Adaptation Skills and Temporomandibular Joint Neutrality: A Case Report of a Failed Orthognathic Surgery Intervention
Abstract
1. Introduction
2. Case Report
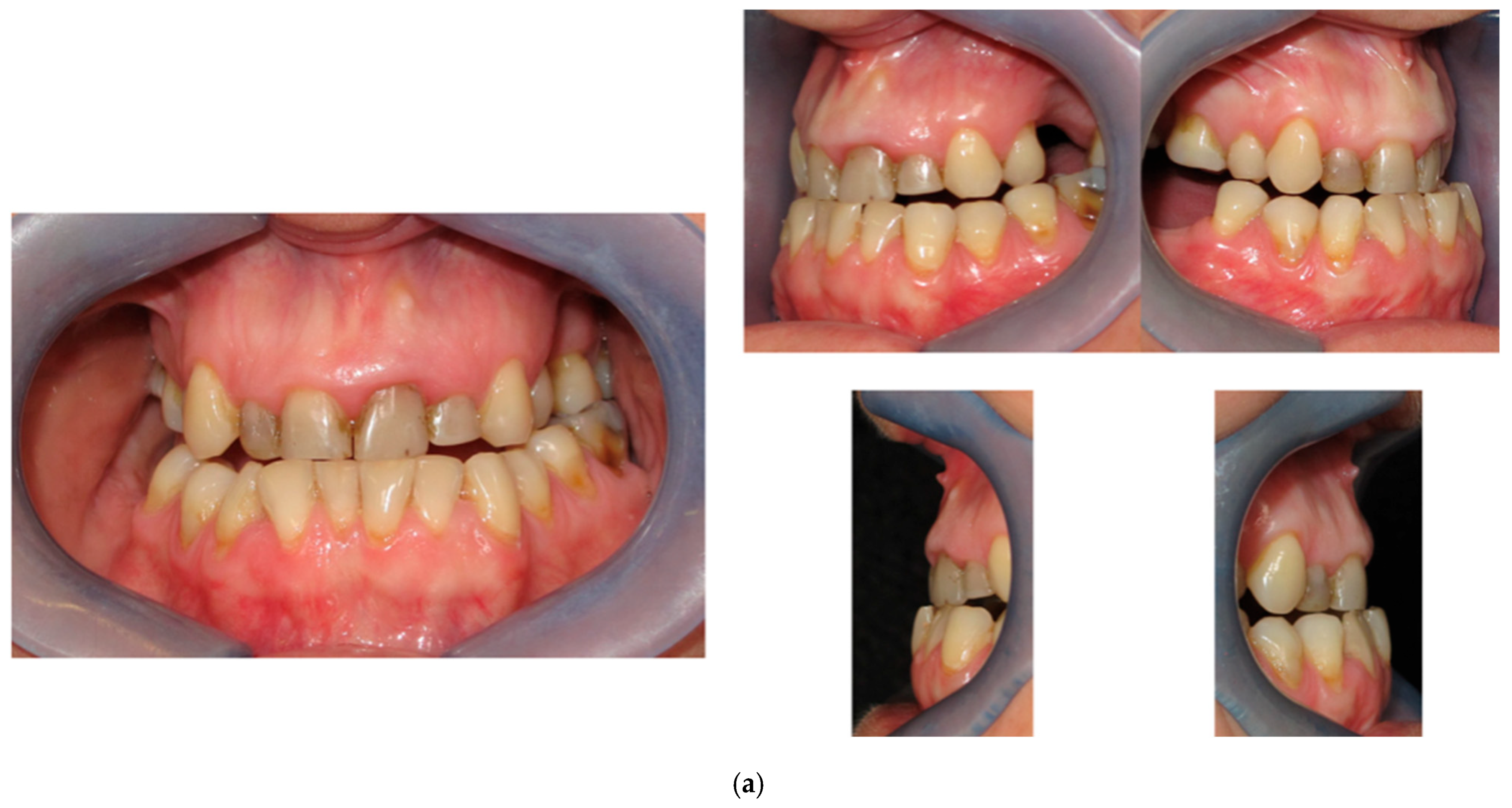
2.1. Patient’s Complaint
2.2. Case History
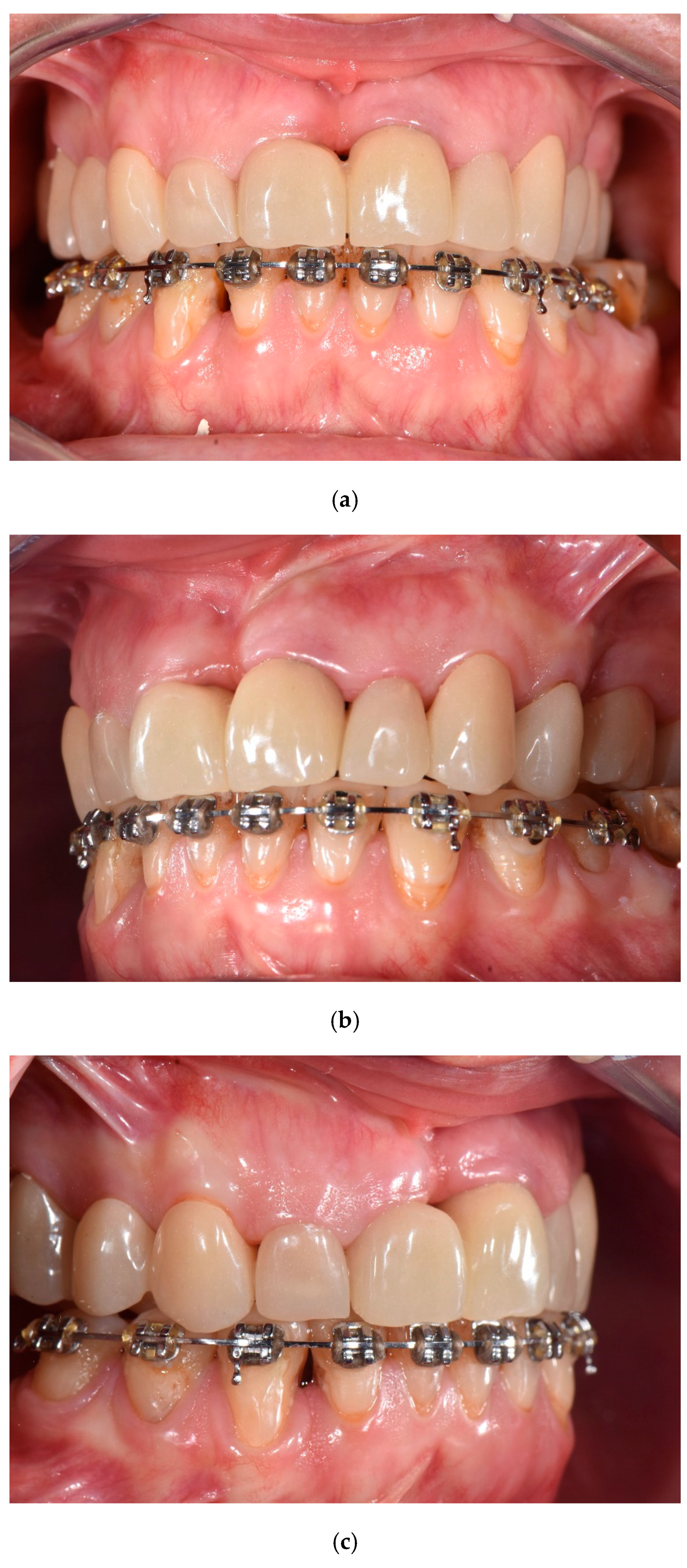
2.3. Prosthetic Phase
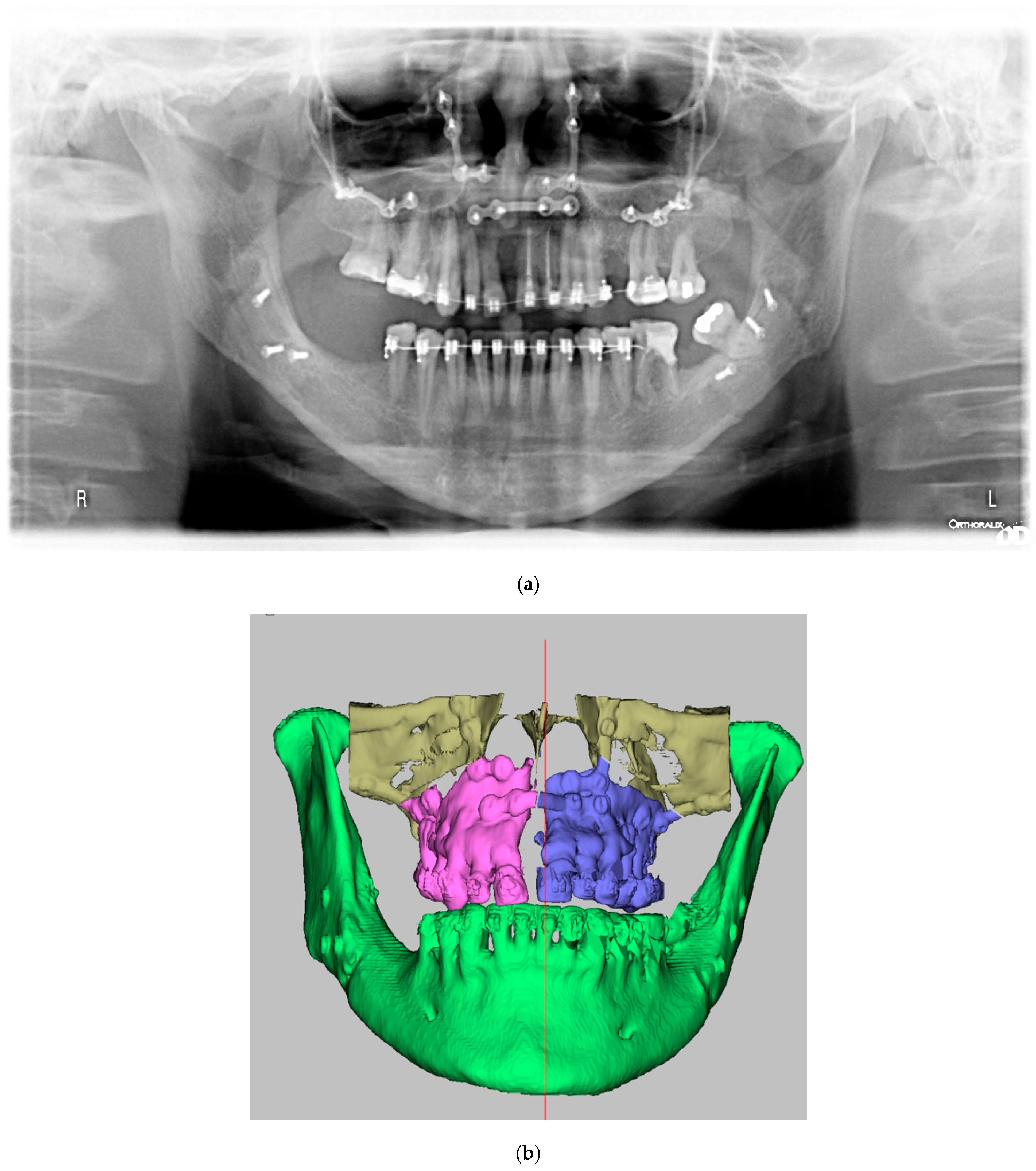
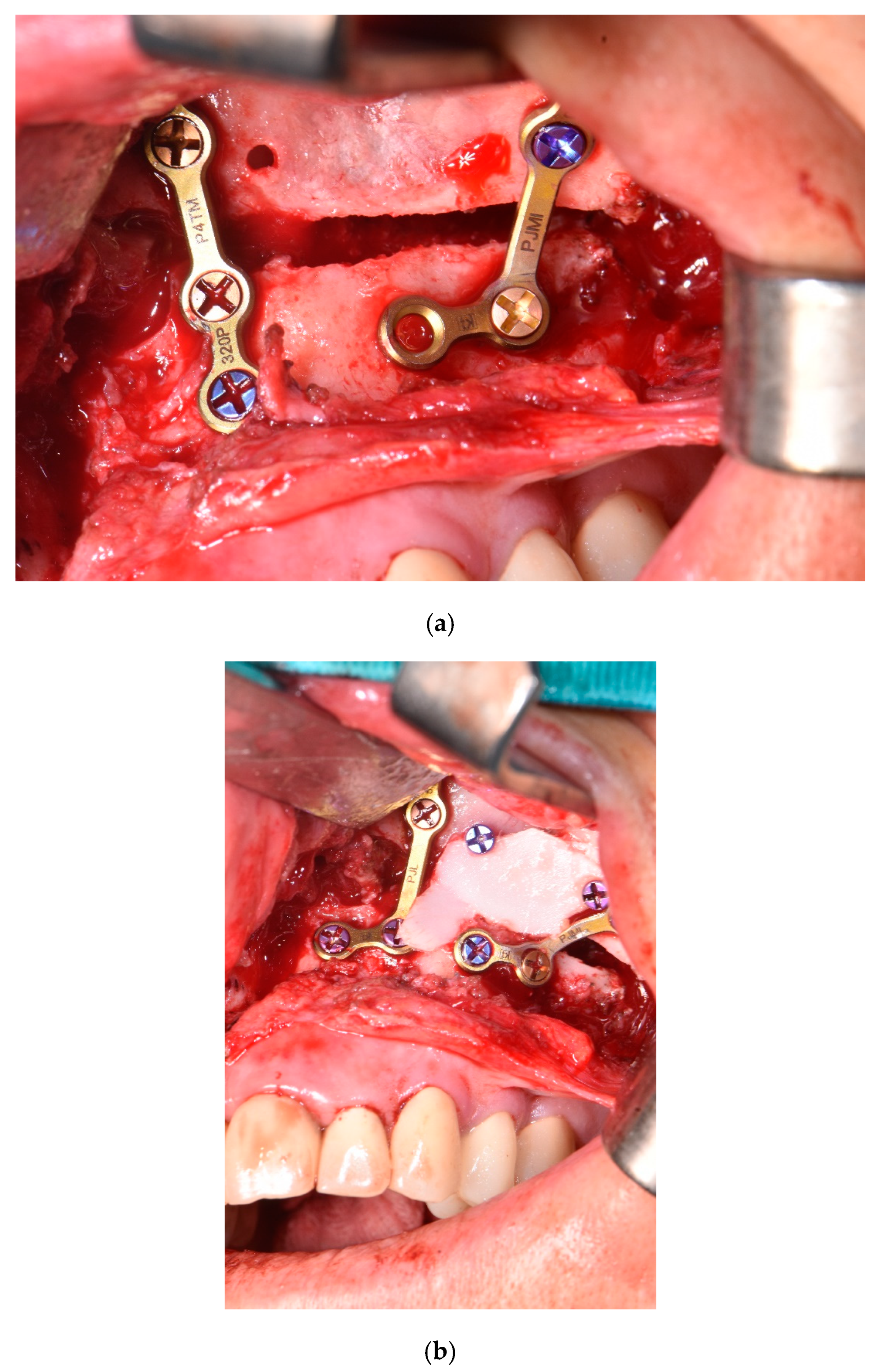
2.4. Surgical Phase
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zheng, Z.; Hasebe, D.; Suda, D.; Saito, N.; Saito, D.; Nihara, J.; Nohno, K.; Saito, I.; Kobayashi, T. Investigation of orthognathic surgery indicators-combination with index of orthognathic functional treatment needs (IOFTN) and maxillofacial morphometric analysis. Oral. Maxillofac. Surg. 2024, 28, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Weiss, R.O., 2nd; Ong, A.A.; Reddy, L.V.; Bahmanyar, S.; Vincent, A.G.; Ducic, Y. Orthognathic Surgery-LeFort I Osteotomy. Facial Plast. Surg. 2021, 37, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Leck, R.; Paul, N.; Rolland, S.; Birnie, D. The consequences of living with a severe malocclusion: A review of the literature. J. Orthod. 2022, 49, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Steinhäuser, E.W. Historical development of orthognathic surgery. J. Craniomaxillofac. Surg. 1996, 24, 195–204. [Google Scholar] [CrossRef]
- Almadi, D.; Benington, P.; Ju, X.; Ayoub, A. Reproducibility and reliability of digital occlusal planning for orthognathic surgery. Int. J. Oral. Maxillofac. Surg. 2023, 52, 1074–1080. [Google Scholar] [CrossRef]
- Friedrich, C.; Graw, C.; Kröplin, J. A narrative review of present knowledge and digital approaches in orthognathic surgery. Innov. Surg. Sci. 2024, 9, 175–179. [Google Scholar] [CrossRef]
- Alkaabi, S.; Maningky, M.; Helder, M.N.; Alsabri, G. Virtual and traditional surgical planning in orthognathic surgery—Systematic review and meta-analysis. Br. J. Oral. Maxillofac. Surg. 2022, 60, 1184–1191. [Google Scholar] [CrossRef]
- Benington, P.; Anwar, M.; Mohan, A.; Gillgrass, T.; Ayoub, A. Outcome measures of the surgery first approach for orthognathic correction of dentofacial deformities. Br. J. Oral. Maxillofac. Surg. 2024, 62, 71–75. [Google Scholar] [CrossRef]
- Kim, Y.K. Complications associated with orthognathic surgery. J. Korean Assoc. Oral. Maxillofac. Surg. 2017, 43, 3–15. [Google Scholar] [CrossRef]
- Klein, K.P.; Kaban, L.B.; Masoud, M.I. Orthognathic Surgery and Orthodontics: Inadequate Planning Leading to Complications or Unfavorable Results. Oral. Maxillofac. Surg. Clin. North. Am. 2020, 32, 71–82. [Google Scholar] [CrossRef]
- Ferri, J.; Druelle, C.; Schlund, M.; Bricout, N.; Nicot, R. Complications in orthognathic surgery: A retrospective study of 5025 cases. Int. Orthod. 2019, 17, 789–798. [Google Scholar] [CrossRef]
- Takahara, N.; Tomomatsu, N.; Kimura, A.; Kosugi, M.; Kurasawa, Y.; Morita, K.I.; Yoda, T. Changes in the condylar volume and skeletal relapse following orthognathic surgery in patients with dentofacial deformity: A retrospective study. Cranio 2022, 4, 1–11. [Google Scholar] [CrossRef]
- Endo, S.; Niimi, K.; Kato, Y.; Nohno, K.; Hasebe, D.; Hayashi, T.; Saito, I.; Kobayashi, T. Examination of factors affecting condylar bone changes following surgical-orthodontic treatment. Cranio 2022, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lombardo, L.; Siciliani, G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: End of an era? J. Oral. Rehabil. 2017, 44, 908–923. [Google Scholar] [CrossRef]
- Manfredini, D.; Stellini, E.; Gracco, A.; Lombardo, L.; Nardini, L.G.; Siciliani, G. Orthodontics is temporomandibular disorder-neutral. Angle Orthod. 2016, 86, 649–654. [Google Scholar] [CrossRef]
- Manfredini, D. The evolution of a field: A challenge and an opportunity. Cranio 2024, 42, 251–252. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Roberts, W.E.; Goldstein, G.; Wiens, J.P. Does the Stomatognathic System Adapt to Changes in Occlusion? Best Evidence Consensus Statement. J. Prosthodont. 2020, 30(S1), 5–11. [Google Scholar] [CrossRef]
- Farrell, B.B.; Tucker, M.R. Orthognathic surgery in the office setting. Oral. Maxillofac. Surg. Clin. North. Am. 2014, 26, 611–620. [Google Scholar] [CrossRef]
- González, M.B.; Casellas, J.B.; Fernández Mondragón, M.P.; Nuño, V.C.; Amezaga, J.A.; De Carlos Villafra, F. Clinical, esthetic, and quality of life outcomes after telegnathic surgery in Caucasian OSAS patients. Cranio 2022, 40, 425–432. [Google Scholar] [CrossRef]
- Ehrmann, E.; Bernabeu, M.; Tillier, Y.; Camia, J.; Ecalle, C.; Savoldelli, C.; Charavet, C. Impact of Orthodontic-Surgical Treatments on the Signs and Symptoms of Temporomandibular Disorders: A Systematic Review. Dent. J. 2024, 12, 132. [Google Scholar] [CrossRef]
- Kandasamy, S.; Greene, C.S.; Obrez, A. An evidence-based evaluation of the concept of centric relation in the 21st century. Quintessence Int. 2018, 49, 755–760. [Google Scholar] [PubMed]
- Steel, B.J.; Cope, M.R. Unusual and rare complications of orthognathic surgery: A literature review. J. Oral. Maxillofac. Surg. 2012, 70, 1678–1691. [Google Scholar] [CrossRef]
- Akamatsu, T.; Hanai, U.; Miyasaka, M.; Muramatsu, H.; Yamamoto, S. Comparison of mandibular stability after SSRO with surgery-first approach versus conventional ortho-first approach. J. Plast. Surg. Hand Surg. 2016, 50, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Valls-Ontañón, A.; Triginer-Roig, S.; Trujillo, I.; Brabyn, P.J.; Giralt-Hernando, M.; Hernández-Alfaro, F. Three-dimensional evaluation of postoperative stability: A comparative study between surgery-first and surgery-late protocols. Int. J. Oral. Maxillofac. Surg. 2023, 52, 353–360. [Google Scholar] [CrossRef]
- Marion, F.; Mercier, J.M.; Odri, G.A.; Perrin, J.P.; Longis, J.; Kün-Darbois, J.D.; Corre, P.; Bertin, H. Associated relapse factors in Le Fort I osteotomy. A retrospective study of 54 cases. J. Stomatol. Oral. Maxillofac. Surg. 2019, 120, 419–427. [Google Scholar] [CrossRef]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. Orthognathic surgery: A hierarchy of stability. Int. J. Adult Orthodon Orthognath. Surg. 1996, 11, 191–204. [Google Scholar]
- Liebregts, J.; Baan, F.; van Lierop, P.; de Koning, M.; Bergé, S.; Maal, T.; Xi, T. One-year postoperative skeletal stability of 3D planned bimaxillary osteotomies: Maxilla-first versus mandible-first surgery. Sci. Rep. 2019, 9, 3000. [Google Scholar] [CrossRef]
- Thiem, D.G.; Schneider, D.; Hammel, M.; Saka, B.; Frerich, B.; Al-Nawas, B.; Kämmerer, P.W. Complications or rather side effects? Quantification of patient satisfaction and complications after orthognathic surgery–A retrospective, cross-sectional long-term analysis. Clin. Oral. Investig. 2021, 25, 3315–3327. [Google Scholar] [CrossRef]
- Alrashidi, H.A.; Almutairi, M.H.; Almohaimeed, S.M.; Homdi, L.A.; Alharbi, A.F.; Alazmi, G.S.; Mesmeli, R.O.; Alanazi, A.M.; Muaini, S.A.; Alraddadi, K.A.; et al. Evaluating Post-surgical Stability and Relapse in Orthognathic Surgery: A Comprehensive Review. Cureus 2024, 16, e72163. [Google Scholar] [CrossRef]
- Kim, C.S.; Lee, S.C.; Kyung, H.M.; Park, H.S.; Kwon, T.G. Stability of mandibular setback surgery with and without presurgical orthodontics. J. Oral. Maxillofac. Surg. 2014, 72, 779–787. [Google Scholar] [CrossRef]
- Navarro-Fernández, G.; Bravo-Aparicio, J.; Del Castillo, J.L.; Beltran-Alacreu, H.; Gil-Martínez, A. Pre-Surgical Factors Influencing Post-Surgical Outcomes in Orthognathic Surgery Patients: A Longitudinal Study. J. Clin. Med. 2024, 13, 4445. [Google Scholar] [CrossRef] [PubMed]
- Ito, G.; Koh, M.; Fujita, T.; Shirakura, M.; Ueda, H.; Tanne, K. Factors related to stability following the surgical correction of skeletal open bite. Aust. Orthod. J. 2014, 30, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Bendor-Samuel, R.; Chen, Y.R.; Chen, P.K. Unusual complications of the Le Fort I osteotomy. Plast. Reconstr. Surg. 1995, 96, 1289–1296. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Lee, J.Y.; Yang, S.J.; Koh, K.S. The reliability of a surgery-first orthognathic approach without presurgical orthodontic treatment for skeletal class III dentofacial deformity. Ann. Plast. Surg. 2015, 74, 333–341. [Google Scholar] [CrossRef]
- Huang, C.S.; Hsu, S.S.; Chen, Y.R. Systematic review of the surgery-first approach in orthognathic surgery. Biomed. J. 2014, 37, 184–190. [Google Scholar] [CrossRef]
- Saracutu, O.I.; Pollis, M.; Cagidiaco, E.F.; Ferrari, M.; Manfredini, D. Repeatability of Teethan® indexes analysis of the masseter and anterior temporalis muscles during maximum clenching: A pilot study. Clin. Oral. Investig. 2023, 27, 5309–5316. [Google Scholar] [CrossRef]
- Moreno-Hay, I.; Okeson, J.P. Does altering the occlusal vertical dimension produce temporomandibular disorders? A literature review. J. Oral. Rehabil. 2015, 42, 875–882. [Google Scholar] [CrossRef]
- Luraschi, J.; Korgaonkar, M.S.; Whittle, T.; Schimmel, M.; Müller, F.; Klineberg, I. Neuroplasticity in the adaptation to prosthodontic treatment. J. Orofac. Pain. 2013, 27, 206–216. [Google Scholar] [CrossRef]
- Imhoff, B.; Ahlers, M.O.; Hugger, A.; Lange, M.; Schmitter, M.; Ottl, P.; Wolowski, A.; Türp, J.C. Occlusal dysesthesia-A clinical guideline. J. Oral. Rehabil. 2020, 47, 651–658. [Google Scholar] [CrossRef]
- von Piekartz, H.; Stein, Y.; Wenneker, L.; Hall, T.; Ballenberger, N. Evaluation of somatosensory bedside testing and neurodynamics of the trigeminal nerve in craniofacial pain: A matched case-control study. Cranio 2024, 4, 1–15. [Google Scholar] [CrossRef]
- Uehara, L.M.; Tardelli, J.D.C.; Botelho, A.L.; Valente, M.L.D.C.; Dos Reis, A.C. Association between depression and temporomandibular dysfunction in adults—A systematic review. Cranio 2023, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ballenberger, N.; von Piekartz, H.; Danzeisen, M.; Hall, T. Patterns of cervical and masticatory impairment in subgroups of people with temporomandibular disorders-an explorative approach based on factor analysis. Cranio 2018, 36, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral. Facial Pain. Headache. 2014, 28, 6–27. [Google Scholar]
- Bernardi, S.; Memè, L.; Belfioretti, C.; Bambini, F.; Gerardi, D.; Macchiarelli, G.; Bianchi, S.; Mummolo, S. Psoriatic Arthritis Involving TMJ: A Review on Pathogenesis and Consideration on Eventual Gender Differences. Dent. J. 2024, 12, 31. [Google Scholar] [CrossRef]
- Kurup, S.; Perez-Pino, A.; Litt, M. The association between temporomandibular disorders signs and symptoms, bruxism, and health variables: A cross-sectional study. Cranio 2024, 9, 1–9. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom. Med. 2002, 64, 258–266. [Google Scholar] [CrossRef]
- De La Torre Canales, G.; Christidis, N.; Grigoriadis, A.; Strandberg, T.; Montan, V.; Medina Flores, D.; Al-Moraissi, E.A.; Christidis, M. Associations between temporomandibular disorders and tinnitus—A systematic review. Cranio 2024, 17, 1–17. [Google Scholar] [CrossRef]
- Michelotti, A.; Rongo, R.; D’Antò, V.; Bucci, R. Occlusion, orthodontics, and temporomandibular disorders: Cutting edge of the current evidence. J. World Fed. Orthod. 2020, 9, S15–S18. [Google Scholar] [CrossRef]
- de Sousa, S.T.; de Mello, V.V.; Magalhães, B.G.; de Assis Morais, M.P.; Vasconcelos, M.M.; de França Caldas Junior, A.; Gomes, S.G. The role of occlusal factors on the occurrence of temporomandibular disorders. Cranio 2015, 33, 211–216. [Google Scholar] [CrossRef]
- Türp, J.C. «Centric relation»: From red giant to white dwarf. Cranio 2021, 39, 461–462. [Google Scholar] [CrossRef]
- Zonnenberg, A.J.J.; Türp, J.C.; Greene, C.S. Centric relation critically revisited-What are the clinical implications? J. Oral. Rehabil. 2021, 48, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Häggman-Henrikson, B.; Al Jaghsi, A.; Baad-Hansen, L.; Beecroft, E.; Bijelic, T.; Bracci, A.; Brinkmann, L.; Bucci, R.; Colonna, A.; et al. International Network for Orofacial Pain and Related Disorders Methodology. Temporomandibular disorders: INfORM/IADR key points for good clinical practice based on standard of care. Cranio 2024, 43(1), 1–5. [Google Scholar] [CrossRef] [PubMed]
- Poggio, C.E.; Manfredini, D. Does increasing vertical dimension of occlusion in centric relation affect muscular activity? An electromyographic study. J. Esthet. Restor. Dent. 2024, 36, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Kandasamy, S. The painful mind. Cranio 2024, 28, 1–3. [Google Scholar] [CrossRef]
- Saracutu, O.I.; Manfredini, D.; Bracci, A.; Ferrari Cagidiaco, E.; Ferrari, M.; Colonna, A. Awake bruxism behaviors frequency in a group of healthy young adults with different psychological scores. Cranio 2024, 1–8. [Google Scholar] [CrossRef]
- De La Torre Canales, G.; Câmara-Souza, M.B.; Muñoz Lora, V.R.M.; Guarda-Nardini, L.; Conti, P.C.R.; Rodrigues Garcia, R.M.; Del Bel Cury, A.A.; Manfredini, D. Prevalence of psychosocial impairment in temporomandibular disorder patients: A systematic review. J. Oral. Rehabil. 2018, 45, 881–889. [Google Scholar] [CrossRef]
- Dworkin, S.F.; Sherman, J.; Mancl, L.; Ohrbach, R.; LeResche, L.; Truelove, E. Reliability, validity, and clinical utility of the research diagnostic criteria for Temporomandibular Disorders Axis II Scales: Depression, non-specific physical symptoms, and graded chronic pain. J. Orofac. Pain. 2002, 16, 207–220. [Google Scholar]
- Tran, C.; Ghahreman, K.; Huppa, C.; Gallagher, J.E. Management of temporomandibular disorders: A rapid review of systematic reviews and guidelines. Int. J. Oral. Maxillofac. Surg. 2022, 51, 1211–1225. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pollis, M.; Colonna, A.; Manfredini, D.; Ferrari, M.; Ferrari Cagidiaco, E. Adaptation Skills and Temporomandibular Joint Neutrality: A Case Report of a Failed Orthognathic Surgery Intervention. Prosthesis 2025, 7, 15. https://doi.org/10.3390/prosthesis7010015
Pollis M, Colonna A, Manfredini D, Ferrari M, Ferrari Cagidiaco E. Adaptation Skills and Temporomandibular Joint Neutrality: A Case Report of a Failed Orthognathic Surgery Intervention. Prosthesis. 2025; 7(1):15. https://doi.org/10.3390/prosthesis7010015
Chicago/Turabian StylePollis, Matteo, Anna Colonna, Daniele Manfredini, Marco Ferrari, and Edoardo Ferrari Cagidiaco. 2025. "Adaptation Skills and Temporomandibular Joint Neutrality: A Case Report of a Failed Orthognathic Surgery Intervention" Prosthesis 7, no. 1: 15. https://doi.org/10.3390/prosthesis7010015
APA StylePollis, M., Colonna, A., Manfredini, D., Ferrari, M., & Ferrari Cagidiaco, E. (2025). Adaptation Skills and Temporomandibular Joint Neutrality: A Case Report of a Failed Orthognathic Surgery Intervention. Prosthesis, 7(1), 15. https://doi.org/10.3390/prosthesis7010015







