Transforming COVID-19 Research Priorities for Sustainable Development in Africa
Abstract
1. Introduction
1.1. Historical Review
1.2. Epidemiology of COVID-19
1.3. The Clinical Classification of COVID-19
1.4. COVID-19 Structure and Proteins
1.5. The Effectiveness of COVID-19 Vaccines
1.6. Potential Therapeutic Targets and Treatments
| Drug | Target | Reference |
|---|---|---|
| Antiviral drugs | ||
| Remdisivir | Inhibits RNA-dependent RNA polymerase. | [30] |
| Ribavirin | Inhibits the metabolism of RNA, which is essential for the proliferation and replication of the virus. | [31] |
| Novaferon | Inhibits the spread of COVID-19 in healthy cells by limiting viral replication in contaminated cells. | [30] |
| Lopinavir | Inhibits chymotrypsin-like protease enzyme (3CLpro), which is responsible for viral transcription and replication. | [32] |
| Nirmatrelvir-ritonavir | Inhibits chymotrypsin-like protease enzyme (3CLpro). | [33] |
| Molnupiravir | Inhibits RNA-dependent RNA polymerase. | [34] |
| Plant-derived compounds | ||
| Quercetin | Inhibits 3CLpro, S-protein, PLpro, ACE2 and RdRp. | [35,36,37] |
| Artemisinin | Inhibits 3CLpro. | [38] |
| Kaempferol | Inhibits chymotrypsin-like protease enzyme (3CLpro), which is responsible for viral transcription and replication. | [39] |
| 2,4-dihydroxycinnamic acid | Inhibits angiotensin-converting enzyme 2, a key component of the renin–angiotensin system, orchestrating fluid balance and blood pressure regulation. | [40] |
| Apigenin | Inhibits RNA-dependent RNA polymerase and 3CLpro. | [40] |
| Anacardic acid and Ginkgolic acid | Inhibits papain-like protease (PLpro) and 3CLpro. | [41] |
2. Materials and Methods
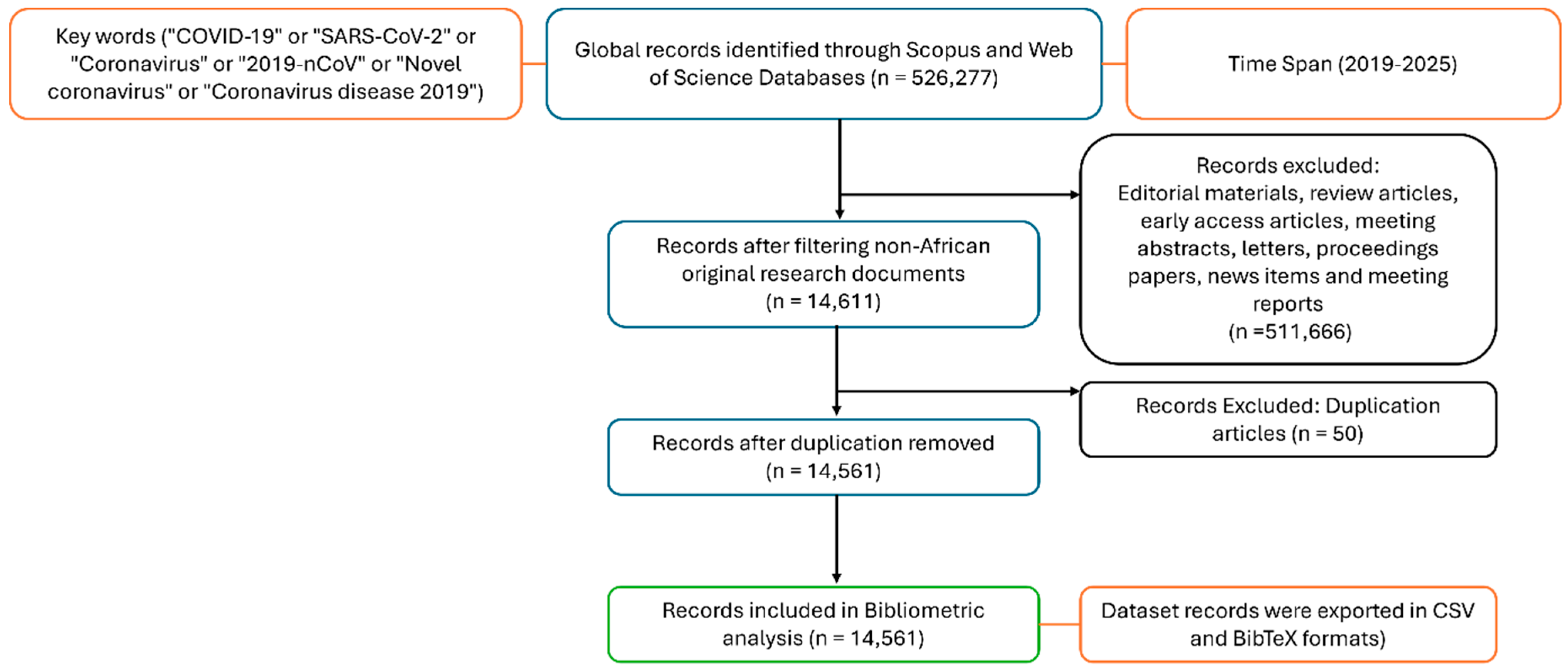
2.1. Data Extraction
2.2. Data Analysis and Visualizations
3. Results
3.1. Publication Trends and Citation Performance
3.2. African Countries’ Research on COVID-19
3.3. Subject Research Areas Related to Sustainable Development Goals
3.4. Financial Support for Original Research Publication
3.5. Intra-African Collaboration
4. Discussion
- Requirements for Cross-SDG Funding
- Prioritization of Grant Calls for Underrepresented SDGs
- Monitoring and Reporting
5. Conclusions
Study Limitation
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard; WHO: Geneva, Switzerland, 2023; Available online: https://data.who.int/dashboards/covid19/more-resources (accessed on 15 May 2025).
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554776/ (accessed on 10 August 2025). [PubMed]
- Ullrich, S.; Nitsche, C. The SARS-CoV-2 main protease as a drug target. Bioorg. Med. Chem. Lett. 2020, 30, 127377. [Google Scholar] [CrossRef]
- World Health Organization. Tracking SARS-CoV-2 Variants; WHO: Geneva, Switzerland, 2022; Available online: https://www.who.int/en/activities/tracking-sars-cov-2-variants (accessed on 13 June 2025).
- Sawicki, A.J.; Żemojtel-Piotrowska, M.; Balcerowska, J.M.; Sawicka, M.J.; Piotrowski, J.; Sedikides, C.; Jonason, P.K.; Maltby, J.; Adamovic, M.; Agada, A.M.D.; et al. The fear of COVID-19 scale: Its structure and measurement invariance across 48 countries. Psychol. Assess. 2022, 34, 294–310. [Google Scholar] [CrossRef]
- Kaftan, V.; Kandalov, W.; Molodtsov, I.; Sherstobitova, A.; Strielkowski, W. Socio-economic stability and sustainable development in the post-COVID era: Lessons for the business and economic leaders. Sustainability 2023, 15, 2876. [Google Scholar] [CrossRef]
- Assefa, Y.; Gilks, C.F.; Reid, S.; van de Pas, R.; Gete, D.G.; Van Damme, W. Analysis of the COVID-19 pandemic: Lessons towards a more effective response to public health emergencies. Glob. Health 2022, 18, 10. [Google Scholar] [CrossRef] [PubMed]
- Hamre, D.; Procknow, J.J. A new virus isolated from the human respiratory tract. Proc. Soc. Exp. Biol. Med. 1966, 121, 190–193. [Google Scholar] [CrossRef]
- Liu, D.X.; Liang, J.Q.; Fung, T.S. Human coronavirus-229E, -OC43, -NL63, and -HKU1 (Coronaviridae). In Encyclopedia of Virology, 4th ed.; Bamford, D.H., Zuckerman, M., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 428–440. [Google Scholar]
- Zhou, P.; Yang, X.-L.; Wang, X.-G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef]
- World Health Organization. Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 17 March 2024).
- Liu, P.; Jiang, J.-Z.; Wan, X.-F.; Hua, Y.; Li, L.; Zhou, J.; Wang, X.; Hou, F.; Chen, J.; Zou, J.; et al. Are pangolins the intermediate host of the 2019 novel coronavirus (SARS-CoV-2)? PLoS Pathog. 2020, 16, e1008421. [Google Scholar] [CrossRef]
- Chakraborty, C.; Sharma, A.R.; Sharma, G.; Bhattacharya, M.; Lee, S.S. SARS-CoV-2 Causing Pneumonia-Associated Respiratory Disorder (COVID-19): Diagnostic and Proposed Therapeutic Options. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 4016–4026. [Google Scholar] [CrossRef]
- Krishnamoorthy, Y.; Nagarajan, R.; Saya, G.K.; Menon, V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 293, 113382. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.K.; Tripathi, T. One-year update on the COVID-19 pandemic: Where are we now? Acta Trop. 2021, 214, 105778. [Google Scholar] [CrossRef]
- Susilawathi, N.M.; Tini, K.; Wijayanti, I.A.S.; Rahmawati, P.L.; Wardhana, D.P.W.; Samatra, D.G.P.; Sudewi, A.A.R. Neurological manifestations of COVID-19: A clinical approach. Med. J. Indones. 2021, 30, 157–165. [Google Scholar] [CrossRef]
- Bulut, C.; Kato, Y. Epidemiology of COVID-19. Turk. J. Med. Sci. 2020, 50, 563–570. [Google Scholar] [CrossRef]
- World Health Organization. Asymptomatic COVID-19; WHO: Geneva, Switzerland, 2021; Available online: https://www.who.int/westernpacific/emergencies/covid-19/information/asymptomatic-covid-19 (accessed on 12 July 2025).
- Hadj Hassine, I. COVID-19 vaccines and variants of concern: A review. Rev. Med. Virol. 2022, 32, e2313. [Google Scholar] [CrossRef] [PubMed]
- Mohamadian, M.; Chiti, H.; Shoghli, A.; Biglari, S.; Parsamanesh, N.; Esmaeilzadeh, A. COVID-19: Virology, biology and novel laboratory diagnosis. J. Gene Med. 2021, 23, e3303. [Google Scholar] [CrossRef]
- Skrajnowska, D.; Brumer, M.; Kankowska, S.; Matysek, M.; Miazio, N.; Bobrowska-Korczak, B. COVID-19: Diet composition and health. Nutrients 2021, 13, 2980. [Google Scholar] [CrossRef] [PubMed]
- Krause, P.R.; Fleming, T.R.; Peto, R.; Longini, I.M.; Figueroa, J.P.; Sterne, J.A.C.; Cravioto, A.; Rees, H.; Higgins, J.P.T.; Boutron, I.; et al. SARS-CoV-2 variants and vaccines. N. Engl. J. Med. 2021, 385, 179–186. [Google Scholar] [CrossRef]
- Sharma, K.; Koirala, A.; Nicolopoulos, K.; Chiu, C.; Wood, N.; Britton, P.N. Vaccines for COVID-19: Where do we stand in 2021? Paediatr. Respir. Rev. 2021, 39, 22–31. [Google Scholar] [CrossRef]
- Nachega, J.B.; Sam-Agudu, N.A.; Mellors, J.W.; Zumla, A.; Mofenson, L.M. Scaling up COVID-19 vaccination in Africa—Lessons from the HIV pandemic. N. Engl. J. Med. 2021, 385, 196–198. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhao, S.; Teng, T.; Abdalla, A.E.; Zhu, W.; Xie, L.; Wang, Y.; Guo, X. Systematic Comparison of Two Animal-to-Human Transmitted Human Coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses 2020, 12, 244. [Google Scholar] [CrossRef]
- Ilyas, U.; Jadoon, S.S.; Ahmed, T.; Iqbal, S.; Khan, M.A.; Khan, S.; Ullah, A. COVID-19 and progress in therapeutic approaches: A narrative review. Çukurova Med. J. 2024, 49, 204–223. [Google Scholar] [CrossRef]
- Yavuz, S.; Ünal, S. Antiviral treatment of COVID-19. Turk. J. Med. Sci. 2020, 50, 611–619. [Google Scholar] [CrossRef]
- Liu, L.; Kapralov, M.; Ashton, M. Plant-derived compounds as potential leads for new drug development targeting COVID-19. Phytother. Res. 2024, 38, 1522–1554. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020, 181, 271–280. [Google Scholar] [CrossRef]
- Khalili, J.S.; Zhu, H.; Mak, N.S.A.; Yan, Y.; Zhu, Y. Novel coronavirus treatment with ribavirin: Groundwork for an evaluation concerning COVID-19. J. Med. Virol. 2020, 92, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Zha, L.; Li, S.; Pan, L.; Tefsen, B.; Li, Y.; French, N.; Chen, L.; Yang, G.; Villanueva, E.V. Corticosteroid treatment of patients with coronavirus disease 2019 (COVID-19). Med. J. Aust. 2020, 212, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Hashemian, S.M.R.; Sheida, A.; Taghizadieh, M.; Jamaati, H.; Dastan, F.; Varahram, M.; Kazempour-Dizaji, M.; Yousefian, S.; Farzanegan, B.; Emami, H.; et al. Paxlovid (nirmatrelvir/ritonavir): A new approach to COVID-19 therapy? Biomed. Pharmacother. 2023, 162, 114367. [Google Scholar] [CrossRef] [PubMed]
- Abdelnabi, R.; Foo, C.S.; Kaptein, S.J.; Zhang, X.; Do, T.N.D.; Langendries, L.; Vangeel, L.; Breuer, J.; Pang, J.; Williams, R.; et al. The combined treatment of molnupiravir and favipiravir results in a potentiation of antiviral efficacy in a SARS-CoV-2 hamster infection model. EBioMedicine 2021, 73, 103595. [Google Scholar] [CrossRef]
- Hariyono, P.; Patramurti, C.; Candrasari, D.S.; Hariono, M. An integrated virtual screening of compounds from Carica papaya leaves against multiple protein targets of SARS-CoV-2. Results Chem. 2021, 3, 100113. [Google Scholar] [CrossRef] [PubMed]
- Gasmi, A.; Mujawdiya, P.K.; Lysiuk, R.; Shanaida, M.; Peana, M.; Gasmi Benahmed, A.; Beley, N.; Kovalska, N.; Bjørklund, G. Quercetin in the prevention and treatment of coronavirus infections: A focus on SARS-CoV-2. Pharmaceuticals 2022, 15, 1049. [Google Scholar] [CrossRef]
- Huang, F.; Li, Y.; Leung, E.L.-H.; Liu, Z.; Liu, J.; Wang, N.; Zhang, Y.; Zhou, H.; Wang, Y. A review of therapeutic agents and Chinese herbal medicines against SARS-CoV-2 (COVID-19). Pharmacol. Res. 2020, 158, 104929. [Google Scholar] [CrossRef]
- Khan, A.; Heng, W.; Wang, Y.; Qiu, J.; Wei, X.; Peng, S.; Liu, Y.; Li, X. In silico and in vitro evaluation of kaempferol as a potential inhibitor of the SARS-CoV-2 main protease (3CLpro). Phytother. Res. 2021, 35, 2841–2845. [Google Scholar] [CrossRef]
- Murali, M.; Nair, B.; Vishnu, V.R.; Aneesh, T.P.; Nath, L.R. 2,4-Dihydroxycinnamic acid as spike ACE2 inhibitor and apigenin as RdRp inhibitor in Nimbamritadi Panchatiktam Kashayam against COVID-19: An in silico and in vitro approach. Mol. Divers. 2023, 27, 2353–2363. [Google Scholar] [CrossRef]
- Chen, Y.W.; Yiu, C.P.B.; Wong, K.Y. Prediction of the SARS-CoV-2 (2019-nCoV) 3C-like protease (3CLpro) structure: Virtual screening reveals velpatasvir, ledipasvir, and other drug repurposing candidates. F1000Research 2020, 9, 129. [Google Scholar] [CrossRef]
- Tijssen, R.; Kraemer-Mbula, E. Research excellence in Africa: Policies, perceptions, and performance. Sci. Public Policy 2018, 45, 392–403. [Google Scholar] [CrossRef]
- African Union Commission. Science, Technology and Innovation Strategy for Africa 2024 (STISA-2024); African Union Commission: Addis Ababa, Ethiopia, 2014; Available online: https://au.int/en/documents/29957-doc-stisa-published_book (accessed on 20 July 2025).
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.-M.; Wang, W.; Song, Z.-G.; Hu, Y.; Tao, Z.-W.; Tian, J.-H.; Pei, Y.-Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, C.; Mathew, G.; Franchi, T.; Kerwan, A.; Griffin, M.; Del Mundo, J.S.; Ali, S.A.; Agha, M.; Agha, R. Impact of the coronavirus (COVID-19) pandemic on scientific research and implications for clinical academic training: A review. Int. J. Surg. 2021, 86, 57–63. [Google Scholar] [CrossRef]
- Kozlov, M. NIH to cut grants for COVID research, documents reveal. Nature 2025, 640, 17–18. Available online: https://www.nature.com/articles/d41586-025-00954-y (accessed on 13 August 2025).
- Aristodemou, L.; Galindo-Rueda, F.; Matsumoto, K.; Murakami, A. Measuring Governments’ R&D Funding Response to COVID-19: An Application of the OECD Fundstat Infrastructure to the Analysis of R&D Directionality; OECD Science, Technology and Industry Working Papers 2023, No. 2023/10; OECD Publishing: Paris, France, 2023. [Google Scholar]
- Uthman, O.A.; Wiysonge, C.S.; Ota, M.O.; Nicol, M.; Hussey, G.D.; Ndumbe, P.M.; Mayosi, B.M. Increasing the value of health research in the WHO African Region beyond 2015—Reflecting on the past, celebrating the present and building the future: A bibliometric analysis. BMJ Open 2015, 5, e006340. [Google Scholar] [CrossRef] [PubMed]
- Motshudi, M.C.; Naidoo, C.M.; Mkolo, N.M. The race against time for the enhancement of African national strategic plans in the neuroblastoma research heterogeneity. Publications 2024, 12, 45. [Google Scholar] [CrossRef]
- Heleta, S.; Jithoo, D. International research collaboration between South Africa and rest of the world: An analysis of 2012-2021 trends. Transform. High. Educ. 2023, 8, 246. [Google Scholar] [CrossRef]
- Miles, S.; Renedo, A.; Marston, C. Reimagining authorship guidelines to promote equity in co-produced academic collaborations. Glob. Public Health 2021, 17, 2547–2559. [Google Scholar] [CrossRef]
- Department of Higher Education and Training (DHET). White Paper for Post-School Education and Training: Building an Expanded, Effective and Integrated Post-School System; Department of Higher Education and Training: Pretoria, South Africa, 2013. Available online: https://www.dhet.gov.za/ (accessed on 20 July 2025).
- Talisuna, A.O.; Bonkoungou, B.; Mosha, F.S.; Struminger, B.B.; Lehmer, J.; Arora, S.; Conteh, I.N.; Appiah, J.A.; Nel, J.; Mehtar, S.; et al. The COVID-19 pandemic: Broad partnerships for the rapid scale-up of innovative virtual approaches for capacity building and credible information dissemination in Africa. Pan Afr. Med. J. 2020, 37, 255. [Google Scholar] [CrossRef]
- Kinyanjui, S.; Fonn, S.; Kyobutungi, C.; Vicente-Crespo, M.; Bonfoh, B.; Ndung’u, T.; Sewankambo, N.K.; Djimde, A.A.; Gaye, O.; Chirwa, T.; et al. Enhancing science preparedness for health emergencies in Africa through research capacity building. BMJ Glob. Health 2020, 5, e003072. [Google Scholar] [CrossRef]
- German Federal Ministry of Education and Research (BMBF). Scientific Publications per One Million Inhabitants. 2023. Available online: https://www.datenportal.bmbf.de/portal/en/Table-1.8.3.pdf (accessed on 6 November 2025).
- FAPESP. Scientific Papers Published by Each Brazilian State. Revista Pesquisa FAPESP. 2023. Available online: https://revistapesquisa.fapesp.br/en/scientific-papers-published-by-each-brazilian-state/ (accessed on 6 November 2025).
- Our World in Data. Scientific and Technical Journal Articles per Million People. 2022. Available online: https://ourworldindata.org/grapher/scientific-publications-per-million (accessed on 6 November 2025).
- OECD. France: Country Health Profile 2021; OECD/European Observatory on Health Systems and Policies: Paris, France, 2021; Available online: https://www.oecd.org/content/dam/oecd/en/publications/reports/2021/12/france-country-health-profile-2021_d1658aae/7d668926-en.pdf (accessed on 6 November 2025).
- Pacheco, C.M.; Salles, J.R.; Oliveira, L.A. COVID-19 Epidemiological Patterns in Brazil: A Cross-Sectional Study (2020–2023). BMC Infect. Dis. 2024, 24, 9598. [Google Scholar] [CrossRef]
- Galal, S.; African Countries with the Highest Gross Domestic Product (GDP) in 2025. Statista. 2025. Available online: https://www.statista.com/ (accessed on 12 July 2025).
- Simpkin, V.; Namubiru-Mwaura, E.; Clarke, L.; Mossialos, E. Investing in health R&D: Where we are, what limits us, and how to make progress in Africa. BMJ Glob. Health 2019, 4, e001047. [Google Scholar] [CrossRef]
- El Hajj, T.; Gregorius, S.; Pulford, J.; Bates, I. Strengthening capacity for natural sciences research: A qualitative assessment to identify good practices, capacity gaps and investment priorities in African research institutions. PLoS ONE 2020, 15, e0228261. [Google Scholar] [CrossRef] [PubMed]
- Homolak, J.; Kodvanj, I.; Virag, D. Preliminary analysis of COVID-19 academic information patterns: A call for open science in the times of closed borders. Scientometrics 2020, 124, 2687–2701. [Google Scholar] [CrossRef] [PubMed]
- Safitri, Y.; Ningsih, R.D.; Agustianingsih, D.P.; Nurhasanah, S.; Supriyanto, A.; Mutiarin, D.; Damayanti, T.P. COVID-19 impact on SDGs and the fiscal measures: Case of Indonesia. Int. J. Environ. Res. Public Health 2021, 18, 2911. [Google Scholar] [CrossRef] [PubMed]
- Takian, A.; Raoofi, A.; Haghighi, H. COVID-19 pandemic: The fears and hopes for SDG 3, with focus on prevention and control of noncommunicable diseases (SDG 3.4) and universal health coverage (SDG 3.8). In COVID-19 and the Sustainable Development Goals; Elsevier: Amsterdam, The Netherlands, 2022; pp. 211–234. [Google Scholar] [CrossRef]
- UNESCO. The UNESCO Science Report: Factsheet on SDG 3—Good Health and Well-Being; UNESCO: Paris, France, 2022; Available online: https://www.unesco.org/reports/science/2021/sites/default/files/medias/fichiers/2022/05/Factsheet%20USR21%20SDG%203.pdf (accessed on 10 August 2025).
- Yuan, H.; Wang, X.; Gao, L.; Sun, Y.; Zhang, R.; Wang, P.; Liu, J. Progress towards the Sustainable Development Goals has been slowed by indirect effects of the COVID-19 pandemic. Commun. Earth Environ. 2023, 4, 184. [Google Scholar] [CrossRef]
- Jones, K.E.; Patel, N.G.; Levy, M.A.; Storeygard, A.; Balk, D.; Gittleman, J.L.; Daszak, P. Global trends in emerging infectious diseases. Nature 2008, 451, 990–993. [Google Scholar] [CrossRef]
- Formenti, B.; Gregori, N.; Crosato, V.; Marchese, V.; Tomasoni, L.R.; Castelli, F. The impact of COVID-19 on communicable and non-communicable diseases in Africa: A narrative review. Infez. Med. 2022, 30, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Lawson-Lartego, L.; Cohen, M.J. Ten recommendations for African governments to ensure food security for poor and vulnerable populations during COVID-19. Food Secur. 2020, 12, 899–902. [Google Scholar] [CrossRef] [PubMed]








| Classification | Symptoms | Reference |
|---|---|---|
| Asymptomatic | No clinical symptoms in infected individuals | [18] |
| Mild | Infected individuals experience symptoms such as sore throat, cough, runny nose, sneezing, fever, fatigue, and myalgia | [19] |
| Moderate | Cough, regular fever, and pneumonia | [18] |
| Severe | Difficulty breathing, chest pain, loss of speech, death | [19] |
| Critical | Respiratory failure, shock, multiple organ dysfunction, and death | [19] |
| Research Area Category | Subject Area | Publications % | Sustainable Development Goals (SDGs) |
|---|---|---|---|
| Social Sciences and Humanities | Social Sciences | 14.51 | SDG 16 (Peace, Justice and Strong Institutions), SDG 10 (Reduced Inequalities), SDG 1 (No Poverty) |
| Arts and Humanities | 4.00 | SDG 11 (Sustainable Cities and Communities), SDG 4 (Quality Education) | |
| Business, Management, and Accounting | 3.58 | SDG 9 (Industry, Innovation and Infrastructure), SDG 8 (Decent Work and Economic Growth), | |
| Economics, Econometrics, and Finance | 2.72 | SDG 8 (Decent Work and Economic Growth), SDG 1 (No Poverty) | |
| Psychology | 1.91 | SDG 3 (Good Health and Well-Being) | |
| Decision Sciences | 0.74 | SDG 12 (Responsible Consumption and Production), SDG 9 (Industry, Innovation and Infrastructure) | |
| Health and Life Sciences | Medicine | 33.96 | SDG 3 (Good Health and Well-Being) |
| Pharmacology, Toxicology, and Pharmaceutics | 4.14 | SDG 3 (Good Health and Well-Being) | |
| Nursing | 4.01 | SDG 3 (Good Health and Well-Being) | |
| Biochemistry, Genetics, and Molecular Biology | 3.23 | SDG 9 (Industry, Innovation and Infrastructure), SDG 3 (Good Health and Well-Being) | |
| Health Professions | 3.01 | SDG 3 (Good Health and Well-Being) | |
| Immunology and Microbiology | 2.44 | SDG 3 (Good Health and Well-Being) | |
| Neuroscience | 0.83 | SDG 3 (Good Health and Well-Being) | |
| Veterinary | 0.46 | SDG 3 (Good Health and Well-Being) and SDG 2 (Zero Hunger), | |
| Dentistry | 0.34 | SDG 3 (Good Health and Well-Being) | |
| Engineering and Technology | Engineering | 3.92 | SDG 9 (Industry, Innovation and Infrastructure) |
| Computer Science | 2.81 | SDG 9 (Industry, Innovation and Infrastructure) | |
| Chemical Engineering | 0.71 | SDG 12 (Responsible Consumption and Production) and SDG 9 (Industry, Innovation and Infrastructure) | |
| Energy | 0.56 | SDG 13 (Climate Action) and SDG 7 (Affordable and Clean Energy) | |
| Natural Sciences | Environmental Science | 2.24 | SDG 15 (Life on Land) and SDG 13 (Climate Action) |
| Agricultural and Biological Sciences | 1.29 | SDG 15 (Life on Land) and SDG 2 (Zero Hunger) | |
| Earth and Planetary Sciences | 0.65 | SDG 15 (Life on Land), SDG 14 (Life Below Water), SDG 13 (Climate Action), | |
| Physics and Astronomy | 0.65 | SDG 9 (Industry, Innovation and Infrastructure) | |
| Chemistry | 1.43 | SDG 12 (Responsible Consumption and Production), SDG 9 (Industry, Innovation and Infrastructure) | |
| Materials Science | 1.22 | SDG 12 (Responsible Consumption and Production) and SDG 9 (Industry, Innovation and Infrastructure) | |
| Mathematics | 1.53 | SDG 9 (Industry, Innovation and Infrastructure) and SDG 4 (Quality Education), | |
| Multidisciplinary Fields | Multidisciplinary | 3.10 | Multiple SDGs are reliant on the study focus area |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makhafola, M.A.; Naidoo, C.M.; Mkolo, N.M. Transforming COVID-19 Research Priorities for Sustainable Development in Africa. World 2025, 6, 157. https://doi.org/10.3390/world6040157
Makhafola MA, Naidoo CM, Mkolo NM. Transforming COVID-19 Research Priorities for Sustainable Development in Africa. World. 2025; 6(4):157. https://doi.org/10.3390/world6040157
Chicago/Turabian StyleMakhafola, Mmamudi Anna, Clarissa Marcelle Naidoo, and Nqobile Monate Mkolo. 2025. "Transforming COVID-19 Research Priorities for Sustainable Development in Africa" World 6, no. 4: 157. https://doi.org/10.3390/world6040157
APA StyleMakhafola, M. A., Naidoo, C. M., & Mkolo, N. M. (2025). Transforming COVID-19 Research Priorities for Sustainable Development in Africa. World, 6(4), 157. https://doi.org/10.3390/world6040157








