Transform Suffering by Cultivating Resilience: Embedding SDGs into Intergenerational Digital Health Platform for Navigating the Post-Pandemic Landscape †
Abstract
:1. Introduction
1.1. Global Challenges, Trends, and Awareness after the Outbreak
1.2. Population Aging in China and Response to Elderly Primary Care Amid COVID-19
1.3. Changes for Preventing the Detrimental Effect of Loneliness and Social Isolation under COVID-19
2. Methods
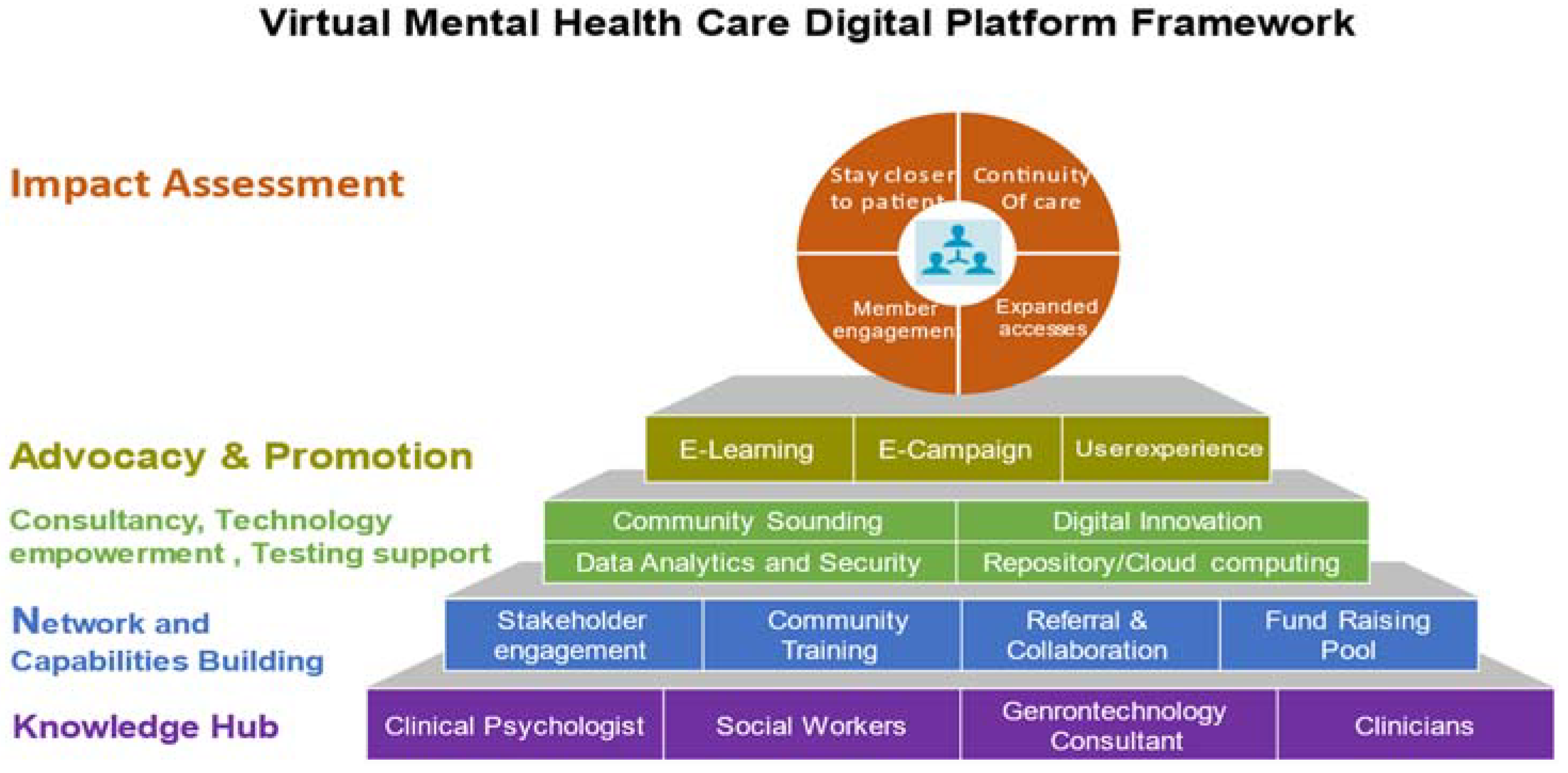
2.1. Elderly Mental Health Digital Platform Framework Design Embedding the SDG3 Goals
2.2. Study Design
- Health (accessible and affordable healthcare services and opportunities without the constraint of time, place, and resources to stay active);
- Participation (accessible digital tools, information services, social connections, volunteer help, and the need to be valued and respected);
- Utilization of information technology (recent and ongoing innovations in digital health technologies are achieving great potential and gaining a user base to bring about a transformative impact on mental health diagnosis, preventing, monitoring, and invention).
3. Results
- Overcoming barriers of elderly people’s equal right to health: a basket of indicators should be considered holistically before jumping to policy implementation, since the elderly population is subjected to numerous physical, psychosocial, and environmental concerns with their mental health situation.
- Maintaining social connections with the use of technology-based platform: many of the elderly are neither familiar nor receptive toward new technologies, and the modern style of mobile interaction may not effectively serve their emotional needs without coaching and advocating. The platform developed embedding SDG3 concepts should help older family members and their caregivers with the needed information literacy to overcome such technology barriers.
- Managing emotions and psychiatric symptoms with minimum stigma: loneliness is often associated with negative cognitions, especially under the pandemic and without deployment of sufficient resources to primary care. In addition, anxiety and depression brought by the social distancing policies during the pandemic may have aggravated social withdrawal issues and exacerbated the feeling of loneliness and isolation.
- Special care should be taken for elderly people with mental health issues and their family caregivers: In response to the COVID-19 pandemic, the world and the way in which people think and live have changed significantly. In addition to the elderly, caregivers within the family might also be facing high levels of stress and experiencing the feeling of isolation and loneliness. More detailed information on the unique aspects of the effects of the pandemic on elderly mental health should also be considered and highlighted by government agencies, social service organizations, and healthcare providers.
4. Discussion and Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alzheimer’s Disease International. ADI Offers Advice and Support during COVID-19. 2020. Available online: https://www.alz.co.uk/news/adi-offers-advice-and-support-during-covid-19 (accessed on 15 May 2020).
- Hu, B.; Ma, S. Receipt of informal care in the Chinese older population. Ageing Soc. 2018, 38, 766–793. [Google Scholar] [CrossRef] [Green Version]
- Hu, B. Projecting future demand for informal care among older people in China: The road towards a sustainable long-term care system. Health Econ. Policy Law 2019, 14, 61–81. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xu, L.; Chi, I. Perceived Need for Home- and Community-Based Services: Experiences of Urban Chinese Older Adults With Functional Impairments. J. Aging Soc. Policy 2017, 29, 182–196. [Google Scholar] [CrossRef] [PubMed]
- Hwang, T.J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Chen, L. Deciding to Institutionalize: Caregiving Crisis, Intergenerational Communication, and Uncertainty Management for Elders and Their Children in Shanghai. J. Gerontol. Soc. Work 2015, 58, 128–148. [Google Scholar] [CrossRef] [PubMed]
- Lum, T. Long-term Care in Asia. J. Gerontol. Soc. Work 2012, 55, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Ma, G.; Cai, S. Disparities in the provision of aging-friendly communities in old and new urban neighborhoods in China. Eng. Constr. Archit. Manag. 2019, 26, 1277–1293. [Google Scholar] [CrossRef]
- Zhang, F.; Li, D.; Ahrentzen, S.; Zhang, J. Assessing spatial disparities of accessibility to community-based service resources for Chinese older adults based on travel behavior: A city-wide study of Nanjing, China. Habitat Int. 2019, 88, 101984. [Google Scholar] [CrossRef]
- Fu, L.; Sun, Z.; He, L.; Liu, F.; Jing, X. Global long-term care research: A scientometric review. Int. J. Environ. Res. Public Health 2019, 16, 2077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, E.E.; Depp, C.; Palmer, B.W.; Glorioso, D.; Daly, R.; Liu, J.; Tu, X.M.; Kim, H.-C.; Tarr, P.; Yamada, Y.; et al. High prevalence and adverse health effects of loneliness in community-dwelling adults across the lifespan: Role of wisdom as a protective factor. Int. Psychogeriatr. 2019, 31, 1447–1462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talaie, T. Asian Care Certificate (ACC): A care quality assurance framework. Int. J. Health Care Qual. Assur. 2018, 31, 260–264. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Marier, P. Awaiting Long-Term Care Services in a Rapidly Changing Environment: Voices from Older Chinese Adults. J. Popul. Ageing 2017, 10, 385–401. [Google Scholar] [CrossRef]
- Yu, J.; Ma, G.; Jiang, X. Impact of the built environment and care services within rural nursing homes in China on quality of life for elderly residents. Eng. Constr. Archit. Manag. 2017, 24, 1170–1183. [Google Scholar] [CrossRef]
- Zhong, X.B.; Lou, V.W.Q. Person-centered care in Chinese residential care facilities: A preliminary measure. Aging Ment. Health 2013, 17, 952–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, W. The development of community-based service for older people in urban China: A case study in Guangzhou city. Int. Soc. Work 2017, 60, 1606–1618. [Google Scholar] [CrossRef]
- Song, Y.; Sörensen, S.; Yan, E.C.W. Family support and preparation for future care needs among urban Chinese baby boomers. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2018, 73, 1066–1076. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y. Characterising Long Term Care Needs among Chinese Older Adults with Cognitive Impairment or ADL Limitations. J. Cross. Cult. Gerontol. 2020, 35, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Scales, K.; Anderson, R.A.; Wu, B.; Corazzini, K.N. Resident challenges with daily life in Chinese long-term care facilities: A qualitative pilot study. Geriatr. Nurs. 2018, 39, 18–23. [Google Scholar] [CrossRef] [PubMed]
- WHO. Checklist of Essential Features of Age-Friendly Cities. 2007. Available online: http://www.who.int/ageing/publications/Age_friendly_cities_checklist.pdf?ua=1 (accessed on 1 April 2020).
- WHO. Global Age-Friendly Cities: A Guide. 2007. Available online: www.who.int/ageing/en (accessed on 1 April 2020).
- WHO. WHO Age-Friendly Cities Project Methodology Vancouver Protocol. 2007. Available online: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/07/AFC_Vancouver-protocol.pdf (accessed on 1 April 2020).
- World Health Organization. 8 Things to Know about a Pandemic. 2019. Available online: https://www.who.int/news-room/feature-stories/detail/8-things-to-know-about-pandemic-influenza (accessed on 1 April 2020).
- World Federation of Public Health Associations. A Global Charter for the Public’s Health. 2016. Available online: https://www.wfpha.org/wfpha-projects/14-projects/171-a-global-charter-for-the-public-s-health-3 (accessed on 1 April 2020).
- Feng, Z.; Falkingham, J.; Liu, X.; Vlachantoni, A. Changes in living arrangements and mortality among older people in China. SSM-Popul. Health 2017, 3, 9–19. [Google Scholar] [CrossRef] [PubMed]

| Group | Age | Socio-Economic Status |
|---|---|---|
| 1 | 60-69 | Low |
| 2 | 60-69 | Middle |
| 3 | 60-69 | High |
| 4 | 70 and over | Low |
| 5 | 70 and over | Middle |
| 6 | 70 and over | High |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, L. Transform Suffering by Cultivating Resilience: Embedding SDGs into Intergenerational Digital Health Platform for Navigating the Post-Pandemic Landscape. Environ. Sci. Proc. 2022, 15, 12. https://doi.org/10.3390/environsciproc2022015012
Cheng L. Transform Suffering by Cultivating Resilience: Embedding SDGs into Intergenerational Digital Health Platform for Navigating the Post-Pandemic Landscape. Environmental Sciences Proceedings. 2022; 15(1):12. https://doi.org/10.3390/environsciproc2022015012
Chicago/Turabian StyleCheng, Lan. 2022. "Transform Suffering by Cultivating Resilience: Embedding SDGs into Intergenerational Digital Health Platform for Navigating the Post-Pandemic Landscape" Environmental Sciences Proceedings 15, no. 1: 12. https://doi.org/10.3390/environsciproc2022015012
APA StyleCheng, L. (2022). Transform Suffering by Cultivating Resilience: Embedding SDGs into Intergenerational Digital Health Platform for Navigating the Post-Pandemic Landscape. Environmental Sciences Proceedings, 15(1), 12. https://doi.org/10.3390/environsciproc2022015012





