple, E.C.; McKay, M.T.; Zivkovic, U.; Perry, J.L.; Mello, Z.R.; Musil, B.; Cole, J.C. A theoretical approach to resolving the psychometric problems associated with the Zimbardo time perspective inventory. Eur. J. Psychol. Assess. 2018, 34, 41–51. [Google Scholar] [CrossRef]
- Song, S.J.; Ventevogel, P. Principles of the mental health assessment of refugee children and adolescents. In Child, Adolescent and Family Refugee Mental Health, a Global Perspective; Song, S.J., Ventevogel, P., Eds.; Springer: Cham, Switzerland, 2020; pp. 69–80. [Google Scholar]
- Hvidtfeldt, C.; Schultz-Nielsen, M.L.; Tekin, E.; Fosgerau, M. An estimate of the effect of waiting time in the Danish asylum system on post-resettlement employment among refugees: Separating the pure delay effect from the effects of the conditions under which refugees are waiting. PLoS ONE 2018, 13, e0206737. [Google Scholar] [CrossRef] [PubMed]
- Bakker, L.; Dagevos, J.; Engbersen, G. The importance of resources and security in the socio-economic integration of refugees. A study on the impact of length of stay in asylum accommodation and residence status on socio-economic integration for the four largest refugee groups in the Netherlands. Int. Migr. Integr. 2014, 15, 431–448. [Google Scholar] [CrossRef]
- Schick, M.; Zumwald, A.; Knöpfli, B.; Nickerson, A.; Bryant, R.A.; Schnyder, U.; Müller, J.; Morina, N. Challenging future, challenging past: The relationship of social integration and psychological impairment in traumatized refugees. Eur. J. Psychotraumatol. 2016, 7, 28057. [Google Scholar] [CrossRef]
| Scale | Arabic Version | Dari Version |
|---|---|---|
| ZTPI scales | ||
| Past Negative | 0.78 | 0.73 |
| Past Positive | 0.61 | 0.68 |
| Present Fatalistic | 0.82 | 0.63 |
| Present Hedonistic | 0.63 | 0.53 |
| Future | 0.72 | 0.54 |
| IES-R | 0.91 | 0.95 |
| BSCL scales | ||
| Total distress GSI | 0.97 | 0.92 |
| Anger-hostility | 0.81 | 0.83 |
| Total | Secure Status | Insecure Status | Subgroup Comparison | ||||
|---|---|---|---|---|---|---|---|
| (N = 33) | (n = 17) | (n = 16) | U | z | p | d | |
| ZTPI scales (M ± SD) | |||||||
| Past Negative | 3.4 ± 0.6 | 3.3 ± 0.6 | 3.5 ± 0.7 | 111.5 | −0.9 | 0.38 | 0.3 |
| Past Positive | 3.2 ± 0.7 | 3.3 ± 0.6 | 3.1 ± 0.7 | 104.0 | −1.2 | 0.26 | 0.4 |
| Present Fatalistic | 3.1 ± 0.7 | 3.2 ± 0.7 | 3.1 ± 0.6 | 111.5 | −0.9 | 0.38 | 0.3 |
| Present Hedonistic | 3.3 ± 0.4 | 3.4 ± 0.4 | 3.1 ± 0.4 | 70.5 | −2.4 | 0.02 | 0.9 |
| Future | 3.6 ± 0.5 | 3.7 ± 0.4 | 3.5 ± 0.5 | 113.0 | −0.8 | 0.42 | 0.3 |
| IES-R (M ± SD) | 42.1 ± 19.6 | 36.4 ± 20.1 | 48.1 ± 17.9 | 89.5 | −1.7 | 0.09 | 0.6 |
| BSCL scales (M ± SD) | |||||||
| Total distress GSI | 1.4 ± 0.7 | 1.0 ± 0.7 | 1.9 ± 0.4 | 41.0 | −3.4 | 0.001 | 1.5 |
| Anger-hostility | 1.2 ± 0.7 | 0.9 ± 0.7 | 1.5 ± 0.5 | 69.5 | −2.4 | 0.02 | 0.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eder, L.L.; Martin, A.; Hapfelmeier, G.; Walg, M. Perspectives Matter: Insecure Residency Status Accounts for Aggressive Emotions in Adolescent Refugees. Adolescents 2024, 4, 28-40. https://doi.org/10.3390/adolescents4010003
Eder LL, Martin A, Hapfelmeier G, Walg M. Perspectives Matter: Insecure Residency Status Accounts for Aggressive Emotions in Adolescent Refugees. Adolescents. 2024; 4(1):28-40. https://doi.org/10.3390/adolescents4010003
Chicago/Turabian StyleEder, Lara L., Alexandra Martin, Gerhard Hapfelmeier, and Marco Walg. 2024. "Perspectives Matter: Insecure Residency Status Accounts for Aggressive Emotions in Adolescent Refugees" Adolescents 4, no. 1: 28-40. https://doi.org/10.3390/adolescents4010003
APA StyleEder, L. L., Martin, A., Hapfelmeier, G., & Walg, M. (2024). Perspectives Matter: Insecure Residency Status Accounts for Aggressive Emotions in Adolescent Refugees. Adolescents, 4(1), 28-40. https://doi.org/10.3390/adolescents4010003






