Risk Factors for Incisional Hernia After Kidney Transplantation: Impact of Fascial Closure Suture Type
Abstract
1. Introduction
2. Materials and Methods
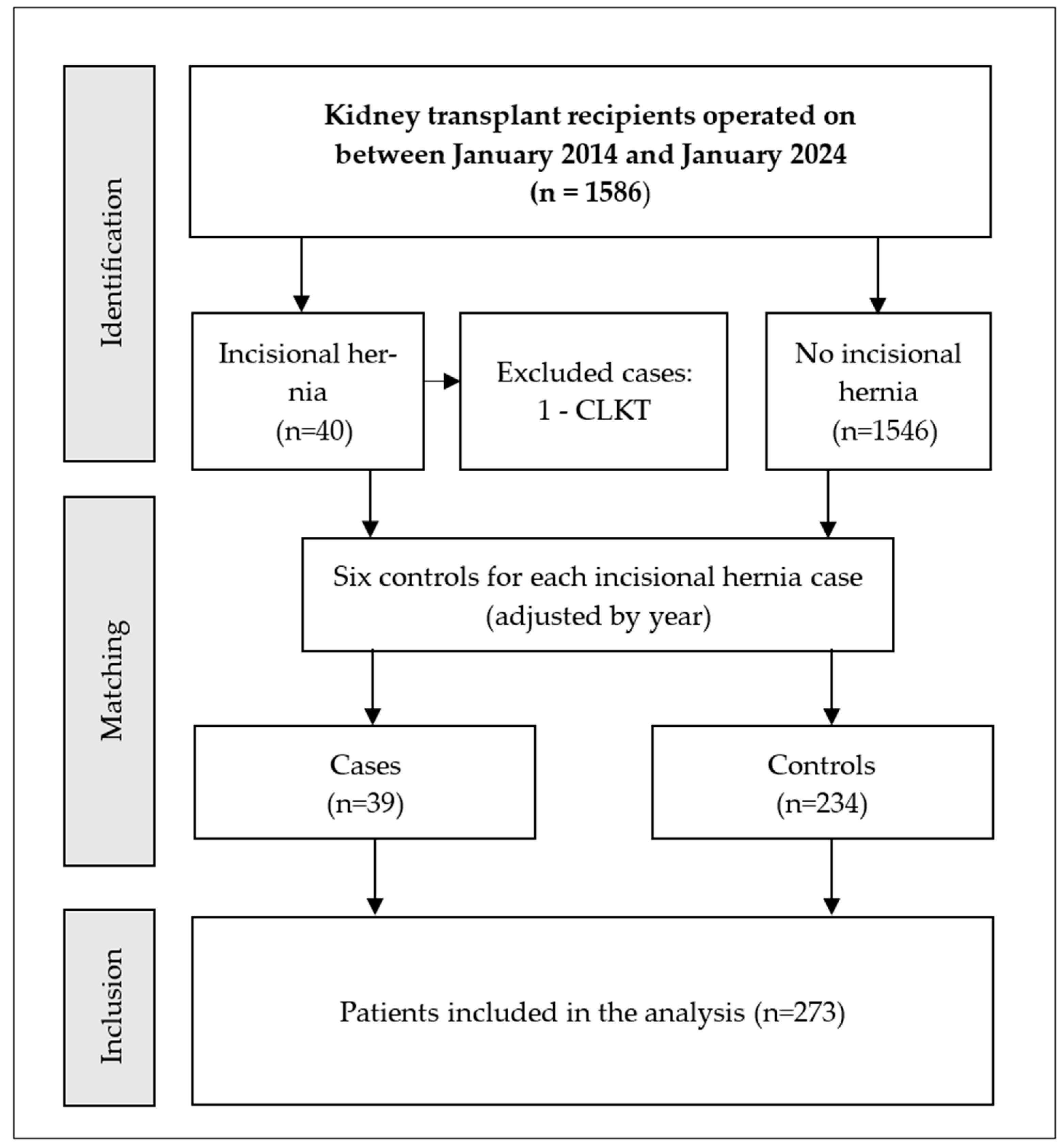
2.1. Study Design and Setting
2.2. Participants
2.3. Procedure
2.3.1. Transplant Technique
2.3.2. Immunosuppression
2.3.3. Incisional Hernia Diagnosis
2.4. Variables
2.5. Data Sources and Measurements
2.6. Statistical Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IH | Incisional hernia |
| PKD | Polycystic kidney disease |
| PD | Peritoneal dialysis |
| BMI | Body mass index |
| CLKT | Combined liver and kidney transplantation |
| IQR | Interquartile range |
References
- Nachiappan, S.; Subramanian, A.; Stewart, S.; Oke, T. Prophylactic mesh placement in high-risk patients undergoing elective laparotomy: A systematic review. World J. Surg. 2013, 37, 1861–1871. [Google Scholar] [CrossRef]
- van Ramshorst, G.H.; Eker, H.H.; Hop, W.C.; Jeekel, J.; Lange, J.F. Impact of incisional hernia on health-related quality of life and body image: A prospective cohort study. Am. J. Surg. 2012, 204, 144–150. [Google Scholar] [CrossRef]
- de Goede, B.; Eker, H.H.; Klitsie, P.J.; van Kempen, B.J.; Polak, W.G.; Hop, W.C.; Metselaar, H.J.; Tilanus, H.W.; Lange, J.F.; Kazemier, G. Incisional hernia after liver transplantation: Risk factors and health-related quality of life. Clin. Transplant. 2014, 28, 829–836. [Google Scholar] [CrossRef]
- Itatsu, K.; Yokoyama, Y.; Sugawara, G.; Kubota, H.; Tojima, Y.; Kurumiya, Y.; Kono, H.; Yamamoto, H.; Ando, M.; Nagino, M. Incidence of and risk factors for incisional hernia after abdominal surgery. Br. J. Surg. 2014, 101, 1439–1447. [Google Scholar] [CrossRef]
- Røine, E.; Bjørk, I.T.; Øyen, O. Targeting risk factors for impaired wound healing and wound complications after kidney transplantation. Transplant. Proc. 2010, 42, 2542–2546. [Google Scholar] [CrossRef] [PubMed]
- Chiu, P.H.; Liu, J.M.; Hsieh, M.L.; Kao, W.T.; Yu, K.J.; Pang, S.T.; Lin, P.H. The risk factors of the occurrence of inguinal hernia in ESRD patients receiving dialysis treatment: An observational study using national health insurance research database. Medicine 2022, 101, e31794. [Google Scholar] [CrossRef] [PubMed]
- Mazzucchi, E.; Nahas, W.C.; Antonopoulos, I.M.; Ianhez, L.E.; Arap, S. Incisional hernia and its repair with polypropylene mesh in renal transplant recipients. J. Urol. 2001, 166, 816–819. [Google Scholar] [CrossRef] [PubMed]
- Birolini, C.; Mazzucchi, E.; Utiyama, E.M.; Yoshimura, E.M.; Nahas, W.C.; Rasslan, S. Prosthetic repair of incisional hernia in kidney transplant patients: A technique with onlay polypropylene mesh. Hernia 2001, 5, 31–35. [Google Scholar] [CrossRef]
- Ooms, L.S.; Verhelst, J.; Jeekel, J.; Ijzermans, J.N.; Lange, J.F.; Terkivatan, T. Incidence, risk factors, and treatment of incisional hernia after kidney transplantation: An analysis of 1564 consecutive patients. Surgery 2016, 159, 1407–1411. [Google Scholar] [CrossRef]
- Smith, C.T.; Katz, M.G.; Foley, D.; Vandenberg, S.L.; Leverson, G.E.; Mezrich, J.D. Incidence and risk factors of incisional hernia formation following abdominal organ transplantation. Surg. Endosc. 2015, 29, 398–404. [Google Scholar] [CrossRef]
- Montalti, R.; Mimmo, A.; Rompianesi, G.; Serra, V.; Cautero, N.; Ballarin, R.; De Ruvo, N.; Cunningham, R.; Enrico, G.; Di Benedetto, F. Early use of mammalian target of rapamycin inhibitors is an independent risk factor for incisional hernia development after liver transplantation. Liver Transplant. 2012, 18, 188–194. [Google Scholar] [CrossRef]
- Huitfeldt Sola, K.; Brismar, T.; Lorant, T.; Fränneby, U.; Larsson, O.; Genberg, H. Prediction of incisional hernia after kidney transplantation: Analysis of wound closure technique and risk factors. Hernia 2025, 29, 256–265. [Google Scholar] [CrossRef]
- Deerenberg, E.B.; Harlaar, J.J.; Steyerberg, E.W.; Lont, H.E.; van Doorn, H.C.; Heisterkamp, J.; Wijnhoven, B.P.; Schouten, W.R.; Cense, H.A.; Stockmann, H.B.; et al. Small bites versus large bites for closure of abdominal midline incisions (STITCH): A double-blind, randomised controlled trial. Lancet 2015, 386, 1254–1260. [Google Scholar] [CrossRef]
- Murtha, A.P.; Kaplan, A.L.; Paglia, M.J.; Mills, B.B.; Feldstein, M.L.; Ruff, G.L. Evaluation of a novel technique for wound closure using a barbed, bidirectional suture. Obstet. Gynecol. 2006, 107, 143–149. [Google Scholar] [CrossRef]
- Varga, M.; Matia, I.; Kucera, M.; Oliverius, M.; Adamec, M. Polypropylene mesh repair of incisional hernia after kidney transplantation: Single-center experience and review of the literature. Ann. Transplant. 2011, 16, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Li, E.N.; Silverman, R.P.; Goldberg, N.H. Incisional hernia repair in renal transplantation patients. Hernia 2005, 9, 231–237. [Google Scholar] [CrossRef]
- Höer, J.; Lawong, G.; Klinge, U.; Schumpelick, V. Einflussfaktoren der Narbenhernienentstehung. Retrospektive Untersuchung an 2.983 laparotomierten Patienten über einen Zeitraum von 10 Jahren [Factors influencing the development of incisional hernia. A retrospective study of 2,983 laparotomy patients over a period of 10 years]. Chirurg 2002, 73, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, A.D.; Mukherjee, T.; Tashjian, N.; Siu, M.; Fitzgibbons, R., Jr.; Nandipati, K. Staged complex abdominal wall hernia repair in morbidly obese patients. Hernia 2021, 25, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Mahdavi, R.; Mehrabi, M. Incisional hernia after renal transplantation and its repair with propylene mesh. Urol. J. 2004, 1, 259–262. [Google Scholar] [PubMed]
- Humar, A.; Ramcharan, T.; Denny, R.; Gillingham, K.J.; Payne, W.D.; Matas, A.J. Are wound complications after a kidney transplant more common with modern immunosuppression? Transplantation 2001, 72, 1920–1923. [Google Scholar] [CrossRef]
- Yang, S.F.; Liu, C.J.; Yang, W.C.; Chang, C.F.; Yang, C.Y.; Li, S.Y.; Lin, C.C. The risk factors and the impact of hernia development on technique survival in peritoneal dialysis patients: A population-based cohort study. Perit. Dial. Int. 2015, 35, 351–359. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cheng, X.B.J.; Bargman, J. Complications of Peritoneal Dialysis Part I: Mechanical Complications. Clin. J. Am. Soc. Nephrol. 2024, 19, 784–790. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pirson, Y. Extrarenal manifestations of autosomal dominant polycystic kidney disease. Adv. Chronic Kidney Dis. 2010, 17, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Chapman, A.B.; Devuyst, O.; Eckardt, K.U.; Gansevoort, R.T.; Harris, T.; Horie, S.; Kasiske, B.L.; Odland, D.; Pei, Y.; Perrone, R.D.; et al. Autosomal-dominant polycystic kidney disease (ADPKD): Executive summary from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2015, 88, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Endo, T.; Miyahara, K.; Shirasu, T.; Mochizuki, Y.; Taniguchi, R.; Takayama, T.; Hoshina, K. Risk Factors for Incisional Hernia After Open Abdominal Aortic Aneurysm Repair. In Vivo 2023, 37, 2803–2807. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Variable | Incisional Hernia (n = 39) | No Incisional Hernia (n = 234) | p-Value | |
|---|---|---|---|---|
| Sex (%) | Male Female | 30 (76.9) 9 (23.1) | 136 (57.9) 99 (42.1) | 0.02 a |
| Age (years), median [IQR] | 68 [14] | 59 [19] | 0.009 b | |
| BMI (kg/m2), median [IQR] | 28.2 [5.9] | 25.3 [5.5] | 0.001 b | |
| BMI (%) | <25.0 kg/m2 | 12 (30.8) | 101 (43.5) | 0.03 b |
| 25.0–29.9 kg/m2 | 13 (33.3) | 90 (38.8) | ||
| >30 kg/m2 | 14 (35.9) | 41 (17.7) | ||
| Hypertension (%) | Yes No | 37 (94.9) 2 (5.1) | 196 (84.5) 36 (15.5) | 0.08 c |
| Diabetes mellitus (%) | Yes No | 9 (23.1) 30 (76.9) | 43 (18.5) 189 (81.5) | 0.50 b |
| Diabetic nephropathy | Yes No | 6 (15.8) 32 (84.2) | 18 (7.9) 211 (92.1) | 0.11 b |
| PKD (%) | Yes No | 1 (2.6) 38 (97.4) | 39 (16.8) 193 (83.2) | 0.02 c |
| Peritoneal dialysis (%) | Yes No | 29 (74.4) 10 (25.6) | 134 (57.0) 101 (43.0) | 0.04 b |
| Repeat transplantation (%) | Yes No | 4 (10.3) 35 (89.7) | 41 (17.4) 195 (82.6) | 0.26 c |
| Surgical site (%) | RIF LIF | 9 (23.7) 29 (76.3) | 80 (34.1) 155 (65.9) | 0.20 b |
| Suture type (%) | Stratafix Maxon Loop | 10 (25.6) 29 (74.4) | 78 (33.2) 157 (66.8) | 0.35 b |
| Variable | OR | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Sex (male) | 1.57 | 0.85–4.39 | 0.11 |
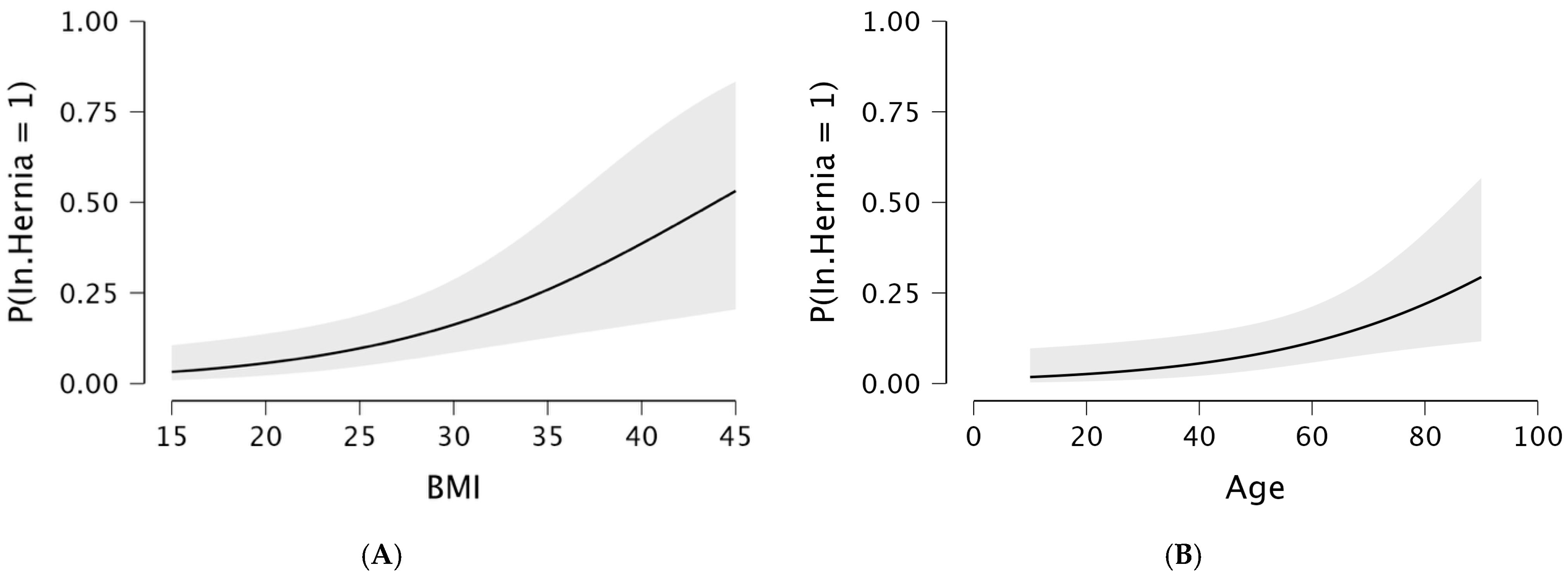
| Age | 1.04 | 1.01–1.07 | 0.01 |
| Obesity * | 2.55 | 1.18–5.49 | 0.01 |
| Peritoneal dialysis | 1.81 | 0.94–4.60 | 0.07 |
| Variable | Stratafix N = 88 | Maxon Loop N = 186 | p-Value | |
|---|---|---|---|---|
| Sex (%) | Male Female | 61 (69.3) 27 (30.7) | 105 (56.4) 81 (43.6) | 0.04 a |
| Age (years), median [IQR] | 61 [13.0] | 60.0 [21.7] | 0.86 b | |
| BMI (kg/m2), median [IQR] | 26.4 [6.0] | 25.3 [5.8] | 0.09 b | |
| BMI (%) | <25.0 kg/m2 | 32 (36.4) | 81 (44.3) | 0.31 a |
| 25.0–29.9 kg/m2 | 34 (38.6) | 69 (37.7) | ||
| >30 kg/m2 | 22 (25.0) | 33 (18.0) | ||
| Hypertension (%) | Yes No | 73 (82.9) 15 (17.1) | 23 (12.6) 160 (87.4) | 0.32 a |
| Diabetes mellitus (%) | Yes No | 19 (21.6) 69 (78.4) | 33 (18.0) 150 (82.0) | 0.48 a |
| PKD (%) | Yes No | 15 (17.1) 73 (82.9) | 25 (13.7) 158 (86.3) | 0.46 a |
| Peritoneal dialysis (%) | Yes No | 31 (35.2) 57 (54.8) | 89 (43.0) 106 (57.0) | 0.22 a |
| Repeat transplantation (%) | Yes No | 25 (28.4) 63 (71.6) | 20 (10.7) 166 (89.2) | 0.001 a |
| Surgical site (%) | RIF LIF | 20 (23.0) 67 (77.0) | 69 (37.1) 117 (62.9) | 0.02 a |
| Incisional Hernia | Yes No | 10 (11.4) 78 (88.6) | 29 (15.6) 158 (84.4) | 0.35 a |
| Incisional Hernia | All Recipients N (%) | Stratafix N (%) | Maxon Loop N (%) | p-Value a | |
|---|---|---|---|---|---|
| BMI | |||||
| <25.0 kg/m2 | Yes No | 12 (10.6) 101 (89.4) | 3 (9.4) 29 (90.6) | 9 (11.1) 72 (88.9) | 0.78 |
| 25.0–29.9 kg/m2 | Yes No | 13 (12.6) 90 (87.4) | 5 (14.7) 29 (85.3) | 8 (11.6) 61 (88.4) | 0.65 |
| >30 kg/m2 | Yes No | 14 (25.5) 41 (74.5) | 2 (9.1) 20 (90.9) | 12 (36.4) 21 (63.6) | 0.02 |
| Transplantation History | |||||
| Repeat | Yes No | 4 (8.8) 41 (91.1) | 2 (8.0) 23 (92.0) | 2 (10.0) 18 (90.0) | 0.81 |
| First | Yes No | 35 (15.3) 194 (84.7) | 8 (12.7) 55 (87.3) | 27 (16.3) 139 (83.7) | 0.51 |
| Sex | |||||
| Male | Yes No | 30 (18.1) 136 (81.9) | 7 (11.5) 54 (88.5) | 23.0 (21.9) 82 (78.1) | 0.09 |
| Female | Yes No | 9 (8.3) 99 (91.7) | 3 (11.1) 24 (88.9) | 6 (7.4) 75 (92.6) | 0.54 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
de la Mata, J.; Boiko, O.; Zarraga, S.; Garcia-Olaverri, J.; Llorente, A.; Prieto, S.; Lecumberri, D. Risk Factors for Incisional Hernia After Kidney Transplantation: Impact of Fascial Closure Suture Type. Transplantology 2026, 7, 4. https://doi.org/10.3390/transplantology7010004
de la Mata J, Boiko O, Zarraga S, Garcia-Olaverri J, Llorente A, Prieto S, Lecumberri D. Risk Factors for Incisional Hernia After Kidney Transplantation: Impact of Fascial Closure Suture Type. Transplantology. 2026; 7(1):4. https://doi.org/10.3390/transplantology7010004
Chicago/Turabian Stylede la Mata, Jorge, Oleksandr Boiko, Sofia Zarraga, Jorge Garcia-Olaverri, Ana Llorente, Sergio Prieto, and David Lecumberri. 2026. "Risk Factors for Incisional Hernia After Kidney Transplantation: Impact of Fascial Closure Suture Type" Transplantology 7, no. 1: 4. https://doi.org/10.3390/transplantology7010004
APA Stylede la Mata, J., Boiko, O., Zarraga, S., Garcia-Olaverri, J., Llorente, A., Prieto, S., & Lecumberri, D. (2026). Risk Factors for Incisional Hernia After Kidney Transplantation: Impact of Fascial Closure Suture Type. Transplantology, 7(1), 4. https://doi.org/10.3390/transplantology7010004






