Nutritional and Sarcopenia Assessment in Bilateral Lung Transplantation Recipient: Can “The Strongest One” Expect Improved Short-Term Outcomes?
Abstract
:1. Introduction
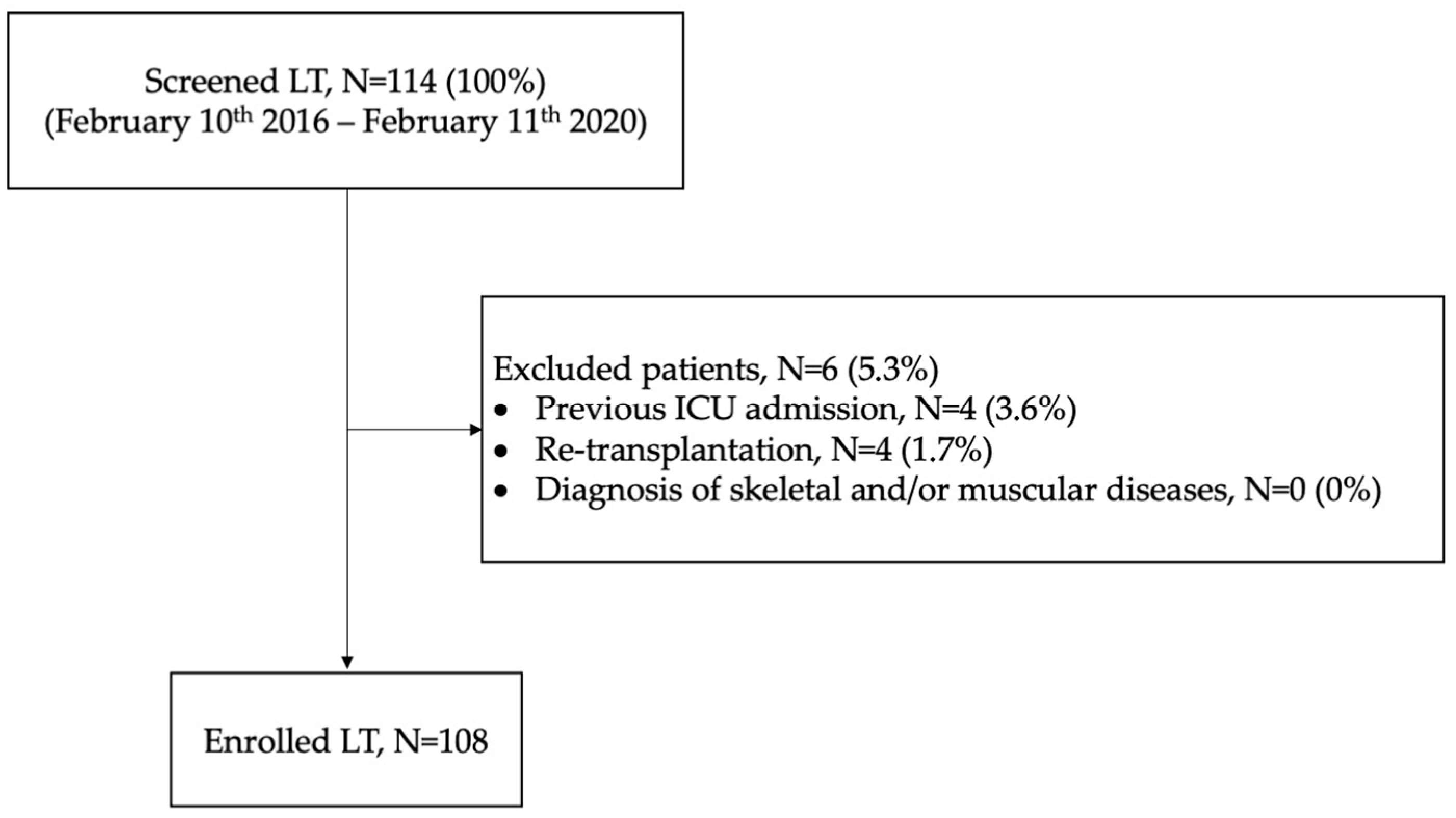
2. Materials and Methods
2.1. Nutritional Indexes
- (i)
- (ii)
- The prognostic nutritional index (PNI), which is calculated as the product between the serum albumin level and total lymphocyte count in the peripheral blood [29,30]. A reference value is still missing. Our median value (i.e., 50) was used to distinguished between “high PNI” versus “low PNI” recipients;
- (iii)
- The mini nutritional assessment short-form (MNA-SF) is a shorter and faster screening version of the MNA, validated for the assessment of nutritional problems in elderly populations [31]. In the MNA-SF, there are six items totaling 14 points (decrease in food intake in the previous three months, involuntary weight loss in the previous three months, mobility, psychological stress or acute disease in the previous three months, neuropsychological problems, and BMI or calf circumference). Based on the total score, patients were divided into three different categories of nutritional status (“well-nourished”: 12–14; “at risk”: 8–11; “malnourished”: 0–7).
2.2. Sarcopenia Indexes
- (i)
- The CHI score [32] was calculated by a standard formula as follows: CHI = (1⁄4 Daily urinary creatinine of patient/daily expected urinary creatinine for individuals of same height and sex) × 100. The expected value for daily urinary creatinine was obtained from reference charts. Based on CHI, nutritional status was classified as normal for CHI > 90%, mild malnutrition for CHI 80% to 90%, moderate malnutrition for CHI 60% to 80% and severe malnutrition for CHI < 60%;
- (ii)
- Paravertebral muscular densitometry: two musculoskeletal imaging radiologists, each possessing a decade of experience, gathered the mean Hounsfield Unit (Hu) value for the right paravertebral muscle at the level of the 12th dorsal vertebra through manual segmentation and extraction of Hu values. Muscle loss was defined as values < 30 Hu, according to the literature [24];
- (iii)
2.3. Statistical Analysis
3. Results
3.1. Description of Preoperative Nutritional and Muscular Status
3.2. Relationship between Preoperative Nutritional and Muscular Status and Outcomes
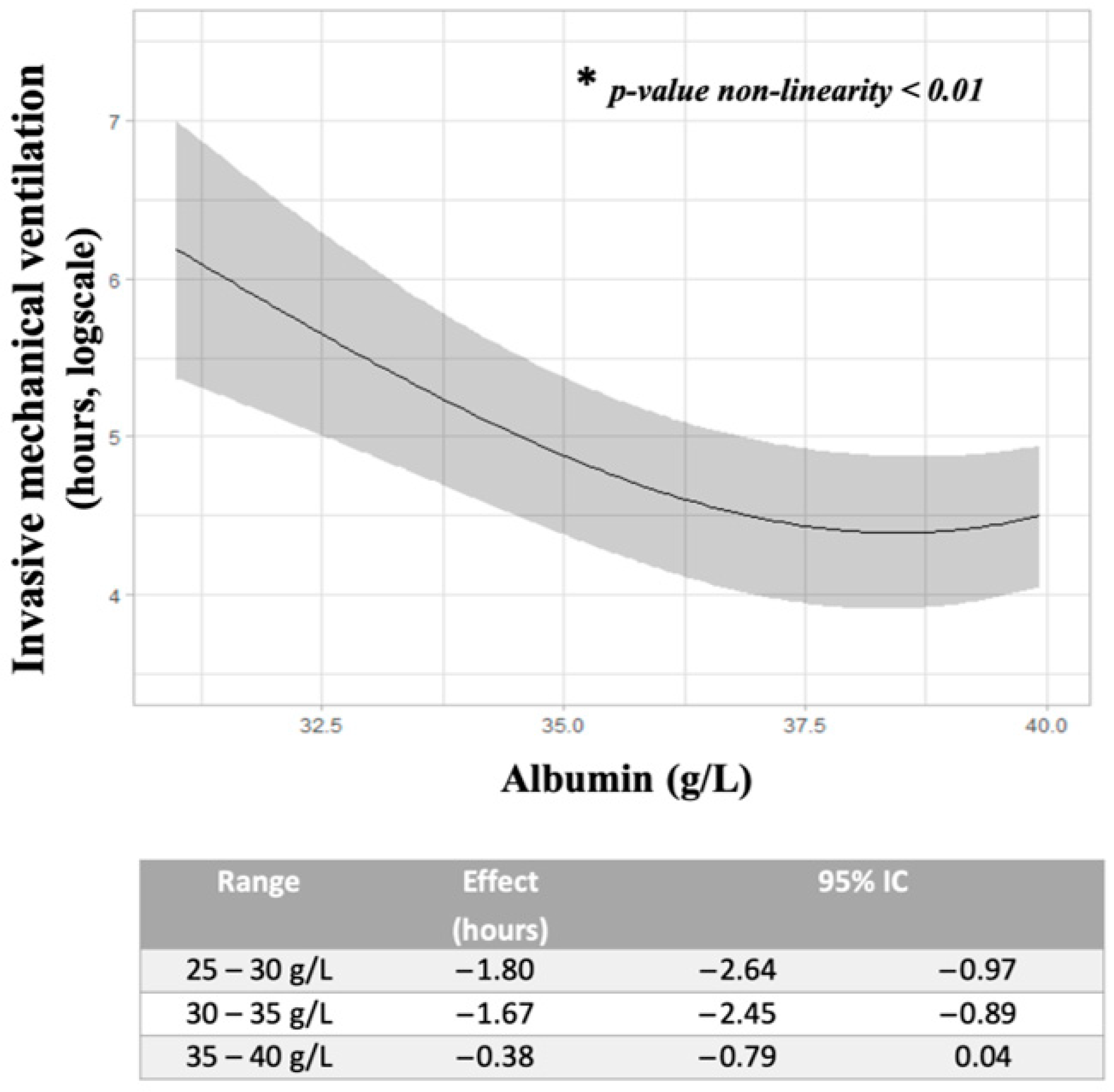
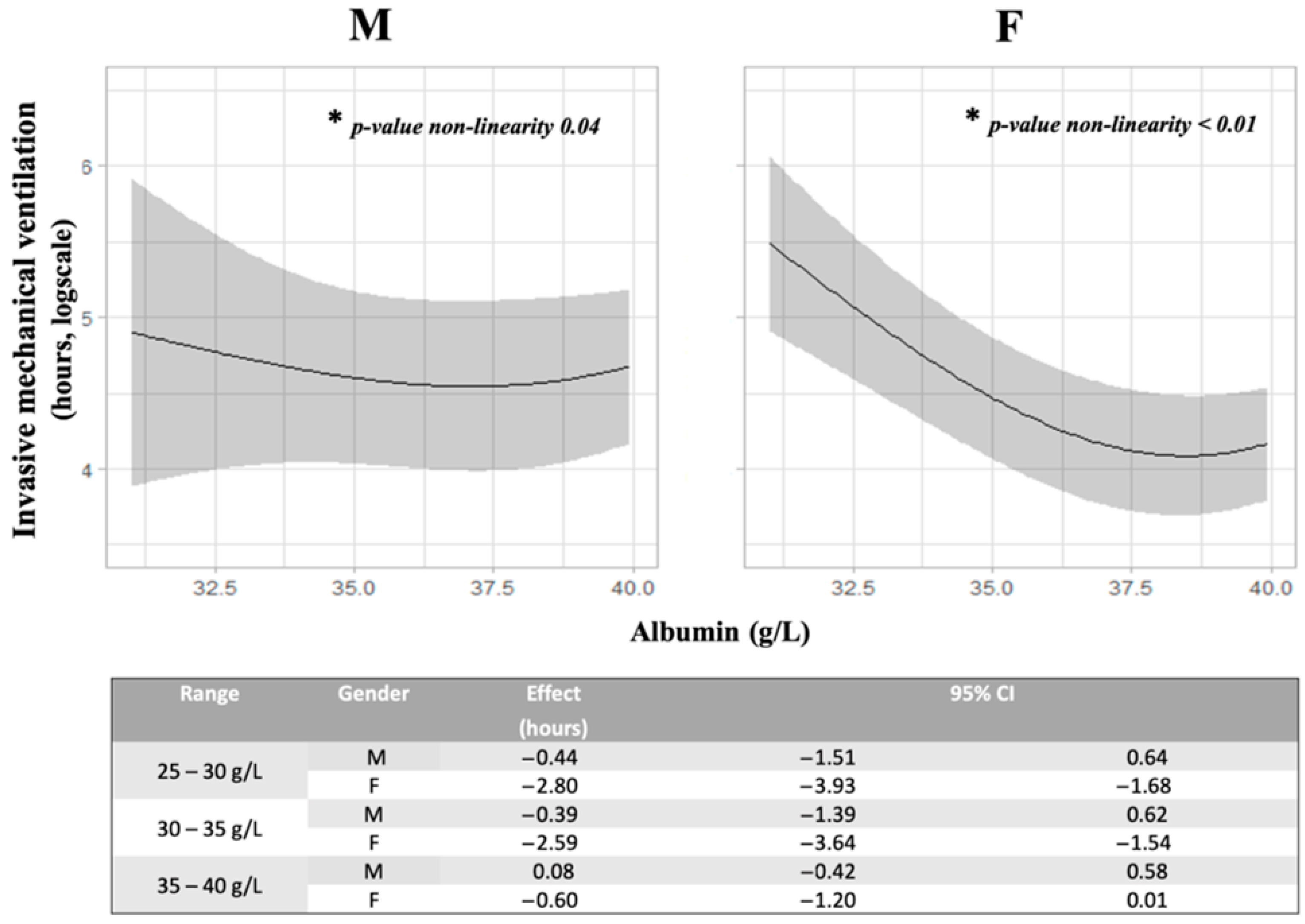
3.2.1. Relationship between Albumin Values and IMV
3.2.2. Relationship between Albumin Value, PNI Score, BMI and ICU Long-Stay
3.2.3. Additional Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khush, K.K.; Cherikh, W.S.; Chambers, D.C.; Harhay, M.O.; Hayes, D.; Hsich, E.; Meiser, B.; Potena, L.; Robinson, A.; Rossano, J.W.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-sixth adult heart transplantation report—2019; focus theme: Donor and recipient size match. J. Heart Lung Transplant. 2019, 38, 1056–1066. [Google Scholar] [CrossRef]
- Nosotti, M.; Tarsia, P.; Morlacchi, L.C. Infections after lung transplantation. J. Thorac. Dis. 2018, 10, 3849–3868. [Google Scholar] [CrossRef]
- Yusen, R.D.; Christie, J.D.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Dipchand, A.I.; Dobbels, F.; Kirk, R.; Lund, L.H.; Rahmel, A.O.; et al. The Registry of the International Society for Heart and Lung Transplantation: Thirtieth Adult Lung and Heart-Lung Transplant Report--2013; focus theme: Age. J. Heart Lung Transplant. 2013, 32, 965–978. [Google Scholar] [CrossRef] [PubMed]
- Weiss, E.S.; Allen, J.G.; Merlo, C.A.; Conte, J.V.; Shah, A.S. Factors indicative of long-term survival after lung transplantation: A review of 836 10-year survivors. Heart Lung Transplant. 2010, 29, 240–246. [Google Scholar] [CrossRef]
- Singh, V.K.; George, M.P.; Gries, C.J. Pulmonary hypertension is associated with increased post-lung transplant mortality risk in patients with chronic obstructive pulmonary disease. J. Heart Lung Transplant. 2015, 34, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Gries, C.J.; Bhadriraju, S.; Edelman, J.D.; Goss, C.; Raghu, G.; Mulligan, M.S. Obese patients with idiopathic pulmonary fibrosis have a higher 90-day mortality risk with bilateral lung transplantation. J. Heart Lung Transplant. 2015, 34, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Chamogeorgakis, T.; Mason, D.P.; Murthy, S.C.; Thuita, L.; Raymond, D.P.; Pettersson, G.B.; Blackstone, E.H. Impact of nutritional state on lung transplant outcomes. J. Heart Lung Transplant. 2013, 32, 693–700. [Google Scholar] [CrossRef] [PubMed]
- Congedi, S.; Navalesi, P.; Boscolo, A. Multidrug-resistant organisms in lung transplant: A narrative review. Curr. Opin. Organ Transplant. 2023, 28, 174–179. [Google Scholar] [CrossRef]
- Boscolo, A.; Sella, N.; Pettenuzzo, T.; De Cassai, A.; Crociani, S.; Schiavolin, C.; Simoni, C.; Geraldini, F.; Lorenzoni, G.; Faccioli, E.; et al. Multidrug-Resistant and Extended-Spectrum β-Lactamase Gram-Negative Bacteria in Bilateral Lung Transplant Recipients: Incidence, Risk Factors, and In-Hospital Mortality. Chest 2022, 162, 1255–1264. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef]
- Schaenman, J.M.; Diamond, J.M.; Greenland, J.R.; Gries, C.; Kennedy, C.C.; Parulekar, A.D.; Rozenberg, D.; Singer, J.P.; Singer, L.G.; Snyder, L.D.; et al. Frailty and aging-associated syndromes in lung transplant candidates and recipients. Am. J. Transplant. 2021, 21, 2018–2024. [Google Scholar] [CrossRef] [PubMed]
- Singer, J.P.; Calfee, C.S.; Delucchi, K.; Diamond, J.M.; Anderson, M.A.; Benvenuto, L.A.; Gao, Y.; Wang, P.; Arcasoy, S.M.; Lederer, D.J.; et al. Subphenotypes of frailty in lung transplant candidates. Am. J. Transplant. 2023, 23, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.I.; Ko, K.-P.; Choi, C.H.; Park, C.-H.; Park, K.Y.; Son, K.H. Does the prognostic nutritional index have a predictive role in the outcomes of adult cardiac surgery? J. Thorac. Cardiovasc. Surg. 2020, 160, 145–153.e3. [Google Scholar] [CrossRef]
- Jeon, H.G.; Choi, D.K.; Sung, H.H.; Jeong, B.C.; Seo, S.I.; Jeon, S.S.; Choi, H.-Y.; Lee, H.M. Preoperative Prognostic Nutritional Index is a Significant Predictor of Survival in Renal Cell Carcinoma Patients Undergoing Nephrectomy. Ann. Surg. Oncol. 2016, 23, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Allard, J.P.; Keller, H.; Jeejeebhoy, K.N.; Laporte, M.; Duerksen, D.R.; Gramlich, L.; Payette, H.; Bernier, P.; Davidson, B.; Teterina, A.; et al. Decline in nutritional status is associated with prolonged length of stay in hospitalized patients admitted for 7 days or more: A prospective cohort study. Clin. Nutr. 2016, 35, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Peng, D.; Gong, Y.-Q.; Hao, H.; He, Z.-S.; Li, X.-S.; Zhang, C.-J.; Zhou, L.-Q. Preoperative Prognostic Nutritional Index is a Significant Predictor of Survival with Bladder Cancer after Radical Cystectomy: A retrospective study. BMC Cancer 2017, 17, 391. [Google Scholar] [CrossRef] [PubMed]
- Piggott, K.D.; Liu, A.; Monczka, J.; Fakioglu, H.; Narasimhulu, S.S.; Pourmoghadam, K.; De Campli, W. Inadequate preoperative nutrition might be associated with acute kidney injury and greater illness severity postoperatively. J. Thorac. Cardiovasc. Surg. 2018, 155, 2104–2109. [Google Scholar] [CrossRef]
- Lu, K.; Li, H.; Chen, Y.; Wu, B.; Zhang, J.; Huang, M.; Chen, J. Can the preoperative nutritional risk score be a predictor of the outcomes in critically ill patients of lung transplantation: A retrospective study. Ann. Transl. Med. 2020, 8, 40. [Google Scholar] [CrossRef]
- Upala, S.; Panichsillapakit, T.; Wijarnpreecha, K.; Jaruvongvanich, V.; Sanguankeo, A. Underweight and obesity increase the risk of mortality after lung transplantation: A systematic review and meta-analysis. Transpl. Int. 2016, 29, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Singer, J.P.; Peterson, E.R.; Snyder, M.E.; Katz, P.P.; Golden, J.A.; D’ovidio, F.; Bacchetta, M.; Sonett, J.R.; Kukreja, J.; Shah, L.; et al. Body composition and mortality after adult lung transplantation in the United States. Am. J. Respir. Crit. Care Med. 2014, 190, 1012–1021. [Google Scholar] [CrossRef]
- Kim, C.Y.; Kim, S.Y.; Song, J.H.; Kim, Y.S.; Jeong, S.J.; Lee, J.G.; Paik, H.C.; Park, M.S. Usefulness of the preoperative prognostic nutritional index score as a predictor of the outcomes of lung transplantation: A single-institution experience. Clin. Nutr. 2019, 38, 2423–2429. [Google Scholar] [CrossRef] [PubMed]
- Schwebel, C.; Pin, I.; Barnoud, D.; Devouassoux, G.; Brichon, P.; Chaffanjon, P.; Chavanon, O.; Sessa, C.; Blin, D.; Guignier, M.; et al. Prevalence and consequences of nutritional depletion in lung transplant candidates. Eur. Respir. J. 2000, 16, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Efremov, S.M.; Boboshko, V.A.; Nikolaev, D.A.; Vedernikov, P.E.; Deryagin, M.N.; Lomivorotov, V.N.; Karaskov, A.M. Prognostic value of nutritional screening tools for patients scheduled for cardiac surgery. Thorac. Surg. 2013, 16, 612–618. [Google Scholar] [CrossRef]
- Giraudo, C.; Librizzi, G.; Fichera, G.; Motta, R.; Balestro, E.; Calabrese, F.; Carretta, G.; Cattelan, A.M.; Navalesi, P.; Pelloso, M.; et al. Reduced muscle mass as predictor of intensive care unit hospitalization in COVID-19 patients. PLoS ONE. 2021, 16, e0253433. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Kim, Y.S.; Park, I.; Ahn, H.K.; Cho, E.K.; Jeong, Y.M. Prognostic Significance of CT-Determined Sarcopenia in Patients with Small-Cell Lung Cancer. J. Thorac. Oncol. 2015, 10, 1795–1799. [Google Scholar] [CrossRef]
- Moisey, L.L.; Mourtzakis, M.; Cotton, B.A.; Premji, T.; Heyland, D.K.; Wade, C.; Bulger, E.; Kozar, R. Skeletal muscle predicts ventilator-free days, ICU-free days, and mortality in elderly ICU patients. Crit. Care 2013, 17, R206. [Google Scholar] [CrossRef]
- Kanasky, W.F.; Anton, S.D.; Rodrigue, J.R.; Perri, M.G.; Szwed, T.; Baz, M.A. Impact of body weight on long-term survival after lung transplantation. Chest 2002, 121, 401–406. [Google Scholar] [CrossRef]
- Hasse, J.M. Nutrition assessment and support of organ transplant recipients. J. Parenter. Enter. Nutr. 2001, 25, 120–131. [Google Scholar] [CrossRef]
- Schwegler, I.; von Holzen, A.; Gutzwiller, J.; Schlumpf, R.; Mühlebach, S.; Stanga, Z. Nutritional risk is a clinical predictor of postoperative mortality and morbidity in surgery for colorectal cancer. Br. J. Surg. 2010, 97, 92–97. [Google Scholar] [CrossRef]
- Gong, J.; Zuo, S.; Zhang, J.; Li, L.; Yin, J.; Li, X.; Yu, F.; Hu, W. Comparison of four nutritional screening tools in perioperative elderly patients: Taking orthopedic and neurosurgical patients as examples. Front. Nutr. 2023, 10, 1081956. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef] [PubMed]
- Datta, D.; Foley, R.; Wu, R.; Grady, J.; Scalise, P. Can Creatinine Height Index Predict Weaning and Survival Outcomes in Patients on Prolonged Mechanical Ventilation After Critical Illness? J. Intensive Care Med. 2018, 33, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Goodpaster, B.H.; Thaete, F.L.; Kelley, D.E. Composition of skeletal muscle evaluated with computed tomography. Ann. N. Y. Acad. Sci. 2000, 904, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Aubrey, J.; Esfandiari, N.; Baracos, V.E.; Buteau, F.A.; Frenette, J.; Putman, C.T.; Mazurak, V.C. Measurement of skeletal muscle radiation attenuation and basis of its biological variation. Acta Physiol. 2014, 210, 489–497. [Google Scholar] [CrossRef]
- Rozenberg, D.; Orsso, C.E.; Chohan, K.; Orchanian-Cheff, A.; Nourouzpour, S.; Nicholson, J.M.; Elangeswaran, B.; Vagaon, A.; Fidler, L.; Singer, L.G.; et al. Clinical outcomes associated with computed tomography-based body composition measures in lung transplantation: A systematic review. Transpl. Int. 2020, 33, 1610–1625. [Google Scholar] [CrossRef]
- Harrell, F.E., Jr. Regression Modeling Strategies. 2020. Available online: https://cran.r-project.org/package=rms (accessed on 1 April 2023).
- Leeper, T.J. Marginal Effects for Model Objects. 2021. Available online: https://cran.r-project.org/web/packages/margins/margins.pdf (accessed on 1 April 2023).
- Madill, J.; Gutierrez, C.; Grossman, J.; Allard, J.; Chan, C.; Hutcheon, M.; Keshavjee, S.H. Nutritional assessment of the lung transplant patient: Body mass index as a predictor of 90-day mortality following transplantation. J. Heart Lung Transplant. 2001, 20, 288–296. [Google Scholar] [CrossRef]
- Egan, T.M.; Murray, S.; Bustami, R.T.; Shearon, T.H.; McCullough, K.P.; Edwards, L.B.; Coke, M.A.; Garrity, E.R.; Sweet, S.C.; Heiney, D.A.; et al. Development of the new lung allocation system in the United States. Am. J. Transplant. 2006, 6, 1212–1227. [Google Scholar] [CrossRef]
- Weill, D.; Benden, C.; Corris, P.A.; Dark, J.H.; Davis, R.D.; Keshavjee, S.; Lederer, D.J.; Mulligan, M.J.; Patterson, G.A.; Singer, L.G.; et al. A consensus document for the selection of lung transplant candidates: 2014--an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2015, 34, 1–15. [Google Scholar] [CrossRef]
- Nicholson, J.; Wolmarans, M.; Park, G. The role of albumin in critical illness. Br. J. Anaesth. 2000, 85, 599–610. [Google Scholar] [CrossRef]
- Atrash, A.; De Vasconcellos, K. Low albumin levels are associated with mortality in the critically ill: A retrospective observational study in a multidisciplinary intensive care unit. Afr. J. Crit. Care 2020, 36, 74–79. [Google Scholar] [CrossRef]
- Bernard, F.M.; Al-Tamimi, Y.Z.; Chatfield, D.B.; Lynch, A.G.; Matta, B.F.F.; Menon, D.K.M. Serum albumin level as a predictor of outcome in traumatic brain injury: Potential for treatment. J. Trauma Inj. Infect. Crit. Care 2008, 64, 872–875. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.P.; Rios-Diaz, A.J.; Dalela, D.; Ravi, P.; Sood, A.; Hanske, J.; Chun, F.K.; Kibel, A.S.; Lipsitz, S.R.; Sun, M.; et al. The association of hypoalbuminemia with early perioperative—A comprehensive assessment across 16 major procedures. Am. J. Surg. 2017, 214, 871–883. [Google Scholar] [CrossRef] [PubMed]
- Lyons, O.; Whelan, B.; Bennett, K.; O’Riordan, D.; Silke, B. Serum albumin as an outcome predictor in hospital emergency medical admissions. Eur. J. Intern. Med. 2010, 21, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L.; Dubois, M.-J.; Navickis, R.J.; Wilkes, M.M. Hypoalbuminemia in acute illness: Is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann. Surg. 2003, 237, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Chewcharat, A.; Mao, M.A.; Thirunavukkarasu, S.M.; Kashani, K.B. Risk of acute respiratory failure among hospitalized patients with various admission serum albumin levels: A cohort study. Medicine 2020, 99, e19352. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Alekh, K.; Mathew, J.; Azam, H.; Alfakir, M.; DeBari, V.; Khan, M. Hypoalbuminemia and Length of Mechanical Ventilation in ARDS. Chest 2011, 140, 200A. [Google Scholar] [CrossRef]
- Álvares-Da-Silva, M.R.; da Silveira, T.R. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition 2005, 21, 113–117. [Google Scholar] [CrossRef]
- Schiesser, M.; Kirchhoff, P.; Müller, M.K.; Schäfer, M.; Clavien, P.-A. The correlation of nutrition risk index, nutrition risk score, and bioimpedance analysis with postoperative complications in patients undergoing gastrointestinal surgery. Surgery 2009, 145, 519–526. [Google Scholar] [CrossRef]
- Bin, C.M.; Flores, C.; Álvares-Da-Silva, M.R.; Francesconi, C.F.M. Comparison between handgrip strength, subjective global assessment, anthropometry, and biochemical markers in assessing nutritional status of patients with Crohn’s disease in clinical remission. Dig. Dis. Sci. 2010, 55, 137–144. [Google Scholar] [CrossRef]
- Chohan, K.B.; Park, J.B.; Dales, S.R.; Varughese, R.; Wickerson, L.P.; Singer, L.G.; Stewart, B.R.; Rozenberg, D. Evaluation of Malnutrition Risk in Lung Transplant Candidates Using the Nutritional Risk Index. Transplant. Direct 2020, 6, e574. [Google Scholar] [CrossRef]
- Schweitzer, L.; Geisler, C.; Pourhassan, M.; Braun, W.; Glüer, C.-C.; Bosy-Westphal, A.; Müller, M.J. What is the best reference site for a single MRI slice to assess whole-body skeletal muscle and adipose tissue volumes in healthy adults? Am. J. Clin. Nutr. 2015, 102, 58–65. [Google Scholar] [CrossRef]
- Kelm, D.J.; Bonnes, S.L.; Jensen, M.D.; Eiken, P.W.; Hathcock, M.A.; Kremers, W.K.; Kennedy, C.C. Pre-transplant wasting (as measured by muscle index) is a novel prognostic indicator in lung transplantation. Clin. Transplant. 2016, 30, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Swaminathan, A.C.; McConnell, A.; Peskoe, S.; Bashir, M.R.; Buckley, E.B.; Frankel, C.W.; Turner, D.J.; Smith, P.J.; Zaffiri, L.; Singer, L.G.; et al. Evaluation of Frailty Measures and Short-term Outcomes After Lung Transplantation. Chest 2023, 164, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Singer, J.P.; Christie, J.D.; Diamond, J.M.; Anderson, M.A.; Benvenuto, L.A.; Gao, Y.; Arcasoy, S.M.; Lederer, D.J.; Calabrese, D.; Wang, P.; et al. Development of the Lung Transplant Frailty Scale (LT-FS). J. Heart Lung Transplant. 2023, 42, 892–904. [Google Scholar] [CrossRef] [PubMed]

| Over-All Population, n = 108 | ||
|---|---|---|
| Baseline characteristics | ||
| Age, years | 52 [43–60] | |
| Male gender, n (%) | 72 (67%) | |
| Weight, Kg | 69 [57–83] | |
| IBW, Kg | 64 [59–70] | |
| BSA, m2 | 1.84 [1.61–1.99] | |
| Admission from home, n (%) | 108 (100) | |
| Comorbidities | ||
| Arterial hypertension, n (%) | 33 (30%) | |
| Diabetes mellitus, n (%) | 19 (18%) | |
| Chronic kidney disease, n (%) | 2 (2%) |
| Over-All Population, n = 108 | ||
|---|---|---|
| Nutritional indexes | ||
| BMI, kg/m2 | 23 [21–27] | |
| Underweight, <18.50 kg/m2 | 12 (11%) | |
| normal weight, 18.50–24.90 kg/m2 | 59 (55%) | |
| Overweight, >30.00 kg/m2 | 37 (34%) | |
| albumin, g/L | 39 [36–42] | |
| <35 g/L | 18 (17%) | |
| 35–55 g/L | 90 (83%) | |
| prealbumin, mg/L | 232 [186–276] | |
| PNI | 50 [4–54] | |
| PNI-high group, >50 | 52 (48%) | |
| PNI-low group, <50 | 56 (52%) | |
| MNA-SF score | 13 [12–14] | |
| MNA-SF < 7, malnourished | 3 (3%) | |
| MNA-SF 8–11, risk of Malnutrition | 23 (21%) | |
| MNA-SF > 12, normal nutritional status | 82 (76%) | |
| Muscular indexes | ||
| CHI, % | 80 [59–100] | |
| muscular density, Hu | 36.90 [31.80–41.30] | |
| SMI, cm2/BSA | 36.50 [31.70–40.80] | |
| sarcopenia, n (%) | 14 (17) |
| Over-All Population, n = 108 | |
|---|---|
| Invasive mechanical ventilation, hours | 33 [21–96] |
| Re-intubation, n (%) | 17 (16%) |
| Tracheostomy, n (%) | 32 (30%) |
| ICU stay, days | 9 [6–21] |
| Hospital stay, days | 33 [28–46] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Congedi, S.; Boscolo, A.; Nardelli, M.; Biscaro, M.; Legnaro, C.; Sella, N.; Fichera, G.; Giacon, T.A.; Zanon, P.; Lovison, D.; et al. Nutritional and Sarcopenia Assessment in Bilateral Lung Transplantation Recipient: Can “The Strongest One” Expect Improved Short-Term Outcomes? Transplantology 2023, 4, 218-229. https://doi.org/10.3390/transplantology4040021
Congedi S, Boscolo A, Nardelli M, Biscaro M, Legnaro C, Sella N, Fichera G, Giacon TA, Zanon P, Lovison D, et al. Nutritional and Sarcopenia Assessment in Bilateral Lung Transplantation Recipient: Can “The Strongest One” Expect Improved Short-Term Outcomes? Transplantology. 2023; 4(4):218-229. https://doi.org/10.3390/transplantology4040021
Chicago/Turabian StyleCongedi, Sabrina, Annalisa Boscolo, Marco Nardelli, Martina Biscaro, Christian Legnaro, Nicolò Sella, Giulia Fichera, Tommaso Antonio Giacon, Paola Zanon, Davide Lovison, and et al. 2023. "Nutritional and Sarcopenia Assessment in Bilateral Lung Transplantation Recipient: Can “The Strongest One” Expect Improved Short-Term Outcomes?" Transplantology 4, no. 4: 218-229. https://doi.org/10.3390/transplantology4040021
APA StyleCongedi, S., Boscolo, A., Nardelli, M., Biscaro, M., Legnaro, C., Sella, N., Fichera, G., Giacon, T. A., Zanon, P., Lovison, D., Bassi, M., Borrelli, B. M., Lorenzoni, G., Giraudo, C., Gregori, D., Rea, F., & Navalesi, P. (2023). Nutritional and Sarcopenia Assessment in Bilateral Lung Transplantation Recipient: Can “The Strongest One” Expect Improved Short-Term Outcomes? Transplantology, 4(4), 218-229. https://doi.org/10.3390/transplantology4040021









