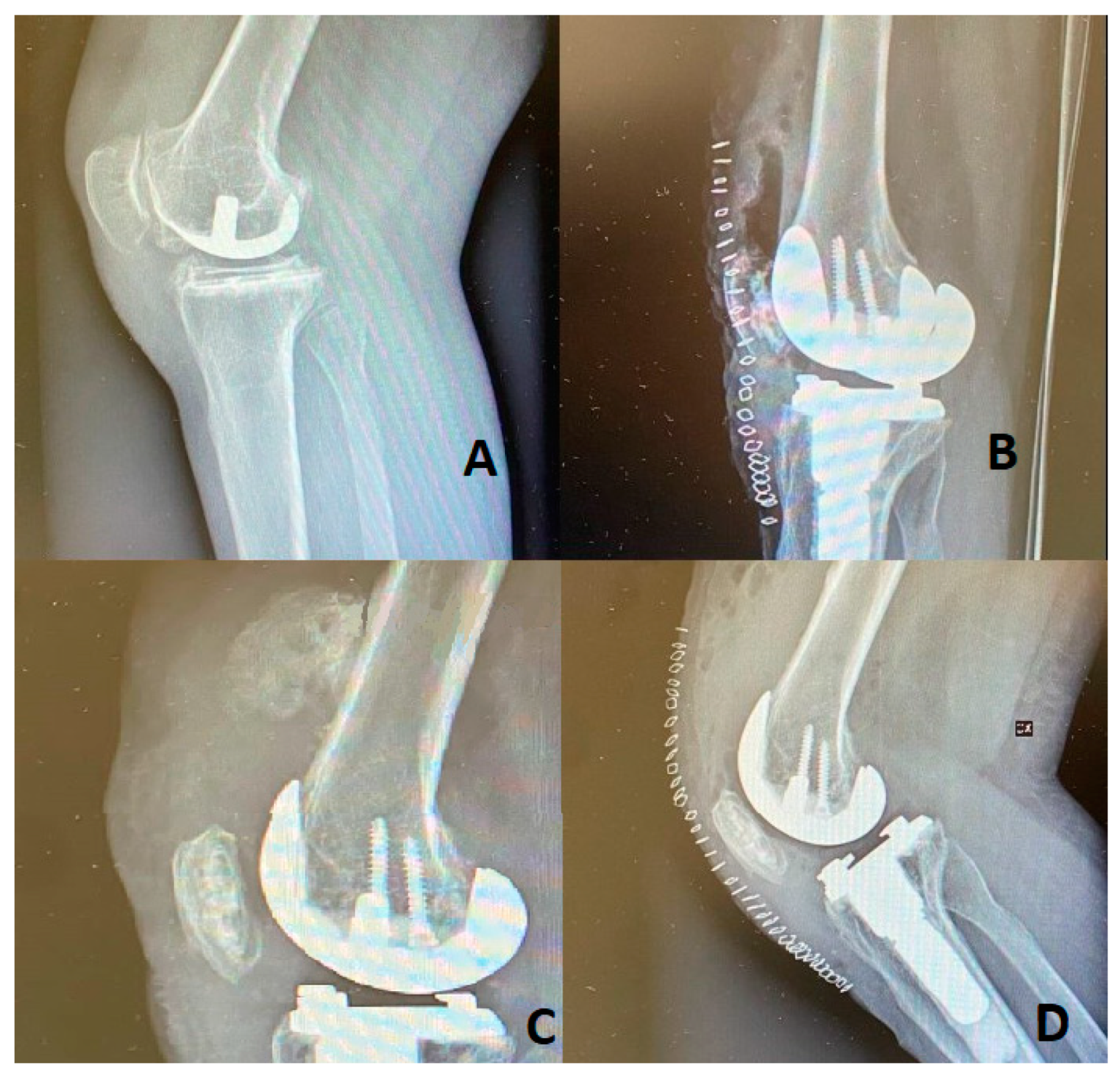
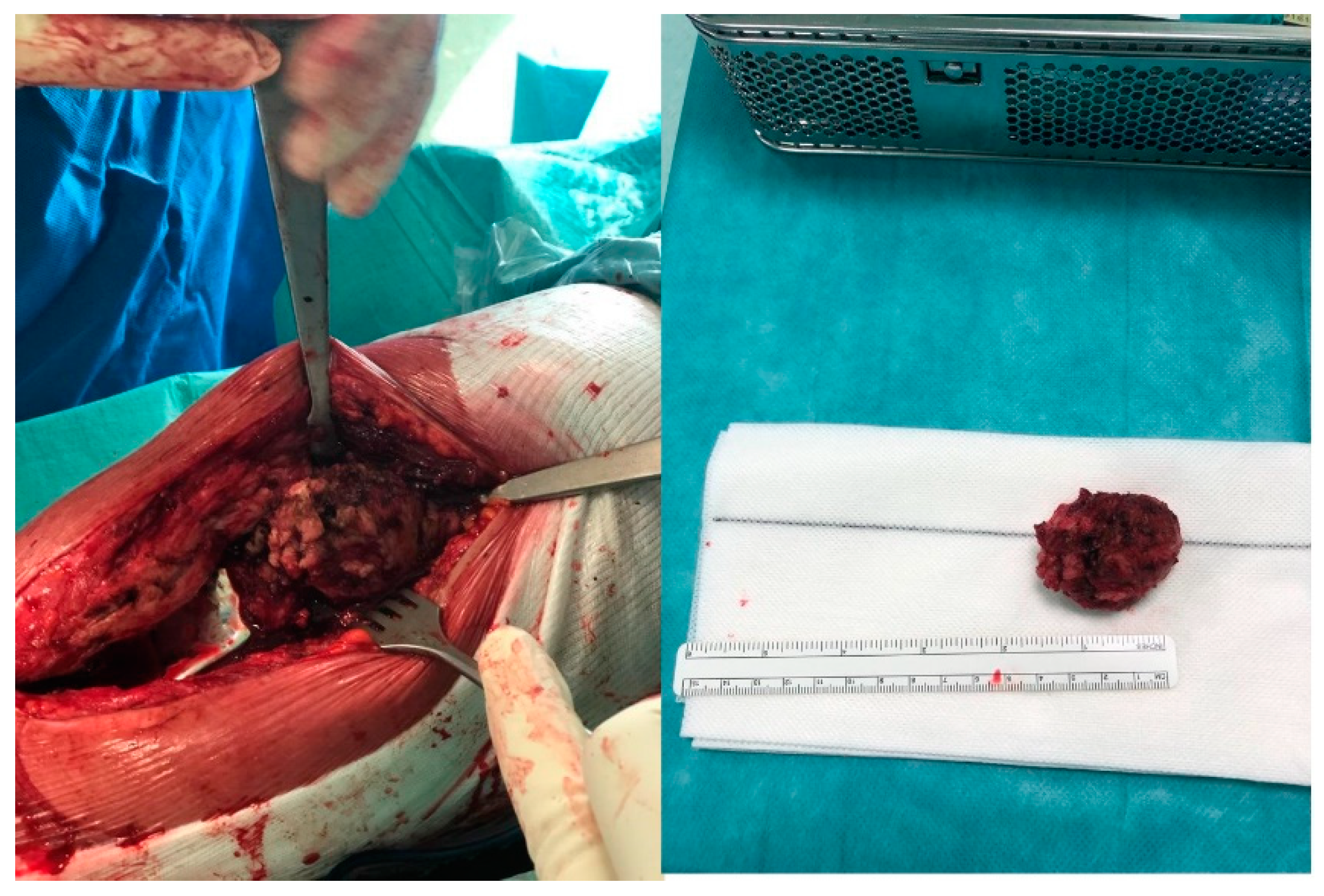
Severe Quadriceps Heterotopic Ossification after Knee Revision Arthroplasty in a 42-Year-Old Suffering from Rheumatoid Arthritis: A Case Report
Abstract
1. Introduction
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lespasio, M.J.; Guarino, A.J. Awareness of Heterotopic Ossification in Total Joint Arthroplasty: A Primer. Perm. J. 2020, 24, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Sterner, T.; Saxler, G.; Barden, B. Limited range of motion caused by heterotopic ossifications in primary total knee arthroplasty: A retrospective study of 27/191 cases. Arch. Orthop. Trauma Surg. 2005, 125, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Eggli, S.; Woo, A. Risk factors for heterotopic ossification in total hip arthroplasty. Arch. Orthop. Trauma Surg. 2001, 121, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Morcos, M.; Smith, K.; Tanzer, M. The effect of late radiotherapy on the progression of heterotopic ossification following total hip arthroplasty. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2018, 28, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, F.; Memon, N.; Noor, S.S.; Ahmed, N.; Sozera, M.F.; Abro, A. Bilateral severe heterotopic ossification following primary total knee arthroplasty: A case report in Pakistan. Arthroplasty 2021, 3, 5. [Google Scholar] [CrossRef] [PubMed]
- Gkiatas, I.; Xiang, W.; Nocon, A.A.; Youssef, M.P.; Tarity, T.D.; Sculco, P.K. Heterotopic Ossification Negatively Influences Range of Motion After Revision Total Knee Arthroplasty. J. Arthroplast. 2021, 36, 2907–2912. [Google Scholar] [CrossRef] [PubMed]
- Heterotopic Ossification; Craig Hospital: Englewood, CO, USA, 2015; Available online: https://craighospital.org/resources/heterotopic-ossification (accessed on 3 January 2020).
- Daugherty, L.C.; Bell, J.R.; Fisher, B.J.; Sankhla, N.; Tzou, K.S.; Troicki, F.T.; Wong, M.; Komarnicky, L.T.; Brady, L.W. Radiation prophylaxis as primary prevention of heterotopic ossification of the knee: Classification of disease and indications for treatment. J. Radiat. Oncol. 2012, 2, 87–94. [Google Scholar] [CrossRef][Green Version]
- Gkiatas, I.; Xiang, W.; Karasavvidis, T.; Windsor, E.N.; Malahias, M.A.; Tarity, T.D.; Sculco, P.K. Relatively Low Rate of Heterotopic Ossification Following Primary Total Knee Arthroplasty: A Systematic Review and Meta-analysis. Journal of the American Academy of Orthopaedic Surgeons. Glob. Res. Rev. 2021, 5, e21.00096. [Google Scholar] [CrossRef]
- Oberberg, S.; Nottenkämper, J.; Heukamp, M.; Krapp, J.; Willburger, R.E. Etoricoxib is safe and effective in preventing heterotopic ossification after primary total hip arthroplasty. J. Orthop. Surg. Res. 2021, 16, 163. [Google Scholar] [CrossRef] [PubMed]
- Kölbl, O.; Barthel, T.; Krödel, A.; Seegenschmiedt, M.H. Prävention von heterotopen Ossifikationen nach Totalendoprothese des Hüftgelenks. Dtsch. Ärzteblatt Int. 2003, 100, 2944–2954. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Massaro, M.; Mela, F.; Esposito, R.; Maiorano, E.; Laskow, G. Severe Quadriceps Heterotopic Ossification after Knee Revision Arthroplasty in a 42-Year-Old Suffering from Rheumatoid Arthritis: A Case Report. Osteology 2022, 2, 161-165. https://doi.org/10.3390/osteology2040019
Massaro M, Mela F, Esposito R, Maiorano E, Laskow G. Severe Quadriceps Heterotopic Ossification after Knee Revision Arthroplasty in a 42-Year-Old Suffering from Rheumatoid Arthritis: A Case Report. Osteology. 2022; 2(4):161-165. https://doi.org/10.3390/osteology2040019
Chicago/Turabian StyleMassaro, Michele, Federico Mela, Roberto Esposito, Emanuele Maiorano, and Guy Laskow. 2022. "Severe Quadriceps Heterotopic Ossification after Knee Revision Arthroplasty in a 42-Year-Old Suffering from Rheumatoid Arthritis: A Case Report" Osteology 2, no. 4: 161-165. https://doi.org/10.3390/osteology2040019
APA StyleMassaro, M., Mela, F., Esposito, R., Maiorano, E., & Laskow, G. (2022). Severe Quadriceps Heterotopic Ossification after Knee Revision Arthroplasty in a 42-Year-Old Suffering from Rheumatoid Arthritis: A Case Report. Osteology, 2(4), 161-165. https://doi.org/10.3390/osteology2040019





