Improving Zirconia–Resin Cement Bonding Through Laser Surface Texturing: A Comparative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Scanning Electron Microscopy (SEM) and White Light Interferometry (WLI)
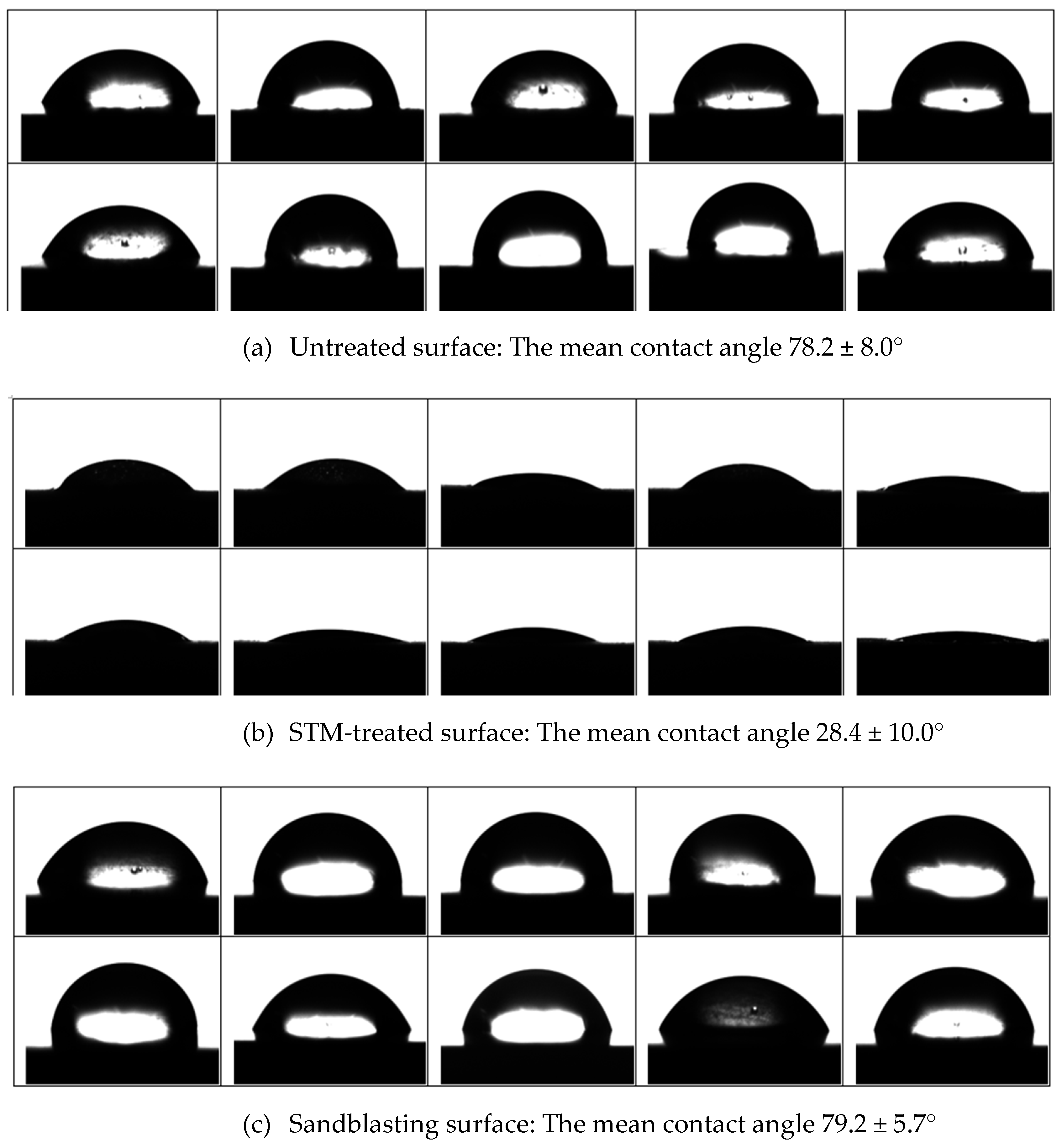
2.2. Surface Contact Angle Measurement Experiment
2.3. SBS Test
3. Results
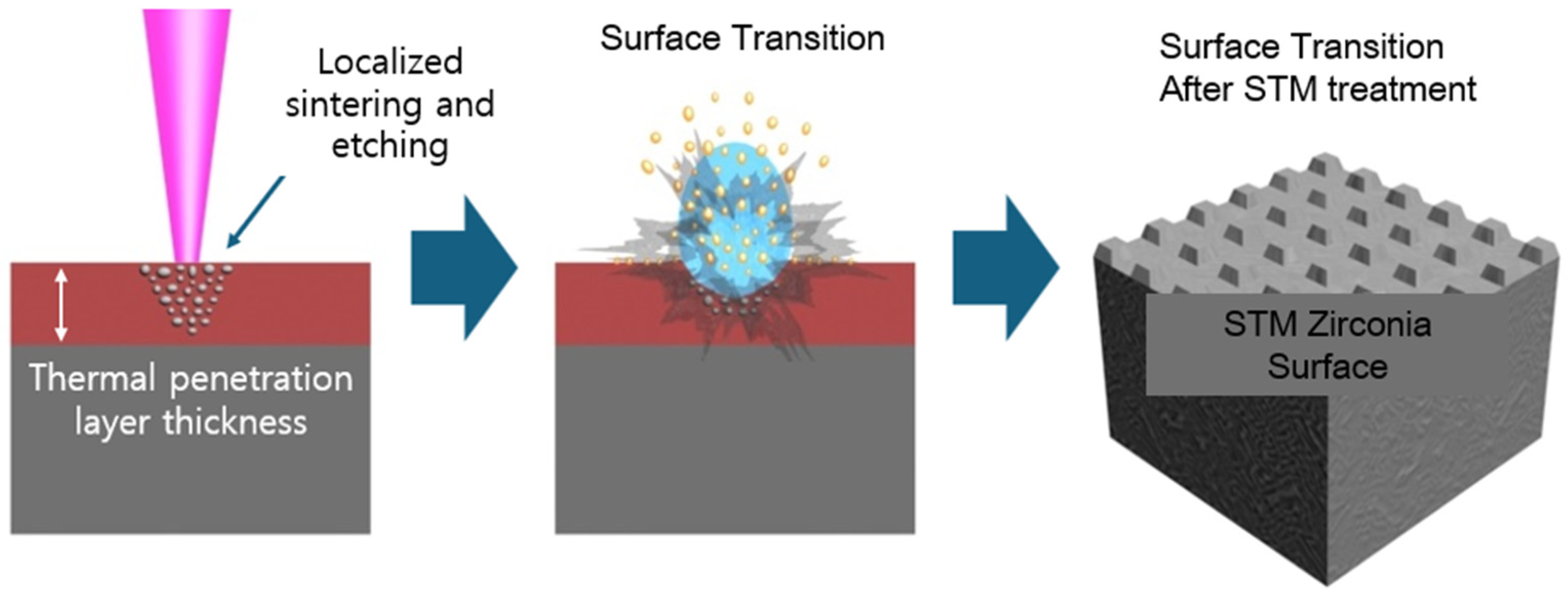
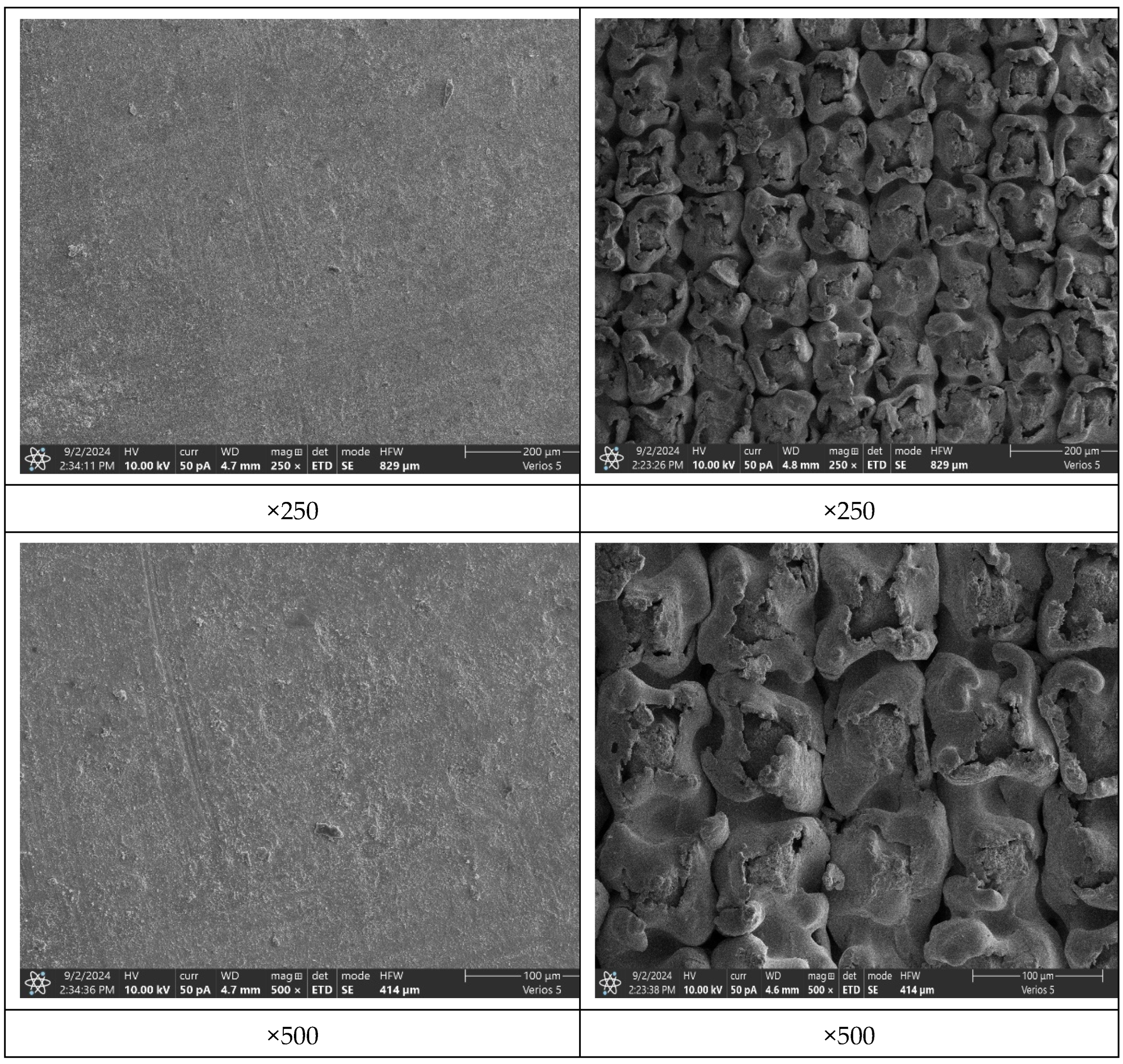
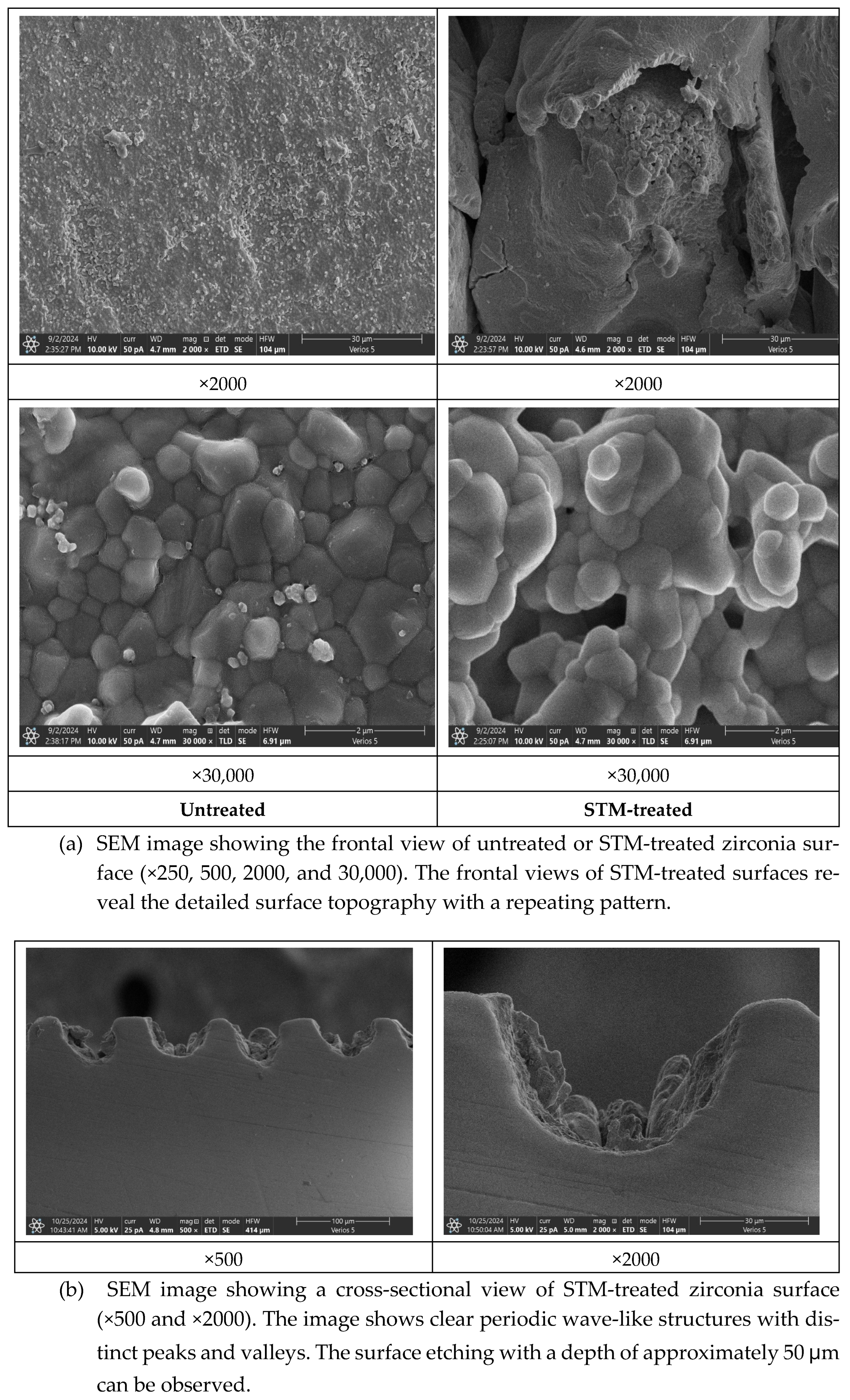
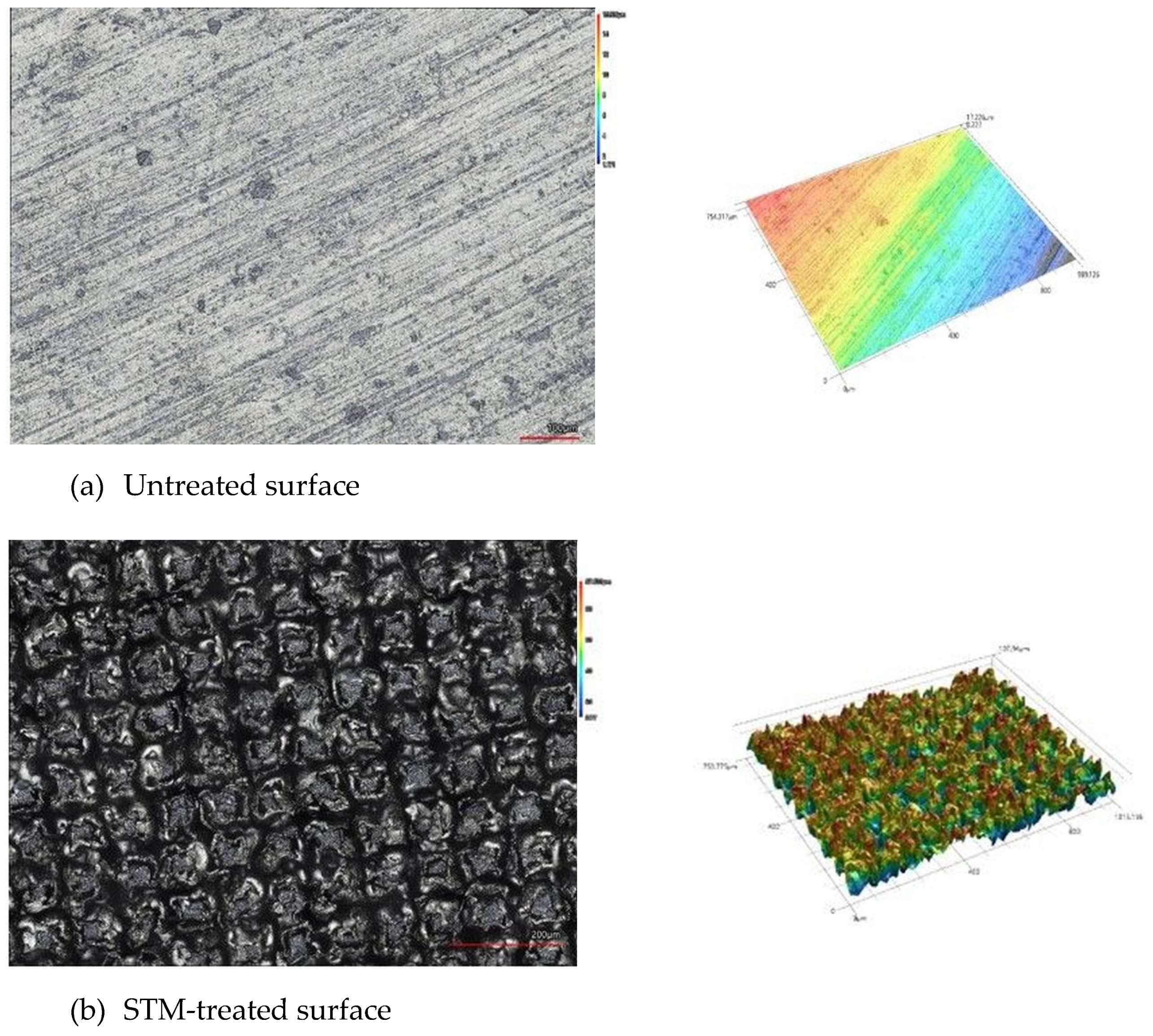
3.1. SEM and WLI Analyses
3.2. Surface Contact Angle Analyses
3.3. SBS Test
4. Discussion
5. Conclusions
6. Patents
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MDP | 10-Methacryloyloxydecyl dihydrogen phosphate |
| LST | Laser Surface Texturing |
| STM | Surface Transition Machine |
| SBS | Shear bond strength |
References
- Sulaiman, T.A.; Suliman, A.A.; Abdulmajeed, A.A.; Zhang, Y. Zirconia restoration types, properties, tooth preparation design, and bonding. A narrative review. J. Esthet. Restor. Dent. 2024, 36, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Gautam, C.; Joyner, J.; Gautam, A.; Rao, J.; Vajtai, R. Zirconia Based Dental Ceramics: Structure, Mechanical Properties, Biocompatibility and Applications. Dalton Trans. 2016, 45, 19194–19215. [Google Scholar] [CrossRef] [PubMed]
- Harada, K.; Shinya, A.; Yokoyama, D.; Shinya, A. Effect of Loading Conditions on the Fracture Toughness of Zirconia. J. Prosthodont. Res. 2013, 57, 82–87. [Google Scholar] [CrossRef]
- Piconi, C.; Maccauro, G. Zirconia as a Ceramic Biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.; Bonfante, E.A. A New Classification System for All-Ceramic and Ceramic-Like Restorative Materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef]
- Al-Amari, A.S.; Saleh, M.S.; Albadah, A.A.; Almousa, A.A.; Mahjoub, W.K.; Al-Otaibi, R.M.; Alanazi, E.M.; Alshammari, A.K.; Malki, A.T.; Alghelaiqah, K.F.; et al. A Comprehensive Review of Techniques for Enhancing Zirconia Bond Strength: Current Approaches and Emerging Innovations. Cureus 2024, 16, e70893. [Google Scholar] [CrossRef] [PubMed]
- Dbradovic-Djuricic, K.; Medic, V.; Dodic, S.; Gavrilov, D.; Antonijevic, D.; Zrilic, M. Dilemmas in Zirconia Bonding: A Review. Srp. Arh. Celok. Lek. 2013, 141, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Karami Zarandi, P.; Madani, A.; Bagheri, H.; Moslemion, M. The Effect of Sandblasting and Coating of Zirconia by Nano Composites on Bond Strength of Zirconia to Resin Cements. J. Dent. 2020, 21, 63–68. [Google Scholar] [CrossRef]
- Su, N.; Yue, L.; Liao, Y.; Liu, W.; Zhang, H.; Li, X.; Wang, H.; Shen, J. The Effect of Various Sandblasting Conditions on Surface Changes of Dental Zirconia and Shear Bond Strength between Zirconia Core and Indirect Composite Resin. J. Adv. Prosthodont. 2015, 7, 214–223. [Google Scholar] [CrossRef]
- Chen, Y.; Lu, Z.; Qian, M.; Zhang, H.; Xie, H.; Chen, C. Effect of 10-Methacryloxydecyl Dihydrogen Phosphate Concentration on Chemical Coupling of Methacrylate Resin to Yttria-Stabilized Zirconia. J. Adhes. Dent. 2017, 19, 349–355. [Google Scholar] [CrossRef]
- Limpuangthip, N.; Surintanasarn, A.; Vitavaspan, P. Mechanical and Chemical Surface Treatment Enhances Bond Strength between Zirconia and Orthodontic Brackets: An in Vitro Study. BDJ Open 2023, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Koko, M.; Takagaki, T.; Abdou, A.; Wada, T.; Nikaido, T.; Tagami, J. Influence of 10-methacryloyloxydecyl dihydrogen phosphate (MDP) incorporated experimental cleaners on the bonding performance of saliva-contaminated zirconia ceramic. Clin. Oral. Investig. 2022, 26, 1785–1795. [Google Scholar] [CrossRef] [PubMed]
- Abdou, A.; Hussein, N.; Kusumasari, C.; Abo-Alazm, E.A.; Rizk, A. Alumina and glass-bead blasting effect on bond strength of zirconia using 10-methacryloyloxydecyl dihydrogen phosphate (MDP) containing self-adhesive resin cement and primers. Sci. Rep. 2023, 13, 19127. [Google Scholar] [CrossRef]
- Moradi, Z.; Akbari, F.; Valizadeh, S. Effects of Universal Adhesive on Shear Bond Strength of Resin Cement to Zirconia Ceramic with Different Surface Treatments. Int. J. Dent. 2021, 5517382. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Yoo, K.W.; Kim, S.J.; Jung, C.H. Phase Transformations and Subsurface Changes in Three Dental Zirconia Grades after Sandblasting with Various Al2O3 Particle Sizes. Materials 2021, 14, 5321. [Google Scholar] [CrossRef]
- Chintapalli, R.K.; Mestra Rodriguez, A.; Garcia Marro, F.; Anglada, M. Effect of sandblasting and residual stress on strength of zirconia for restorative dentistry applications. J. Mech. Behav. Biomed. Mater. 2014, 29, 126–137. [Google Scholar] [CrossRef]
- He, M.; Zhang, Z.; Zheng, D.; Ding, N.; Liu, Y. Effect of sandblasting on surface roughness of zirconia-based ceramics and shear bond strength of veneering porcelain. Dent. Mater. J. 2014, 33, 778–785. [Google Scholar] [CrossRef]
- Tomanik, M.; Kobielarz, M.; Filipiak, J.; Szymonowicz, M.; Rusak, A.; Mroczkowska, K.; Antonczak, A.; Pezowicz, C. Laser Texturing as a Way of Influencing the Micromechanical and Biological Properties of the Poly(L-Lactide) Surface. Materials 2020, 13, 3786. [Google Scholar] [CrossRef]
- Henriques, B.; Fabris, D.; Souza, J.C.M.; Silva, F.S.; Carvalho, O.; Fredel, M.C.; Mesquita-Guimaraes, J. Bond strength enhancement of zirconia-porcelain interfaces via Nd:YAG laser surface structuring. J. Mech. Behav. Biomed. Mater. 2018, 81, 161–167. [Google Scholar] [CrossRef]
- Iwaguro, S.; Shimoe, S.; Hirata, I.; Murayama, T.; Satoda, T. Effect of microslit retention on the bond strength of zirconia to dental materials. Dent. Mater. J. 2019, 38, 1043–1052. [Google Scholar] [CrossRef] [PubMed]
- Carek, A.; Slokar Benic, L.; Komar, D.; Krebelj, E. Roughness of the Surface of Zirconia Reinforced Lithium Disilicate Ceramic Treated by Different Procedures. Materials 2022, 16, 265. [Google Scholar] [CrossRef] [PubMed]
- Grigore, A.; Spallek, S.; Petschelt, A.; Butz, B.; Spiecker, E.; Lohbauer, U. Microstructure of veneered zirconia after surface treatments: A TEM study. Dent. Mater. 2013, 29, 1098–1107. [Google Scholar] [CrossRef] [PubMed]
- Sismanoglu, S.; Yildirim-Bilmez, Z.; Erten-Taysi, A.; Ercal, P. Influence of different surface treatments and universal adhesives on the repair of CAD-CAM composite resins: An in vitro study. J. Prosthet. Dent. 2020, 124, 238. [Google Scholar] [CrossRef] [PubMed]
- Ismail, A.M.; Bourauel, C.; ElBanna, A.; Salah Eldin, T. Micro versus Macro Shear Bond Strength Testing of Dentin-Composite Interface Using Chisel and Wireloop Loading Techniques. Dent. J. 2021, 9, 140. [Google Scholar] [CrossRef] [PubMed]
- Yue, X.; Hou, X.; Gao, J.; Bao, P.; Shen, J. Effects of MDP-based primers on shear bond strength between resin cement and zirconia. Exp. Ther. Med. 2019, 17, 3564–3572. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.J.; Yu, M.K.; Lee, K.W. The effect of continuous application of MDP-containing primer and luting resin cement on bond strength to tribochemical silica-coated Y-TZP. Restor. Dent. Endod. 2018, 43, e19. [Google Scholar] [CrossRef]
- Ahn, J.S.; Yi, Y.A.; Lee, Y.; Seo, D.G. Shear Bond Strength of MDP-Containing Self-Adhesive Resin Cement and Y-TZP Ceramics: Effect of Phosphate Monomer-Containing Primers. BioMed Res. Int. 2015, 2015, 389234. [Google Scholar] [CrossRef]
- Han, J.; Zhang, F.; Van Meerbeek, B.; Vleugels, J.; Braem, A.; Castagne, S. Laser surface texturing of zirconia-based ceramics for dental applications: A review. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 123, 112034. [Google Scholar] [CrossRef] [PubMed]
- Cunha, W.; Carvalho, O.; Henriques, B.; Silva, F.S.; Ozcan, M.; Souza, J.C.M. Surface modification of zirconia dental implants by laser texturing. Lasers Med. Sci. 2022, 37, 77–93. [Google Scholar] [CrossRef]
- Noda, M.; Okuda, Y.; Tsuruki, J.; Minesaki, Y.; Takenouchi, Y.; Ban, S. Surface damages of zirconia by Nd:YAG dental laser irradiation. Dent. Mater. J. 2010, 29, 536–541. [Google Scholar] [CrossRef]
- Andrei, A.D.; Constantin, C.A.; Tabitha, A.L.; Anca, J. Zirconia single retainer fixed dental prostheses for the posterior region-A novel preparation technique and literature review. Clin. Case Rep. 2024, 12, e9460. [Google Scholar] [CrossRef]

| Treatment Group | N | Mean + Standard Deviation (MPa) |
|---|---|---|
| G-SB | 10 | 9.8 ± 3.7 a |
| G-SB+P | 10 | 30.1 ± 3.1 b |
| G-STM | 10 | 43.4 ± 4.3 c |
| G-STM+P | 10 | 46.3 ± 8.3 c |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, J.-Y. Improving Zirconia–Resin Cement Bonding Through Laser Surface Texturing: A Comparative Study. Prosthesis 2025, 7, 19. https://doi.org/10.3390/prosthesis7010019
Yoon J-Y. Improving Zirconia–Resin Cement Bonding Through Laser Surface Texturing: A Comparative Study. Prosthesis. 2025; 7(1):19. https://doi.org/10.3390/prosthesis7010019
Chicago/Turabian StyleYoon, Ji-Young. 2025. "Improving Zirconia–Resin Cement Bonding Through Laser Surface Texturing: A Comparative Study" Prosthesis 7, no. 1: 19. https://doi.org/10.3390/prosthesis7010019
APA StyleYoon, J.-Y. (2025). Improving Zirconia–Resin Cement Bonding Through Laser Surface Texturing: A Comparative Study. Prosthesis, 7(1), 19. https://doi.org/10.3390/prosthesis7010019







