Risk of Secondary Household Transmission of COVID-19 from Health Care Workers in a Hospital in Spain
Abstract
:1. Introduction
2. Materials and Methods
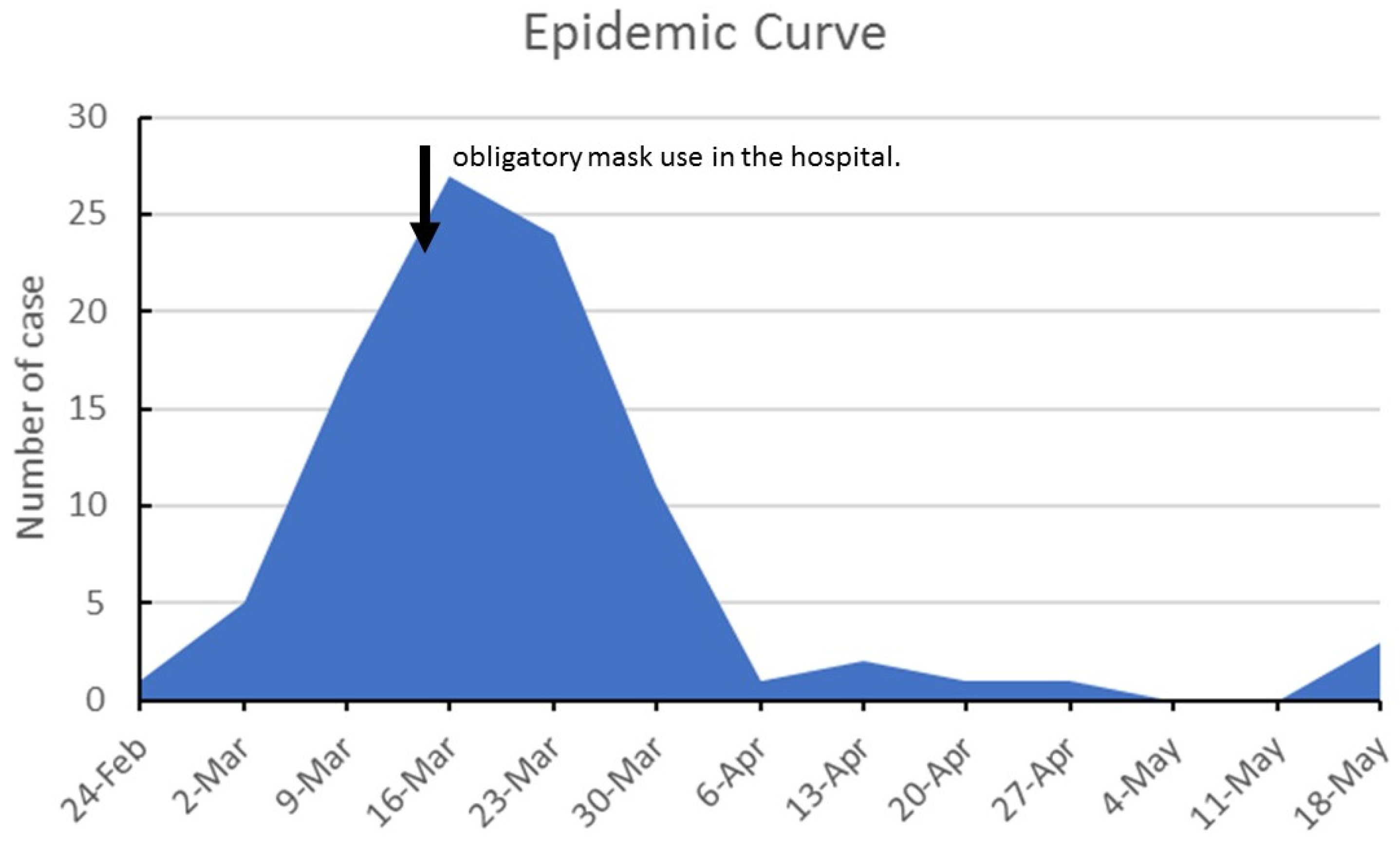
3. Results
3.1. Index Cases Characteristic and Risk of Secondary Transmission
3.2. Household and Risk of Secondary Transmission
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tadj, A.; Lahbib, S.S.M. Our Overall Current Knowledge of COVID 19: An Overview. Microbes Infect. Chemother. 2021, 1, e1262. [Google Scholar] [CrossRef]
- Angulo-Bazán, Y.; Solis-Sánchez, G.; Cardenas, F.; Jorge, A.; Acosta, J.; Cabezas, C. Household transmission of SARS-CoV-2 (COVID-19) in Lima, Peru. Cad. Saude Publica 2021, 37, e00238720. [Google Scholar] [CrossRef]
- Thompson, H.A.; Mousa, A.; Dighe, A.; Fu, H.; Arnedo-Pena, A.; Barrett, P.; Bellido-Blasco, J.; Bi, Q.; Caputi, A.; Chaw, L.; et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Setting-specific Transmission Rates: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2021, 73, e754–e764. [Google Scholar] [CrossRef]
- WHO. Health Workforce Requirements for Universal Health Coverage and the Sustainable Development Goals; WHO: Geneva, Switzerland, 2016; pp. 1–40. [Google Scholar]
- WHO. Health Workers: A Global Profile; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Viego, V.; Geri, M.; Castiglia, J.; Jouglard, E. Incubation period and serial interval of COVID-19 in a chain of infections in Bahia Blanca (Argentina). Cien. Saude Colet. 2020, 25, 3503–3510. [Google Scholar] [CrossRef] [PubMed]
- Kalra, A.; Michos, E.D.; Chinnaiyan, K.M. COVID-19 and the healthcare workers. Eur. Heart J. 2020, 41, 2936–2937. [Google Scholar] [CrossRef]
- McConnell, D. Balancing the duty to treat with the duty to family in the context of the COVID-19 pandemic. J. Med. Ethics 2020, 46, 360–363. [Google Scholar] [CrossRef]
- Wilson, W.; Raj, J.P.; Rao, S.; Ghiya, M.; Nedungalaparambil, N.M.; Mundra, H.; Mathew, R. Prevalence and Predictors of Stress, anxiety, and Depression among Healthcare Workers Managing COVID-19 Pandemic in India: A Nationwide Observational Study. Indian J. Psychol. Med. 2020, 42, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Mohindra, R.; Sharma, K.; Soni, R.K.; Rana, K.; Singh, S.M. The impact of working in a COVID hospital on sexual functioning in male nurses: A study from North India. Ind. Psychiatry J. 2021, 30, 187–190. [Google Scholar] [CrossRef]
- Farahat, S.A.; Amin, O.R.; Hamdy, H.S.; Fouad, M.M. The impact of work-related stress on the cognition domain of executive functioning of health care workers during the COVID-19 pandemic. Int. Arch. Occup. Environ. Health 2021, 1–12. [Google Scholar] [CrossRef]
- Nissan, D.; Weiss, G.; Siman-Tov, M.; Spitz, A.; Bodas, M.; Shenhar, G.; Adini, B. Differences in levels of psychological distress, perceived safety, trust, and efficacy amongst hospital personnel during the COVID-19 pandemic. Res. Nurs. Health 2021, 44, 776–786. [Google Scholar] [CrossRef]
- Lake, E.T.; Narva, A.M.; Holland, S.; Smith, J.G.; Cramer, E.; Rosenbaum, K.E.F.; French, R.; Clark, R.R.S.; Rogowski, J.A. Hospital nurses’ moral distress and mental health during COVID-19. J. Adv. Nurs. 2021. [Google Scholar] [CrossRef]
- Brand, M.W.; Wiskur, B.; Rojas, J.I. Assessing fear of COVID-19 at an academic medical center. J. Emerg. Manag. 2020, 18, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, U.; Fraenkel, C.-J. COVID-19: Risks to Healthcare Workers and Their Families. Available online: https://www.cebm.net/wp-content/uploads/2020/04/Are-interventions-such-as-social-distancing-effective-at-reducing-the-risk-of-asymptomatic-healthcare-workers-transmitting-COVID-final.pdf (accessed on 13 November 2021).
- Shah, A.S.V.; Wood, R.; Gribben, C.; Caldwell, D.; Bishop, J.; Weir, A.; Kennedy, S.; Reid, M.; Smith-Palmer, A.; Goldberg, D.; et al. Risk of hospital admission with coronavirus disease 2019 in healthcare workers and their households: Nationwide linkage cohort study. BMJ 2020, 371, m3582. [Google Scholar] [CrossRef]
- Quental, K.N.; Leite, A.L.; de Oliveira, Z.N.P.; de Sousa Tavares, L.V.; de Sousa Tavares, W.G.; Pinheiro, E.F.; Lacsina, J.R.; DeSouza-Vieira, T.; Silva, J.B.N.F. SARS-CoV-2 co-infection with dengue virus in Brazil: A potential case of viral transmission by a health care provider to household members. Travel Med. Infect. Dis. 2021, 40, 101975. [Google Scholar] [CrossRef]
- Ministerio de Sanidad y Consumo. Estrategia de Detección Precoz, Vigilancia y Control de COVID-19. [Strategy for Early Detection, Surveillance and Control of COVID-19]; Ministerio de Sanidad: Madrid, Spain, 2020.
- Sahu, A.K.; Amrithanand, V.T.; Mathew, R.; Aggarwal, P.; Nayer, J.; Bhoi, S. COVID-19 in health care workers—A systematic review and meta-analysis. Am. J. Emerg. Med. 2020, 38, 1727–1731. [Google Scholar] [CrossRef] [PubMed]
- Stock, A.D.; Bader, E.R.; Cezayirli, P.; Inocencio, J.; Chalmers, S.A.; Yassari, R.; Yanamadala, V.; Eskandar, E. COVID-19 Infection among Healthcare Workers: Serological Findings Supporting Routine Testing. Front. Med. 2020, 7, 471. [Google Scholar] [CrossRef]
- Meylan, S.; Dafni, U.; Lamoth, F.; Tsourti, Z.; Lobritz, M.A.; Regina, J.; Bressin, P.; Senn, L.; Grandbastien, B.; Andre, C.; et al. SARS-CoV-2 seroprevalence in healthcare workers of a Swiss tertiary care centre at the end of the first wave: A cross-sectional study. BMJ Open 2021, 11, e049232. [Google Scholar] [CrossRef]
- He, S.; Hecimovic, A.; Matijasevic, V.; Mai, H.T.; Heslop, L.; Foster, J.; Alexander, K.E.; Pal, N.; Alexandrou, E.; Davidson, P.M.; et al. Prevalence of SARS-CoV-2 antibodies among nurses: A systematic review and meta-analysis. J. Clin. Nurs. 2021. [Google Scholar] [CrossRef] [PubMed]
- Riccò, M.; Gualerzi, G.; Ranzieri, S.; Peruzzi, S.; Valente, M.; Marchesi, F.; Bragazzi, N.L.; Signorelli, C. Occurrence of SARS-CoV-2 infection among healthcare personnel: Results from an early systematic review and meta-analysis. Acta Biomed. 2021, 92, e2021311. [Google Scholar] [CrossRef]
- Madewell, Z.J.; Yang, Y.; Longini, I.M.; Halloran, M.E.; Dean, N.E. Household Transmission of SARS-CoV-2. JAMA Netw. Open 2020, 3, e2031756. [Google Scholar] [CrossRef]
- Huang, P.-Y.; Wu, T.-S.; Cheng, C.-W.; Chen, C.-J.; Huang, C.-G.; Tsao, K.-C.; Lin, C.-S.; Chung, T.-Y.; Lai, C.-C.; Yang, C.-T.; et al. A hospital cluster of COVID-19 associated with a SARS-CoV-2 superspreading event. J. Microbiol. Immunol. Infect. 2021. [Google Scholar] [CrossRef]
- Pérez-Lago, L.; Martínez-Lozano, H.; Pajares-Díaz, J.A.; Díaz-Gómez, A.; Machado, M.; Sola-Campoy, P.J.; Herranz, M.; Valerio, M.; Olmedo, M.; Suárez-González, J.; et al. Overlapping of Independent SARS-CoV-2 Nosocomial Transmissions in a Complex Outbreak. mSphere 2021, 6, e0038921. [Google Scholar] [CrossRef]
- Arnedo-Pena, A.; Sabater-Vidal, S.; Meseguer-Ferrer, N.; Pac-Sa, M.R.; Mañes-Flor, P.; Gascó-Laborda, J.C.; Larrea, R.M.; Tirado-Balaguer, M.D.; Romeu-García, M.Á.; Gil-Fortuño, M.; et al. COVID-19 secondary attack rate and risk factors in household contacts in Castellon (Spain): Preliminary report. Enferm. Emerg. 2020, 19, 64–70. [Google Scholar]
- Méndez-Echevarría, A.; Sainz, T.; de Felipe, B.; Alcolea, S.; Olbrich, P.; Goycochea-Valdivia, W.A.; Escosa-García, L.; Cobo, L.; Calvo, C.; Neth, O. High Rates of SARS-CoV-2 Family Transmission in Children of Healthcare Workers during the First Pandemic Wave in Madrid, Spain: Serologic Study. Pediatr. Infect. Dis. J. 2021, 40, e185–e188. [Google Scholar] [CrossRef] [PubMed]
- Sabetian, G.; Moghadami, M.; Hashemizadeh Fard Haghighi, L.; Shahriarirad, R.; Fallahi, M.J.; Asmarian, N.; Moeini, Y.S. COVID-19 infection among healthcare workers: A cross-sectional study in southwest Iran. Virol. J. 2021, 18, 58. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zhou, Q.; He, Y.; Liu, L.; Ma, X.; Wei, X.; Jiang, N.; Liang, L.; Zheng, Y.; Ma, L.; et al. Nosocomial outbreak of COVID-19 pneumonia in Wuhan, China. Eur. Respir. J. 2020, 55, 2000544. [Google Scholar] [CrossRef] [PubMed]
- Koopsen, J.; Dekker, M.; Thung, P.; Jonges, M.; Vennema, H.; Leenstra, T.; Eggink, D.; Welkers, M.R.A.; Struijs, P.A.A.; Reusken, C.; et al. Rapid reinfection with SARS-CoV-2 variant-of-concern Alpha detected in a nurse during an outbreak at a non-COVID inpatient ward: Lessons learned. Antimicrob. Resist. Infect. Control 2021, 10, 137. [Google Scholar] [CrossRef]
- Abbas, M.; Robalo Nunes, T.; Martischang, R.; Zingg, W.; Iten, A.; Pittet, D.; Harbarth, S. Nosocomial transmission and outbreaks of coronavirus disease 2019: The need to protect both patients and healthcare workers. Antimicrob. Resist. Infect. Control 2021, 10, 7. [Google Scholar] [CrossRef]
- Vimercati, L.; Tafuri, S.; Chironna, M.; Loconsole, D.; Fucilli, F.I.M.; Migliore, G.; Gesualdo, L. The COVID-19 hotel for healthcare workers: An Italian best practice. J. Hosp. Infect. 2020, 105, 387–388. [Google Scholar] [CrossRef]
- Shin, H.; Sharma, A.; Nicolau, J.L.; Kang, J. The impact of hotel CSR for strategic philanthropy on booking behavior and hotel performance during the COVID-19 pandemic. Tour. Manag. 2021, 85, 104322. [Google Scholar] [CrossRef]
- Teng, X.; Teng, Y.-M.; Wu, K.-S.; Chang, B.-G. Corporate Social Responsibility in Public Health during the COVID-19 Pandemic: Quarantine Hotel in China. Front. Public Health 2021, 9, 620930. [Google Scholar] [CrossRef] [PubMed]
- Jordan-Martin, N.C.; Madad, S.; Alves, L.; Wang, J.; O’Gere, L.; Smith, Y.G.; Pressman, M.; Shure, J.A.; Cosmi, M. Isolation Hotels: A Community-Based Intervention to Mitigate the Spread of the COVID-19 Pandemic. Health Secur. 2020, 18, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Chersich, M.F.; Gray, G.; Fairlie, L.; Eichbaum, Q.; Mayhew, S.; Allwood, B.; English, R.; Scorgie, F.; Luchters, S.; Simpson, G.; et al. COVID-19 in Africa: Care and protection for frontline healthcare workers. Glob. Health 2020, 16, 46. [Google Scholar] [CrossRef]
- Gürlek, M.; Kılıç, İ. A true friend becomes apparent on a rainy day: Corporate social responsibility practices of top hotels during the COVID-19 pandemic. Curr. Issues Tour. 2021, 24, 905–918. [Google Scholar] [CrossRef]
- Public Health England. Understanding the Impact of COVID-19 on BAM; PHE: London, UK, 2020.
- Denford, S.; Morton, K.; Horwood, J.; de Garang, R.; Yardley, L. Preventing within household transmission of COVID-19: Is the provision of accommodation to support self-isolation feasible and acceptable? BMC Public Health 2021, 21, 1641. [Google Scholar] [CrossRef] [PubMed]
- Gobierno de España. Ley 14/1986, de 25 de abril, General de Sanidad. Boletín Of. Del Estado 1986, 102, 15207–15224. [Google Scholar]
- Gobierno de España. Ley 16/2003, de 28 de mayo, de cohesión y calidad del Sistema Nacional de Salud. Boletín Of. Del Estado 2003, 128, 20567–20588. [Google Scholar]
- Gobierno de España. Ley 33/2011, de 4 de octubre, General de Salud Pública. Boletín Of. Del Estado 2011, 10240, 104593–104626. [Google Scholar]
- Gobierno de España. Ley 2/2021, de 29 de marzo, de medidas urgentes de prevención, contención y coordinación para hacer frente a la crisis sanitaria ocasionada por el COVID-19. Boletín Of. Del Estado 2020, 76, 35952–35980. [Google Scholar]
- Código de Vigilancia Epidemiológica; Agencia Estatal Boletín Oficial del Estado: Madrid, Spain, 2021. Available online: https://www.boe.es/biblioteca_juridica/codigos/codigo.php?id=352_Codigo_de_Vigilancia_Epidemiologica&modo=2 (accessed on 13 November 2021).
- Consejo Interterritorial del Sistema Nacional de Salud. Plan de Respuesta Temprana en un Escenario de Control de la Pandemia por el COVID-19; Ministerio de Sanidad: Madrid, Spain, 2020.
- COVID-19: Derecho Europeo y Estatal; Agencia Estatal Boletín Oficial del Estado: Madrid, Spain, 2021. Available online: https://boe.es/biblioteca_juridica/codigos/codigo.php?id=355_Crisis_Sanitaria_COVID-19&tipo=C&modo=2 (accessed on 13 November 2021).

| Profession | n | AR | OR | 95% CI |
|---|---|---|---|---|
| Cleaning, laundry, and Kitchen staff | 208 | 0.96% | 1 | |
| Physicians | 475 | 4.00% | 4.29 | 0.99–18.60 |
| Nurses | 657 | 7.15% | 7.94 | 1.91–32.96 |
| Nursing assistant | 298 | 6.04% | 6.62 | 1.52–28.85 |
| Orderlies | 39 | 15.38% | 18.73 | 3.63–96.73 |
| Other professionals | 495 | 1.21% | 1.26 | 0.25–6.31 |
| Variable | Case | No Case | Total | IRR | 95% CI | p |
|---|---|---|---|---|---|---|
| Age | 0.993 | 0.975–1.012 | 0.492 | |||
| Age Group | ||||||
| 18–29 | 19 | 31 | 50 | 1.180 | 0.591–2.353 | 0.638 |
| 30–39 | 23 | 23 | 46 | 2.054 | 1.056–3.990 | 0.034 |
| 40–49 | 29 | 126 | 155 | 1.380 | 0.729–2.613 | 0.321 |
| 50–62 | 14 | 61 | 75 | 1 | ||
| Sex | ||||||
| Female | 10 | 79 | 89 | 1 | ||
| Male | 75 | 162 | 237 | 1.351 | 1.060–1.725 | 0.015 |
| Occupation | ||||||
| other professionals | 2 | 39 | 41 | 1 | - | - |
| Physician | 26 | 89 | 115 | 5.777 | 1.371–24.342 | 0.017 |
| nurse | 36 | 82 | 118 | 3.512 | 0.845–14.586 | 0.084 |
| auxiliary | 15 | 29 | 44 | 3.529 | 0.807–15.433 | 0.094 |
| orderlies | 6 | 2 | 8 | 4.800 | 0.968–23.781 | 0.055 |
| Variable | Case | No Case | Total | IRR | 95% CI | p |
|---|---|---|---|---|---|---|
| n. Household members | ||||||
| 2 | 6 | 13 | 19 | 1 | ||
| 3 | 9 | 27 | 36 | 1.583 | 0.563–4.448 | 0.383 |
| 4 | 21 | 51 | 72 | 2.770 | 1.118–6.865 | 0.028 |
| 5 | 20 | 40 | 60 | 1.965 | 1.696–10.513 | 0.002 |
| >5 | 29 | 110 | 139 | 7.064 | 2.932–17.014 | <0.001 |
| n. Bedrooms | ||||||
| 2 | 8 | 13 | 21 | 1 | ||
| 3 | 32 | 53 | 85 | 2.133 | 0.983–4.629 | 0.055 |
| 4 | 22 | 57 | 79 | 1.760 | 0.783–3.953 | 0.171 |
| >4 | 15 | 113 | 128 | 2.000 | 0.847–4.717 | 0.113 |
| n. Bathrooms | 0.973 | 0.902–1.050 | 0.486 | |||
| n. Persons/Bedroom | ||||||
| <1 | 8 | 13 | 21 | 1 | ||
| 1 | 32 | 53 | 85 | 2.213 | 0.908–5.396 | 0.080 |
| 1–1.499 | 22 | 57 | 79 | 2.125 | 0.825–5.477 | 0.119 |
| ≥1.5 | 15 | 113 | 128 | 5.167 | 2.156–12.383 | <0.001 |
| n. persons/bathroom | ||||||
| >1 | 9 | 62 | 1 | |||
| 1–2 | 44 | 133 | 2.095 | 1.022–4.292 | 0.043 | |
| >2 | 24 | 41 | 1.368 | 1.627–7.529 | 0.001 |
| Variable | Case | No Case | Total | IRR | 95% CI | p |
|---|---|---|---|---|---|---|
| Wearing a mask at home | ||||||
| No | 22 | 42 | 64 | 1 | ||
| Yes | 63 | 199 | 262 | 0.534 | 0.329–0.869 | 0.011 |
| Wearing Gloves | ||||||
| No | 61 | 134 | 195 | 1 | ||
| Yes | 24 | 107 | 131 | 0.607 | 0.362–0.988 | 0.044 |
| Hand washing | ||||||
| No | 26 | 55 | 81 | 1 | - | - |
| Yes | 59 | 186 | 245 | 0.616 | 0.382–1.018 | 0.059 |
| Wash clothes separately | ||||||
| No | 33 | 74 | 107 | 1 | ||
| Yes | 52 | 167 | 219 | 0.650 | 0.413–1.039 | 0.0723 |
| Individual or disposable tableware | ||||||
| No | 29 | 47 | 76 | 1 | - | - |
| Yes | 56 | 194 | 250 | 0.456 | 0.286–0.740 | 0.002 |
| Cleaning surfaces with disinfectant | ||||||
| No | 33 | 59 | 92 | 1 | - | - |
| Yes | 52 | 182 | 234 | 0.487 | 0.315–0.753 | 0.001 |
| Individual Bedroom | ||||||
| No | 19 | 34 | 53 | 1 | - | - |
| Yes | 66 | 207 | 273 | 0.490 | 0.294–0.816 | 0.001 |
| Individual Bathroom | ||||||
| No | 19 | 34 | 53 | 1 | - | - |
| Yes | 66 | 207 | 273 | 0.650 | 0.413–1.039 | 0.0723 |
| Variable | IRR * | 95% CI | p |
|---|---|---|---|
| Wearing a mask at home | 0.540 | 0.311–0.937 | 0.028 |
| Wearing Gloves at home | 0.599 | 0.367–0.977 | 0.040 |
| individual or disposable tableware | 0.517 | 0.313–0.855 | 0.010 |
| Cleaning surfaces with disinfectant | 0.510 | 0.312–0.833 | 0.007 |
| Individual Bedroom | 0.453 | 0.268–0.764 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Remón-Berrade, M.; Guillen-Aguinaga, S.; Sarrate-Adot, I.; Garcia-Garcia, M.P.; Lerga-Berruezo, M.d.C.; Guillen-Aguinaga, L.; Guillen-Grima, F. Risk of Secondary Household Transmission of COVID-19 from Health Care Workers in a Hospital in Spain. Epidemiologia 2022, 3, 1-10. https://doi.org/10.3390/epidemiologia3010001
Remón-Berrade M, Guillen-Aguinaga S, Sarrate-Adot I, Garcia-Garcia MP, Lerga-Berruezo MdC, Guillen-Aguinaga L, Guillen-Grima F. Risk of Secondary Household Transmission of COVID-19 from Health Care Workers in a Hospital in Spain. Epidemiologia. 2022; 3(1):1-10. https://doi.org/10.3390/epidemiologia3010001
Chicago/Turabian StyleRemón-Berrade, Miren, Sara Guillen-Aguinaga, Isabel Sarrate-Adot, Maria Pilar Garcia-Garcia, Maria del Carmen Lerga-Berruezo, Laura Guillen-Aguinaga, and Francisco Guillen-Grima. 2022. "Risk of Secondary Household Transmission of COVID-19 from Health Care Workers in a Hospital in Spain" Epidemiologia 3, no. 1: 1-10. https://doi.org/10.3390/epidemiologia3010001
APA StyleRemón-Berrade, M., Guillen-Aguinaga, S., Sarrate-Adot, I., Garcia-Garcia, M. P., Lerga-Berruezo, M. d. C., Guillen-Aguinaga, L., & Guillen-Grima, F. (2022). Risk of Secondary Household Transmission of COVID-19 from Health Care Workers in a Hospital in Spain. Epidemiologia, 3(1), 1-10. https://doi.org/10.3390/epidemiologia3010001







