How the COVID-19 Pandemic Alters the Landscapes of the HIV and Tuberculosis Epidemics in South Africa: A Case Study and Future Directions
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Case Presentation
3.1.1. Demographic, Economic, Geographic, and Political Characteristics of the Country
3.1.2. Overview of South Africa’s Healthcare System
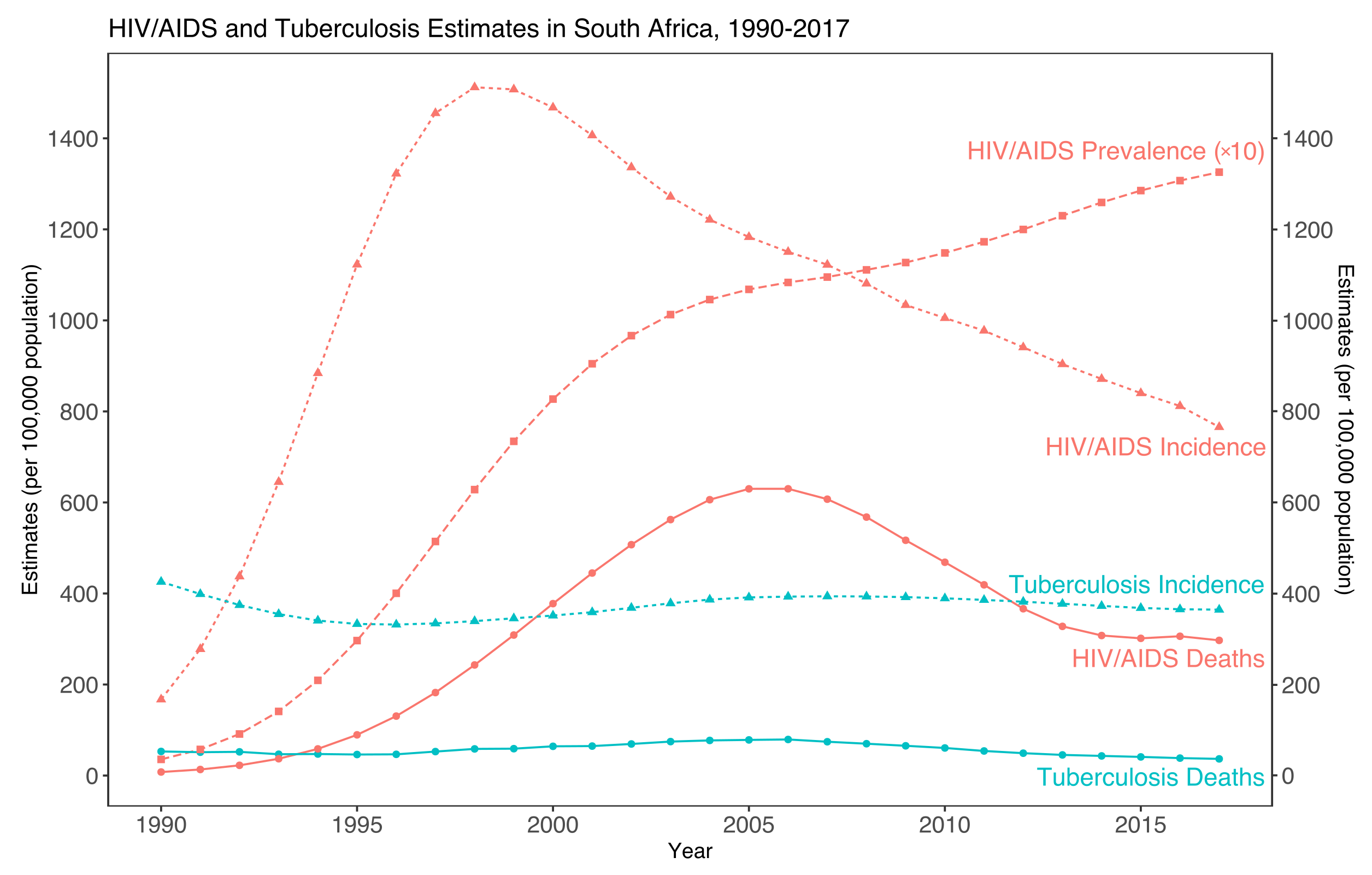
3.1.3. Historical Context of HIV and Tuberculosis in South Africa
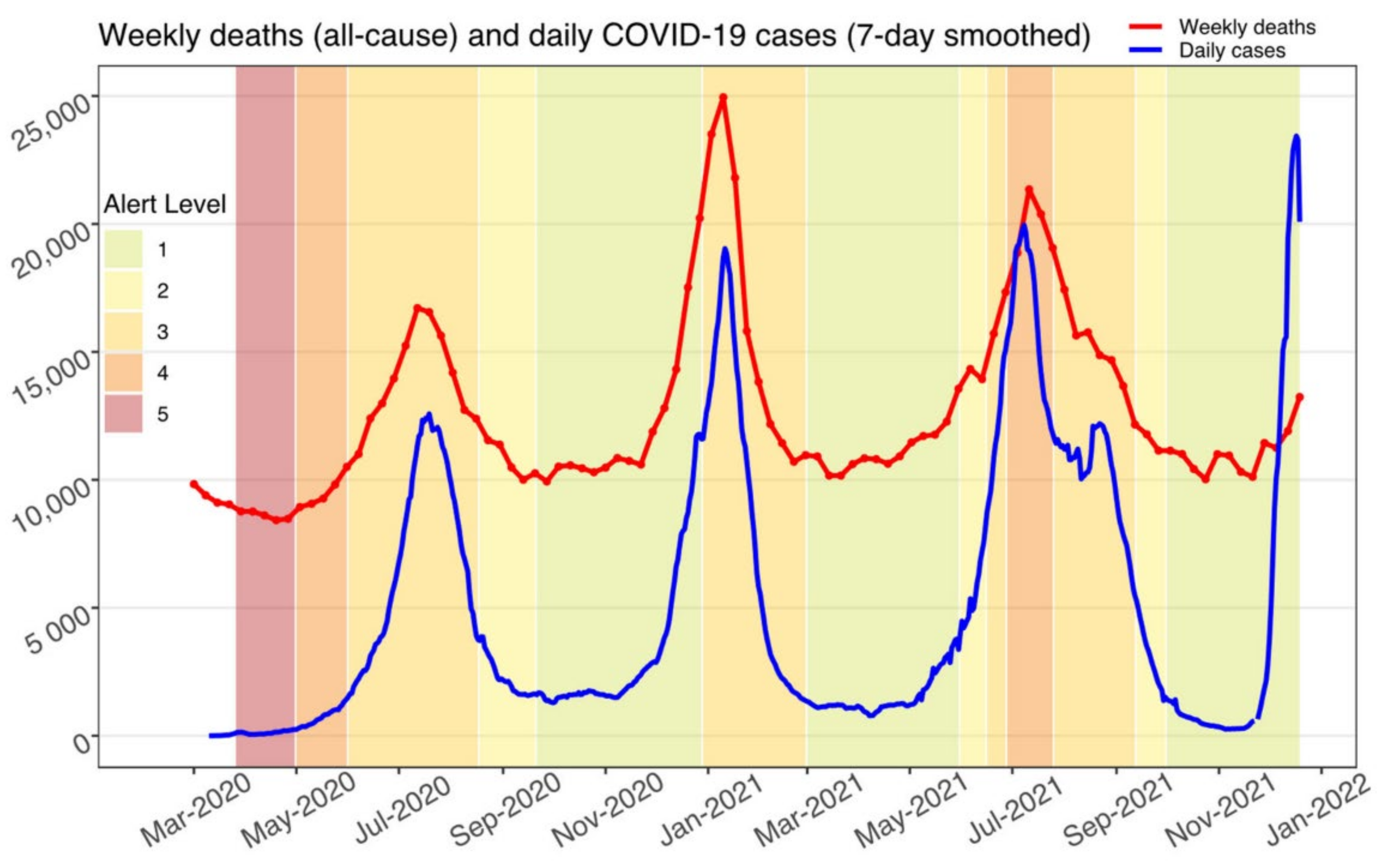
3.1.4. Impact of COVID-19 on Country Level
3.2. Current Impact and Long-Term Influence of the COVID-19 Pandemic on Global and Public Health, Public Policy, and Healthcare Systems
3.2.1. The Indirect Consequences of the COVID-19 Measures
3.2.2. Limited Access to Healthcare Resources
3.2.3. Predicted Risks for Immunocompromised and Coinfected Patients
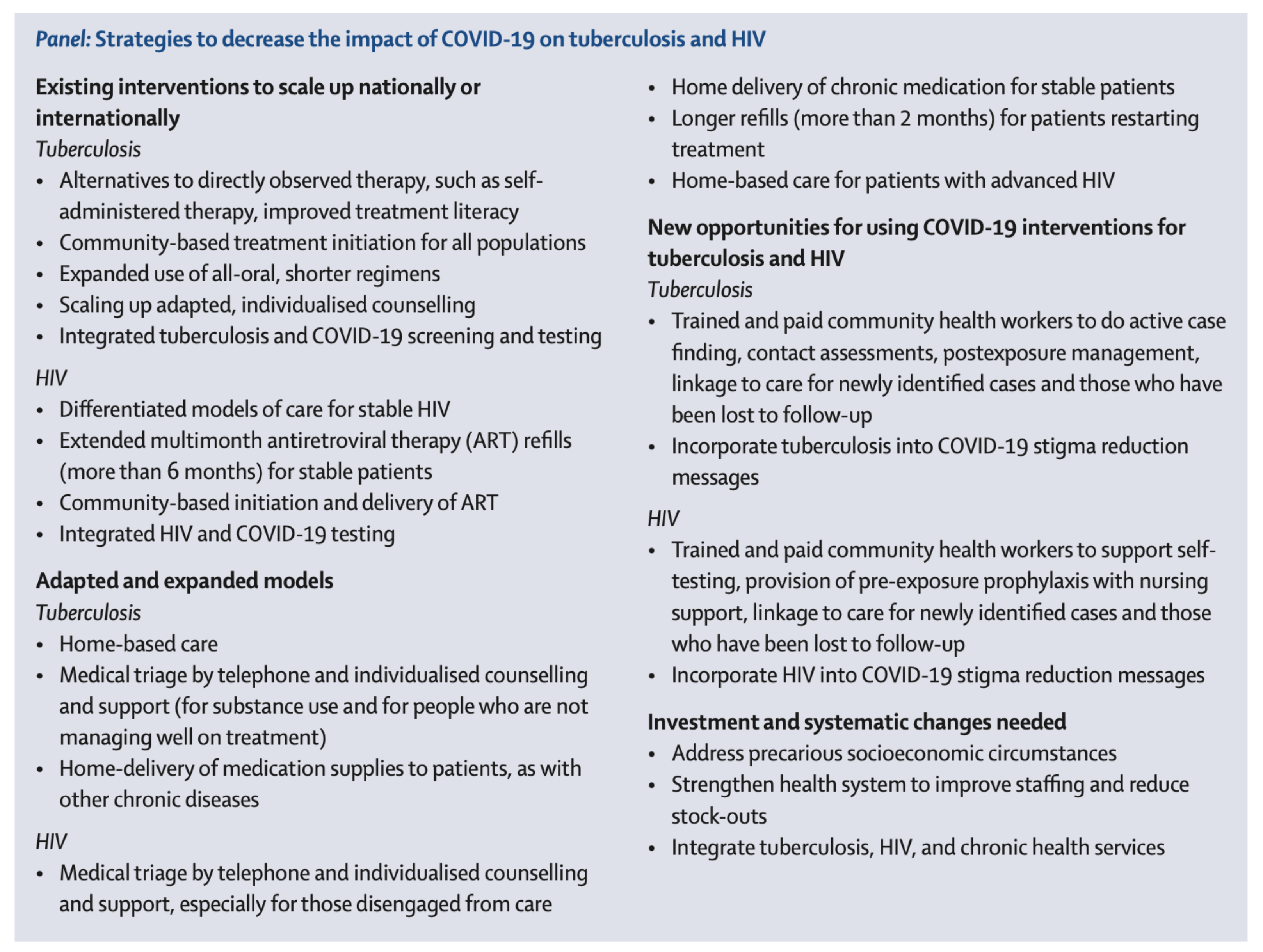
3.2.4. Potential Positive Outcomes of the COVID-19 Pandemic on the Fight against HIV and TB
4. Discussion
4.1. Insights from Reviews
4.2. Limitations
4.3. Discovery of the SARS-CoV-2 B.1.1.529 Variant (Omicron)
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stiegler, N.; Bouchard, J.-P. South Africa: Challenges and Successes of the COVID-19 Lockdown. Ann. Méd. Psychol. Rev. Psychiatr. 2020, 178, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Arndt, C.; Davies, R.; Gabriel, S.; Harris, L.; Makrelov, K.; Robinson, S.; Levy, S.; Simbanegavi, W.; van Seventer, D.; Anderson, L. Covid-19 Lockdowns, Income Distribution, and Food Security: An Analysis for South Africa. Glob. Food Secur. 2020, 26, 100410. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Rego, S.; Rajal, J.B.; Bond, V.; Fatima, R.K.; Isani, A.K.; Sutherland, J.; Kranzer, K. Mitigating the Impact of COVID-19 on Tuberculosis and HIV Services: A Cross-Sectional Survey of 669 Health Professionals in 64 Low and Middle-Income Countries. PLoS ONE 2021, 16, e0244936. [Google Scholar] [CrossRef]
- Bulled, N.; Singer, M. In the Shadow of HIV & TB: A Commentary on the COVID Epidemic in South Africa. Glob. Public Health 2020, 15, 1231–1243. [Google Scholar] [CrossRef]
- Simelela, N.; Venter, W.D.F.; Pillay, Y.; Barron, P. A Political and Social History of HIV in South Africa. Curr. HIV/AIDS Rep. 2015, 12, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Rossouw, T.M.; Boswell, M.T.; Nienaber, A.G.; Moodley, K. Comorbidity in Context: Part 1. Medical Considerations around HIV and Tuberculosis during the COVID-19 Pandemic in South Africa. S. Afr. Med. J. 2020, 110, 621–624. [Google Scholar] [PubMed]
- Jewell, B.L.; Mudimu, E.; Stover, J.; ten Brink, D.; Phillips, A.N.; Smith, J.A.; Martin-Hughes, R.; Teng, Y.; Glaubius, R.; Mahiane, S.G.; et al. Potential Effects of Disruption to HIV Programmes in Sub-Saharan Africa Caused by COVID-19: Results from Multiple Mathematical Models. Lancet HIV 2020, 7, e629–e640. [Google Scholar] [CrossRef]
- Lowe, C.C.; Gordon, D.F.; Hall, M.; Bundy, C.J.; Thompson, L.M.; Nel, A.; Cobbing, J.R.D.; Mabin, A.S.; Vigne, R. South Africa. Available online: https://www.britannica.com/place/South-Africa (accessed on 17 November 2021).
- Republic of South Africa About SA. Available online: https://www.gov.za/about-sa (accessed on 8 November 2021).
- Nyashanu, M.; Simbanegavi, P.; Gibson, L. Exploring the Impact of COVID-19 Pandemic Lockdown on Informal Settlements in Tshwane Gauteng Province, South Africa. Glob. Public Health 2020, 15, 1443–1453. [Google Scholar] [CrossRef]
- Department of Human Settlements Remarks by the Miniser of Human Settlements, Mmamoloko Kubayi, Dubai Expo, Virtual. Available online: https://www.gov.za/speeches/remarks-minister-human-settlements-mmamoloko-kubayi-dubai-expo-virtual-3-nov-2021-0000 (accessed on 12 January 2021).
- Clark, N.L.; Worger, W.H. South. Africa: The Rise and Fall of Apartheid, 2nd ed.; Longman: Harlow, UK; New York, NY, USA, 2011; ISBN 978-1-4082-4564-4. [Google Scholar]
- Omotoso, K.O.; Koch, S.F. Assessing Changes in Social Determinants of Health Inequalities in South Africa: A Decomposition Analysis. Int. J. Equity Health 2018, 17, 181. [Google Scholar] [CrossRef]
- Lu, Y.; Treiman, D.J. Migration, Remittances and Educational Stratification among Blacks in Apartheid and Post-Apartheid South Africa. Soc. Forces 2011, 89, 1119–1143. [Google Scholar] [CrossRef] [Green Version]
- The World Bank. The World Bank in South Africa. Overview. Available online: https://www.worldbank.org/en/country/southafrica/overview (accessed on 8 November 2021).
- The World Bank Gini Index (World Bank Estimate)—South Africa. Available online: https://data.worldbank.org/indicator/SI.POV.GINI?locations=ZA (accessed on 20 November 2021).
- Francis, D.; Webster, E. Poverty and Inequality in South Africa: Critical Reflections. Dev. S. Afr. 2019, 36, 788–802. [Google Scholar] [CrossRef]
- Statistics South Africa. Quarterly Labour Force Survey. Quarter 2. 2021. Available online: http://www.statssa.gov.za/publications/P0211/P02112ndQuarter2021.pdf (accessed on 21 November 2021).
- The World Bank. GDP Growth (Annual %)—South Africa. Available online: https://data.worldbank.org/indicator/NY.GDP.MKTP.KD.ZG?locations=ZA (accessed on 10 November 2021).
- Coovadia, H.; Jewkes, R.; Barron, P.; Sanders, D.; McIntyre, D. The Health and Health System of South Africa: Historical Roots of Current Public Health Challenges. Lancet 2009, 374, 817–834. [Google Scholar] [CrossRef]
- Constitution of the Republic of South Africa. 1996. Available online: https://linkinghub.elsevier.com/retrieve/pii/S014067360960951X (accessed on 11 November 2021).
- Van Rensburg, H.C. South Africa’s Protracted Struggle for Equal Distribution and Equitable Access—Still Not There. Hum. Resour. Health 2014, 12, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Statistics South Africa General Household Survey 2019. 2020. Available online: http://www.statssa.gov.za/publications/P0318/P03182019.pdf (accessed on 10 November 2021).
- Rispel, L.C.; Blaauw, D.; Ditlopo, P.; White, J. Human resources for health and universal health coverage: Progress, Complexities and contestations. In South African Health Review 2018; Health Systems Trust: Durban, South Africa, 2018. [Google Scholar]
- Van Ryneveld, M.; Schneider, H.; Lehmann, U. Looking Back to Look Forward: A Review of Human Resources for Health Governance in South Africa from 1994 to 2018. Hum. Resour. Health 2020, 18, 92. [Google Scholar] [CrossRef]
- Burger, R.; Christian, C. Access to Health Care in Post-Apartheid South Africa: Availability, Affordability, Acceptability. Health Econ. Policy Law 2020, 15, 43–55. [Google Scholar] [CrossRef] [Green Version]
- Karim, Q.A.; Karim, S.S.A. The Evolving HIV Epidemic in South Africa. Int. J. Epidemiol. 2002, 31, 37–40. [Google Scholar] [CrossRef] [Green Version]
- Burton, R.; Giddy, J.; Stinson, K. Prevention of Mother-to-Child Transmission in South Africa: An Ever-Changing Landscape. Obstet. Med. 2015, 8, 5–12. [Google Scholar] [CrossRef]
- ‘T Hoen, E.; Berger, J.; Calmy, A.; Moon, S. Driving a Decade of Change: HIV/AIDS, Patents and Access to Medicines for All. J. Int. AIDS Soc. 2011, 14, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karim, S.S.A.; Churchyard, G.J.; Karim, Q.A.; Lawn, S.D. HIV Infection and Tuberculosis in South Africa: An Urgent Need to Escalate the Public Health Response. Lancet 2009, 374, 921–933. [Google Scholar] [CrossRef] [Green Version]
- Global Burden of Disease Collaborative Network Global Burden of Disease Study 2019 (GBD 2019) Results; Institute for Health Metrics and Evaluation (IHME): Seattle, WA, USA, 2020.
- UN AIDS. I Keypopulation Atlas SOUTH AFRICA. Available online: https://kpatlas.unaids.org/dashboard (accessed on 18 November 2021).
- Statista, Inc. Available online: https://www.statista.com/statistics/1127548/main-causes-of-death-in-south-africa/ (accessed on 18 November 2021).
- SANAC. The National Strategic Plan. Available online: https://sanac.org.za/the-national-strategic-plan/ (accessed on 19 November 2021).
- Cox, H.; Dickson-Hall, L.; Jassat, W.; Moshabela, M.; Kielmann, K.; Grant, A.; Nicol, M.; Black, J.; Mlisana, K.; Vanleeuw, L. Drug-Resistant Tuberculosis in South Africa: History, Progress and Opportunities for Achieving Universal Access to Diagnosis and Effective Treatment. S. Afr. Health Rev. 2017, 2017, 157–167. [Google Scholar]
- Skinner, D.; Mfecane, S. Stigma, Discrimination and the Implications for People Living with HIV/AIDS in South Africa. SAHARA J. Soc. Asp. HIV/AIDS 2004, 1, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Avert. Avert Global Information and Education on HIV and AIDS. Available online: https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/south-africa (accessed on 16 November 2021).
- Coetzee, J.; Jewkes, R.; Gray, G.E. Cross-Sectional Study of Female Sex Workers in Soweto, South Africa: Factors Associated with HIV Infection. PLoS ONE 2017, 12, e0184775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canetti, D.; Riccardi, N.; Martini, M.; Villa, S.; Di Biagio, A.; Codecasa, L.; Castagna, A.; Barberis, I.; Gazzaniga, V.; Besozzi, G. HIV and Tuberculosis: The Paradox of Dual Illnesses and the Challenges of Their Fighting in the History. Tuberculosis 2020, 122, 101921. [Google Scholar] [CrossRef] [PubMed]
- Daftary, A. HIV and Tuberculosis: The Construction and Management of Double Stigma. Soc. Sci. Med. 2012, 74, 1512–1519. [Google Scholar] [CrossRef]
- Dovel, K.; Yeatman, S.; Watkins, S.; Poulin, M. Men’s Heightened Risk of AIDS-Related Death: The Legacy of Gendered HIV Testing and Treatment Strategies. AIDS 2015, 29, 1123–1125. [Google Scholar] [CrossRef]
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 24 November 2021).
- South Africa: Coronavirus Pandemic Country Profile. Available online: https://ourworldindata.org/coronavirus/country/south-africa (accessed on 24 November 2021).
- Mbow, M.; Lell, B.; Jochems, S.P.; Cisse, B.; Mboup, S.; Dewals, B.G.; Jaye, A.; Dieye, A.; Yazdanbakhsh, M. COVID-19 in Africa: Dampening the Storm? Science 2020, 369, 624–626. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, C.; Walker, P.G.T.; Alhaffar, M.; Hamlet, A.; Djaafara, B.A.; Ghani, A.; Ferguson, N.; Dahab, M.; Checchi, F.; Watson, O.J. Under-Reporting of Deaths Limits Our Understanding of True Burden of Covid-19. BMJ 2021, 375, n2239. [Google Scholar] [CrossRef] [PubMed]
- Minister Zweli Mkhize Reports First Case of Coronavirus Covid-19. Available online: https://www.gov.za/speeches/health-reports-first-case-covid-19-coronavirus-5-mar-2020-0000 (accessed on 24 November 2021).
- South African Government About Alert System. Available online: https://www.gov.za/covid-19/about/about-alert-system (accessed on 8 December 2021).
- Kotze, J.; Bohler-Muller, N.; Roberts, B.; Pienaar, G.; Derek Davids, Y.; Mchunu, N. South Africa’s Thuma Mina Moment: Public Opinion and Political Trust in South Africa’s COVID-19 Response. 2021. Available online: https://repository.hsrc.ac.za/bitstream/handle/20.500.11910/16281/12077.pdf?sequence=1&isAllowed=y (accessed on 20 November 2021).
- Dong, E.; Du, H.; Gardner, L. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Our World in Data team Our World in Data COVID-19 Dataset. 2021. Available online: https://covid.ourworldindata.org/ (accessed on 5 December 2021).
- South African Medical Research Council Report on Weekly Deaths in South Africa. Available online: https://www.samrc.ac.za/reports/report-weekly-deaths-south-africa (accessed on 8 December 2021).
- Bhattacharya, S.; Tanisha, T. Social Strife of South Africa in 2021 Fueled by Economic Issue than Political Instability. Int. J. Res. Eng. Sci. Manag. 2021, 4, 38–40. [Google Scholar]
- South Africa. Available online: https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/south-africa/ (accessed on 25 November 2021).
- COVID-19 Coronavirus Vaccine Strategy. Available online: https://www.gov.za/covid-19/vaccine/strategy (accessed on 14 November 2021).
- Mueller, B.; Robbins, R.; Lynsey, C. AstraZeneca’s Vaccine Does Not Work Well Against Virus Variant in South Africa. The New York Times, 7 February 2021. [Google Scholar]
- Hussey, H.; Zinyakatira, N.; Morden, E.; Ismail, M.; Paleker, M.; Bam, J.L.; London, L.; Boulle, A.; Davies, M.A. Higher COVID-19 Mortality in Low-Income Communities in the City of Cape Town—A Descriptive Ecological Study. Gates Open Res. 2021, 5, 1–12. [Google Scholar] [CrossRef]
- Nwosu, C.O.; Oyenubi, A. Income-Related Health Inequalities Associated with the Coronavirus Pandemic in South Africa: A Decomposition Analysis. Int. J. Equity Health 2021, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Garba, N.W.F. Covid-19, the Working Class and the Poor in South Africa. Available online: https://africanarguments.org/2020/06/covid-19-the-working-class-and-the-poor-in-south-africa/ (accessed on 11 November 2021).
- Nduna, M.; Tshona, S.O. Domesticated Poly-Violence Against Women During the 2020 Covid-19 Lockdown in South Africa. Psychol. Stud. 2021, 66, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Dunkle, K.L.; Jewkes, R.K.; Brown, H.C.; Gray, G.E.; McIntryre, J.A.; Harlow, S.D. Gender-Based Violence, Relationship Power, and Risk of HIV Infection in Women Attending Antenatal Clinics in South Africa. Lancet 2004, 363, 1415–1421. [Google Scholar] [CrossRef]
- Men, Women and Children—Findings of the Living Conditions Survey, 2014/15; Statistics South Africa (Stats SA): South Africa, 2018; Available online: https://www.statssa.gov.za/publications/Report-03-10-02%20/Report-03-10-02%202015.pdf (accessed on 17 November 2021).
- Fengler, W.; Nelly, M.-F.; Gill, I.; Baduel, B.; Cuevas, F. South Africa after COVID-19—Light at the End of a Very Long Tunnel. Available online: https://www.brookings.edu/blog/future-development/2021/07/13/south-africa-after-covid-19-light-at-the-end-of-a-very-long-tunnel/ (accessed on 17 November 2021).
- Sikkema, K.J.; Watt, M.H.; Meade, C.S.; Ranby, K.W.; Kalichman, S.C.; Skinner, D.; Pieterse, D. Mental Health and HIV Sexual Risk Behavior Among Patrons of Alcohol Serving Venues in Cape Town, South Africa. JAIDS J. Acquir. Immune Defic. Syndr. 2011, 57, 230–237. [Google Scholar] [CrossRef] [Green Version]
- Latkin, C.A.; German, D.; Vlahov, D.; Galea, S. Neighborhoods and HIV: A Social Ecological Approach to Prevention and Care. Am. Psychol. 2013, 68, 210–224. [Google Scholar] [CrossRef] [Green Version]
- Schur, C.L.; Berk, M.L.; Dunbar, J.R.; Shapiro, M.E.; Cohn, S.E.; Bozzette, S.A. Where to Seek Care: An Examination of People in Rural Areas With HIV/AIDS. J. Rural Health 2002, 18, 337–347. [Google Scholar] [CrossRef]
- StopTB Partnership The Potential Impact of the COVID-19 Response on Tuberculosis in High-Burden Countries: A Modelling Analysis. Available online: https://stoptb.org/assets/documents/news/Modeling%20Report_1%20May%202020_FINAL.pdf (accessed on 19 November 2021).
- Alene, K.A.; Wangdi, K.; Clements, A.C.A. Impact of the COVID-19 Pandemic on Tuberculosis Control: An Overview. Trop. Med. Infect. Dis. 2020, 5, 123. [Google Scholar] [CrossRef] [PubMed]
- Moyo, S.; Boffa, J.; Mhlaba, T.; Sulis, G.; Sifumba, Z.; Pai, M.; Daftary, A. COVID-19 and Tuberculosis in South Africa: A Dangerous Combination. S. Afr. Med. J. 2020, 110, 341–342. [Google Scholar]
- Glaziou, P. Predicted Impact of the COVID-19 Pandemic on Global Tuberculosis Deaths in 2020. medRxiv 2020. [Google Scholar] [CrossRef]
- Hogan, A.B.; Jewell, B.L.; Sherrard-Smith, E.; Vesga, J.F.; Watson, O.J.; Whittaker, C.; Hamlet, A.; Smith, J.A.; Winskill, P.; Verity, R.; et al. Potential Impact of the COVID-19 Pandemic on HIV, Tuberculosis, and Malaria in Low-Income and Middle-Income Countries: A Modelling Study. Lancet Glob. Health 2020, 8, e1132–e1141. [Google Scholar] [CrossRef]
- National Department of Health, South Africa COVID-19 South African Coronavirus News and Information Portal. Available online: https://sacoronavirus.co.za/ (accessed on 17 November 2021).
- The Global Fund. The Impact of COVID-19 on HIV, TB and Malaria Services and Systems for Health: A Snapshot From 502 Health Facilities Across Africa and Asia; The Global Fund: Geneva, Switzerland, 2021; p. 18. [Google Scholar]
- South African National AIDS Council. Midterm Review of The National Strategic Plan for HIV, TB and STIs 2017–2022; South African National Aids Council: Pretoria, South Africa, 2019; p. 127. [Google Scholar]
- Gonzalez, L.L. SPOTLIGHT: New South African Plan for HIV/TB Delayed Because of Covid-19. Available online: https://www.dailymaverick.co.za/article/2021-05-13-new-south-african-plan-for-hiv-tb-delayed-because-of-covid-19/ (accessed on 21 November 2021).
- Gopalan, P.D.; De Vasconcellos, K. Factors Influencing Decisions to Admit or Refuse Patients Entry to a South African Tertiary Intensive Care Unit. S. Afr. Med. J. 2019, 109, 645. [Google Scholar] [CrossRef] [Green Version]
- Waters, L.J.; Pozniak, A.L. COVID-19 Death in People with HIV: Interpret Cautiously. Lancet HIV 2021, 8, e2–e3. [Google Scholar] [CrossRef]
- World Health Organization. Clinical Features and Prognostic Factors of COVID-19 in People Living with HIV Hospitalized with Suspected or Confirmed SARS-CoV-2 Infection; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Geretti, A.M.; Stockdale, A.J.; Kelly, S.H.; Cevik, M.; Collins, S.; Waters, L.; Villa, G.; Docherty, A.; Harrison, E.M.; Turtle, L.; et al. Outcomes of Coronavirus Disease 2019 (COVID-19) Related Hospitalization Among People with Human Immunodeficiency Virus (HIV) in the ISARIC World Health Organization (WHO) Clinical Characterization Protocol (UK): A Prospective Observational Study. Clin. Infect. Dis. 2021, 73, e2095–e2106. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Sun, J.; Patel, R.C.; Zhang, J.; Guo, S.; Zheng, Q.; Olex, A.L.; Olatosi, B.; Weissman, S.B.; Islam, J.Y.; et al. Associations between HIV Infection and Clinical Spectrum of COVID-19: A Population Level Analysis Based on US National COVID Cohort Collaborative (N3C) Data. Lancet HIV 2021, 8, e690–e700. [Google Scholar] [CrossRef]
- Ziegler, C.G.K.; Allon, S.J.; Nyquist, S.K.; Mbano, I.M.; Miao, V.N.; Tzouanas, C.N.; Cao, Y.; Yousif, A.S.; Bals, J.; Hauser, B.M.; et al. SARS-CoV-2 Receptor ACE2 Is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets across Tissues. Cell 2020, 181, 1016–1035.e19. [Google Scholar] [CrossRef] [PubMed]
- Keene, C.; Mohr-Holland, E.; Cassidy, T.; Scott, V.; Nelson, A.; Furin, J.; Triviño-Duran, L. How COVID-19 Could Benefit Tuberculosis and HIV Services in South Africa. Lancet Respir. Med. 2020, 8, 844–846. [Google Scholar] [CrossRef]
- Nachega, J.B.; Atteh, R.; Ihekweazu, C.; Sam-Agudu, N.A.; Adejumo, P.; Nsanzimana, S.; Rwagasore, E.; Condo, J.; Paleker, M.; Mahomed, H.; et al. Contact Tracing and the COVID-19 Response in Africa: Best Practices, Key Challenges, and Lessons Learned from Nigeria, Rwanda, South Africa, and Uganda. Am. J. Trop. Med. Hyg. 2021, 104, 1179–1187. [Google Scholar] [CrossRef]
- Roberts, T.; Sahu, S.; Malar, J.; Abdullaev, T.; Vandevelde, W.; Pillay, Y.G.; Fujiwara, P.I.; Reid, A.; Hader, S.; Singh, S.; et al. Turning Threats into Opportunities: How to Implement and Advance Quality TB Services for People with HIV during the COVID-19 Pandemic and Beyond. J. Intern. AIDS Soc. 2021, 24, e25696. [Google Scholar] [CrossRef]
- Dorward, J.; Khubone, T.; Gate, K.; Ngobese, H.; Sookrajh, Y.; Mkhize, S.; Jeewa, A.; Bottomley, C.; Lewis, L.; Baisley, K.; et al. The Impact of the COVID-19 Lockdown on HIV Care in 65 South African Primary Care Clinics: An Interrupted Time Series Analysis. Lancet HIV 2021, 8, e158–e165. [Google Scholar] [CrossRef]
- Loveday, M.; Cox, H.; Evans, D.; Furin, J.; Ndjeka, N.; Osman, M.; Naidoo, K. Opportunities from a New Disease for an Old Threat: Extending COVID-19 Efforts to Address Tuberculosis in South Africa. S. Afr. Med. J. 2020, 110, 1160. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Rentsch, C.T.; MacKenna, B.; Schultze, A.; Mehrkar, A.; Bates, C.J.; Eggo, R.M.; Morton, C.E.; Bacon, S.C.J.; Inglesby, P.; et al. HIV Infection and COVID-19 Death: A Population-Based Cohort Analysis of UK Primary Care Data and Linked National Death Registrations within the OpenSAFELY Platform. Lancet HIV 2021, 8, e24–e32. [Google Scholar] [CrossRef]
- Naidoo, P. South Africa’s Unemployment Rate Is Now Highest in the World. Available online: https://www.aljazeera.com/economy/2021/8/24/south-africas-unemployment-rate-is-now-the-worlds-highest (accessed on 21 November 2021).
- National Department of Health. South Africa Annual Performance Plan 2021–2022. 2021. Available online: https://www.health.gov.za/annual-performance-plan/ (accessed on 10 November 2021).
- De Villiers, K. Bridging the Health Inequality Gap: An Examination of South Africa’s Social Innovation in Health Landscape. Infect. Dis. Poverty 2021, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Update on Omicron. Available online: https://www.who.int/news/item/28-11-2021-update-on-omicron (accessed on 1 December 2021).
- Africa CDC. Africa Centres for Disease Control and Prevention’s Statement Regarding the New SARS-CoV-2 Virus Variant B.1.1.529. Available online: https://africacdc.org/news-item/africa-centres-for-disease-control-and-preventions-statement-regarding-the-new-sars-cov-2-virus-variant-b-1-1-529/ (accessed on 29 November 2021).
- World Health Organization. Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. Available online: https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern (accessed on 29 November 2021).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 31 May 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eike, D.; Hogrebe, M.; Kifle, D.; Tregilgas, M.; Uppal, A.; Calmy, A. How the COVID-19 Pandemic Alters the Landscapes of the HIV and Tuberculosis Epidemics in South Africa: A Case Study and Future Directions. Epidemiologia 2022, 3, 297-313. https://doi.org/10.3390/epidemiologia3020023
Eike D, Hogrebe M, Kifle D, Tregilgas M, Uppal A, Calmy A. How the COVID-19 Pandemic Alters the Landscapes of the HIV and Tuberculosis Epidemics in South Africa: A Case Study and Future Directions. Epidemiologia. 2022; 3(2):297-313. https://doi.org/10.3390/epidemiologia3020023
Chicago/Turabian StyleEike, Daniel, Maximilia Hogrebe, Dagem Kifle, Miriam Tregilgas, Anshu Uppal, and Alexandra Calmy. 2022. "How the COVID-19 Pandemic Alters the Landscapes of the HIV and Tuberculosis Epidemics in South Africa: A Case Study and Future Directions" Epidemiologia 3, no. 2: 297-313. https://doi.org/10.3390/epidemiologia3020023
APA StyleEike, D., Hogrebe, M., Kifle, D., Tregilgas, M., Uppal, A., & Calmy, A. (2022). How the COVID-19 Pandemic Alters the Landscapes of the HIV and Tuberculosis Epidemics in South Africa: A Case Study and Future Directions. Epidemiologia, 3(2), 297-313. https://doi.org/10.3390/epidemiologia3020023







