A 16-Year Chronicle of Developing a Healthy Workplace Participatory Program for Total Worker Health® in the Connecticut Department of Correction: The Health Improvement through Employee Control (HITEC) Program
Abstract
1. Introduction
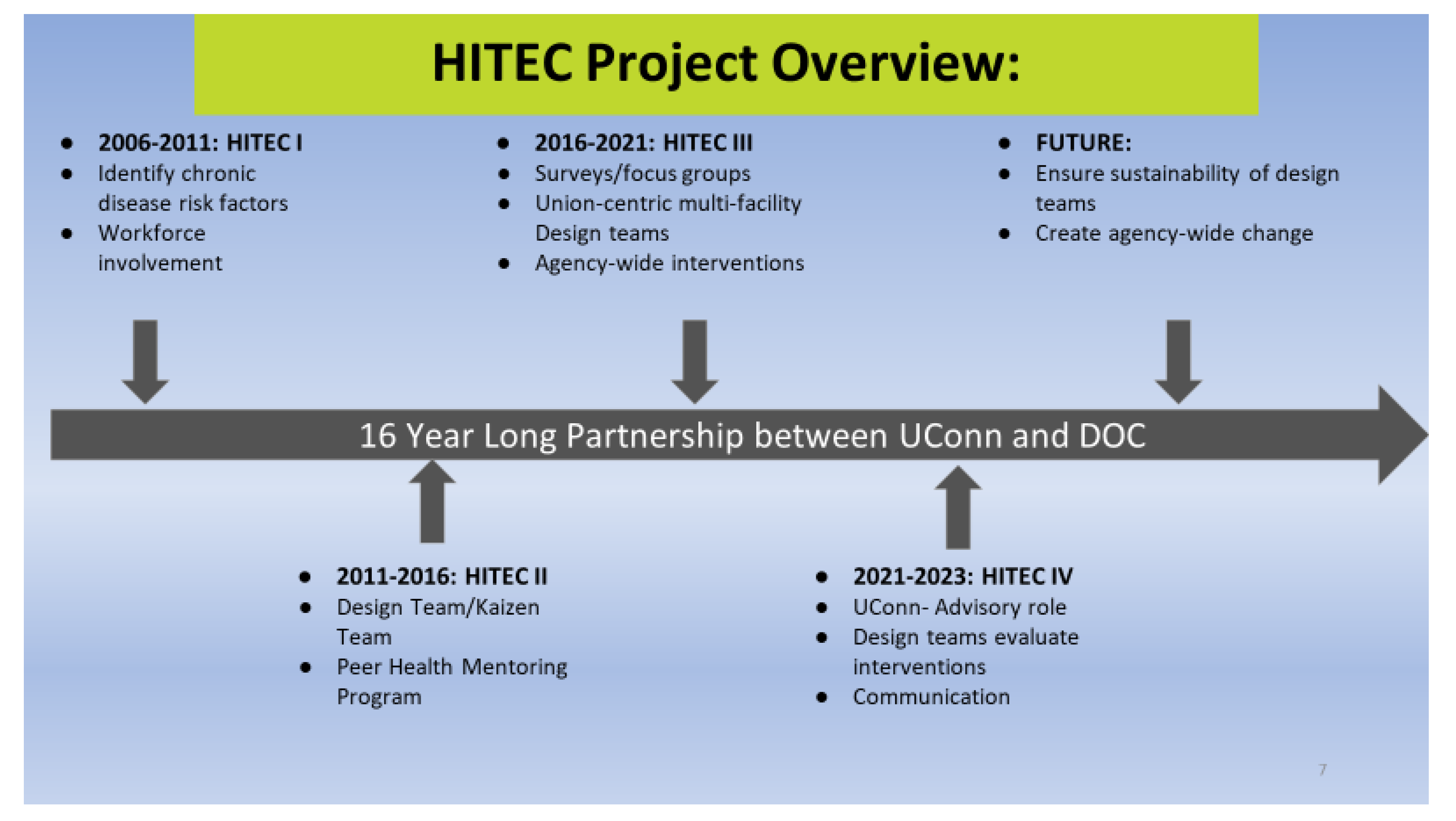
Background: The HITEC Program
2. Methods
- i.
- Intervention Assessment Survey (IAS). The IAS is a short health and environment survey that contains fewer than 10 questions and requires about 5 min to complete. It is intended for DT administration and reflects a reluctance on the part of the population to respond to written or electronic surveys. Domains (general health, physical symptoms, physical and emotional health, work conditions, workplace change, work environment) were factored by the study team from Core Survey responses. The IAS is modular, so the DT can select a specific question set. To allow for pre- and post- comparisons that are identifiable only to the participant, respondents provide their own idiosyncratic code (i.e., phone digits + PIN). The domains and format are IRB-approved so that DTs can choose modules without repeated IRB submission. The form provides de-identified content to the study team for analyses, but it also blinds the DT to the respondent. The format does require that respondents maintain their own unique code to enable follow-up. Follow-up response rates have ranged from <5% to >90%. Factors associated with a high-post intervention response rate include intensity of the intervention, post-survey administration by well-recognized DT representatives, and provision for protected time and space for survey completion. Those contingencies led to a preference for written rather than electronic entry.
- ii.
- The Nutrition and Physical Activity Questionnaire (NPAQ) was developed by the CPH-NEW team. It includes 10 questions adopted from the Hawkes and Nowak nutrition knowledge questionnaire [32] and 26 items that assess eating patterns at the workplace. It was subsequently customized to corrections for weight loss and exercise programs. One reason for customization was specific to corrections where high-calorie ordered-in food, frequent snacking, and bringing in well-packed lunch boxes prevailed due to the need to work double shifts on demand in accordance with their labor contract.
- iii.
- The Food and Physical Activity Liking Survey (FPALS) utilized in this study was customized for direct feedback to DOC users. Participants answer demographic questions, estimate their body size (based on a nine-figure Stunkard Scale [33]), and rate 59 food/beverage items and 10 non-food related items on a general Labeled Magnitude Scale. This was used in the three weight loss programs that were administered by HITEC.
3. Results
3.1. Participation Rates and Demographic Information
3.2. Types of Interventions Resulting from DT Development
Physical Environment
3.3. Peer Health Mentoring
4. Discussion
4.1. Participatory Design
4.2. HITEC Program Sustainability
4.3. Workforce Centricity and Labor Representation
4.4. Importance of Established Governing Structures and Resiliency
4.5. Comparing Community and Workplace Interventions
4.6. Mentoring
4.7. Multi-Level Organizational Strategies
5. Conclusions and Remarkable Findings
- DTs proved to be more resilient and capable of regeneration than expected. The HWPP presupposed that DTs would devolve and require assistance from the SWSC and facility leadership to persist. The DTs proved highly successful at internal replacement and longevity.
- DTs were not satisfied with simply handing over their intervention plans. In all cases, they were interested in carrying on through the implementation phase: for example, assisting with the evaluation efforts of intervention processes and outcomes.
- Cooperative work and engagement produce synthetic solutions. Perceived a priori barriers, such as the inertness of facility-based teams and the supervisor versus CO division, were difficult to resolve in a priori planning but were successfully addressed in practice.
- Cultural change is a long-term continuous process. The importance of supporting an ongoing effort was intuitively grasped by DTs and the workforce.
- The centrality of key issue identification and gauging sizes of effects through surveys was implicitly understood and was not seen as an academic imposition. The acceptance of quantifiable outcomes was likely a product of both curiosity and lengthy experience with the academic team, that had established trust.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schill, A.L.; Chosewood, L.C. The NIOSH Total Worker Health™ program: An overview. J. Occup. Environ. Med. 2013, 55, S8–S11. [Google Scholar] [CrossRef]
- Faghri, P.D.; Omokaro, C.; Parker, C.; Nichols, E.; Gustavesen, S.; Blozie, E. E-technology and pedometer walking program to increase physical activity at work. J. Prim. Prev. 2008, 29, 73–91. [Google Scholar] [CrossRef] [PubMed]
- Benedict, M.A.; Arterburn, D. Worksite-based weight loss programs: A systematic review of recent literature. Am. J. Health Promot. 2008, 22, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Ghaddar, A.; Mateo, I.; Sanchez, P. Occupational stress and mental health among correctional officers: A cross-sectional study. J. Occup. Health 2008, 50, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Schaufeli, W.B.; Peeters, M.C.W. Job stress and burnout among correctional officers: A literature review. Int. J. Stress Manag. 2000, 7, 19–48. [Google Scholar] [CrossRef]
- Albertsen, K.; Borg, V.; Oldenburg, B. A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Prev. Med. 2006, 43, 291–305. [Google Scholar] [CrossRef]
- Hignett, S.; Wilson, J.R.; Morris, W. Finding ergonomic solutions—Participatory approaches. Occup. Med. 2005, 55, 200–207. [Google Scholar] [CrossRef]
- World Health Organization. Ottawa Charter for Health Promotion; World Health Organization: Geneva, Switzerland, 1986; WHO/HPR/HEP/95.1.
- Jensen, P.L. Can participatory ergonomics become ‘the way we do things in this firm’—The Scandinavian approach in participatory ergonomics. Ergonomics 1997, 40, 1078–1087. [Google Scholar] [CrossRef]
- Vink, P.; Peeters, M.C.E.; Grundemann, R.W.M.; Smulders, P.G.W.; Kompier, M.; Dul, J. A participatory ergonomics approach to reduce mental and physical workload. Int. J. Ind. Ergon. 1995, 15, 385–396. [Google Scholar] [CrossRef]
- Lewin, K. Action research and minority problems. J. Soc. Issues 1946, 2, 34–46. [Google Scholar] [CrossRef]
- Argyris, C.; Schön, D.A. Participatory action research and action science compared: A commentary. Am. Behav. Sci. 1989, 32, 612–623. [Google Scholar] [CrossRef]
- Greenwood, D.J.; Whyte, W.F.; Harkavy, I. Participatory action research as a process and as a goal. Hum. Relat. 1993, 46, 175–192. [Google Scholar] [CrossRef]
- McTaggart, R. Participatory action research: Issues in theory and practice. Educ. Action Res. 1994, 2, 313–337. [Google Scholar] [CrossRef]
- Mordock, K.; Krasny, M.E. Participatory action research: A theoretical and practical framework for EE. J. Environ. Educ. 2001, 32, 15–20. [Google Scholar] [CrossRef]
- Viswanathan, M.; Ammerman, A.; Eng, E.; Garlehner, G.; Lohr, K.N.; Griffith, D.; Rhodes, S.; Samuel-Hodge, C.; Maty, S.; Lux, L.; et al. Community-based participatory research: Assessing the evidence. Evid. Rep. Technol. Assess. 2004, 99, 1–8. [Google Scholar]
- Hugentobler, M.K.; Israel, B.A.; Schurman, S.J. An action research approach to workplace health: Integrating methods. Health Educ. Q. 1992, 19, 55–76. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, K.; Abildgaard, J.S. Organizational interventions: A research-based framework for the evaluation of both process and effects. Work Stress 2013, 27, 278–297. [Google Scholar] [CrossRef]
- Tamers, S.L.; Chosewood, L.C.; Childress, A.; Hudson, H.; Nigam, J.; Chang, C.C. Total Worker Health® 2014–2018: The novel approach to worker safety, health, and well-being evolves. Int. J. Environ. Res. Public Health 2019, 16, 321. [Google Scholar] [CrossRef] [PubMed]
- Cherniack, M.G.; Punnett, L. A participatory framework for integrated interventions. In Total Worker Health; Hudson, H.L., Nigam, J.A.S., Sauter, S.L., Chosewood, L.C., Schill, A.L., Howard, J., Eds.; American Psychological Association: Worcester, MA, USA, 2019; pp. 107–124. [Google Scholar] [CrossRef]
- Henning, R.; Warren, N.; Robertson, M.; Faghri, P.; Cherniack, M.; CPH-NEW Research Team. Workplace health protection and promotion through participatory ergonomics: An integrated approach. Public Health Rep. 2009, 124, 26–35. [Google Scholar] [CrossRef]
- Introduction to Total Worker Health Mentoring Toolkit for the Corrections Workforce. Center for the Promotion of Health in the New England Workplace (CPH-NEW). Available online: https://www.uml.edu/Research/CPH-NEW/Resources/Corrections-Officer-Health-Resources/TWH-Mentoring-Toolkit-Corrections.aspx (accessed on 13 March 2023).
- Nobrega, S.; Kernan, L.; Plaku-Alakbarova, B.; Robertson, M.; Warren, N.; Henning, R.; CPH-NEW Research Team. Field tests of a participatory ergonomics toolkit for Total Worker Health. Appl. Ergon. 2017, 60, 366–379. [Google Scholar] [CrossRef]
- Strickland, J.R.; Kinghorn, A.M.; Evanoff, B.A.; Dale, A.M. Implementation of the Healthy Workplace Participatory Program in a retail setting: A feasibility study and framework for evaluation. Int. J. Environ. Res. Public Health 2019, 16, 590. [Google Scholar] [CrossRef]
- Ilmarinen, J.; Tuomi, K.; Eskelinen, L.; Nygård, C.H.; Huuhtanen, P.; Klockars, M. Background and objectives of the Finnish research project on aging workers in municipal occupations. Scand. J. Work Environ. Health 1991, 1, 7–11. [Google Scholar]
- Tuomi, K.; Ilmarinen, J.; Klockars, M.; Nygârd, C.H.; Seitsamo, J.; Huuhtanen, P.; Martikainen, R.; Aalto, L. Finnish research project on aging workers in 1981–1992. Scand. J. Work Environ. Health 1997, 1, 7–11. [Google Scholar]
- Savinainen, M.; Nygård, C.H.; Korhonen, O.; Ilmarinen, J. Changes in physical capacity among middle-aged municipal employees over 16 years. Exp. Aging Res. 2004, 30, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.S.; Chumlea, W.C.; Heymsfield, S.B.; Lukaski, H.C.; Schoeller, D.; Friedl, K.; Kuczmarski, R.J.; Flegal, K.M.; Johnson, C.L.; Hubbard, V.S. Development of bioelectrical impedance analysis prediction equations for body composition with the use of a multicomponent model for use in epidemiologic surveys. Am. J. Clin. Nutr. 2003, 77, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Mathiowetz, V.; Kashman, N.; Volland, G.; Weber, K.; Dowe, M.; Rogers, S. Grip and pinch strength: Normative data for adults. Arch. Phys. Med. Rehabil. 1985, 66, 69–74. [Google Scholar] [PubMed]
- McCartney, N.E.; Heigenhauser, G.J.; Sargeant, A.J.; Jones, N.L. A constant-velocity cycle ergometer for the study of dynamic muscle function. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 1983, 55, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Behrman, A.L.; Light, K.E.; Flynn, S.M.; Thigpen, M.T. Is the functional reach test useful for identifying falls risk among individuals with Parkinson’s disease? Arch. Phys. Med. Rehabil. 2002, 83, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, A.; Nowak, M. Patient education. Nutrition knowledge questionnaire. Aust. Fam. Physician. 1998, 27, 1057–1058. [Google Scholar]
- Stunkard, A.J.; Waxman, M. Accuracy of self-reports of food intake. J. Am. Diet Assoc. 1981, 79, 547–551. [Google Scholar] [CrossRef]
- Woods, M.; Paulus, T.; Atkins, D.P.; Macklin, R. Advancing qualitative research using qualitative data analysis software (QDAS)? Reviewing potential versus practice in published studies using ATLAS.ti and NVivo, 1994–2013. Soc. Sci. Comput. Rev. 2016, 34, 597–617. [Google Scholar] [CrossRef]
- Hughes, J.M.; Henning, R.A.; Robertson, M.M. Organizational sensemaking systems as a determinant of successful organizational change: A grounded theory approach. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2022, 66, 90–94. [Google Scholar] [CrossRef]
- Charmaz, K.; Thornberg, R. The pursuit of quality in grounded theory. Qual. Res. Psychol. 2021, 18, 305–327. [Google Scholar] [CrossRef]
- Weick, K.E.; Sutcliffe, K.M.; Obstfeld, D. Organizing and the process of sensemaking. Organ. Sci. 2005, 16, 409–421. [Google Scholar] [CrossRef]
- Buchholz, B.; Paquet, V.; Punnett, L.; Lee, D.; Moir, S. PATH: A work sampling-based approach to ergonomic job analysis for construction and other non-repetitive work. Appl. Ergon. 1996, 27, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Akas, O.; Azari, D.; Chen, C.-H.; Hu, Y.H.; Armstrong, T.J.; Ulin, S.S.; Radwin, R.G. An equation for estimating hand activity level based on measured hand speed and duty cycle. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2014, 58, 1600–1604. [Google Scholar] [CrossRef]
- Arnold, P.J. From the union hall: A labor critique of the new manufacturing and accounting regimes. Crit. Perspect. Account. 1999, 10, 399–423. [Google Scholar] [CrossRef]
- Riley, T.; Hawe, P. Researching practice: The methodological case for narrative inquiry. Health Educ. Res. 2005, 20, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Hawe, P. Lessons from complex interventions to improve health. Annu. Rev. Public Health 2015, 36, 307–323. [Google Scholar] [CrossRef]
- Blumenthal, D.S. Is community-based participatory research possible? Am. J. Prev. Med. 2011, 40, 386–389. [Google Scholar] [CrossRef]
- Buchanan, D.R.; Miller, F.G.; Wallerstein, N. Ethical issues in community-based participatory research: Balancing rigorous research with community participation in community intervention studies. Prog. Community Health Partnersh. 2007, 1, 153–160. [Google Scholar] [CrossRef] [PubMed]

| Topic Area | Citation | Findings and Key Themes |
|---|---|---|
| Participatory Approaches Utilized in HITEC | Henning, R.; Warren, N.; Robertson, M.; Faghri, P.; Cherniack, M.; CPH-NEW Research Team. Workplace health protection and promotion through participatory ergonomics: An integrated approach. Public Health Rep. 2009, 124, 26–35. | Integrating participatory ergonomics with traditional health promotion approaches in a bottom–up participatory model for engaging employees in innovative iterative design of workplace interventions to benefit worker wellbeing. |
| Punnett, L.; Warren, N.; Henning, R.; Nobrega, S.; Cherniack, M.; CPH-NEW Research Team. Participatory ergonomics as a model for integrated programs to prevent chronic disease. J. Occup. Environ. Med. 2013, 55, S19–S24. | Use of participatory methods for achieving successful workplace health promotion (WHP) programming, and, specifically, the relevance of participatory ergonomics (PE) for the NIOSH TWH initiative. | |
| Cherniack, M.; Dussetschleger, J.; Dugan, A.; Farr, D.; Namazi, S.; El Ghaziri, M.; Henning, R. Participatory action research in corrections: The HITEC 2 program. Appl. Ergon. 2016, 53, 169–180. | Programmatic overview of participatory interventions for corrections staff. Description of a peer health mentoring program which had positive health effects at 1 year and in diluting effects from overtime work. | |
| Dugan, A.G.; Farr, D.A.; Namazi, S.; Henning, R.; Wallace, K.N.; El Ghaziri, M.; Punnett, L.; Dussetschleger, J.L.; Cherniack, M.G. Process evaluation of two participatory approaches: Implementing Total Worker Health® interventions in a correctional workforce. Am J. Ind. Med. 2016, 59, 897–918. | HITEC-2 comparison of two participatory programs: a CO-only Design Team (DT) with a task-specific Kaizen Event Team (KET). A Program Evaluation Rating Sheet (PERS) was developed and utilized to document and evaluate program implementation. Key features such as level of bargaining unit involvement were identified. | |
| Cherniack, M.G.; Punnett, L. A participatory framework for integrated interventions. In Total Worker Health; Hudson, H.L., Nigam, J.A.S., Sauter, S.L., Chosewood, L.C., Schill, A.L., Howard, J., Eds.; American Psychological Association: Washington, DC, USA, 2019, pp. 107–124. | Participatory action research principles, participatory ergonomics, and other workplace participatory processes are detailed as foundations for an approach to preventing chronic health conditions including heart disease and diabetes. Compatibility with NIOSH Total Worker Health (TWH) is provided as case examples. | |
| Peer Mentoring and Training | Namazi, S.; Kotejoshyer, R.; Farr, D.; Henning, R.A.; Tubbs, D.C; Dugan, A.G.; El Ghaziri, M.; Cherniack, M. Development and implementation of a Total Worker Health® mentoring program in a correctional workforce. Int. J. Environ. Res. Public Health 2021, 18, 8712. | A Health Mentoring Program (HMP) paired newly hired COs with tenured and trained COs to provide health coaching. Goals were prevention of an observed early decline in physical fitness and promotion of healthy eating, stress management, and work–family balance. Methods for training, selection, quality maintenance, and documentation of status by survey and performance testing are described. |
| Kotejoshyer, R.; Gilmer, D.O.; Namazi, S.; Farr, D.; Henning, R.A.; Cherniack, M. Impact of a Total Worker Health® mentoring program in a correctional workforce. Int. J. Environ. Res. Public Health 2021, 18, 8436. | At 5 years, positive health effects in 269 corrections cadets, mentored for 1 year, were no longer observable compared to controls. The authors concluded that the results did not justify the extensive outside professional effort. Successful program elements continue to be adopted. | |
| Design Team Sponsored Interventions | Namazi, S.; Dugan, A.G.; Cavallari, J.M.; Rinker, R.D.; Preston, J.C.; Steele, V.L.; El Ghaziri, M.; Cherniack, M.G. Participatory design of a sleep intervention with correctional supervisors using a root causes approach. Am. J. Ind. Med. 2023, 66, 167–177. | The IDEAS tool, a structured seven-step planning process, was used to develop, implement, and evaluate sleep interventions. Customized surveys and an app were developed by the supervisors’ DT. Reduction of distractions and rumination were effective. Proposed scheduled changes were submitted to administration. |
| Dugan, A.G.; Namazi, S.; Cavallari, J.M.; Rinker, R.D.; Preston, J.C.; Steele, V.L.; Cherniack, M.G. Participatory survey design of a workforce health needs assessment for correctional supervisors. Am. J. Ind. Med. 2021, 64, 414–430. | Corrections supervisors developed their own survey to evaluate health and well-being. There were distinct advantages over conventional survey items, particularly for personal issues of substance use and mental health. | |
| Dugan, A.G.; Namazi, S.; Cavallari, J.M.; El Ghaziri, M.; Rinker, R.D.; Preston, J.C.; Cherniack, M.G. Participatory assessment and selection of workforce health intervention priorities for correctional supervisors. J. Occup. Environ. Med. 2022, 64, 578–592. | Methods for survey development compatible with investigator rigor and PAR and CBPR principles are described as developed in HITEC. The use of focus groups and a DT to set health priorities are explained. | |
| Methods Customized for Participatory Research in Corrections | Cherniack, M.; Berger, S.; Namazi, S.; Henning, R.; Punnett, L.; CPH-NEW Research Team. A Participatory action research approach to mental health interventions among corrections officers: Standardizing priorities and maintaining design autonomy. Occup. Health Sci. 2019, 3, 387–407. | Novel methodology for combining multiple sites where principles of autonomy across sites and inter-site comparability are objectives. The direct application of the multi-state priority selection process is presented. Comparison with other methods such as DELPHI is provided. |
| Punnett, L.; Cavallari, J.M.; Henning, R.A.; Nobrega, S.; Dugan, A.G.; Cherniack, M.G. Defining ‘integration’ for Total Worker Health®: A new proposal. Ann. Work. Expo. Health 2020, 64, 223–235. | A theoretical approach to homogenizing workplace health with work organizational change is presented. Methods for accommodating conflicting managerial priorities for efficiency alongside Total Worker Health worker-centricity are described. | |
| Hughes, J.M.; Henning, R.A.; Robertson, M.M. Organizational sensemaking systems as a determinant of successful organizational change: A grounded theory approach. Proc. Hum. Factors Ergon. 2022, 66, 90–94. | Organizational sense-making is offered as an alternative option to large-scale survey assessments to recognize explanatory points of consensus and priority in corrections cohorts. | |
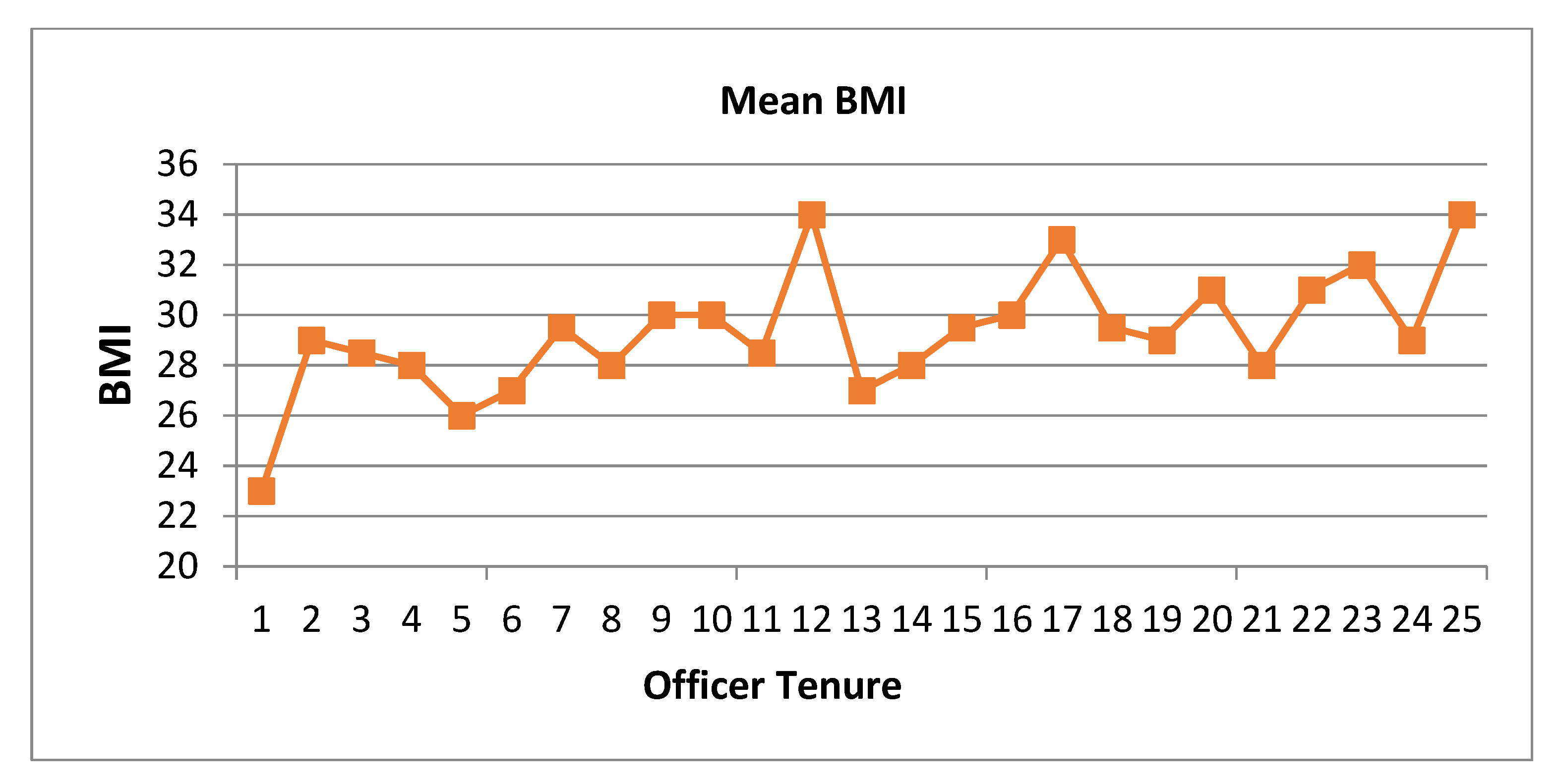
| Physical and General Health Issues in the HITEC Corrections Cohort | Warren, N.; Dussetschleger, J.; Punnett, L.; Cherniack, M.G. Musculoskeletal disorder symptoms in correction officers: Why do they increase rapidly with job tenure? Hum. Factors 2015, 57, 262–275. | The rapid onset of musculoskeletal disorders in corrections workers compared with manufacturing personnel appears to be a combination of psychosocial as well as biomechanical factors. |
| Morse, T.; Dussetschleger, J.; Warren, N.; Cherniack, M. Talking about health: Correction employees’ assessments of obstacles to healthy living. J. Occup. Environ. Med. 2011, 53, 1037–1045. | Hypertension was a double national norm. Officers related their elevated stress to concerns with security, administrative requirements, and work/family imbalance. Authors concluded that corrections workers are at high risk of chronic disease, and environmental changes are needed to reduce risk factors. | |
| Mignano, C; Faghri, P.D.; Huedo-Medina, T.; Cherniack, M.C. Psychological health, behavior, and bodyweight (PBBW) model: An evaluation of predictors of health behaviors and body mass index (BMI). J. Workplace Behav. Health. 2016, 31, 37–56. | Psychological health and reported stress were associated with body weight in corrections officers. Healthy behaviors mediated the negative effect of work stress on body weight. | |
| Obidoa, C.; Reeves, D.; Warren, N.; Reisine, S.; Cherniack, M. Depression and work family conflict among corrections officers. J. Occup. Environ. Med. 2011, 53, 1294–1301. | Work family conflict in corrections workers was elevated and associated with high levels of clinical depression. However, responses were muted below expectations, raising questions about the utility of validated surveys developed in other populations. | |
| Buden, J.C.; Dugan, A.G.; Faghri, P.D.; Huedo-Medina, T.B.; Namazi, S.; Cherniack, M.G. Associations among work and family health climate, health behaviors, work schedule, and body weight. J. Occup. Environ. Med. 2017, 59, 588–599. | Over 85% of the sample was overweight/obese. Both favorable workplace climate and family climate were associated with a lower BMI. Overtime shift work appeared to share a relationship with higher BMI. | |
| Buden, J.C.; Dugan, A.G.; Namazi, S.; Huedo-Medina, T.B.; Cherniack, M.G.; Faghri, P.D. Work characteristics as predictors of correctional supervisors’ health outcomes. J. Occup. Environ. Med. 2016, 58, e325–e334. | Corrections supervisors had a higher prevalence of obesity and comorbidities than the general US adult population. Burnout was significantly associated with nutrition, physical activity, sleep duration, sleep quality, diabetes, and anxiety/depression. Job meaning, job satisfaction, and workplace social support may predict health behaviors. | |
| Mental Health Issues in the HITEC Corrections Cohort | Gilmer, D.O.; Magley, V.J.; Dugan, A.G.; Namazi, S.; Cherniack, M.G. Relative importance of incivility and loneliness in occupational health outcomes. Occup. Health Sci. 2023, 7, 1–25. | General loneliness in corrections officers appears to be an important explanatory factor in emotional exhaustion, job satisfaction, and depression when work stress is controlled. |
| Namazi, S.; Dugan, A.G.; Fortinsky, R.H.; El Ghaziri, M.; Barnes-Farrell, J.L.; Noel, J.; Cavallari, J.M.; Shaw, W.S.; Cole, W.A.; Cherniack, M.G. Traumatic incidents at work, work-to-family conflict, and depressive symptoms among correctional supervisors: The moderating role of social support. Occup. Health Sci. 2021, 5, 493–517. | One-hundred and fifty-six (156) corrections supervisors were studied to assess the effects of direct and indirect trauma on work-to-family conflict and depressive symptoms. Work-to-family conflict mediated the association between traumatic incidents and depression. Social support moderated the association between traumatic incidents and depression. Interventions directed to supervisor mental health and family health are discussed. | |
| Namazi, S.; Dugan, A.G.; Fortinsky, R.H.; Barnes-Farrell, J.; Coman, E.; El Ghaziri, M.; Cherniack, M.G. Examining a comprehensive model of work and family demands, work-family conflict, and depressive symptoms in a sample of correctional supervisors. J. Occup. Environ. Med. 2019, 61, 818–828. | In corrections supervisors, overtime significantly predicted work-to-family conflict, and work-to-family conflict significantly predicted greater depression. Overtime work had an indirect effect on depression. |
| KET | DT | |
|---|---|---|
| Number of Interventions | 4 interventions, each with a separate KET, and each lasting 3 months | 4 interventions with a continuous DT and the sole restriction being completion by study end |
| Intervention Themes | Same as DT | Same as KET |
| Duration of Each Intervention | Fixed Time Limit/Intervention | Variable Time Limit/Intervention |
| Participatory Team Composition | Line Staff and Supervisors | Line Staff only |
| Team Solicitation | Open Recruitment | Labor and Management |
| Evaluation Tools | Group Surveys and Tests Intervention specific pre/post | Group Surveys and Tests Intervention specific pre/post |
| Name of Test | Purpose | Status for f/u |
|---|---|---|
| Anthropometric assessment | Height (cm), weight (kg), waist circumference (CM) | Maintained |
| Body composition/BIA [28] | Body fat | Maintained |
| Grip strength [29] | Hand strength | Maintained |
| Max. power/ergometry exercise test [30] | Lean muscle function and v02 max. approximation | Maintained |
| Functional reach test [31] | Upper body mobility | Dropped due to unreliability |
| Spine mobility [27] | Spinal intervals | Dropped due to unreliability |
| Blood pressure | Hypertension assessment | Maintained |
| Sites | Total Workers | COs | Participant | Inmate Ratio: CO | Avg. Age Years COs | Age Range | Ann. Illness/ Injury | Illness and Injury Rate per CO | Ann. MS Strain | MSI Rate per CO |
|---|---|---|---|---|---|---|---|---|---|---|
| Professional (Site A) | 434 | 349 | 161 | 4.83 | 40.6 | 22–61 | 625 | 1.44 | 210 | 0.48 |
| Participatory (Site B) | 428 | 340 | 157 | 4.39 | 40.9 | 21–68 | 707 | 1.65 | 165 | 0.39 |
| 2007 1,2 | 2008 3,4 | 2009 2,4 | 2011 3,4 | 2013 3,4 | 2016 3,4 | |
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | T5 | ||
| Target population | 598 | 862 | 820 | 826 | 841 | 845 |
| Participants | 124 | 332 | 65 | 382 | 348 | 390 |
| % Participation | 20.7% | 38.5% | 8.0% | 46.2% | 41.4% | 46.2% |
| Supervisors | Sites A and B | Sites A and B | Sites A and B | Sites A and B | Sites A and B |
| All DOC Subjects | |||
|---|---|---|---|
| Variables | Males | Females | Total |
| Participants | 242 | 89 | 332 |
| Age: mean (sd)/median | 41.3 (8.3) | 43.9 (8.6) | 42.0 (8.4) |
| SF-12 PCS: mean (sd) | 51.3 (6.5) | 51.3 (8.4) | 51.3 (7.1) |
| SF-12 MCS: mean (sd) | 48.9 (10.2) | 48.4 (10.4) | 48.8 (10.2) |
| BMI | |||
| Mean (sd) | 32.25 (5.31) | 28.72 (5.32) | 31.28 (5.53) |
| % Normal | 4.0% | 24.1% | 9.6% |
| % Overweight | 32.2% | 44.4% | 35.5% |
| % Obese | 63.6% | 31.5% | 54.8% |
| Body Fat | |||
| %Healthy | 17.6% | 55.3% | 27.3% |
| % Overweight | 33.1% | 21.3% | 30.1% |
| % Obese | 48.5% | 23.4% | 42.1% |
| Hypertension | |||
| % Normal | 16.1% | 42.6% | 23.5% |
| % Pre HTN | 54.5% | 44.4% | 51.8% |
| % HTN | 29.4% | 13.0% | 24.9% |
| Location | Mentees | Mentors | ||
|---|---|---|---|---|
| Number | Percent | Number | Percent | |
| A | 30 | 16.4 | 19 | 18.1 |
| B | 17 | 9.3 | 10 | 9.5 |
| C | 14 | 7.6 | 7 | 6.7 |
| D | 23 | 12.5 | 14 | 13.3 |
| E | 19 | 10.4 | 12 | 11.4 |
| F | 18 | 9.8 | 12 | 11.4 |
| G | 7 | 3.8 | 2 | 1.9 |
| H | 24 | 13.1 | 10 | 9.5 |
| I | 20 | 10.9 | 8 | 7.6 |
| All others (n = 4) | 11 | 6.0 | 11 | 10.5 |
| Total | 183 | 105 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cherniack, M.; Namazi, S.; Brennan, M.; Henning, R.; Dugan, A.; El Ghaziri, M. A 16-Year Chronicle of Developing a Healthy Workplace Participatory Program for Total Worker Health® in the Connecticut Department of Correction: The Health Improvement through Employee Control (HITEC) Program. Int. J. Environ. Res. Public Health 2024, 21, 142. https://doi.org/10.3390/ijerph21020142
Cherniack M, Namazi S, Brennan M, Henning R, Dugan A, El Ghaziri M. A 16-Year Chronicle of Developing a Healthy Workplace Participatory Program for Total Worker Health® in the Connecticut Department of Correction: The Health Improvement through Employee Control (HITEC) Program. International Journal of Environmental Research and Public Health. 2024; 21(2):142. https://doi.org/10.3390/ijerph21020142
Chicago/Turabian StyleCherniack, Martin, Sara Namazi, Matthew Brennan, Robert Henning, Alicia Dugan, and Mazen El Ghaziri. 2024. "A 16-Year Chronicle of Developing a Healthy Workplace Participatory Program for Total Worker Health® in the Connecticut Department of Correction: The Health Improvement through Employee Control (HITEC) Program" International Journal of Environmental Research and Public Health 21, no. 2: 142. https://doi.org/10.3390/ijerph21020142
APA StyleCherniack, M., Namazi, S., Brennan, M., Henning, R., Dugan, A., & El Ghaziri, M. (2024). A 16-Year Chronicle of Developing a Healthy Workplace Participatory Program for Total Worker Health® in the Connecticut Department of Correction: The Health Improvement through Employee Control (HITEC) Program. International Journal of Environmental Research and Public Health, 21(2), 142. https://doi.org/10.3390/ijerph21020142







