Parental Dieting and Correlation with Disordered Eating Behaviours in Adolescents: A Narrative Review
Abstract
:1. Introduction
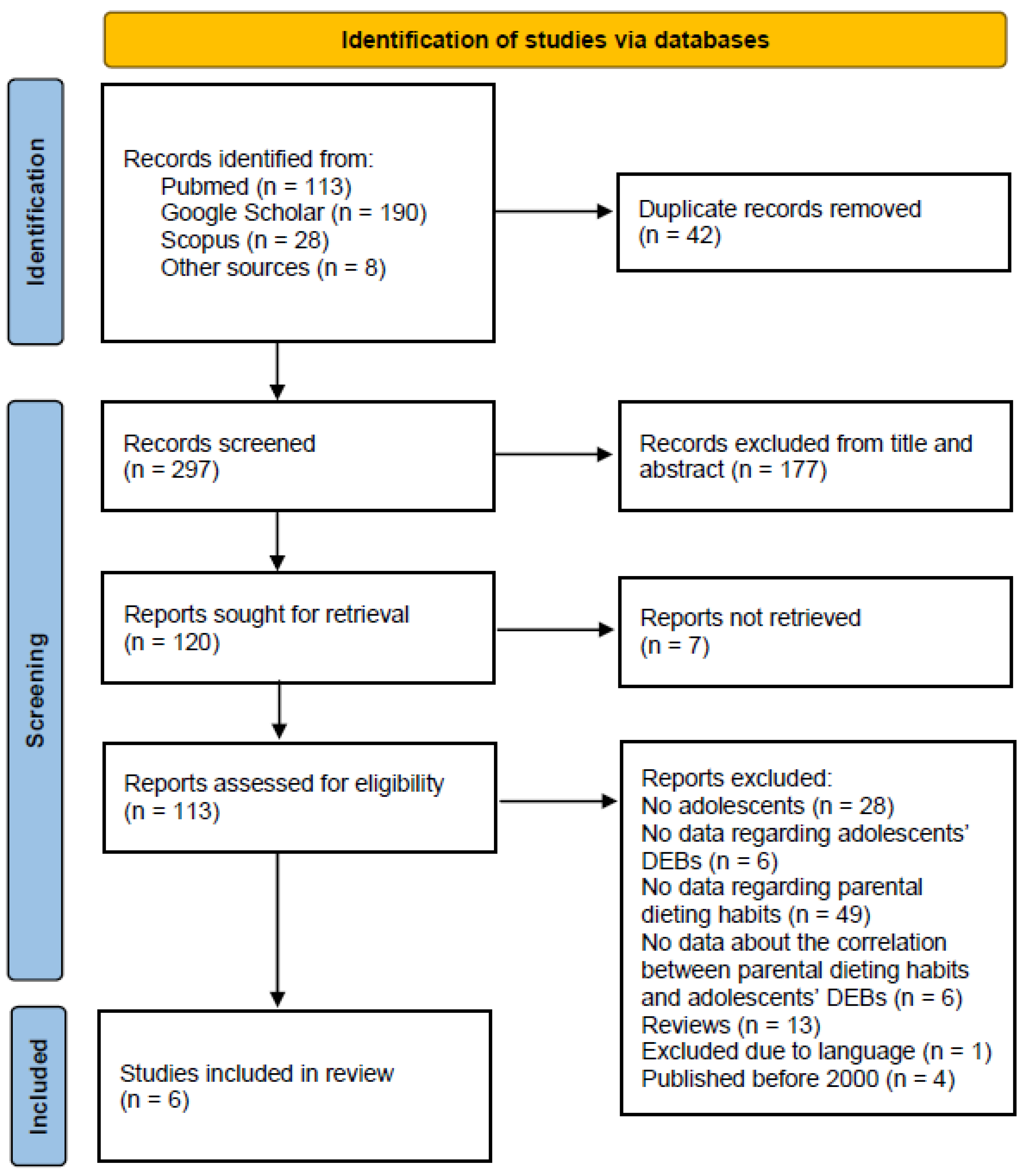
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Eligibility Criteria
3. Results
3.1. Eligible Studies
3.2. Characteristics of Eligible Studies and Population
3.3. Correlations between Parental Dieting and Adolescents’ Disordered Eating Behaviours
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Silén, Y.; Keski-Rahkonen, A. Worldwide Prevalence of DSM-5 Eating Disorders among Young People. Curr. Opin. Psychiatry 2022, 35, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Galmiche, M.; Déchelotte, P.; Lambert, G.; Tavolacci, M.P. Prevalence of Eating Disorders over the 2000–2018 Period: A Systematic Literature Review. Am. J. Clin. Nutr. 2019, 109, 1402–1413. [Google Scholar] [CrossRef] [PubMed]
- Hay, P.; Aouad, P.; Le, A.; Marks, P.; Maloney, D.; Barakat, S.; Boakes, R.; Brennan, L.; Bryant, E.; Byrne, S.; et al. Epidemiology of Eating Disorders: Population, Prevalence, Disease Burden and Quality of Life Informing Public Policy in Australia—A Rapid Review. J. Eat. Disord. 2023, 11, 23. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 978-0-89042-555-8. [Google Scholar]
- Shisslak, C.M.; Crago, M.; Estes, L.S. The Spectrum of Eating Disturbances. Int. J. Eat. Disord. 1995, 18, 209–219. [Google Scholar] [CrossRef]
- Stice, E.; Ng, J.; Shaw, H. Risk Factors and Prodromal Eating Pathology. J. Child Psychol. Psychiatry 2010, 51, 518–525. [Google Scholar] [CrossRef]
- Mancine, R.P.; Gusfa, D.W.; Moshrefi, A.; Kennedy, S.F. Prevalence of Disordered Eating in Athletes Categorized by Emphasis on Leanness and Activity Type—A Systematic Review. J. Eat. Disord. 2020, 8, 47. [Google Scholar] [CrossRef]
- Murray, S.B.; Blashill, A.J.; Calzo, J.P. Prevalence of Disordered Eating and Associations With Sex, Pubertal Maturation, and Weight in Children in the US. JAMA Pediatr. 2022, 176, 1039–1040. [Google Scholar] [CrossRef]
- Littleton, H.L.; Ollendick, T. Negative Body Image and Disordered Eating Behavior in Children and Adolescents: What Places Youth at Risk and How Can These Problems Be Prevented? Clin. Child Fam. Psychol. Rev. 2003, 6, 51–66. [Google Scholar] [CrossRef]
- Klump, K.L. Puberty as a Critical Risk Period for Eating Disorders: A Review of Human and Animal Studies. Horm. Behav. 2013, 64, 399–410. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F.; García-Hermoso, A.; Smith, L.; Firth, J.; Trott, M.; Mesas, A.E.; Jiménez-López, E.; Gutiérrez-Espinoza, H.; Tárraga-López, P.J.; Victoria-Montesinos, D. Global Proportion of Disordered Eating in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2023, 177, 363–372. [Google Scholar] [CrossRef]
- Sawyer, S.M.; Afifi, R.A.; Bearinger, L.H.; Blakemore, S.-J.; Dick, B.; Ezeh, A.C.; Patton, G.C. Adolescence: A Foundation for Future Health. Lancet 2012, 379, 1630–1640. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Larson, N.I.; Eisenberg, M.E.; Loth, K. Dieting and Disordered Eating Behaviors from Adolescence to Young Adulthood: Findings from a 10-Year Longitudinal Study. J. Am. Diet. Assoc. 2011, 111, 1004–1011. [Google Scholar] [CrossRef] [PubMed]
- Barakat, S.; McLean, S.A.; Bryant, E.; Le, A.; Marks, P.; Aouad, P.; Barakat, S.; Boakes, R.; Brennan, L.; Bryant, E.; et al. Risk Factors for Eating Disorders: Findings from a Rapid Review. J. Eat. Disord. 2023, 11, 8. [Google Scholar] [CrossRef] [PubMed]
- le Grange, D.; Lock, J.; Loeb, K.; Nicholls, D. Academy for Eating Disorders Position Paper: The Role of the Family in Eating Disorders. Int. J. Eat. Disord. 2010, 43, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Hampshire, C.; Mahoney, B.; Davis, S.K. Parenting Styles and Disordered Eating among Youths: A Rapid Scoping Review. Front. Psychol. 2022, 12, 802567. [Google Scholar] [CrossRef] [PubMed]
- Dahill, L.; Mitchison, D.; Morrison, N.M.V.; Touyz, S.; Bussey, K.; Trompeter, N.; Lonergan, A.; Hay, P. Prevalence of Parental Comments on Weight/Shape/Eating amongst Sons and Daughters in an Adolescent Sample. Nutrients 2021, 13, 158. [Google Scholar] [CrossRef] [PubMed]
- Dahill, L.M.; Morrison, N.M.V.; Mannan, H.; Mitchison, D.; Touyz, S.; Bussey, K.; Trompeter, N.; Hay, P. Exploring Associations between Positive and Negative Valanced Parental Comments about Adolescents’ Bodies and Eating and Eating Problems: A Community Study. J. Eat. Disord. 2022, 10, 43. [Google Scholar] [CrossRef]
- de Vázquez, C.D.L.; Santoncini, C.U. Parental Negative Weight/Shape Comments and Their Association with Disordered Eating Behaviors: A Systematic Review. Rev. Mex. Trastor. Aliment. 2019, 10, 134–147. [Google Scholar] [CrossRef]
- Abraczinskas, M.; Fisak, B.; Barnes, R.D. The Relation between Parental Influence, Body Image, and Eating Behaviors in a Nonclinical Female Sample. Body Image 2012, 9, 93–100. [Google Scholar] [CrossRef]
- Eisenberg, M.E.; Berge, J.M.; Fulkerson, J.A.; Neumark-Sztainer, D. Associations between Hurtful Weight-Related Comments by Family and Significant Other and the Development of Disordered Eating Behaviors in Young Adults. J. Behav. Med. 2012, 35, 500–508. [Google Scholar] [CrossRef]
- Martin, C.; Herrick, K.; Sarafrazi, N.; Ogden, C. Attempts to Lose Weight Among Adults in the United States, 2013–2016; National Center for Health Statistics: Hyattsville, MD, USA, 2018. [Google Scholar]
- Inchley, J.; Currie, D.; Young, T.; Weltgesundheitsorganisation; Regionalbüro für Europa. Growing up Unequal: Gender and Socioeconomic Differences in Young People’s Health and Well-Being; Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2013/2014 Survey; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-890-5136-1. [Google Scholar]
- Golden, N.H.; Schneider, M.; Wood, C. Preventing Obesity and Eating Disorders in Adolescents. Pediatrics 2016, 138, e20161649. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Guo, J.; Story, M.; Haines, J.; Eisenberg, M. Obesity, Disordered Eating, and Eating Disorders in a Longitudinal Study of Adolescents: How Do Dieters Fare 5 Years Later? J. Am. Diet. Assoc. 2006, 106, 559–568. [Google Scholar] [CrossRef]
- Berge, J.M.; MacLehose, R.; Loth, K.A.; Eisenberg, M.; Bucchianeri, M.M.; Neumark-Sztainer, D. Parent Conversations about Healthful Eating and Weight: Associations with Adolescent Disordered Eating Behaviors. JAMA Pediatr. 2013, 167, 746–753. [Google Scholar] [CrossRef]
- Loth, K.A.; Neumark-Sztainer, D.; Croll, J.K. Informing Family Approaches to Eating Disorder Prevention: Perspectives of Those Who Have Been There. Int. J. Eat. Disord. 2009, 42, 146–152. [Google Scholar] [CrossRef]
- Allen, K.L.; Gibson, L.Y.; McLean, N.J.; Davis, E.A.; Byrne, S.M. Maternal and Family Factors and Child Eating Pathology: Risk and Protective Relationships. J. Eat. Disord. 2014, 2, 11. [Google Scholar] [CrossRef]
- Bould, H.; Sovio, U.; Koupil, I.; Dalman, C.; Micali, N.; Lewis, G.; Magnusson, C. Do Eating Disorders in Parents Predict Eating Disorders in Children? Evidence from a Swedish Cohort. Acta Psychiatr. Scand. 2015, 132, 51–59. [Google Scholar] [CrossRef]
- Canals, J.; Sancho, C.; Arija, M.V. Influence of Parent’s Eating Attitudes on Eating Disorders in School Adolescents. Eur. Child Adolesc. Psychiatry 2009, 18, 353–359. [Google Scholar] [CrossRef]
- Micali, N.; De Stavola, B.; Ploubidis, G.B.; Simonoff, E.; Treasure, J. The Effects of Maternal Eating Disorders on Offspring Childhood and Early Adolescent Psychiatric Disorders. Int. J. Eat. Disord. 2014, 47, 385–393. [Google Scholar] [CrossRef]
- Westerberg, J.; Edlund, B.; Ghaderi, A. A 2-Year Longitudinal Study of Eating Attitudes, BMI, Perfectionism, Asceticism and Family Climate in Adolescent Girls and Their Parents. Eat. Weight Disord. 2008, 13, 64–72. [Google Scholar] [CrossRef]
- Ziobrowski, H.N.; Sonneville, K.R.; Eddy, K.T.; Crosby, R.D.; Micali, N.; Horton, N.J.; Field, A.E. Maternal Eating Disorders and Eating Disorder Treatment Among Girls in the Growing Up Today Study. J. Adolesc. Health 2019, 65, 469–475. [Google Scholar] [CrossRef]
- Chapman, L.; Cartwright-Hatton, S.; Thomson, A.; Lester, K.J. Parental Eating Disorders: A Systematic Review of Parenting Attitudes, Behaviours, and Parent-Child Interactions. Clin. Psychol. Rev. 2021, 88, 102031. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.S.N.; Chen, J.Y.; Ng, M.Y.C.; Yeung, M.H.Y.; Bedford, L.E.; Lam, C.L.K. How Does the Family Influence Adolescent Eating Habits in Terms of Knowledge, Attitudes and Practices? A Global Systematic Review of Qualitative Studies. Nutrients 2021, 13, 3717. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, R.; Chabrol, H. Parental Attitudes, Body Image Disturbance and Disordered Eating amongst Adolescents and Young Adults: A Review. Eur. Eat. Disord. Rev. 2009, 17, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Balantekin, K.N. The Influence of Parental Dieting Behavior on Child Dieting Behavior and Weight Status. Curr. Obes. Rep. 2019, 8, 137–144. [Google Scholar] [CrossRef]
- Dixon, R.; Adair, V.; O’Connor, S. Parental Influences on the Dieting Beliefs and Behaviors of Adolescent Females in New Zealand. J. Adolesc. Health 1996, 19, 303–307. [Google Scholar] [CrossRef]
- Coffman, D.L.; Balantekin, K.N.; Savage, J.S. Using Propensity Score Methods To Assess Causal Effects of Mothers’ Dieting Behavior on Daughters’ Early Dieting Behavior. Child Obes. 2016, 12, 334–340. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Duck, S.A.; Guarda, A.S.; Schreyer, C.C. Parental Dieting Impacts Inpatient Treatment Outcomes for Adolescents with Restrictive Eating Disorders. Eur. Eat. Disord. Rev. 2023, 31, 539–546. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Bauer, K.W.; Friend, S.; Hannan, P.J.; Story, M.; Berge, J.M. Family Weight Talk and Dieting: How Much Do They Matter for Body Dissatisfaction and Disordered Eating Behaviors in Adolescent Girls? J. Adolesc. Health 2010, 47, 270–276. [Google Scholar] [CrossRef]
- Keery, H.; Eisenberg, M.E.; Boutelle, K.; Neumark-Sztainer, D.; Story, M. Relationships between Maternal and Adolescent Weight-Related Behaviors and Concerns: The Role of Perception. J. Psychosom. Res. 2006, 61, 105–111. [Google Scholar] [CrossRef]
- Haynos, A.F.; Watts, A.W.; Loth, K.A.; Pearson, C.M.; Neumark-Stzainer, D. Factors Predicting an Escalation of Restrictive Eating During Adolescence. J. Adolesc. Health 2016, 59, 391–396. [Google Scholar] [CrossRef]
- García de Amusquibar, A.M.; De Simone, C.J. Some Features of Mothers of Patients with Eating Disorders. Eat. Weight Disord. 2003, 8, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Bilali, A.; Galanis, P.; Velonakis, E.; Katostaras, T. Factors Associated with Abnormal Eating Attitudes among Greek Adolescents. J. Nutr. Educ. Behav. 2010, 42, 292–298. [Google Scholar] [CrossRef]
- Dixon, R.S.; Gill, J.M.W.; Adair, V.A. Exploring Paternal Influences on the Dieting Behaviors of Adolescent Girls. Eat. Disord. 2003, 11, 39–50. [Google Scholar] [CrossRef]
- Keel, P.K.; Heatherton, T.F.; Harnden, J.L.; Hornig, C.D. Mothers, Fathers, and Daughters: Dieting and Disordered Eating. Eat. Disord. 1997, 5, 216–228. [Google Scholar] [CrossRef]
- Horesh, N.; Sommerfeld, E.; Wolf, M.; Zubery, E.; Zalsman, G. Father–Daughter Relationship and the Severity of Eating Disorders. Eur. Psychiatry 2015, 30, 114–120. [Google Scholar] [CrossRef] [PubMed]
- NHS UK. Advice for Parents—Eating Disorders. Available online: https://www.nhs.uk/mental-health/feelings-symptoms-behaviours/behaviours/eating-disorders/advice-for-parents/ (accessed on 2 July 2023).
- Boswell, R.G.; Lydecker, J.A. Double Trouble? Associations of Parental Substance Use and Eating Behaviors with Pediatric Disordered Eating. Addict. Behav. 2021, 123, 107089. [Google Scholar] [CrossRef] [PubMed]
- Castillo, M.D.G.; Pina, J.A.L.; Ortuño, A.I.T.; Durán, A.L.; Trives, J.J.R. Parental Eating Disorders Symptoms in Different Clinical Diagnoses. Psicothema 2018, 30, 382–387. [Google Scholar] [CrossRef]
- Linville, D.; Stice, E.; Gau, J.; O’Neil, M. Predictive Effects of Mother and Peer Influences on Increases in Adolescent Eating Disorder Risk Factors and Symptoms: A 3-Year Longitudinal Study. Int. J. Eat. Disord. 2011, 44, 745–751. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Recommendations. Eating Disorders: Recognition and Treatment. Available online: https://www.nice.org.uk/guidance/ng69/chapter/Recommendations#treating-anorexia-nervosa (accessed on 26 August 2023).
| Search String |
|---|
| (“eating disorders” OR “disordered eating” OR “anorexia” OR “bulimia” OR “binge eating”) AND (adolescents OR adolescent OR adolescence OR youth) AND (“parental dieting” OR “parental eating” OR “maternal dieting” OR “maternal eating” OR “paternal dieting” OR “paternal eating” OR “parental eating disorder” OR “parental disordered eating” OR “maternal eating disorder” OR “maternal disordered eating” OR “paternal eating disorder” OR “paternal disordered eating”) |
| Inclusion Criteria |
|---|
|
| Exclusion Criteria |
|
| Study | Country | Population | Study Design | Instruments | Main Findings |
|---|---|---|---|---|---|
| Bilali et al. (2010) [46] | Greece | 540 adolescent boys and girls | cross-sectional | ΕAΤ 26 questionnaire, question on existence of a family member on a diet | Adolescents who reported having a family member who was dieting were more likely to have DEBs than those who did not |
| Neumark-Sztainer et al. (2010) [42] | USA | 356 adolescent girls | cross-sectional | Project EAT questionnaire | Positive association of maternal dieting to unhealthy and extreme weight control behaviours by adolescents. No association of paternal dieting to adverse effects in adolescent dietary habits |
| Keery et al. (2006) [43] | USA | 810 adolescent boys and girls and their mothers | cross-sectional | Project EAT questionnaire | Significant associations between adolescents’ weight concerns and weight control behaviours and adolescents’ perception of maternal dieting. Not significant associations with maternal self-reported dieting |
| Garcia de Amusquibar et al. (2003) [45] | Argentina | 50 mothers of adolescent girls with ED and 30 control-group mothers | case-control | ΕAΤ 26 questionnaire | Mothers’ frequent dieting was a common characteristic in both groups. No significant differences between ED mothers and controls |
| Duck et al. (2023) [41] | USA | 45 adolescent boys and girls diagnosed with a restrictive ED admitted to an inpatient-partial hospitalisation program and their parents | prospective cohort | Questionnaire about parental eating and exercise behaviours answered by the parents. Data on adolescents were abstracted from the electronic medical record | Adolescents whose parents reported current dieting gained weight at a slower rate, compared to adolescents whose parents did not report current dieting |
| Haynos et al. (2016) [44] | USA | 243 adolescent boys and girls who were dieting | prospective cohort | Project EAT questionnaire (ΕAΤ ΙΙ) | Maternal dieting is a predictor for the development of disordered restrictive dieting in adolescents |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kontele, I.; Saripanagiotou, S.; Papadopoulou, A.M.; Zoumbaneas, E.; Vassilakou, T. Parental Dieting and Correlation with Disordered Eating Behaviours in Adolescents: A Narrative Review. Adolescents 2023, 3, 538-549. https://doi.org/10.3390/adolescents3030038
Kontele I, Saripanagiotou S, Papadopoulou AM, Zoumbaneas E, Vassilakou T. Parental Dieting and Correlation with Disordered Eating Behaviours in Adolescents: A Narrative Review. Adolescents. 2023; 3(3):538-549. https://doi.org/10.3390/adolescents3030038
Chicago/Turabian StyleKontele, Ioanna, Stella Saripanagiotou, Agni Maria Papadopoulou, Evangelos Zoumbaneas, and Tonia Vassilakou. 2023. "Parental Dieting and Correlation with Disordered Eating Behaviours in Adolescents: A Narrative Review" Adolescents 3, no. 3: 538-549. https://doi.org/10.3390/adolescents3030038
APA StyleKontele, I., Saripanagiotou, S., Papadopoulou, A. M., Zoumbaneas, E., & Vassilakou, T. (2023). Parental Dieting and Correlation with Disordered Eating Behaviours in Adolescents: A Narrative Review. Adolescents, 3(3), 538-549. https://doi.org/10.3390/adolescents3030038







