Abstract
Objective: This study aims to examine long-term diseases, conditions, self-control, and self-management in kidney transplant recipients. Method: This is a descriptive correlational study, including a total of n = 130 kidney transplant recipients. The data were collected using a demographic information form, the Post-Kidney Transplant Diseases and Conditions Assessment Form, and the Self-Control and Self-Management Scale. Data analysis was conducted using descriptive statistical methods and one-way ANOVA, and paired sample t-tests. Results: Of the kidney transplant recipients, 40% were aged between 31 and 45 years, and 54.6% were male. The long-term diseases and conditions they developed after kidney transplantation were hypertension (46.2%), heart failure (26.2%), diabetes mellitus (10.8%), heartburn (35.4%), acute kidney failure (26.2%), urinary tract infection (39.2%), sleep disorders (23.1%), and chronic pain (50%). In addition, 31.5% of the kidney transplant recipients had poor self-control and self-management. Conclusions: Long-term postoperative mortality in kidney transplant recipients is mostly caused by diseases developing in vital organs. Therefore, it is crucial to recognize these diseases and conditions for their diagnosis. This study found various diseases and conditions in almost all body systems of kidney transplant recipients. Additionally, there were patients with poor self-control and self-management. We consider that the results of our study will increase awareness among clinicians.
1. Introduction
After kidney transplantation, graft viability and increased survival, as well as good patient outcomes, often result from various factors, primarily the effectiveness of immunosuppression [1,2,3]. Effective immunosuppression plays a central role in achieving optimal outcomes in kidney transplant recipients, although it is associated with an increased burden of toxicity and various complications [4,5]. Patients with end-stage renal disease who have developed kidney dysfunction prior to transplantation experience significant physiological and psychological problems due to increased toxicity and disrupted homeostasis. The goal of kidney transplantation is to eliminate all these problems. Although kidney transplant surgery aims for high survival and improved quality of life, kidney recipients may encounter various problems in the postoperative long term, including pre-existing issues before kidney transplantation. Complications and undesirable events that occur after kidney transplantation can lead to neuropsychiatric and physiological problems in patients [6,7].
Despite difficulties in finding kidney donors, the demand for kidney transplantation is increasing day by day. In the United States, the number of candidates on the waiting list for kidney transplantation increased from 61,488 in 2004 to 94,863 in 2019 [8,9]. In Turkey, a total of 3867 kidney transplants were performed in 2018, including 3009 live donor and 858 cadaveric donor transplants [10]. The situation is slightly different in Turkey. In this context, live kidney transplantation is used more frequently as a donor source compared to cadaveric kidney transplantation. However, this situation has not alleviated the shortage of donors. The Turkish Ministry of Health reports that there are over 19,000 candidates waiting for kidney transplantation [11]. According to the Organ Procurement and Transplantation Network, the kidney donor risk index indicates that kidneys with a higher risk of failure are transplanted more frequently from cadaveric donors [12]. The selection of live or cadaveric donor organs has the greatest impact on the risk of organ rejection, but its effect on other short- and long-term complications is not fully known.
In the short term after kidney transplant surgery, the return and integration of recipients into social life are often facilitated with the support of their loved ones. There is insufficient literature on the diseases and conditions that kidney recipients face in the long term, as well as their levels of self-management and self-control. Strong self-management and self-control enable individuals to have control over all aspects when needed. The care and treatment regimen for kidney recipients often lasts for years. The ability to be resilient against internal and external problems in postoperative long term, willingness to collaborate with healthcare professionals and social circle, and critical thinking are essential elements that contribute to strong self-management and self-control skills in organ recipients [13,14]. Sustainability and continuity are crucial in meeting the postoperative care needs of kidney transplant recipients. Personal hygiene, adherence to medication therapy and care management, and monitoring of current and potential diseases and conditions are essential for their survival. This study aimed to examine the long-term diseases, conditions, self-control, and self-management in kidney transplant recipients.
2. Materials and Methods
2.1. Research Design and Participants
This is a descriptive cross-sectional study. Our study was conducted on participating kidney transplant recipients after obtaining ethical approval. The data were collected by the researchers at the organ transplantation unit of an education and research hospital in western Turkey. Data collection was conducted between 15 July 2022 and 25 November 2022. Written informed consent was obtained from the kidney transplant recipients, followed by the completion of a personal information form and the self-management and self-control scale within 30 min. The recipients’ health-related records and post-kidney transplantation diseases and conditions were extracted from their patient files by the researchers. A power analysis was conducted to calculate the sample size. With a power of 0.95 and considering an error rate α = 0.05, the minimum sample size was calculated as 111 kidney transplant recipients. The sample of this study consisted of 130 kidney transplant recipients. The inclusion and exclusion criteria for the study are listed below.
2.2. Inclusion and Exclusion Criteria
In this study, the inclusion criteria were as follows: (i) being 18 years of age or older and having undergone kidney transplantation at least 1 year ago; (ii) no communication, language, or speech barriers; (iii) kidney transplant recipients who have regular health checks and high compliance with immunosuppressive therapy; (iv) willingness to participate in the study. Individuals who did not meet these criteria and those who underwent kidney transplantation less than one year ago were excluded from the study.
2.3. Data Collection Tools
The data were collected using a personal information form, the Post-Kidney Transplant Diseases and Conditions Assessment Form, the Self-Control and Self-Management Scale, and Charlson comorbidity index. Information about the tools is presented below.
2.4. Personal Information Form
The personal information form was created by the researchers through literature review. It includes questions about the patients’ sociodemographic characteristics (age, gender, marital status, education level, and organ donor).
2.5. Post-Kidney Transplant Diseases and Conditions Assessment Form
This form was developed by the researchers based on the literature [5,14,15,16,17,18] and expert opinions to examine the presence of potential diseases and conditions that may occur after kidney transplantation. The form consists of questions in 10 categories: cardiovascular, endocrine, respiratory, gastrointestinal, musculoskeletal, hematological, renal, dermatological, neuropsychiatric, and others. For the answers, it was required that the diseases and conditions be diagnosed by a physician. Therefore, in addition to patient statements, health records and discharge summaries were also taken into account.
2.6. Self-Control and Self-Management Scale
The scale was developed by Mezo (2009) [19] and adapted into Turkish by Ercoşkun (2016) [20]. This is a 6-point Likert-type scale (0 = Does not describe me at all, 5 = Describes me completely). It consists of 16 items, and the items 7, 8, 9, 10, and 11 are scores in reverse. The scale has 3 subscales: self-motoring, self-evaluating, and self-reinforcing. The Cronbach’s alpha reliability coefficient was found to be 0.87 for the total scale, 0.80 for the self-motoring subscale, 0.73 for the self-evaluating subscale, and 0.81 for the self-reinforcing subscale [20]. In this study, the Cronbach’s alpha reliability coefficient for the total scale was found to be 0.89.
2.7. Charlson Comorbidity Index
A total of 19 conditions and comorbidities are assessed, and a point is constituted accordingly in the Charlson comorbidity index (CCI). CCI was created by Charlson [21]. The CCI estimates 1-year mortality and categorizes various diseases and conditions. Scores are given on a scale of 1, 2, 3, and 6 based on the risk level, and the scores used to predict mortality.
2.8. Statistical Analysis
After data coding by the researchers, the Statistical Package for the Social Sciences 25.0 IBM (Armonk, NY, USA) statistical program was used for statistical analysis. Descriptive statistics were used in data analysis. Prior to the analysis, the data were found to have normal distribution using the Kolmogorov–Smirnov test. One-way analysis of variance (ANOVA) test and paired sample t-test were used to determine the relationship between the scales and descriptive characteristics. Pearson correlation coefficient was used to determine statistical differences between means. The scale reliability coefficient was determined using Cronbach’s alpha. Complementary post hoc analysis was used to determine the differences. The results were evaluated with a 95% confidence interval and significance level of p < 0.05.
2.9. Ethical Considerations
For conducting the study, ethical approval was obtained from the Istanbul University-Cerrahpasa Non-Interventional Clinical Research Ethics Committee (Decision No: 2022, Number: 61, Date: 15 April 2022), and institutional review board (IRB) approval was obtained from the Istanbul University-Cerrahpasa Faculty of Medicine Hospital. In addition, informed consent was obtained from the patients in accordance with the Declaration of Helsinki. Patients who agreed to participate in the study were included in the study after obtaining their verbal and written consent.
3. Results
Table 1 presents the sociodemographic characteristics and SCMSS mean scores of kidney transplant recipients. Of the kidney transplant recipients, 40% were in the 31–45 age range, 54.6% were male, and 56.2% were married. In addition, 30.8% of them had completed primary education, and 50.8% had a middle-income level. The average hospital stay for kidney transplant recipients was 16 ± 5.71 days, and the average time since transplantation was 9.17 ± 5.65 years. Among the recipients, those in the 31–45 age range and those with higher- and middle-income levels had higher SCMSS scores compared to those in other age ranges and those with lower-income levels. Self-control and self-management were poorer in those who developed graft rejection, and this difference was statistically significant (p = 0.023). The mean CCI of kidney transplant recipients was 3.79 ± 1.47.

Table 1.
Sociodemographic characteristics and SCMSS mean scores of kidney transplant recipients (n = 130).
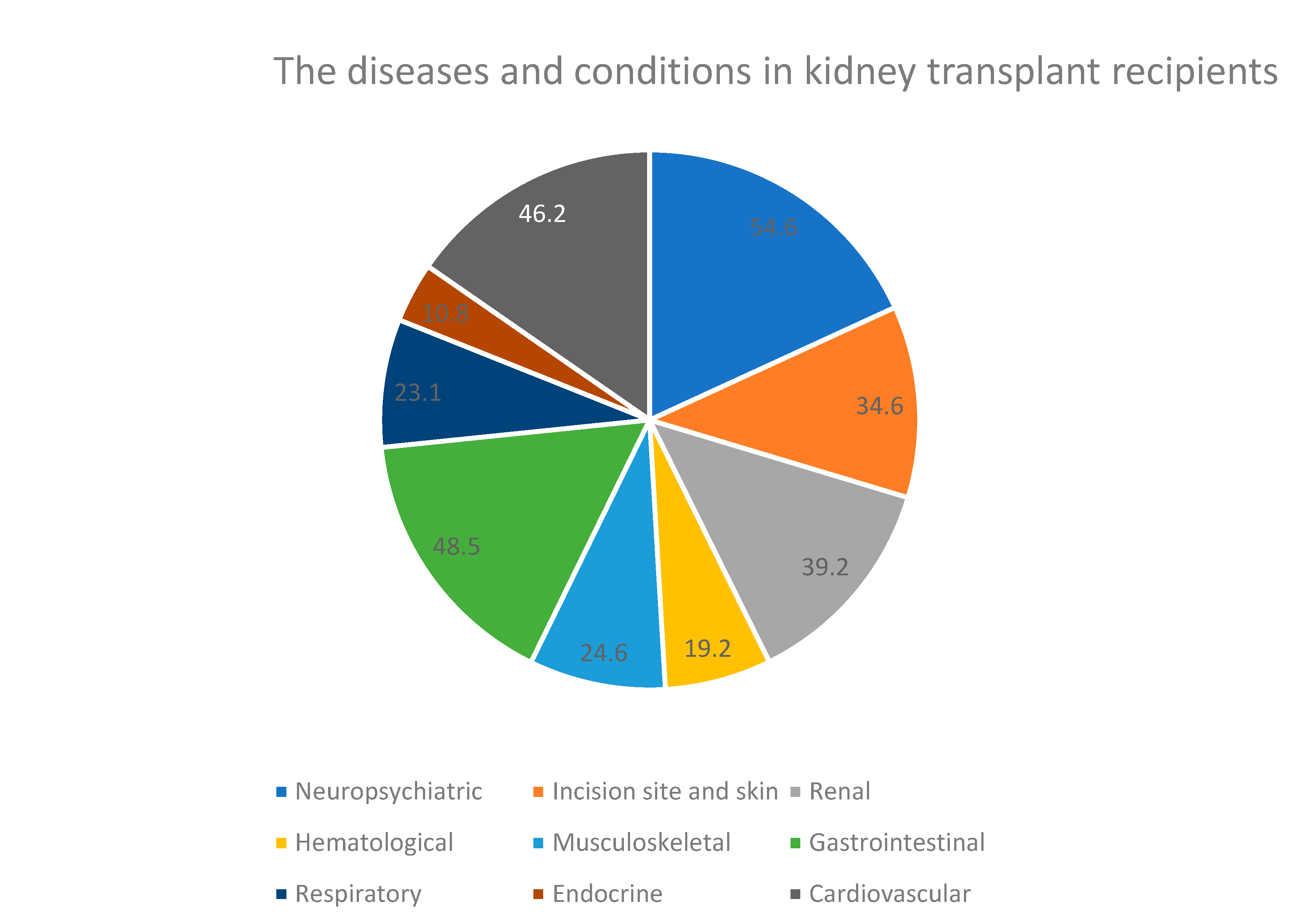
Table 2 shows the diseases and conditions experienced by kidney transplant recipients in the long term. Among the recipients, 46.2% had hypertension, 26.9% had heart failure, and 10.8% had diabetes mellitus (DM). Pneumonia, heartburn, dental problems, increased appetite, acute kidney injury (AKI), urinary system infection (USI), fatigue, sexual dysfunction, sleep disorders, and chronic pain were reported in 23.1%, 35.4%, 34.6%, 48.5%, 26.2%, 39.2%, 54.6%, 26.9%, 23.1%, and 50% of the recipients, respectively. All kidney transplant recipients were using immunosuppressive medication.

Table 2.
Long-term diseases and conditions experienced by kidney transplant recipients.
Figure 1 shows the distribution of commonly encountered diseases and conditions among kidney transplant recipients according to body systems. Based on Figure 1, the most frequent diseases and conditions were seen in the neuropsychiatric (54.6%), gastrointestinal (48.5%), and cardiovascular (46.2%) systems, while endocrine (10.8%) and hematological (19.2%) conditions were less common.
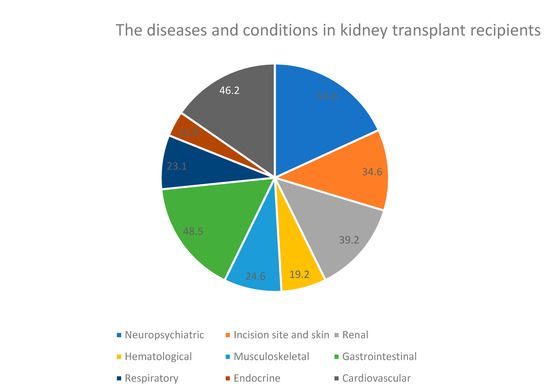
Figure 1.
Distribution of common diseases and conditions in kidney transplant recipients by body systems (n = 130). The distribution of common diseases and conditions in kidney transplant recipients in body systems is shown.
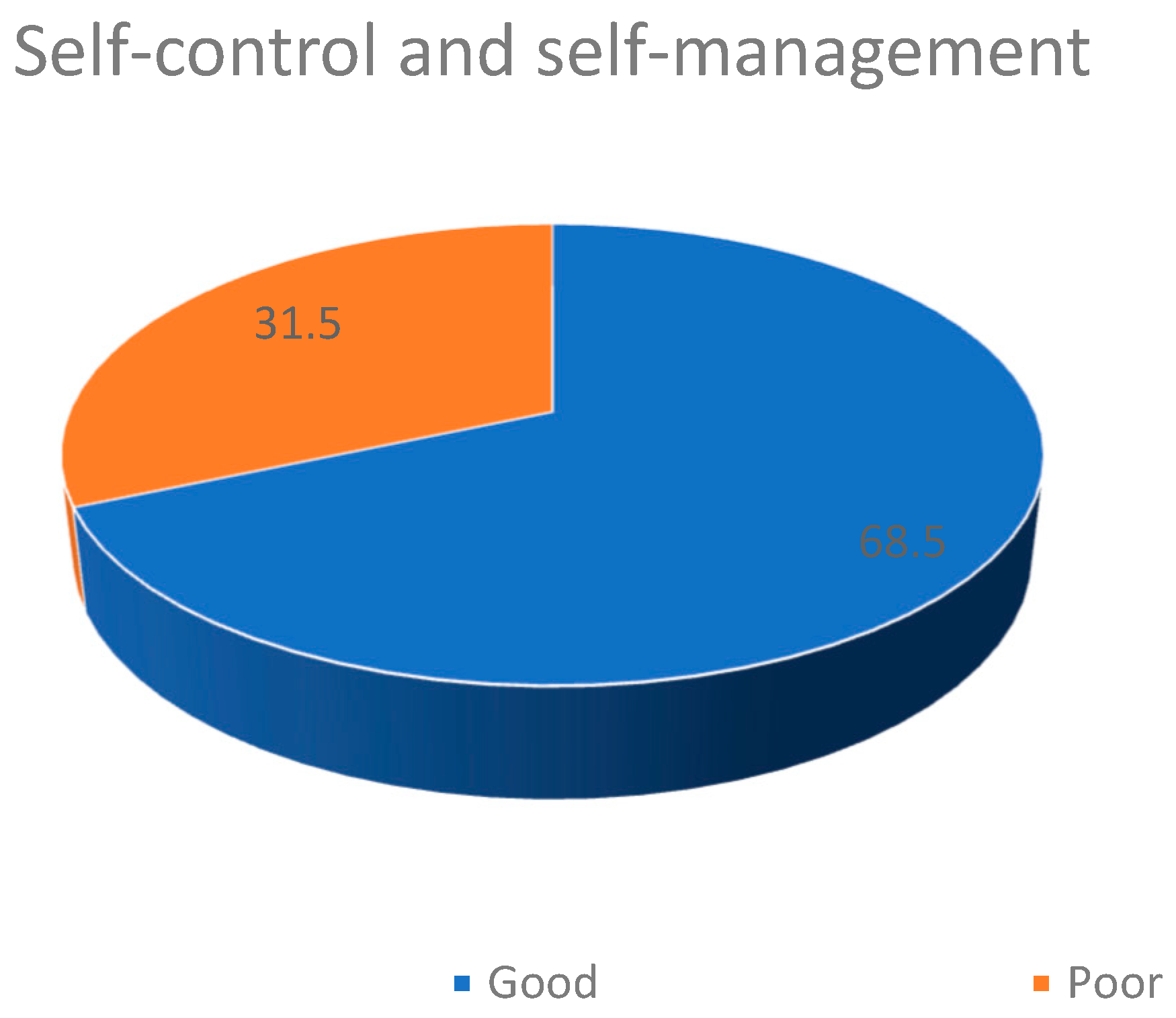
Figure 2 displays the self-control and self-management of kidney transplant recipients. Using a cutoff score of 66 points (mean score), it was determined that 89 (68.5%) kidney transplant recipients had good self-control and self-management (scored 66 or above), while 41 (31.5%) recipients had poor self-control and self-management (Figure 2).
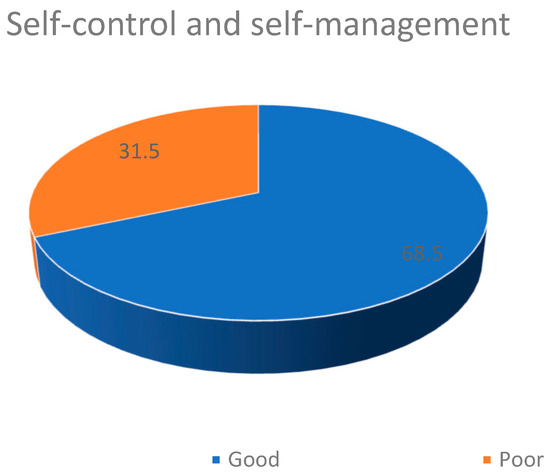
Figure 2.
Self-control and self-management in kidney transplant recipients (n = 130).
Table 3 presents the SCMSS total and subscale mean scores of kidney transplant recipients. Their SCMSS total mean score was 69.83 ± 11.77. Their self-monitoring, self-evaluating, and self-reinforcing subscale mean scores were 29.51 ± 5.11, 17.25 ± 6.07, and 23.06 ± 5.23, respectively. There was a negative, moderate, and statistically significant correlation between CCI score and SCMSS total score as well as self-monitoring. There was a negative, strong and statistically significant correlation between CCI score and self-reinforcing.

Table 3.
SCMSS total and subscale scores of kidney transplant recipients (n = 130).
4. Discussion
Renal transplantation is a commonly used treatment modality for renal failure and is well known for its superiority in prolonging the life expectancy and improving the quality of life of end-stage renal disease patients [22,23,24,25]. According to data from the Turkish Ministry of Health, a total of 3858 kidney transplants were performed as of 2019, with 79% of them using living organ donors [26]. Considering the economic and social factors, kidney transplantation is a more favorable replacement therapy compared to hemodialysis. Periodic hemodialysis treatment not only restricts kidney patients’ freedom to travel but also requires continuous time commitment, which can reduce productivity. In this respect, kidney transplantation is more advantageous, because stable kidney transplant recipients come to the hospital much less frequently than hemodialysis patients. The increased cost of healthcare and the economic crises faced by countries have necessitated the reduction in budgets allocated to treatment and management of chronic diseases.
The decrease in morbidity and mortality after renal transplantation, advancements in surgical techniques, improvements in perioperative care quality, and developments in immunosuppressive treatment options have led to a preference for transplantation surgery as the choice of renal replacement therapy. However, renal transplantation surgery is a stressful and challenging experience, and the psychological and physiological burdens it imposes can lead to the development of psychopathology in kidney transplant recipients [27]. It has been reported that the majority of problems that occur after kidney transplantation are mainly due to the side effects of immunosuppressive drug therapy or treatment non-compliance. In our study, all kidney transplant recipients were still taking immunosuppressive medication, and their medication adherence levels were high. However, acute kidney injury was present in 26.2% of the recipients, and organ rejection was observed in 10.8% of them. Although this issue has not been discussed before in the literature, in this study, those who developed graft rejection had worse self-control and self-management (p < 0.01). In addition, the mean CCI score was 3.79 ± 1.47, and all had at least one comorbidity. The kidney transplant patients were highly aware of the use of immunosuppressive drugs, so those who neglected their medications may have been hesitant to admit their negligence.
In literature reviews, cardiovascular diseases have been identified as the most common cause of morbidity and mortality in kidney transplant recipients [28], and it has been determined that prevalent cardiovascular symptoms originate from the exacerbation of pre-existing risk factors such as hypertension, dyslipidemia, obesity, and diabetes [29]. Additionally, it is noted that coronary artery disease is associated with the use of corticosteroids, cyclosporine, tacrolimus, and to some extent, azathioprine and mycophenolate mofetil (MMF) [30]. In our study, the proportion of kidney transplant recipients with cardiovascular diseases and conditions was quite high at 46.2%.
A previous study involving recipients who had a kidney transplant within the last 2 years determined that indigestion, diarrhea, abdominal pain, and constipation were commonly experienced gastrointestinal symptoms after kidney transplantation, predominantly caused by immunosuppressive drugs [4]. Another study indicated that in patients who had undergone kidney transplantation, immunosuppressants triggered diabetes mellitus (37.3%), cardiovascular problems (21.9%), thyroid disorders (8.5%), and liver problems (4.2%). The same study also noted that immunosuppressive drugs increased anxiety and stress [27]. Studies of post-kidney transplant disorders have mostly focused on patients within the first two years after transplantation. Our study included kidney transplant recipients with an average of 9 years since transplantation, ranging from 1 to 20 years. Kidney transplant recipients routinely use immunosuppressive drugs at lower doses even after 2 years of transplantation. This may result in a decrease in disease and various complications. Indeed, our study found a higher frequency of neuropsychiatric (54.6%), gastrointestinal (48.5%), and cardiovascular (46.2%) diseases and conditions, while endocrine (10.8%) and hematological (19.2%) diseases and conditions were less frequent.
There are no studies in the literature specifically examining the self-management and self-control of kidney transplant recipients. In our study, 46.2% of the kidney transplant recipients had hypertension, 26.9% had heart failure, 10.8% had diabetes mellitus, 26.2% had acute kidney injury, 26.9% had sexual dysfunction, 23.1% had sleep disorders, and 50% experienced chronic pain. In addition, 68.5% of the kidney transplant recipients had good self-control and self-management, while 31.5% had poor self-control and self-management. A previous study involving liver transplant recipients found that their self-control and self-management were below the moderate level [31]. Conducting new studies that comprehensively examine the commonly experienced diseases and conditions in the 2–10/15-year period after kidney transplantation is of great importance in guiding healthcare professionals. In this regard, our study is an important source of information for further studies. Our study is descriptive in nature, conducted at a single center, and could not reach a sample size large enough to be generalized to the population. Additionally, self-control and self-management may be influenced by cultural and social factors, and some living conditions (presence of dependents, responsibilities towards other family members and size, etc.). The effects of low self-control and self-management on social crises and hospitalizations were not investigated in this study. The measurement instruments were based on index, so statistical reliability and validity analyses were not performed. All of these factors were limitations in our study. However, we were able to access a substantial number of kidney transplant recipients, which demonstrates the strength of our study.
5. Conclusions
High survival and allograft recognition in kidney transplant recipients are closely related to effective immunosuppressive treatment for rejection prophylaxis and good self-control and self-management. Previous studies have focused on short-term health problems following kidney transplantation. This study examined the long-term diseases and conditions in kidney transplant recipients and their self-control and self-management. Diseases and conditions that develop in the long term after kidney transplantation can evolve into comorbidities over time. In addition, adhering to the long-term care and treatment regimen after kidney transplantation requires good self-control and self-management. This study found that the kidney transplant recipients developed various diseases and conditions, which are considered serious and mostly involve vital organs, in the long term, and approximately one-third of them had poor self-control and self-management. It is of great importance to monitor these diseases for poor patient outcomes and mortality. In the future, kidney transplant recipients should be supported to reduce life-threatening diseases and conditions and improve their health condition. We recommend implementing non-pharmacological interventions to support self-control and self-management in kidney transplant recipients and directing them towards different activities to enhance their awareness in this regard.
Author Contributions
All of the authors meet the authorship criteria. Research data were collected by Z.S.Y. and S.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Istanbul University Cerrahpasa Rectorate Clinical Research Ethics Committee (Date: 15 April 2022, Decision No: 2022/61).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated and/or analyzed in this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
There are no conflicts of interest for the authors or the article. The authors did not receive institutional support, non-commercial grants, or commercial support.
References
- Hariharan, S.; Israni, A.K.; Danovitch, G. Long-term survival after kidney transplantation. N. Engl. J. Med. 2021, 385, 729–743. [Google Scholar] [CrossRef] [PubMed]
- Sugi, M.D.; Joshi, G.; Maddu, K.K.; Dahiya, N.; Menias, C.O. Imaging of renal transplant complications throughout the life of the allograft: Comprehensive multimodality review. Radiographics 2019, 39, 1327–1355. [Google Scholar] [CrossRef] [PubMed]
- Poggio, E.D.; Augustine, J.J.; Arrigain, S.; Brennan, D.C.; Schold, J.D. Long-term kidney transplant graft survival—Making progress when most needed. Am. J. Transplant. 2021, 21, 2824–2832. [Google Scholar] [CrossRef]
- Bülbüloğlu, S.; Güneş, H.; Saritaş, S. The Effect of Long-Term Immunosuppressive Therapy on Gastrointestinal Symptoms after Kidney Transplantation. J. Transplant. Immunol. 2022, 70, 101515. [Google Scholar] [CrossRef] [PubMed]
- Cajanding, R. Immunosuppression following organ transplantation. Part 1: Mechanisms and immunosuppressive agents. Br. J. Nurs. 2018, 27, 920–927. [Google Scholar] [CrossRef]
- Carrasco, F.R.; Moreno, A.; Ridao, N.; Calvo, N.; Pérez-Flores, I.; Rodríguez, A.; Sánchez, A.; Marques, M.; Barrientos. Kidney transplantation complications related to psychiatric or neurological disorders. Transplant. Proc. 2009, 41, 2430–2432. [Google Scholar] [CrossRef]
- Shoskes, A.; Wilson, R. Neurologic complications of kidney transplantation. Transl. Androl. Urol. 2019, 8, 164. [Google Scholar] [CrossRef]
- Organ Procurement and Transplantation Network. National Data. 2019. Available online: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/ (accessed on 16 April 2023).
- Merion, R.M.; Ashby, V.B.; Wolfe, R.A.; Distant, D.A.; Hulbert-Shearon, T.E.; Metzger, R.A.; Ojo, A.O.; Port, F.K. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 2005, 294, 2726–2733. [Google Scholar] [CrossRef]
- Diniz, G.; Tugmen, C.; Sert, İ. Organ Transplantation in the Turkey and the World. Tepecik Educ. Res. Hosp. J. 2019, 29, 1–10. [Google Scholar] [CrossRef]
- Republic of Turkey Ministry of Health. Kan, Organ ve Doku Nakli Hizmetleri. [Blood, Organ and Tissue Transplant Services]. 2019. Available online: https://organkds.saglik.gov.tr/dss/PUBLIC/PublicDefault2.aspx (accessed on 1 June 2021).
- Organ Procurement and Transplantation Network. Kidney Donor Profile Index (KDPI) for Clinicians. 2019. Available online: https://optn.transplant.hrsa.gov/professionals/by-topic/guidance/kidney-donor-profile-index-kdpi-guide-for-clinicians (accessed on 16 April 2023).
- Zimmer-Gembeck, M.J.; Skinner, E.A.; Modecki, K.L.; Webb, H.J.; Gardner, A.A.; Hawes, T.; Rapee, R.M. The self-perception of flexible coping with stress: A new measure and relations with emotional adjustment. Cogent Psychol. 2018, 5, 1537908. [Google Scholar] [CrossRef]
- Bulbuloglu, S.; Harmanci, P.; Aslan, F.E. Investigation of perceived stress and psychological well-being in liver recipients having immunosuppressive therapy. iLiver 2023, 2, 10–15. [Google Scholar] [CrossRef]
- Carpenito-Moyet, L.J. Nursing Diagnosis: Application to Clinical Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008. [Google Scholar]
- Ordin, Y.S.; Karayurt, Ö.; Çilengiroğlu, Ö.V. Validation and adaptation of the Modified Transplant Symptom Occurrence and Symptom Distress Scale-59 Items Revised into Turkish. Prog. Transplant. 2013, 23, 392–400. [Google Scholar] [CrossRef]
- Cajanding, R. Immunosuppression following organ transplantation. Part 2: Complications and their management. Br. J. Nurs. 2018, 27, 1059–1065. [Google Scholar] [CrossRef] [PubMed]
- Ordin, Y.S. Karaciğer Transplantasyonu Sonrası Destek Grup Girişiminin Hastaların Bilgi, Semptom Ve Yaşam Kalitesi Düzeyine Etkisinin İncelenmesi. Ph.D. Thesis, Dokuz Eylül Üniversitesi, Sağlık Bilimleri Enstitüsü, İzmir, Turkey, 2013. [Google Scholar]
- Mezo, P.G. The Self-Control and Self-Management Scale (SCMS): Development of an adaptive selfregulatory coping skills instrument. J. Psychopathol. Behav. Assess. 2009, 31, 83–93. [Google Scholar] [CrossRef]
- Ercoşkun, M.H. Adaptation of Self-Control and Self-Management Scale (SCMS) into Turkish culture: A study on reliability and validity. Educ. Sci. Theory Pract. 2016, 16, 1125–1145. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Zhang, L.; Guo, Y.; Ming, H. Effects of hemodialysis, peritoneal dialysis, and renal transplantation on the quality of life of patients with end-stage renal disease. Rev. Assoc. Médica Bras. 2020, 66, 1229–1234. [Google Scholar] [CrossRef]
- Legendre, C.; Canaud, G.; Martinez, F. Factors influencing long-term outcome after kidney transplantation. Transplant. Int. 2014, 27, 19–27. [Google Scholar] [CrossRef]
- Ortiz, F.; Aronen, P.; Koskinen, P.K.; Malmström, R.K.; Finne, P.; Honkanen, E.O.; Sintonen, H.; Roine, R.P. Health-related quality of life after kidney transplantation: Who benefits the most? Transplant. Int. 2014, 27, 1143–1151. [Google Scholar] [CrossRef]
- Yang, L.S.; Shan, L.L.; Saxena, A.; Morris, D.L. Liver transplantation: A systematic review of long-term quality of life. Liver Int. 2014, 34, 1298–1313. [Google Scholar] [CrossRef]
- Seyahi, N.; Ateş, K.; Süleymanlar, G. Current status of renal replacement therapy in Turkey: A summary of the 2019 Turkish Society of Nephrology registry report. Turk. J. Nephrol. 2021, 30, 105–111. [Google Scholar] [CrossRef]
- Uyar, B. The analysis of immunosuppressant therapy adherence, depression, anxiety, and stress in kidney transplant recipients in the post-transplantation period. Transpl. Immunol. 2022, 75, 101686. [Google Scholar] [CrossRef]
- Neale, J.; Smith, A.C. Cardiovascular risk factors following renal transplant. World J. Transplant. 2015, 5, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Stoumpos, S.; Jardine, A.G.; Mark, P.B. Cardiovascular morbidity and mortality after kidney transplantation. Transpl. Int. 2015, 28, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Tepperman, E.; Ramzy, D.; Prodger, J.; Sheshgiri, R.; Badiwala, M.; Ross, H.; Rao, V. Surgical biology for the clinician: Vascular effects of immunosuppression. Can. J. Surg. 2010, 53, 57–63. [Google Scholar]
- Çınar, F.; Bulbuloglu, S. The Analysis of Liver Transplant Recipients’ Adherence to Immunosuppressant Therapy, Self-Control, and Self-Management in the Post-Transplantation Period. iLiver J. 2023, 2, 97–102. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).