Does Calm Always Follow the Storm? A Comprehensive Temporal Analysis of Emergency Department Visits in Northern Italy Before and After the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
3. Results
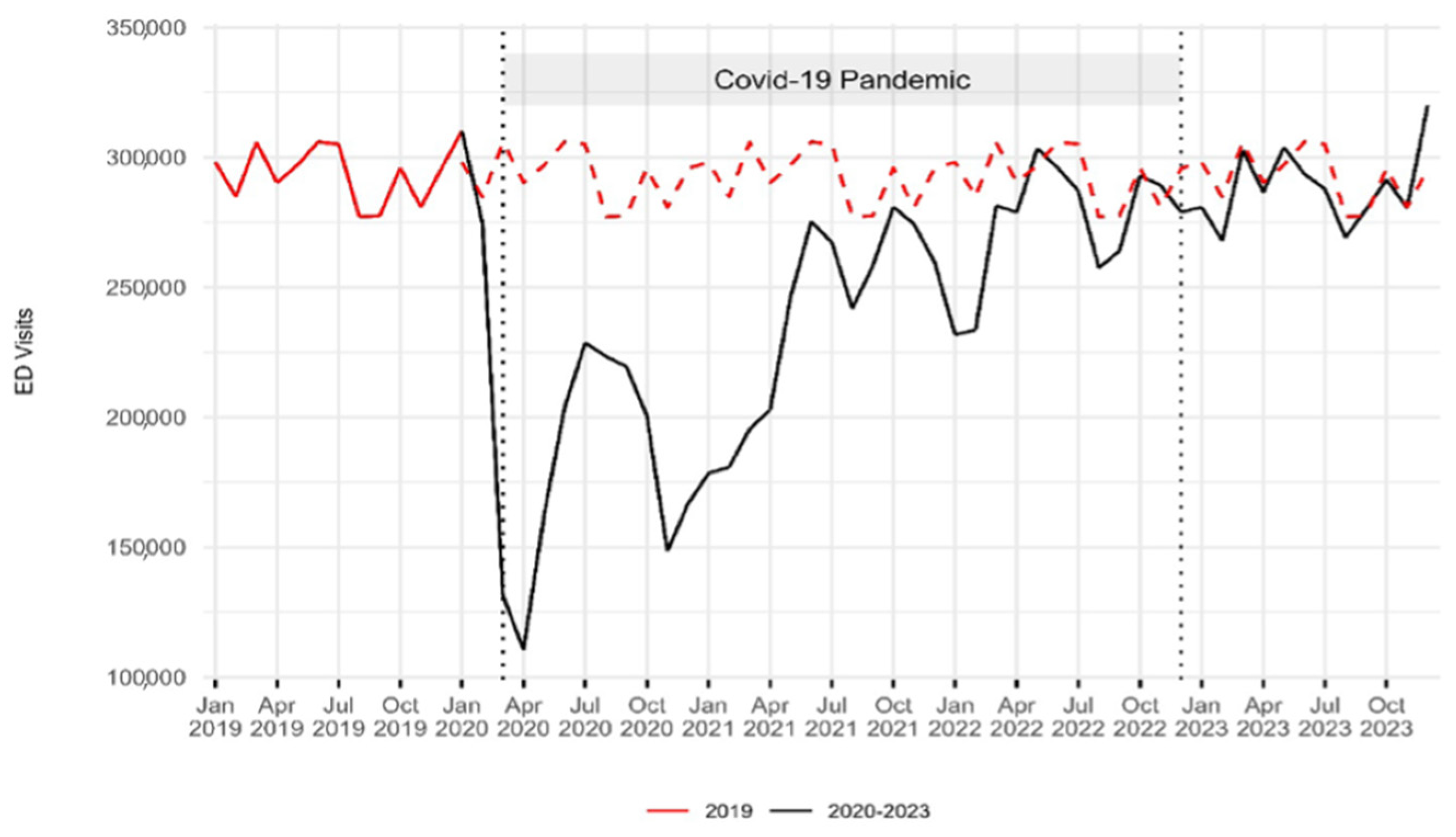
3.1. Study Sample and ED Visit Volumes
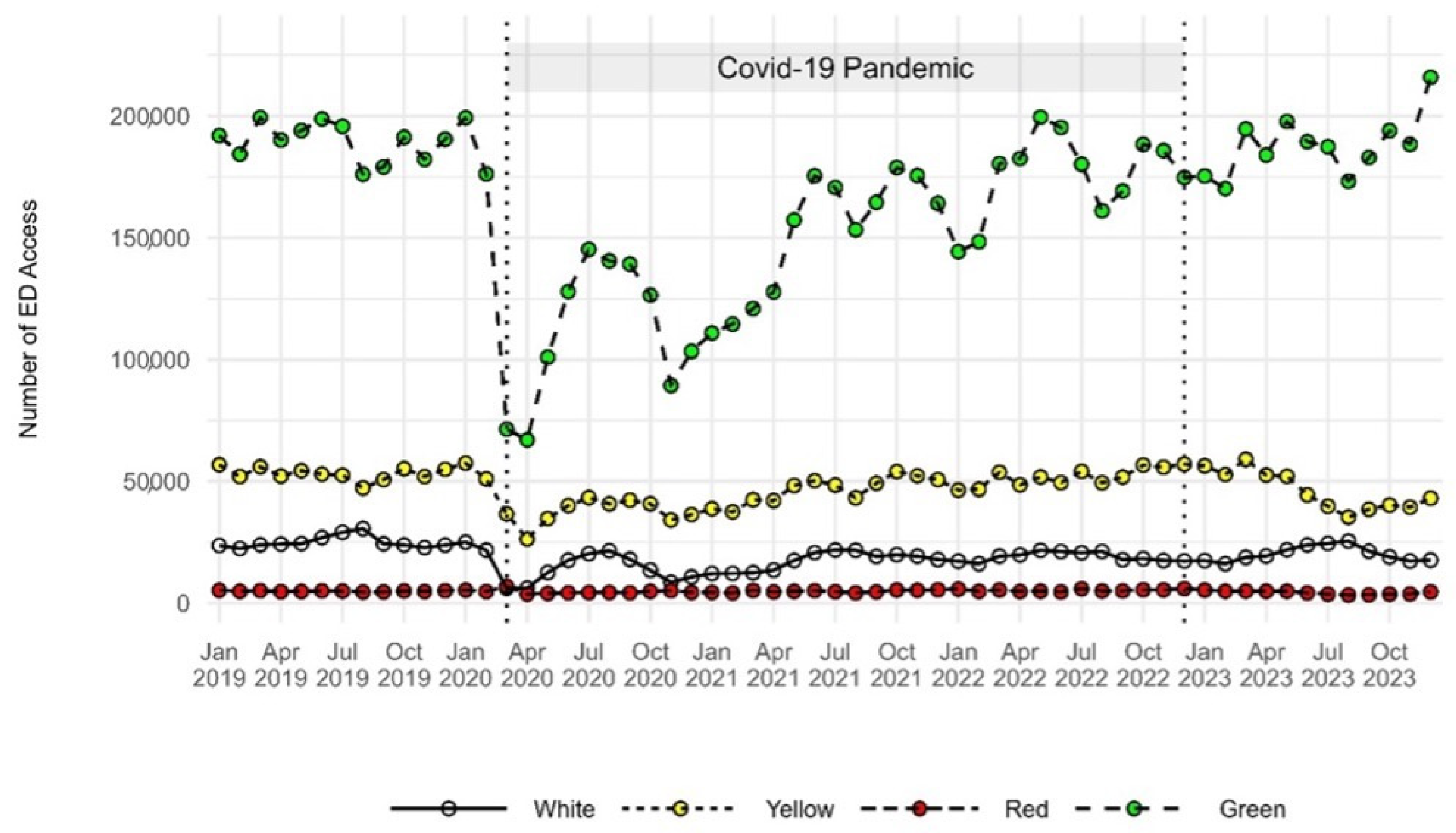
3.2. Acuity Level
3.3. Arrival by Emergency Vehicle
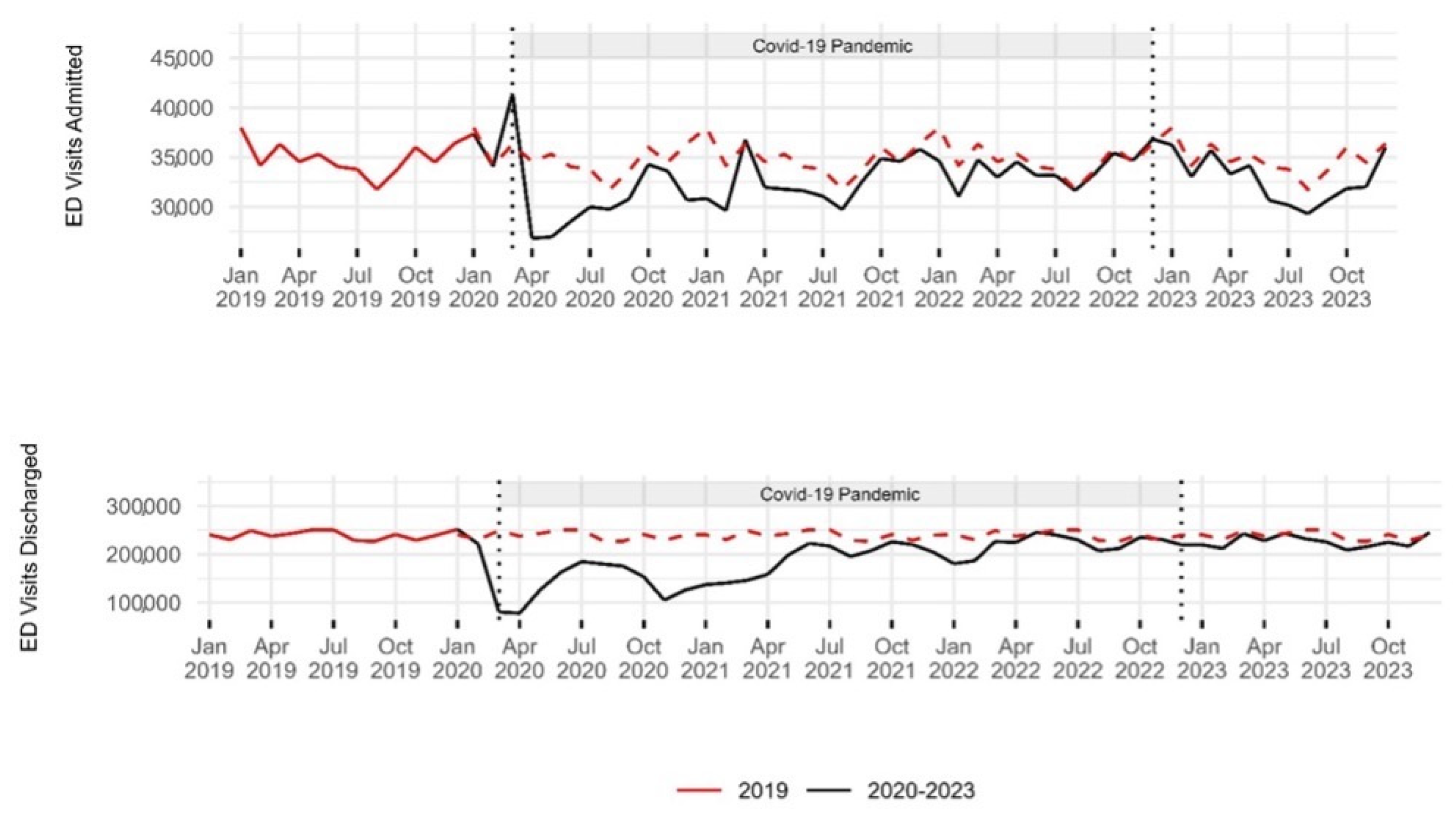
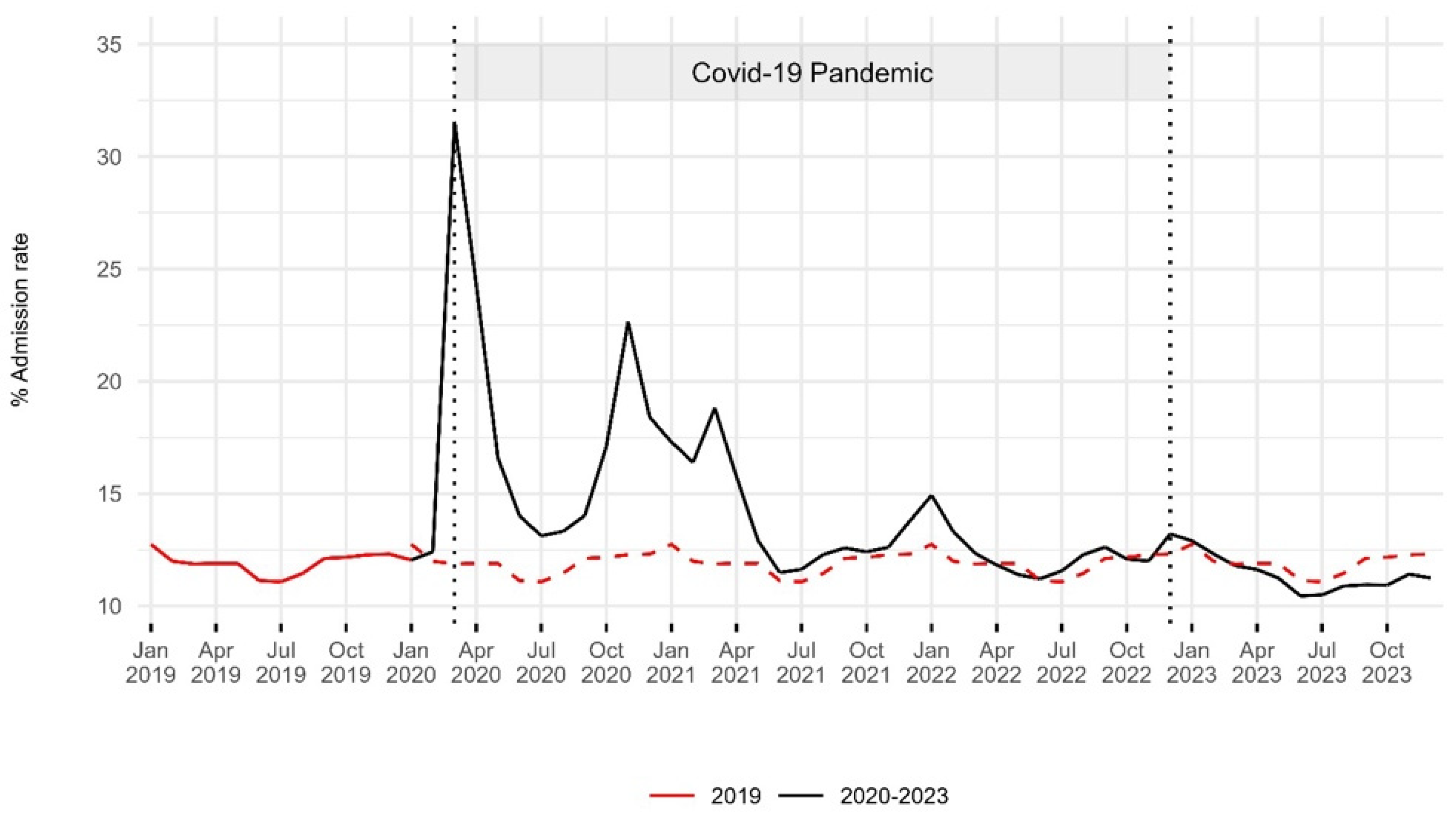
3.4. Hospital Admission Rate
3.5. ED Crowding Metrics
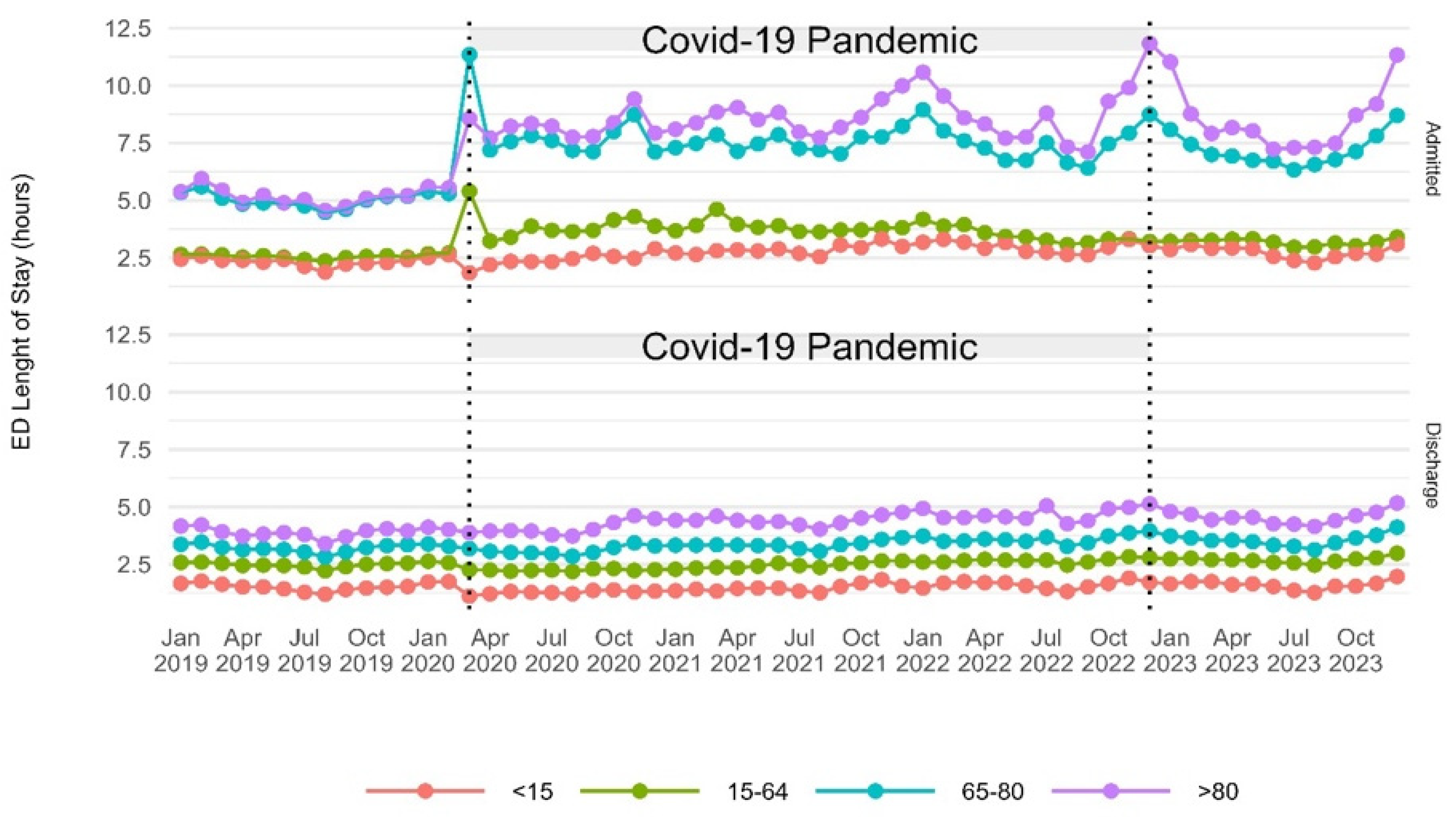
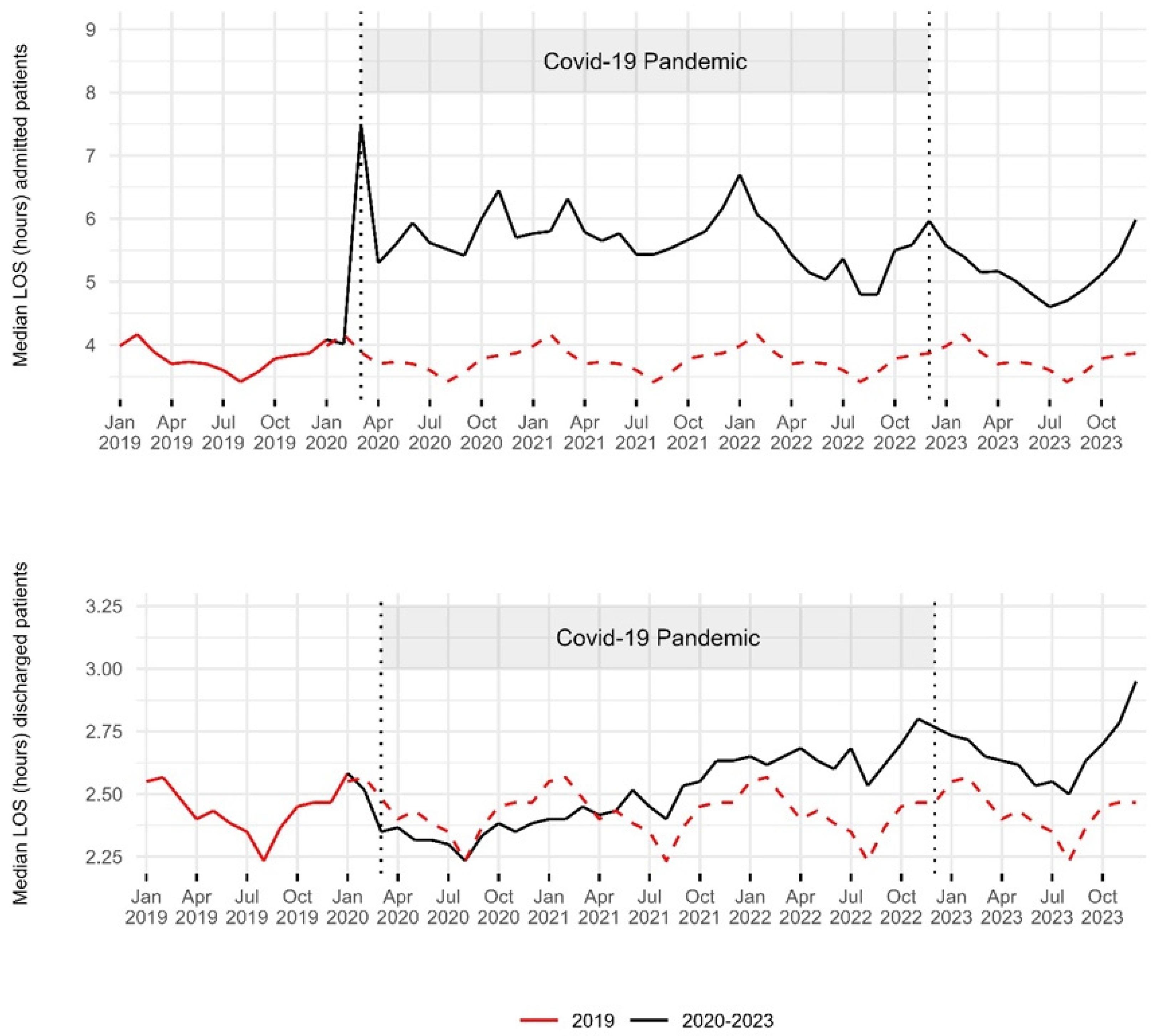
3.5.1. Median ED Length of Stay
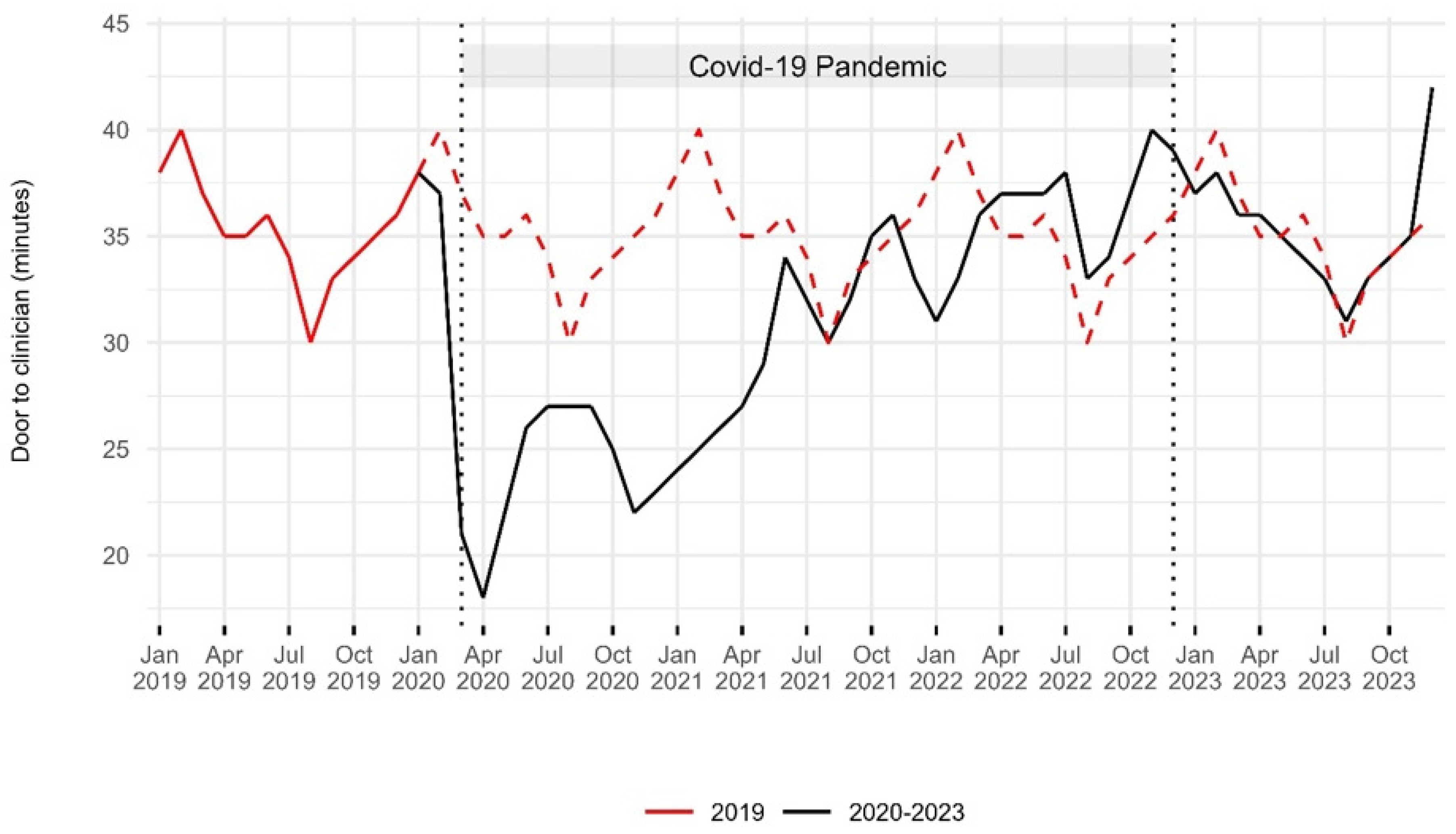
3.5.2. Door-to-Clinician Time
3.5.3. Rate of Patients Leaving Before Treatment Completion
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Oskvarek, J.J.; Zocchi, M.S.; Black, B.S.; Celedon, P.; Leubitz, A.; Moghtaderi, A.; Nikolla, D.A.; Rahman, N.; Pines, J.M. Emergency Department Volume, Severity, and Crowding Since the Onset of the Coronavirus Disease 2019 Pandemic. Ann. Emerg. Med. 2023, 82, 650–660. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.J.; Stiell, I.; Wells, G.; Lee, A.J.; Van Walraven, C. The Effect of Hospital Occupancy on Emergency Department Length of Stay and Patient Disposition. Acad. Emerg. Med. 2003, 10, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Janke, A.T.; Melnick, E.R.; Venkatesh, A.K. Hospital Occupancy and Emergency Department Boarding During the COVID-19 Pandemic. JAMA Netw. Open 2022, 5, e2233964. [Google Scholar] [CrossRef] [PubMed]
- Chun, S.Y.; Kim, H.J.; Kim, H.B. The Effect of COVID-19 Pandemic on the Length of Stay and Outcomes in the Emergency Department. Clin. Exp. Emerg. Med. 2022, 9, 128–133. [Google Scholar] [CrossRef]
- Kelen, G.D.; Wolfe, R.; D’Onofrio, G.; Mills, A.M.; Diercks, D.; Stern, S.A.; Wadman, M.C.; Sokolove, P.E. Emergency Department Crowding: The Canary in the Health Care System. NEJM Catal. 2021, 5, 7. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0217 (accessed on 25 February 2025).
- Institute of Medicine; Board on Health Care Services; Committee on the Future of Emergency Care in the United States Health System. Hospital-Based Emergency Care: At the Breaking Point; National Academies Press: Washington, DC, USA, 2007; p. 11621. ISBN 978-0-309-10173-8. [Google Scholar]
- Cowling, T.E.; Cecil, E.V.; Soljak, M.A.; Lee, J.T.; Millett, C.; Majeed, A.; Wachter, R.M.; Harris, M.J. Access to Primary Care and Visits to Emergency Departments in England: A Cross-Sectional, Population-Based Study. PLoS ONE 2013, 8, e66699. [Google Scholar] [CrossRef]
- Morley, C.; Unwin, M.; Peterson, G.M.; Stankovich, J.; Kinsman, L. Emergency Department Crowding: A Systematic Review of Causes, Consequences and Solutions. PLoS ONE 2018, 13, e0203316. [Google Scholar] [CrossRef]
- Guarducci, G.; Lorenzini, C.; Ciacci, D. How to Reduce Erroneous Emergency Department Admissions for the Frail Elderly. Ann. Ig. Med. Prev. E Comunità 2023, 35, 695–706. [Google Scholar] [CrossRef]
- Javidan, A.P.; Hansen, K.; Higginson, I.; Jones, P.; Lang, E. International Federation for Emergency Medicine Report from the Emergency Department Crowding and Access Block Task Force. Emerg. Med. J. 2021, 38, 245–246. [Google Scholar] [CrossRef]
- Pearce, S.; Marchand, T.; Shannon, T.; Ganshorn, H.; Lang, E. Emergency Department Crowding: An Overview of Reviews Describing Measures Causes, and Harms. Intern. Emerg. Med. 2023, 18, 1137–1158. [Google Scholar] [CrossRef]
- Asplin, B.R.; Magid, D.J.; Rhodes, K.V.; Solberg, L.I.; Lurie, N.; Camargo, C.A. A Conceptual Model of Emergency Department Crowding. Ann. Emerg. Med. 2003, 42, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Forero, R.; McCarthy, S.; Hillman, K. Access block and emergency department overcrowding. Crit. Care 2011, 15, 216. [Google Scholar] [CrossRef] [PubMed]
- Ministero della Salute. Linee Di Indirizzo Nazionali Sul Triage Intraospedaliero. 2019. Available online: https://www.Salute.Gov.It/Imgs/C_17_pubblicazioni_3145_allegato.Pdf (accessed on 15 July 2024).
- Drew, R. Access Block Point Prevalence; Survey; The Road Trauma and Emergency Medicine Unit Australian National University, The Australasian College for Emergency Medicine: Melbourne, Australia, 2016. [Google Scholar]
- Pines, J.M.; Griffey, R.T. What We Have Learned From a Decade of ED Crowding Research. Acad. Emerg. Med. 2015, 22, 985–987. [Google Scholar] [CrossRef]
- Pines, J.M.; Hilton, J.A.; Weber, E.J.; Alkemade, A.J.; Al Shabanah, H.; Anderson, P.D.; Bernhard, M.; Bertini, A.; Gries, A.; Ferrandiz, S.; et al. International Perspectives on Emergency Department Crowding. Acad. Emerg. Med. 2011, 18, 1358–1370. [Google Scholar] [CrossRef]
- Mataloni, F.; Pinnarelli, L.; Perucci, C.A.; Davoli, M.; Fusco, D. Characteristics of ED Crowding in the Lazio Region (Italy) and Short-Term Health Outcomes. Intern. Emerg. Med. 2019, 14, 109–117. [Google Scholar] [CrossRef]
- Buja, A.; Saia, M.; Fusinato, R.; Fonzo, M.; Bertoncello, C.; Baldo, V. Uncompleted Emergency Department Care (UEDC): A 5-Year Population-Based Study in Veneto Region, Italy. J. Prev. Med. Hyg. 2019, 60, E18. [Google Scholar] [CrossRef]
- Lucero, A.; Sokol, K.; Hyun, J.; Pan, L.; Labha, J.; Donn, E.; Kahwaji, C.; Miller, G. Worsening of Emergency Department Length of Stay during the COVID-19 Pandemic. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12489. [Google Scholar] [CrossRef]
- Schranz, M.; Boender, T.S.; Greiner, T.; Kocher, T.; Wagner, B.; Greiner, F.; Bienzeisler, J.; Diercke, M.; Grabenhenrich, L.; AKTIN-Research Group; et al. Changes in Emergency Department Utilisation in Germany before and during Different Phases of the COVID-19 Pandemic, Using Data from a National Surveillance System up to June 2021. BMC Public Health 2023, 23, 799. [Google Scholar] [CrossRef]
- Wyatt, S.; Mohammed, M.A.; Fisher, E.; McConkey, R.; Spilsbury, P. Impact of the SARS-CoV-2 Pandemic and Associated Lockdown Measures on Attendances at Emergency Departments in English Hospitals: A Retrospective Database Study. Lancet Reg. Health Eur. 2021, 2, 100034. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Alfaraj, D.; AlHumaid, J.; Alshahrani, K.; Alsubaie, A.; Almulhim, N.; Althawadi, D.; Alam, S.; Alzahrani, M.; Alwosibai, H.; et al. Prevalence, Causes, and Adverse Clinical Impact of Delayed Presentation of Non-COVID-19-Related Emergencies during the COVID-19 Pandemic: Findings from a Multicenter Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 9818. [Google Scholar] [CrossRef]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed Access or Provision of Care in Italy Resulting from Fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Camine, T.; Rembisz, A.; Barron, R.; Baldwin, C.; Kromer, M. Decrease in Trauma Admissions with COVID-19 Pandemic. West. J. Emerg. Med. 2020, 21, 819. [Google Scholar] [CrossRef] [PubMed]
- Jojczuk, M.; Pawlikowski, J.; Kamiński, P.; Głuchowski, D.; Naylor, K.; Gajewski, J.; Karpiński, R.; Krakowski, P.; Jonak, J.; Nogalski, A.; et al. Evaluating Changes in Trauma Epidemiology during the COVID-19 Lockdown: Insights and Implications for Public Health and Disaster Preparedness. Healthcare 2023, 11, 2436. [Google Scholar] [CrossRef]
- Bhambhvani, H.P.; Rodrigues, A.J.; Yu, J.S.; Carr, J.B.; Hayden Gephart, M. Hospital Volumes of 5 Medical Emergencies in the COVID-19 Pandemic in 2 US Medical Centers. JAMA Intern. Med. 2021, 181, 272. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità Dati Della Sorveglianza Integrata COVID-19 in Italia. Available online: https://www.epicentro.iss.it/Coronavirus/Sars-Cov-2-Dashboard (accessed on 1 February 2024).
- Ministero della Salute di Italia. Annuario Statistico Del Servizio Sanitario Nazionale. Available online: https://www.salute.gov.it/Portale/Temi/P2_6.Jsp?lingua=italiano&id=3835&area=statisticheSSN&menu=annuario (accessed on 15 July 2024).
- Tang, X.R.; Zarisfi, F.; Pek, P.P.; Siddiqui, F.J.; Malhotra, R.; Kwan, Y.H.; Ling, T.; Ho, A.F.W.; Ong, M.E.H. Emergency Department Utilisation among Older Adults—Protocol for a Systematic Review of Determinants and Conceptual Frameworks. PLoS ONE 2022, 17, e0265423. [Google Scholar] [CrossRef]
- Rotulo, G.A.; Percivale, B.; Molteni, M.; Naim, A.; Brisca, G.; Piccotti, E.; Castagnola, E. The Impact of COVID-19 Lockdown on Infectious Diseases Epidemiology: The Experience of a Tertiary Italian Pediatric Emergency Department. Am. J. Emerg. Med. 2021, 43, 115–117. [Google Scholar] [CrossRef]
- Di Fabrizio, V.; Cerini, G.; Rosselli, A.; Szasz, C.; Gemmi, F. Gli Anni della Pandemia da COVID-19: Effetti Sugli Accessi al Pronto Soccorso in Regione Toscana. Available online: https://www.ars.toscana.it/2-articoli/4782-gli-anni-della-pandemia-da-covid-19-effetti-sugli-accessi-al-pronto-soccorso-in-regione-toscana.html (accessed on 15 July 2024).
- Sancton, K.; Sloss, L.; Berkowitz, J.; Strydom, N.; McCracken, R. Low-Acuity Presentations to the Emergency Department: Reasons for and access to other health care providers before presentation. Can. Fam. Physician 2018, 64, e354–e360. [Google Scholar]
- Cowling, T.E.; Harris, M.J.; Watt, H.C.; Gibbons, D.C.; Majeed, A. Access to General Practice and Visits to Accident and Emergency Departments in England: Cross-Sectional Analysis of a National Patient Survey. Br. J. Gen. Pract. 2014, 64, e434–e439. [Google Scholar] [CrossRef]
- Moineddin, R.; Meaney, C.; Agha, M.; Zagorski, B.; Glazier, R.H. Modeling Factors Influencing the Demand for Emergency Department Services in Ontario: A Comparison of Methods. BMC Emerg. Med. 2011, 11, 13. [Google Scholar] [CrossRef]
- SIMG—Sanità Territoriale in Lombardia al Bivio: Mancano i Medici Di Famiglia. Maggio. 2024. Available online: https://www.simg.it/Simg-Sanita-Territoriale-in-Lombardia-al-Bivio-Mancano-i-Medici-Di-Famiglia-Rimasti-Scoperti-Fino-al-90-Dei-Posti-Disponibili-Dal-2030-Cambiera-Landamento/ (accessed on 9 February 2024).
- Stephenson, M.D.; Lisy, K.; Stern, C.J.; Feyer, A.-M.; Fisher, L.; Aromataris, E.C. The Impact of Integrated Care for People with Chronic Conditions on Hospital and Emergency Department Utilization: A Rapid Review. Int. J. Evid. Based Healthc. 2019, 17, 14–26. [Google Scholar] [CrossRef]
- Stirparo, G.; Kacerik, E.; Andreassi, A.; Pausilli, P.; Cortellaro, F.; Coppo, A.; Migliari, M.; Albonico, A.; Sechi, G.M.; Zoli, A.; et al. Emergency Department Waiting-Time in the Post Pandemic Era: New Organizational Models, a Challenge for the Future. Acta Biomed. Atenei Parm. 2023, 94, e2023122. [Google Scholar] [CrossRef]
- Stirparo, G.; Pireddu, R.; Andreassi, A.; Sechi, G.M.; Signorelli, C. Social Illness Before and After the COVID-19 Pandemic: A Regional Study. Prehosp. Disaster Med. 2023, 38, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Di Fabrizio, V.; Cerini, G.; Szasz, C.; Gemmi, F. Gli Effetti della Pandemia da COVID-19 Sugli Accessi in Pronto Soccorso: Aggiornamento al 2022. Available online: https://www.ars.toscana.it/2-articoli/4927-effetti-pandemia-da-covid-19-su-accessi-in-pronto-soccorso-aggiornamento-al-2022.html (accessed on 15 July 2024).
- Morello, F.; Bima, P.; Ferreri, E.; Chiarlo, M.; Balzaretti, P.; Tirabassi, G.; Petitti, P.; Aprà, F.; Vallino, D.; Carbone, G.; et al. After the First Wave and beyond Lockdown: Long-Lasting Changes in Emergency Department Visit Number, Characteristics, Diagnoses, and Hospital Admissions. Intern. Emerg. Med. 2021, 16, 1683–1690. [Google Scholar] [CrossRef] [PubMed]
- Gorski, J.K.; Arnold, T.S.; Usiak, H.; Showalter, C.D. Crowding Is the Strongest Predictor of Left without Being Seen Risk in a Pediatric Emergency Department. Am. J. Emerg. Med. 2021, 48, 73–78. [Google Scholar] [CrossRef]
- Savioli, G.; Ceresa, I.; Guarnone, R.; Muzzi, A.; Novelli, V.; Ricevuti, G.; Iotti, G.; Bressan, M.; Oddone, E. Impact of Coronavirus Disease 2019 Pandemic on Crowding: A Call to Action for Effective Solutions to “Access Block”. West. J. Emerg. Med. 2021, 22, 860–870. [Google Scholar] [CrossRef]
- Ministero Della Salute—Ufficio Legislativo “Camera Dei Deputati—XII Commissione—Indagine Conoscitiva Sulla Situazione della Medicina Dell’emergenza-Urgenza e dei Pronto Soccorso in Italia” 20 Febbraio 2024. Available online: https://documenti.camera.it/Leg19/Resoconti/Commissioni/Stenografici/Pdf/12/Indag/C12_pronto_soccorso/2024/05/21/Leg.19.Stencomm.Data20240521.U1.Com12.Indag.C12_pronto_soccorso.0016.Pdf (accessed on 9 February 2025).
- Federazione delle Associazioni dei Dirigenti Ospedalieri Internisti Indagine FADOI: Ospedali, Anziani Dimessi 7 Giorni Più Tardi. Oltre 2 Giornate Di Degenza Improprie. Available online: https://www.fadoi.org/Press-Room/Ospedali-Anziani-Dimessi-7-Giorni-Piu-Tardi-Oltre-2-Giornate-Di-Degenza-Improprie-Lindagine-Fadoi (accessed on 15 July 2024).
- National Guideline Centre. Bed Occupancy. In Emergency and Acute Medical Care in over 16s: Service Delivery and Organisation; National Institute for Health and Care Excellence: London, UK, 2018; Chapter 39. [Google Scholar]
- Agyeman-Manu, K.; Ghebreyesus, T.A.; Maait, M.; Rafila, A.; Tom, L.; Lima, N.T.; Wangmo, D. Prioritising the Health and Care Workforce Shortage: Protect, Invest, Together. Lancet Glob. Health 2023, 11, e1162–e1164. [Google Scholar] [CrossRef]

| 2019 | 2020 | 2021 | 2022 | 2023 | p-Value † | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total ED visits | 3,514,426 | 2,380,005 | 2,861,473 | 3,294,468 | 3,464,756 | ||||||
| Patient age (year) | |||||||||||
| <15 | 594,592 | 16.92% | 299,904 | 12.60% | 398,977 | 13.94% | 528,408 | 16.04% | 559,608 | 16.15% | <0.01 |
| 15–64 | 1,950,945 | 55.51% | 1,359,697 | 57.13% | 1,648,242 | 57.60% | 1,844,961 | 56.00% | 1,935,642 | 55.87% | <0.01 |
| 65–80 | 590,415 | 16.80% | 434,288 | 18.25% | 485,208 | 16.96% | 536,531 | 16.29% | 566,787 | 16.36% | <0.01 |
| > 80 | 377,519 | 10.74% | 285,396 | 11.99% | 328,128 | 11.47% | 383,185 | 11.63% | 398,179 | 11.49% | <0.01 |
| NA | 955 | 0.03% | 720 | 0.03% | 918 | 0.03% | 1383 | 0.04% | 4540 | 0.13% | <0.01 |
| Sex | |||||||||||
| Female | 1,779,067 | 50.62% | 1,184,902 | 49.79% | 1,429,372 | 49.95% | 1,631,294 | 49.52% | 1,715,285 | 49.51% | <0.01 |
| Male | 1,734,917 | 49.37% | 1,194,770 | 50.20% | 1,431,690 | 50.03% | 1,662,705 | 50.47% | 1,749,046 | 50.48% | <0.01 |
| NA | 442 | 0.01% | 333 | 0.01% | 411 | 0.01% | 469 | 0.01% | 425 | 0.01% | 0.71 |
| Triage Scale | |||||||||||
| White | 348,156 | 9.91% | 205,605 | 8.64% | 239,210 | 8.36% | 268,243 | 8.14% | 310,209 | 8.95% | <0.01 |
| Green | 2,413,238 | 68.67% | 1,572,775 | 66.08% | 1,930,559 | 67.47% | 2,264,322 | 68.73% | 2,484,137 | 71.70% | <0.01 |
| Yellow | 667,713 | 19.00% | 512,502 | 21.53% | 590,752 | 20.65% | 659,367 | 20.01% | 598,032 | 17.26% | <0.01 |
| Red | 65,927 | 1.88% | 65,092 | 2.73% | 67,046 | 2.34% | 73,177 | 2.22% | 61,253 | 1.77% | <0.01 |
| Black | 275 | 0.01% | 295 | 0.01% | 257 | 0.01% | 236 | 0.01% | 105 | 0.00% | <0.01 |
| NA | 19,117 | 0.54% | 23,736 | 1.00% | 33,649 | 1.18% | 29,123 | 0.88% | 11,020 | 0.32% | <0.01 |
| Disposition | |||||||||||
| Admitted | 418,427 | 11.91% | 384,278 | 16.15% | 391,207 | 13.67% | 406,202 | 12.33% | 393,139 | 11.35% | <0.01 |
| Discharge | 2,869,009 | 81.64% | 1,846,172 | 77.57% | 2,274,918 | 79.50% | 2,640,042 | 80.14% | 2,716,720 | 78.41% | <0.01 |
| ED Death | 5715 | 0.16% | 8773 | 0.37% | 7695 | 0.27% | 8428 | 0.26% | 7309 | 0.21% | <0.01 |
| LBTC | 175,238 | 4.99% | 94,955 | 3.99% | 134,409 | 4.70% | 183,783 | 5.58% | 234,476 | 6.77% | <0.01 |
| Refuse Hospitalization | 20,913 | 0.60% | 15,940 | 0.67% | 18,982 | 0.66% | 21,293 | 0.65% | 21,466 | 0.62% | <0.01 |
| Transfer | 25,124 | 0.71% | 29,887 | 1.26% | 34,262 | 1.20% | 34,720 | 1.05% | 27,751 | 0.80% | <0.01 |
| Arrival by emergency vehicle | 746,020 | 21.23% | 661,520 | 27.79% | 731,018 | 25.55% | 820,734 | 24.91% | 825,014 | 23.81% | <0.01 |
| 2019 | 2020 | 2021 | 2022 | 2023 | p-Value † | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total ED visits | 3,514,426 | 2,380,005 | 2,861,473 | 3,294,468 | 3,464,756 | ||||||
| Crowding Measures | |||||||||||
| LBTC (%) | 175,238 | (5.0%) | 94,955 | (4.0%) | 134,409 | (4.7%) | 183,783 | (5.6%) | 234,476 | (6.8%) | <0.01 |
| Median EDLOS of admitted patients in hours [IQR] | 3.8 | [1.6–8.6] | 5.5 | [2.1–16.3] | 5.8 | [2.4–16.6] | 5.5 | [2.3–17.5] | 5.2 | [2.1–17.4] | <0.01 |
| Median EDLOS of discharged patients in hours [IQR] | 2.4 | [1.3–4.4] | 2.4 | [1.2–4.5] | 2.5 | [1.3- 4.7] | 2.7 | [1.4–4.9] | 2.7 | [1.4–4.9] | <0.01 |
| N° of admitted patients with an EDLOS greater than 8 h (%) | 110,411 | (26.4%) | 147,049 | (38.3%) | 152,769 | (39.1%) | 157,278 | (38.7%) | 147,189 | (37.4%) | <0.01 |
| N° of discharged patients with an EDLOS greater than 8 h (%) | 252,404 | (8.8%) | 189,943 | (10.3%) | 239,929 | (10.5%) | 301,454 | (11.4%) | 304,565 | (11.2%) | <0.01 |
| Median door-to-clinician time in minutes [IQR] | 35 | [12–94] | 27 | [10–73] | 30 | [11–81] | 36 | [12–96] | 35 | [11–97] | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De la Rosa, M.J.; Duca, A.; Querci, L.; Cortellaro, F.; Calderaro, M.; Pausilli, P.; Bodina, A.; Albonico, A.; Perotti, G.; Signorelli, C.; et al. Does Calm Always Follow the Storm? A Comprehensive Temporal Analysis of Emergency Department Visits in Northern Italy Before and After the COVID-19 Pandemic. Epidemiologia 2025, 6, 10. https://doi.org/10.3390/epidemiologia6010010
De la Rosa MJ, Duca A, Querci L, Cortellaro F, Calderaro M, Pausilli P, Bodina A, Albonico A, Perotti G, Signorelli C, et al. Does Calm Always Follow the Storm? A Comprehensive Temporal Analysis of Emergency Department Visits in Northern Italy Before and After the COVID-19 Pandemic. Epidemiologia. 2025; 6(1):10. https://doi.org/10.3390/epidemiologia6010010
Chicago/Turabian StyleDe la Rosa, Maria José, Andrea Duca, Lorenzo Querci, Francesca Cortellaro, Martina Calderaro, Paolo Pausilli, Annalisa Bodina, Andrea Albonico, Gabriele Perotti, Carlo Signorelli, and et al. 2025. "Does Calm Always Follow the Storm? A Comprehensive Temporal Analysis of Emergency Department Visits in Northern Italy Before and After the COVID-19 Pandemic" Epidemiologia 6, no. 1: 10. https://doi.org/10.3390/epidemiologia6010010
APA StyleDe la Rosa, M. J., Duca, A., Querci, L., Cortellaro, F., Calderaro, M., Pausilli, P., Bodina, A., Albonico, A., Perotti, G., Signorelli, C., & Lombardo, M. (2025). Does Calm Always Follow the Storm? A Comprehensive Temporal Analysis of Emergency Department Visits in Northern Italy Before and After the COVID-19 Pandemic. Epidemiologia, 6(1), 10. https://doi.org/10.3390/epidemiologia6010010






