The Role of Social Capital, Sex Communication, and Sex Refusal Self-Efficacy in Sexual Risk Behaviors and HIV Testing among a Diverse Sample of Youth
Abstract
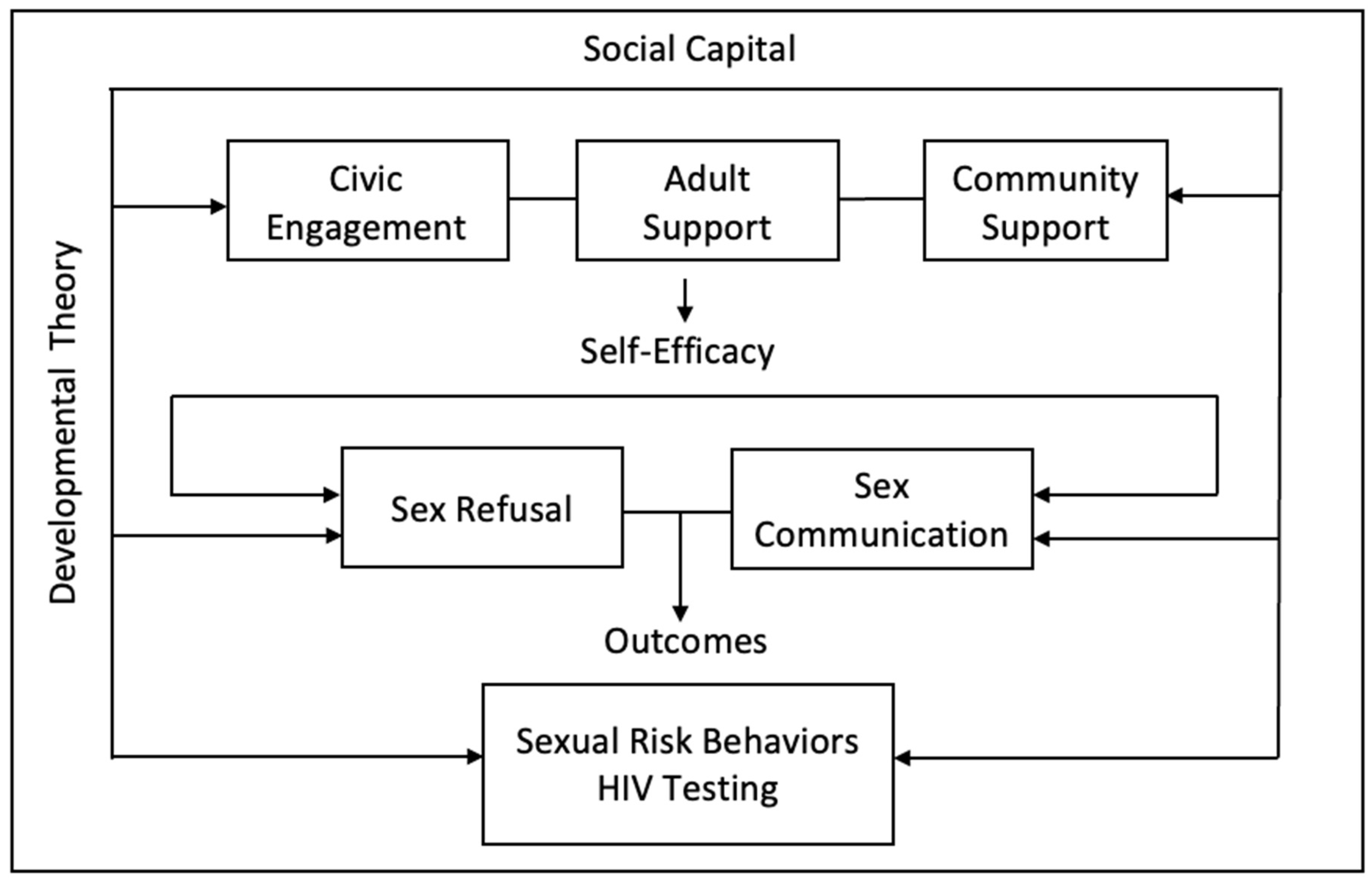
1. Introduction
2. Methods
2.1. Procedures
2.2. Measures
2.3. Analytic Approach
3. Results
3.1. Descriptive Findings
3.2. Measurement Model
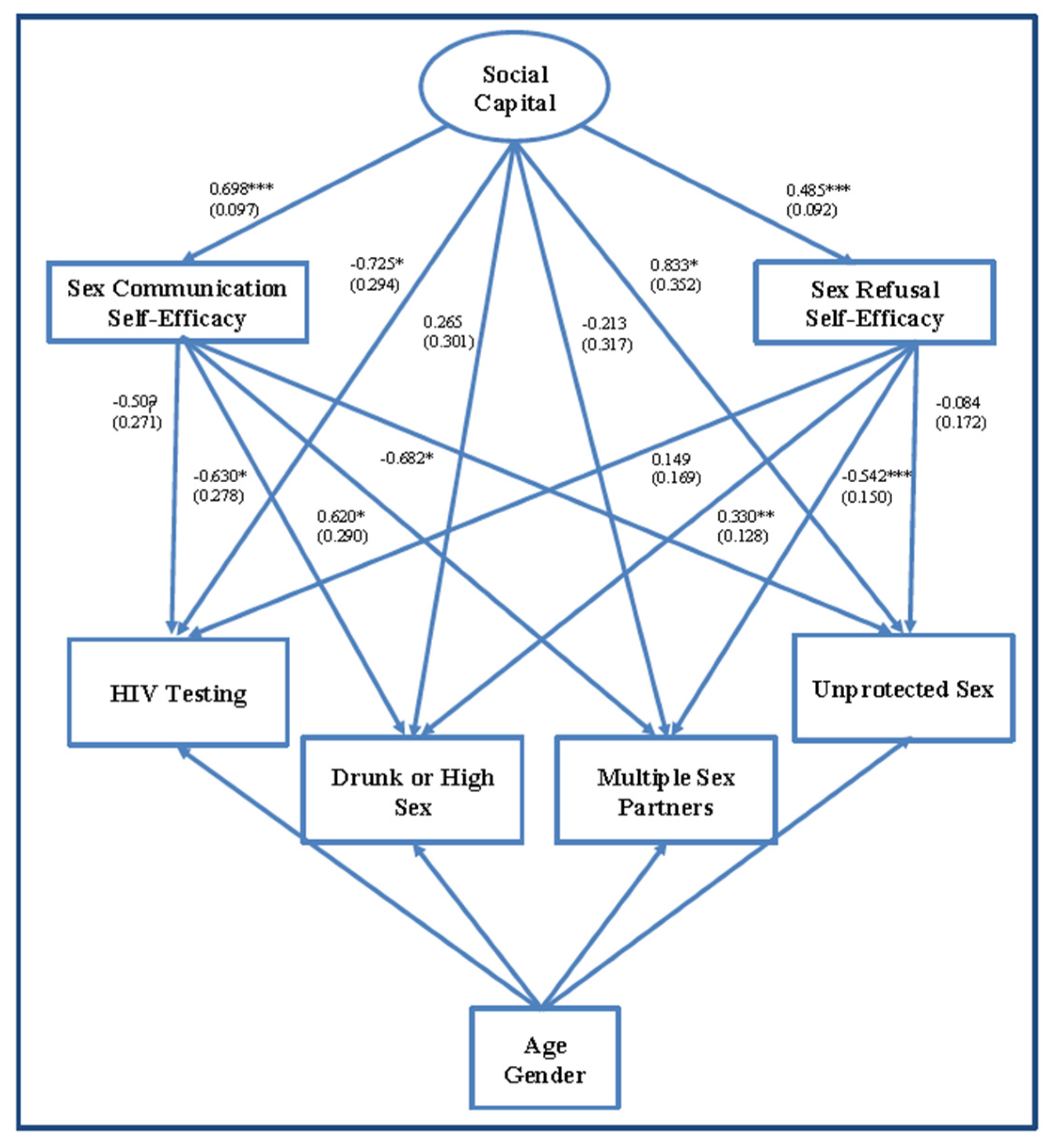
3.3. Structural Equation Modelling
4. Discussion
4.1. Related Work
4.2. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention (CDC). Adolescents and Young Adults. Available online: https://www.cdc.gov/std/life-stages-populations/adolescents-youngadults.htm (accessed on 17 February 2021).
- Centers for Disease Control and Prevention (CDC). HIV and Youth. Available online: https://www.cdc.gov/hiv/group/age/youth/index.html (accessed on 25 February 2021).
- Centers for Disease Control and Prevention (CDC). 1991–2019 High School Youth Risk Behavior Survey Data. Available online: http://nccd.cdc.gov/youthonline/ (accessed on 25 February 2021).
- Cordova, D.; Huang, S.; Lally, M.; Estrada, Y.; Prado, G. Do Parent-Adolescent Discrepancies in Family Functioning Increase the Risk of Hispanic Adolescent HIV Risk Behaviors? Fam. Process 2014, 53, 348–363. [Google Scholar] [CrossRef] [PubMed]
- Farrelly, C.; Cordova, D.; Huang, S.; Estrada, Y.; Prado, G. The Role of Acculturation and Family Functioning in Predicting HIV Risk Behaviors among Hispanic Delinquent Youth. J. Immigr. Minor. Health 2013, 15, 476–483. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Frieden, T.R.; Harold Jaffe, D.W.; Rasmussen, S.A.; Leahy, M.A.; Martinroe, J.C.; Spriggs, S.R.; Doan, Q.M.; King Terraye, M.; Starr, P.H.; Roper, W.L.; et al. Sexually Transmitted Disease Treatment Guidelines. Morbidity and Mortality Weekly Report (MMWR) Recommendations and Reports; Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention (CDC), U.S. Department of Health and Human Services: Atlanta, GA, USA, 2015; Volume 64. [CrossRef]
- United States Preventive Services Task Force. Human Immunodeficiency Virus (HIV) Infection: Screening. Available online: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/human-immunodeficiency-virus-hiv-infection-screening (accessed on 25 February 2021).
- Centers for Disease Control and Prevention. HIV Information and Youth. Available online: https://www.cdc.gov/healthyyouth/youth_hiv/hiv-information-and-youth.htm (accessed on 17 February 2021).
- Centers for Disease Control and Prevention. HIV Testing. Available online: https://www.cdc.gov/hiv/testing/index.html (accessed on 17 February 2021).
- Centers for Disease Control and Prevention. Estimated HIV Incidence and Prevalence in the United States, 2014–2018. Available online: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-25-1.pdf (accessed on 17 February 2021).
- United States Agency International Development (USAID). Social Capital Interventions for HIV: Rigorous Evidence, Usable Results; United States Agency for International Development (USAID): Washington, DC, USA, 2013.
- Kritsotakis, G.; Gamarnikow, E. What Is Social Capital and How Does It Relate to Health? Int. J. Nurs. Stud. 2004, 41, 43–50. [Google Scholar] [CrossRef]
- Putnam, R.D.; Leonardi, R.; Nanetti, R. Making Democracy Work: Civic Traditions in Modern Italy; Princeton University Press: Princeton, NJ, USA, 1993. [Google Scholar]
- Smylie, L.; Medaglia, S.; Maticka-Tyndale, E. The Effect of Social Capital and Socio-Demographics on Adolescent Risk and Sexual Health Behaviours. Can. J. Hum. Sex. 2006, 15, 95. [Google Scholar]
- Vyncke, V.; Hardyns, W.; Peersman, W.; Pauwels, L.; Groenewegen, P.; Willems, S. How Equal Is the Relationship between Individual Social Capital and Psychological Distress? A Gendered Analysis Using Cross-Sectional Data from Ghent (Belgium). BMC Public Health 2014, 14, 960. [Google Scholar] [CrossRef]
- Kawachi, I.; Berkman, L. Social Cohesion, Social Capital and Health. In Social Epidemiology; Oxford University Press: Oxford, UK, 2000; pp. 174–190. [Google Scholar] [CrossRef]
- Murayama, H.; Fujiwara, Y.; Kawachi, I. Social Capital and Health: A Review of Prospective Multilevel Studies. J. Epidemiol. 2012, 22, 179–187. [Google Scholar] [CrossRef]
- Malcolm, S.; Huang, S.; Cordova, D.; Freitas, D.; Arzon, M.; Jimenez, G.L.; Pantin, H.; Prado, G. Predicting Condom Use Attitudes, Norms, and Control Beliefs in Hispanic Problem Behavior Youth: The Effects of Family Functioning and Parent-Adolescent Communication About Sex on Condom Use. Health Educ. Behav. 2013, 40, 384–391. [Google Scholar] [CrossRef]
- McPherson, K.E.; Kerr, S.; McGee, E.; Morgan, A.; Cheater, F.M.; McLean, J.; Egan, J. The Association between Social Capital and Mental Health and Behavioural Problems in Children and Adolescents: An Integrative Systematic Review. BMC Psychol. 2014, 2, 7. [Google Scholar] [CrossRef]
- Oman, R.F.; Vesely, S.K.; Aspy, C.B. Youth Assets and Sexual Risk Behavior: The Importance of Assets for Youth Residing in One-Parent Households. Perspect. Sex. Reprod. Health 2005, 37, 25–31. [Google Scholar] [CrossRef]
- Voisin, D.R.; Hotton, A.; Tan, K.; Diclemente, R. A Longitudinal Examination of Risk and Protective Factors Associated with Drug Use and Unsafe Sex among Young African American Females. Child. Youth Serv. Rev. 2013, 35, 1440–1446. [Google Scholar] [CrossRef]
- Odimegwu, C.; De Wet, N.; Somefun, O.D. Perceptions of Social Capital and Sexual Behaviour among Youth in South Africa. J. Child Adolesc. Ment. Health 2017, 29, 205–217. [Google Scholar] [CrossRef] [PubMed]
- Banstola, R.S.; Ogino, T.; Inoue, S. Self-Esteem, Perceived Social Support, Social Capital, and Risk-Behavior among Urban High School Adolescents in Nepal. SSM-Popul. Health 2020, 11, 100570. [Google Scholar] [CrossRef]
- Jennings, J.M.; Hensel, D.J.; Tanner, A.E.; Reilly, M.L.; Ellen, J.M. Are Social Organizational Factors Independently Associated with a Current Bacterial Sexually Transmitted Infection among Urban Adolescents and Young Adults? Soc. Sci. Med. 2014, 118, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Mendez Rojas, B.; Beogo, I.; Owili, P.O.; Adesanya, O.; Chen, C.-Y. Community Social Capital on the Timing of Sexual Debut and Teen Birth in Nicaragua: A Multilevel Approach. BMC Public Health 2016, 16, 991. [Google Scholar] [CrossRef] [PubMed]
- Villalonga-Olives, E.; Kawachi, I. The Dark Side of Social Capital: A Systematic Review of the Negative Health Effects of Social Capital. Soc. Sci. Med. 2017, 194, 105–127. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.K.J.; O’Hara, C.A.; Koh, W.L.; Le, D.; Tan, A.; Tyler, A.; Tan, C.; Kwok, C.; Banerjee, S.; Wong, M.L. Social Capital and Chemsex Initiation in Young Gay, Bisexual, and Other Men Who Have Sex with Men: The Pink Carpet Y Cohort Study. Subst. Abuse Treat. Prev. Policy 2021, 16, 18. [Google Scholar] [CrossRef]
- Coleman-Minahan, K.; Gutierrez, Y.; Bull, S. Adult and Community Influence on Sexual Experience Among First-, Second-, and Third-Generation Immigrant Youth. Youth Soc. 2018, 52, 1377–1394. [Google Scholar] [CrossRef]
- Coleman-Minahan, K.; Chavez, M.; Bull, S. Immigrant Generation and Sexual Initiation Among a Diverse Racial/Ethnic Group of Urban Youth. J. Immigr. Minor. Health 2017, 19, 1412–1419. [Google Scholar] [CrossRef]
- Glassman, J.R.; Franks, H.M.; Baumler, E.R.; Coyle, K.K. Mediation Analysis of an Adolescent HIV/STI/Pregnancy Prevention Intervention. Sex Educ. 2014, 14, 497–509. [Google Scholar] [CrossRef]
- Bandura, A. Much Ado over a Faulty Conception of Perceived Self-Efficacy Grounded in Faulty Experimentation. J. Soc. Clin. Psychol. 2007, 26, 641–658. [Google Scholar] [CrossRef]
- Jiménez García, M.I. Comunicación sexual en adolescentes y su implicación en la consistencia del uso del condón. Enseñanza Investig. Psicol. 2010, 15, 107–129. [Google Scholar]
- Yuan, R.; Ngai, S.S. Agentic Personality as Mediator of Social Capital on Developmental Outcomes in the Transition to Adulthood: Evidence from Shanghai, China. J. Adolesc. 2016, 46, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.A.; Rimal, R. The Impact of Social Capital on HIV-Related Actions as Mediated by Personal and Proxy Efficacies in Namibia. AIDS Behav. 2009, 13, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Swendeman, D.; Basu, I.; Das, S.; Jana, S.; Rotheram-Borus, M.J. Empowering Sex Workers in India to Reduce Vulnerability to HIV and Sexually Transmitted Diseases. Soc. Sci. Med. 2009, 69, 1157–1166. [Google Scholar] [CrossRef] [PubMed]
- Córdova, D.; Coleman-Minahan, K.; Bull, S.; Borrayo, E.A. Development of the Brief Social Capital for Youth Sexual and Reproductive Health Scale: Exploratory and Confirmatory Factor Analysis. Youth Soc. 2017, 51, 570–587. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Fit Indices in Covariance Structure Modeling: Sensitivity to Underparameterized Model Misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus: Statistical Analysis with Latent Variables: User’s Guide; Muthen & Muthen: Los Angeles, CA, USA, 2012. [Google Scholar]
- Jorgensen-Wells, M.A.; James, S.L. Social Capital and Age at Sexual Debut: Race Differences in South Africa. Soc. Sci. 2020, 9, 197. [Google Scholar] [CrossRef]
- Pronyk, P.M.; Harpham, T.; Busza, J.; Phetla, G.; Morison, L.A.; Hargreaves, J.R.; Kim, J.C.; Watts, C.H.; Porter, J.D. Can Social Capital Be Intentionally Generated? A Randomized Trial from Rural South Africa. Soc. Sci. Med. 2008, 67, 1559–1570. [Google Scholar] [CrossRef]
- Ramírez-Ortiz, D.; Sheehan, D.M.; Moore, M.P.; Ibañez, G.E.; Ibrahimou, B.; De La Rosa, M.; Cano, M.Á. HIV Testing Among Latino Emerging Adults: Examining Associations with Familism Support, Nativity, and Gender. J. Immigr. Minor. Health 2020, 22, 1039–1048. [Google Scholar] [CrossRef]
- Richmond, T.K.; Subramanian, S.V. School Level Contextual Factors Are Associated with the Weight Status of Adolescent Males and Females. Obesity 2008, 16, 1324–1330. [Google Scholar] [CrossRef] [PubMed]
- Vargas Valle, E.D.; Martínez Canizales, G.; Potter, J.E. Religión e Iniciación Sexual Premarital En México. Rev. Latinoam. Población 2010, 4, 7–30. [Google Scholar] [CrossRef]
- Novak, D.; Kawachi, I. Influence of Different Domains of Social Capital on Psychological Distress among Croatian High School Students. Int. J. Ment. Health Syst. 2015, 9, 18. [Google Scholar] [CrossRef] [PubMed]
- Boone-Heinonen, J.; Gordon-Larsen, P. Obesogenic Environments in Youth: Concepts and Methods from a Longitudinal National Sample. Am. J. Prev. Med. 2012, 42, e37–e46. [Google Scholar] [CrossRef] [PubMed]
- Edi Putra, I.G.; Januraga, P.P. Social Capital and HIV Testing Uptake among Indirect Female Sex Workers in Bali, Indonesia. Trop. Med. Infect. Dis. 2020, 5, 73. [Google Scholar] [CrossRef] [PubMed]
- Valente, P.K.; Mimiaga, M.J.; Mayer, K.H.; Safren, S.A.; Biello, K.B. Social Capital Moderates the Relationship Between Stigma and Sexual Risk Among Male Sex Workers in the US Northeast. AIDS Behav. 2020, 24, 29–38. [Google Scholar] [CrossRef]
- Ransome, Y.; Cunningham, K.; Paredes, M.; Mena, L.; Sutten-Coats, C.; Chan, P.; Simmons, D.; Willie, T.C.; Nunn, A. Social Capital and Risk of Concurrent Sexual Partners Among African Americans in Jackson, Mississippi. AIDS Behav. 2020, 24, 2062–2072. [Google Scholar] [CrossRef]
- García Mazorra, M.; Fung Pérez, M.; Leon Pino, H.; Sanchez Ima, M. Comportamiento sexual de las adolescentes que acuden al aborto voluntario. MediSur 2011, 9, 38–41. [Google Scholar]
- Hill, A.O.; Bavinton, B.R.; Kaneko, N.; Lafferty, L.; Lyons, A.; Gilmour, S.; Armstrong, G. Associations Between Social Capital and HIV Risk-Taking Behaviors Among Men Who Have Sex with Men in Japan. Arch. Sex. Behav. 2021, 50, 3103–3113. [Google Scholar] [CrossRef]
- Boone, M.R.; Cherenack, E.M.; Wilson, P.A. Self-Efficacy for Sexual Risk Reduction and Partner HIV Status as Correlates of Sexual Risk Behavior Among HIV-Positive Adolescent Girls and Women. AIDS Patient Care STDS 2015, 29, 346–353. [Google Scholar] [CrossRef]
- Romero, L.M.; Galbraith, J.S.; Wilson-Williams, L.; Gloppen, K.M. HIV Prevention among African American Youth: How Well Have Evidence-Based Interventions Addressed Key Theoretical Constructs? AIDS Behav. 2011, 15, 976–991. [Google Scholar] [CrossRef] [PubMed]
- Stanton, B.; Wang, B.; Deveaux, L.; Lunn, S.; Rolle, G.; Li, X.; Braithwaite, N.; Dinaj-Koci, V.; Marshall, S.; Gomez, P. Assessing the Effects of a Complementary Parent Intervention and Prior Exposure to a Preadolescent Program of HIV Risk Reduction for Mid-Adolescents. Am. J. Public Health 2015, 105, 575–583. [Google Scholar] [CrossRef] [PubMed]
- DE JESÚS-REYES, D.; MENKES-BANCET, C. Prácticas y significados del uso del condón en varones adolescentes de dos contextos de México. Pap. Población 2014, 20, 73–97. [Google Scholar]
- Kim, H.H.-S. School Context, Friendship Ties and Adolescent Mental Health: A Multilevel Analysis of the Korean Youth Panel Survey (KYPS). Soc. Sci. Med. 2015, 145, 209–216. [Google Scholar] [CrossRef] [PubMed]
| Scale | N (%) | Scale Range | Mean | SD | Min. | Max. | Alpha |
|---|---|---|---|---|---|---|---|
| Predictors | |||||||
| Civic Engagement | - | 0–4 | 1.65 | 1.37 | 0 | 4 | 0.56 |
| Community Support | - | 0–4 | 2.29 | 1.08 | 0 | 4 | - |
| Adult Support | - | 0–4 | 3.34 | 0.74 | 0 | 4 | 0.91 |
| Sex Communication Self-Efficacy | - | 0–3 | 2.55 | 0.75 | 0 | 3 | 0.66 |
| Sex Refusal Self-Efficacy | - | 0–3 | 2.68 | 0.67 | 0 | 3 | 0.55 |
| Outcomes | |||||||
| Unprotected Sex | 46 (23) | - | - | - | - | - | - |
| Multiple Sex Partners | 10 (5) | - | - | - | - | - | - |
| Being High/Drunk Prior To Sex | 25 (12.5) | - | - | - | - | - | - |
| HIV Test | 31 (15.5) | - | - | - | - | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cordova, D.; Coleman-Minahan, K.; Romo, T.; Borrayo, E.A.; Bull, S. The Role of Social Capital, Sex Communication, and Sex Refusal Self-Efficacy in Sexual Risk Behaviors and HIV Testing among a Diverse Sample of Youth. Adolescents 2022, 2, 30-42. https://doi.org/10.3390/adolescents2010004
Cordova D, Coleman-Minahan K, Romo T, Borrayo EA, Bull S. The Role of Social Capital, Sex Communication, and Sex Refusal Self-Efficacy in Sexual Risk Behaviors and HIV Testing among a Diverse Sample of Youth. Adolescents. 2022; 2(1):30-42. https://doi.org/10.3390/adolescents2010004
Chicago/Turabian StyleCordova, David, Kate Coleman-Minahan, Tattiana Romo, Evelinn A. Borrayo, and Sheana Bull. 2022. "The Role of Social Capital, Sex Communication, and Sex Refusal Self-Efficacy in Sexual Risk Behaviors and HIV Testing among a Diverse Sample of Youth" Adolescents 2, no. 1: 30-42. https://doi.org/10.3390/adolescents2010004
APA StyleCordova, D., Coleman-Minahan, K., Romo, T., Borrayo, E. A., & Bull, S. (2022). The Role of Social Capital, Sex Communication, and Sex Refusal Self-Efficacy in Sexual Risk Behaviors and HIV Testing among a Diverse Sample of Youth. Adolescents, 2(1), 30-42. https://doi.org/10.3390/adolescents2010004






