IOL Power Calculation in an Unusual Long Fellow Eye: A Case Report
Abstract
:1. Introduction
2. Case Presentation
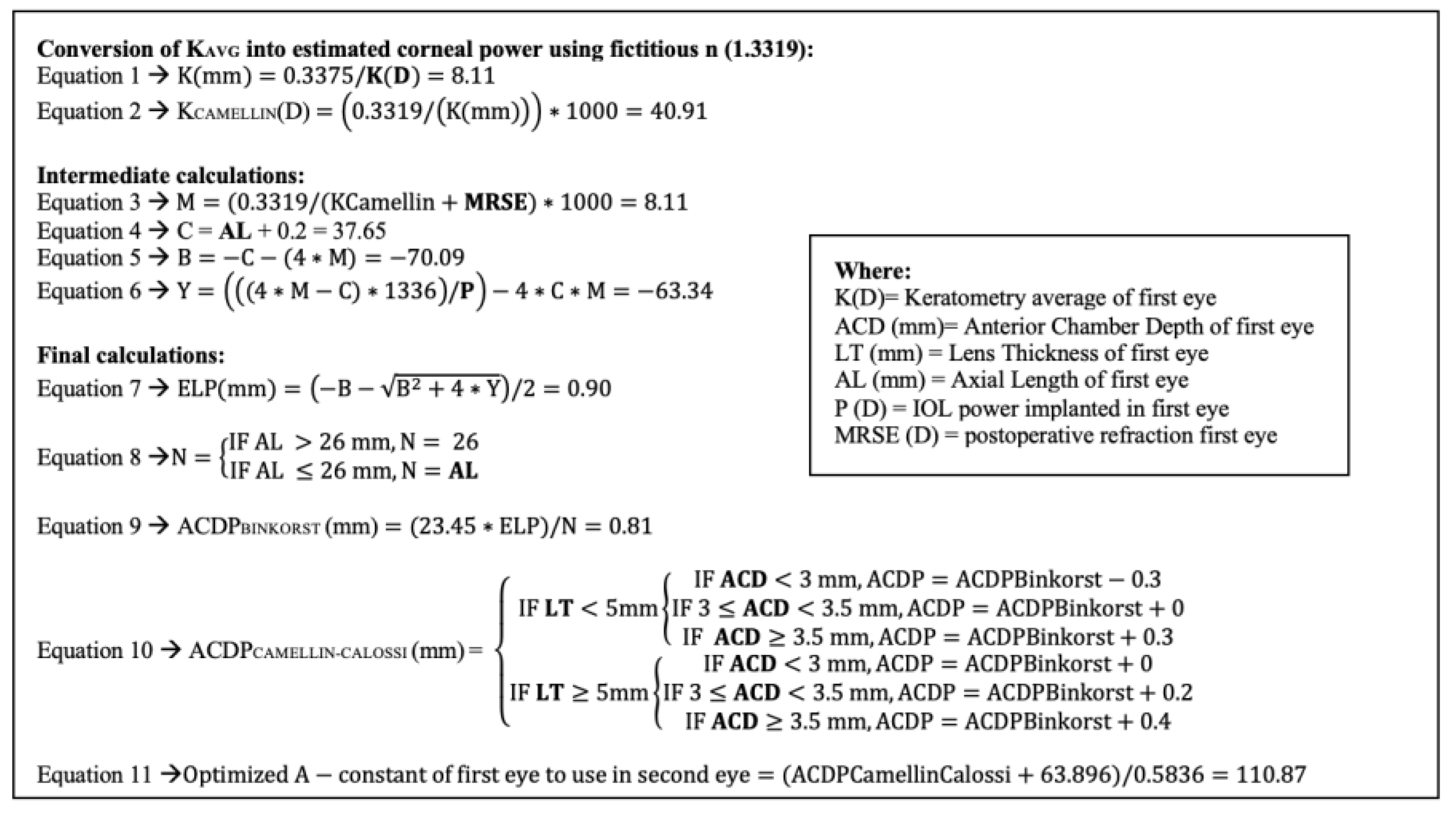
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kane, J.X.; Van Heerden, A.; Atik, A.; Petsoglou, C. Intraocular lens power formula accuracy: Comparison of 7 formulas. J. Cataract. Refract. Surg. 2016, 42, 1490–1500. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Xu, M.; Mo, E.; Huang, S.; Qi, X.; Gu, S.; Sun, W.; Su, Q.; Li, J.; Zhao, Y.-E. Accuracy of Newer Generation IOL Power Calculation Formulas in Eyes with High Axial Myopia. J. Refract. Surg. 2021, 37, 754–758. [Google Scholar] [CrossRef] [PubMed]
- Savini, G.; Taroni, L.; Hoffer, K.J. Recent developments in intraocular lens power calculation methods—Update 2020. Ann. Transl. Med. 2020, 8, 1553. [Google Scholar] [CrossRef] [PubMed]
- Haigis, W.; Lege, B.; Miller, N.; Schneider, B. Comparison of immersion ultrasound biometry and partial coherence interferometry for intraocular lens calculation according to Haigis. Graefe Arch. Clin. Exp. Ophthalmol. 2000, 238, 765–773. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Koch, D.D. Modified axial length adjustment formulas in long eyes. J. Cataract. Refract. Surg. 2018, 44, 1396–1397. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Holladay, J.T.; Koch, D.D. Wang-Koch axial length adjustment for the Holladay 2 formula in long eyes. J. Cataract. Refract. Surg. 2018, 44, 1291–1292, Erratum in J. Cataract. Refract. Surg. 2019, 45, 117. [Google Scholar] [CrossRef] [PubMed]
- Suto, C.; Shimamura, E.; Watanabe, I. Comparison of 2 optical biometers and evaluation of the Camellin-Calossi intraocular lens formula for normal cataractous eyes. J. Cataract. Refract. Surg. 2015, 41, 2366–2372. [Google Scholar] [CrossRef] [PubMed]
- Chylack, L.T., Jr.; Wolfe, J.K.; Singer, D.M.; Leske, M.C.; Bullimore, M.A.; Bailey, I.L.; Friend, J.; McCarthy, D.; Wu, S.Y. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch. Ophthalmol. 1993, 111, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Barrett II Formula. Available online: https://calc.apacrs.org/barrett_universal2105/ (accessed on 1 September 2021).
- Camellin, M.; Calossi, A. A New Formula for Intraocular Lens Power Calculation After Refractive Corneal Surgery. J. Refract. Surg. 2006, 22, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Aristodemou, P.; Cartwright, N.E.K.; Sparrow, J.M.; Johnston, R.L. Intraocular lens formula constant optimization and partial coherence interferometry biometry: Refractive outcomes in 8108 eyes after cataract surgery. J. Cataract. Refract. Surg. 2011, 37, 50–62. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Merriam, J.C. A Method to Improve the Accuracy of Optimized A-Constant for IOL Calculation Formulas. J. Clin. Exp. Ophthalmol. 2018, 9, 1–3. [Google Scholar] [CrossRef]
- Aristodemou, P.; Knox Cartwright, N.E.; Sparrow, J.M.; Johnston, R.L. First eye prediction error improves second eye refractive outcome results in 2129 patients after bilateral sequential cataract surgery. Ophthalmology 2011, 118, 1701–1709. [Google Scholar] [CrossRef] [PubMed]
- Turnbull, A.M.J.; Barrett, G.D. Using the first-eye prediction error in cataract surgery to refine the refractive outcome of the second eye. J. Cataract. Refract. Surg. 2019, 45, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Debellemanière, G.; Dubois, M.; Gauvin, M.; Wallerstein, A.; Brenner, L.F.; Rampat, R.; Saad, A.; Gatinel, D. The PEARL-DGS Formula: The Development of an Open-source Machine Learning–based Thick IOL Calculation Formula. Am. J. Ophthalmol. 2021, 232, 58–69. [Google Scholar] [CrossRef] [PubMed]
| Data | Right Eye | Left Eye |
|---|---|---|
| MRSE (D) | −24.75 | −23 |
| CDVA (logMAR) | 0.2 | 0.2 |
| Kavg (D) | 41.21 | 41.61 |
| ACD (mm) | 3.07 | 3.16 |
| LT (mm) | 4.30 | 4.25 |
| AL (mm) | 39.42 | 37.45 |
| CCT (μm) | 551 | 556 |
| WTW (mm) | 12.12 | 12.06 |
| Constant A | 118.7 | 118.7 |
| IOL Formula | Right Eye | Left Eye |
|---|---|---|
| Barrett (limit AL = 38 mm) * | N/A | −6 D (target: +0.23) |
| Kane (limit AL = 35 mm) * | N/A | N/A |
| EVO (limit AL = 38 mm) * | N/A | −7 (target: +0.23) |
| Pearl DGS formula (limit AL = 40 mm) * | −10 D (target: −3.06) | −10 D (target: −1.60) |
| Hoffer QST (limit AL = 32 mm) * | N/A | N/A |
| Panacea (limit AL = 36 mm) | N/A | N/A |
| Camellin-Calossi formula for virgin eye | −10.16 D (target: 0) | −8.29 D (target: 0) |
| SRK/T | −9.97 D (target: 0) | −8.18 D (target: 0) |
| Right Eye (Fellow Eye) | Left Eye (First Eye) | |
|---|---|---|
| IOL power implanted (D) Postoperative MRSE (D) CDVA (logMAR) | −8 | −6 |
| +0.25 | 0 | |
| 0.1 | 0.1 | |
| Second eye calculation (Pearl DGS formula) * Second eye calculation (Optimized A-constant method using the Camellin-Calossi formula) (D) | N/A | |
| −7.43 (target: 0 D) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camellin, U.; Franchina, F.; Meduri, A.; Aragona, P. IOL Power Calculation in an Unusual Long Fellow Eye: A Case Report. Optics 2023, 4, 396-401. https://doi.org/10.3390/opt4030029
Camellin U, Franchina F, Meduri A, Aragona P. IOL Power Calculation in an Unusual Long Fellow Eye: A Case Report. Optics. 2023; 4(3):396-401. https://doi.org/10.3390/opt4030029
Chicago/Turabian StyleCamellin, Umberto, Francesco Franchina, Alessandro Meduri, and Pasquale Aragona. 2023. "IOL Power Calculation in an Unusual Long Fellow Eye: A Case Report" Optics 4, no. 3: 396-401. https://doi.org/10.3390/opt4030029
APA StyleCamellin, U., Franchina, F., Meduri, A., & Aragona, P. (2023). IOL Power Calculation in an Unusual Long Fellow Eye: A Case Report. Optics, 4(3), 396-401. https://doi.org/10.3390/opt4030029







