Parental Attitudes and Beliefs toward Attention Deficit Hyperactivity Disorder in Prince Sultan Military Medical City, Riyadh City
Abstract
:1. Introduction
2. Materials and Methods
Validating the Questionnaire
3. Results
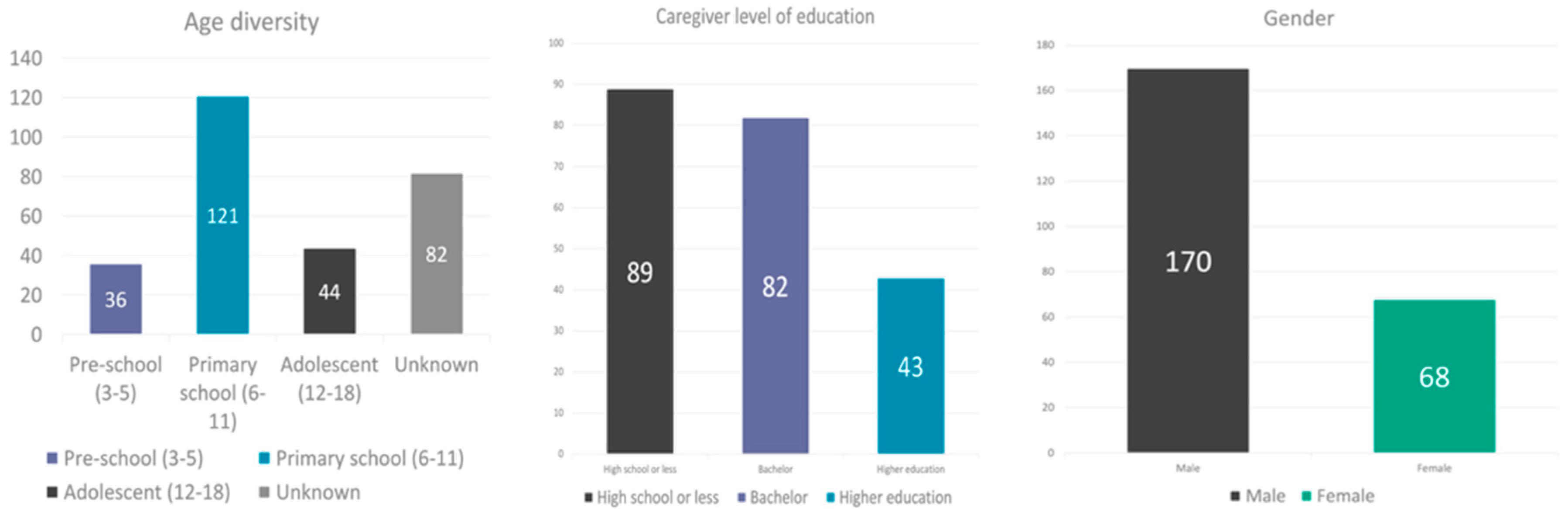
3.1. Participant Characteristics
3.2. Beliefs Related to the Management and Treatment of ADHD
3.3. Beliefs Related to the Etiology of ADHD
3.4. Attitudes Related to the Impact of Media and the Public on ADHD Perceptions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Publishing Inc.: Arlington, TX, USA, 2013. [Google Scholar]
- American Academy of Pediatrics, Project Advisory Committee. The medical home: Medical home initiatives for children with special needs. Pediatrics 2002, 110, 184–186. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Benito, J.; Van de Vijver, F.; Balluerka, N.; Caterino, L. Cross-Cultural and Gender Differences in ADHD Among Young Adults. J. Atten. Disord. 2019, 23, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Corkum, P.; Rimer, P.; Schachar, R. Parental knowledge of attention-deficit hyperactivity disorder and opinions of treatment options: Impact on enrolment and adherence to a 12- month treatment trial. Can. J. Psychiatry 1999, 44, 1043–1048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamrin, V.; McCarthy, E.M.; Tyson, V. Pediatric psychotropic medication initiation and adherence: A literature review based on social exchange theory. J. Child Adolesc. Psychiatr. Nurs. 2010, 23, 151–172. [Google Scholar] [CrossRef]
- Hillemeier, M.M.; Foster, E.M.; Heinrichs, B.; Heier, B.; Conduct Problems Prevention Research Group. Racial differences in parental reports of attention-deficit/hyperactivity disorder behaviors. J. Dev. Behav. Pediatrics JDBP 2007, 28, 353–361. [Google Scholar] [CrossRef] [Green Version]
- DosReis, S.; Barksdale, C.L.; Sherman, A.; Maloney, K.; Charach, A. Stigmatizing experiences of parents of children with a new diagnosis of ADHD. Psychiatr. Serv. 2010, 61, 811–816. [Google Scholar] [CrossRef]
- Coghill, D.; Soutullo, C.; d’Aubuisson, C.; Preuss, U.; Lindback, T.; Silverberg, M.; Buitelaar, J. Impact of attention-deficit/hyperactivity disorder on the patient and family: Results from a European survey. Child Adolesc. Psychiatry Ment. Health 2008, 2, 31. [Google Scholar] [CrossRef] [Green Version]
- Fiks, A.G.; Mayne, S.; DeBartolo, E.; Power, T.J.; Guevara, J.P. Parental preferences and goals regarding ADHD treatment. Pediatrics 2013, 132, 692–702. [Google Scholar] [CrossRef] [Green Version]
- Basudan, M.; Akbar, N.; El-Ghamdi, W.; Ibrahim, A. Knowledge, and attitude of female teachers toward ADHD at elementary schools, Jeddah, KSA, 2017. Int. Ann. Med. 2019, 3, 693–699. [Google Scholar]
- Alfageer, H.H.; Aldawodi, M.D.; Al Queflie, S.A.; Masud, N.; Al Harthy, N.A.; Alogayyel, N.; Alrabah, M.; Qureshi, S. Knowledge and attitude of male primary school teachers about attention deficit and hyperactivity disorder in Riyadh, Saudi Arabia. J. Nat. Sci. Biol. Med. 2018, 9, 257. [Google Scholar]
- Fayyad, J.A.; Jahshan, C.S.; Karam, E.G. Systems development of child mental health services in developing countries. Child Adolesc. Psychiatr. Clin. N. Am. 2001, 10, 745–762. [Google Scholar] [CrossRef]
- Farah, L.G.; Fayyad, J.A.; Eapen, V.; Cassir, Y.; Salamoun, M.M.; Tabet, C.C.; Mneimneh, Z.N.; Karam, E.G. ADHD in the Arab world: A review of epidemiologic studies. J. Atten. Disord. 2009, 13, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Polanczyk, G.V.; Salum, G.A.; Sugaya, L.S.; Caye, A.; Rohde, L.A. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry 2015, 56, 345–365. [Google Scholar] [CrossRef]
- Sciberras, E.; Bisset, M.; Hazell, P.; Nicholson, J.; Anderson, V.; Lycett, K.; Jongeling, B.; Efron, D. Health-related impairments in young children with ADHD: A community-based study. Child Care Health Dev. 2016, 42, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Nunnally, J.C. Psychometric Theory 3E: Tata McGraw-Hill Education; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Dodangi, N.; Vameghi, R.; Habibi, N. Evaluation of knowledge and attitude of parents of attention deficit/hyperactivity disorder children towards attention deficit/hyperactivity disorder in clinical samples. Iran. J. Psychiatry 2017, 12, 42. [Google Scholar] [PubMed]
- Ghanizadeh, A. Educating and counseling of parents of children with attention-deficit hyperactivity disorder. Patient Educ. Couns. 2007, 68, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Pham, A.V.; Carlson, J.S.; Kosciulek, J.F. Ethnic differences in parental beliefs of attention-deficit/hyperactivity disorder and treatment. J. Atten. Disord. 2010, 13, 584–591. [Google Scholar] [CrossRef] [Green Version]
- Perry, C.E.; Hatton, D.; Kendall, J. Latino parents’ accounts of attention deficit hyperactivity disorder. J. Transcult. Nurs. 2005, 16, 312–321. [Google Scholar] [CrossRef]
- Barkley, R.A.; Fischer, M.; Smallish, L.; Fletcher, K. The persistence of attention- deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J. Abnorm. Psychol. 2002, 111, 279. [Google Scholar] [CrossRef]
- Sonuga-Barke, E.J. Psychological heterogeneity in AD/HD—A dual pathway model of behaviour and cognition. Behav. Brain Res. 2002, 130, 29–36. [Google Scholar] [CrossRef]
- Abid, H.; Hamdani, S.U.; Shafique, F.; Aadil, M. Parental psychosocial attitudes and opinions on the use of psychotropic medication in mental disorders of childhood. PAFMJ 2018, 68, 131–136. [Google Scholar]
- Satterfield, J.H.; Satterfield, B.T.; Schell, A.M. Therapeutic interventions to prevent delinquency in hyperactive boys. J. Am. Acad. Child Adolesc. Psychiatry 1987, 26, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Jawaid, A.; Zafar, A.; Naveed, A.; Sheikh, S.; Waheed, S.; Zafar, M.; Syed, E.U.; Fatmi, Z. Knowledge of primary pediatric care providers regarding attention deficit hyperactivity disorder and learning disorder: A study from Pakistan. Singap. Med. J. 2008, 49, 985. [Google Scholar]
| Agree | Disagree | I Do Not Know | |
|---|---|---|---|
| Can diet improve ADHD symptoms? | |||
| Is consuming sugar and candy one of the causes of ADHD? | |||
| Can dietary supplements and vitamins treat ADHD? | |||
| Can electronic devices such as mobiles and tablets cause ADHD? | |||
| Can ADHD medication cause addiction? | |||
| Is ADHD a form of misbehavior and not a neurodevelopmental disorder? | |||
| Is the parents’ method of raising children a cause of ADHD? | |||
| Do I prefer behavioral interventions over medication? | |||
| Is the most common cause of ADHD a genetic factor? | |||
| Does the way the media talks about ADHD prevent me from giving my child medication? | |||
| My child has a history of severe side effects after using ADHD medication. | |||
| Can using ADHD medication for a long period affect my child negatively? | |||
| I follow non-specialist (friends and relatives) advice and recommendations regarding treatment plans for ADHD. | |||
| Level of ADHD symptoms in my child before starting any kind of treatment. | Severe | Moderate | Mild |
| Preschool | |||||
|---|---|---|---|---|---|
| Agree | Disagree | I Do Not Know | N/A | ||
| 1 | Can diet improve ADHD symptoms? | 19 (52.78%) | 3 (8.33%) | 14 (38.89%) | |
| 2 | Is consuming sugar and candy one of the causes of ADHD? | 16 (44.44%) | 14 (38.89%) | 6 (16.67%) | |
| 3 | Can dietary supplements and vitamins treat ADHD? | 5 (13.89%) | 9 (25%) | 22 (61.11%) | |
| 4 | Can electronic devices such as mobiles and tablets cause ADHD? | 2 (5.56%) | 27 (75%) | 7 (19.44%) | |
| 5 | Can ADHD medication cause addiction? | 5 (13.89%) | 25 (69.44%) | 6 (16.67%) | |
| 6 | Is ADHD a form of misbehavior and not a neurodevelopmental disorder? | 27 (75%) | 3 (8.33%) | 6 (16.67%) | |
| 7 | Is the parents’ method of raising children a cause of ADHD? | 12 (33.33%) | 6 (16.67%) | 18 (50%) | |
| 8 | Do I prefer behavioral interventions over medication? | 18 (50%) | 8 (22.22%) | 10 (27.7%) | |
| 9 | Is the most important factor of having ADHD a genetic factor? | 20 (55.56%) | 6 (16.67%) | 10 (27.78%) | |
| 10 | Does the way the media talks about ADHD prevent me from giving my child medication? | 12 (33.33%) | 6 (16.67%) | 18 (50%) | |
| 11 | My child has a history of severe side effects after using ADHD medication. | 4 (11.11%) | 17 (47.22%) | 15 (41.67%) | |
| 12 | Can using ADHD medication for a long period affect my child negatively? | 8 (22.22%) | 3 (8.33%) | 25 (69.44%) | |
| 13 | I follow non-specialist (friends and relatives) advice and recommendations regarding treatment plans for ADHD. | 3 (8.33%) | 32 (88.99%) | 1 (2.78%) | |
| 14 | 20 (55.56%) M | 8 (22.22%) Mi | 6 (16.67%) S | ||
| Primary School | |||||
|---|---|---|---|---|---|
| Agree | Disagree | I Do Not Know | N/A | ||
| 1 | Can diet improve ADHD symptoms? | 69 (52.27) | 18 (13.64) | 42 (31.82) | 3 (2.27) |
| 2 | Is consuming sugar and candy one of the causes of ADHD? | 87 (65.91%) | 30 (22.73%) | 15 (11.36%) | |
| 3 | Can dietary supplements and vitamins treat ADHD? | 17 (12.88%) | 53 (40.15%) | 62 (46.97%) | |
| 4 | Can electronic devices such as mobiles and tablets cause ADHD? | 15 (11.36%) | 92 (69.70%) | 23 (17.42%) | 2 (1.52) |
| 5 | Can ADHD medication cause addiction? | 18 (13.64%) | 88 (66.67%) | 25 (18.94) | 1 (0.76%) |
| 6 | Is ADHD a form of misbehavior and not a neurodevelopmental disorder? | 72 (54.55%) | 29 (21.97%) | 30 (22.73%) | 1 (0.76%) |
| 7 | Is the parents’ method of raising children a cause of ADHD? | 46 (34.85%) | 31 (23.48%) | 55 (41.67%) | |
| 8 | Do I prefer behavioral interventions over medication? | 48 (36.36) | 43 32.58% | 39 (29.55%) | 2 (1.52%) |
| 9 | Is the most important factor of having ADHD a genetic factor? | 69 (52.27%) | 26 (19.70) | 37 (28.03) | |
| 10 | Does the way the media talks about ADHD prevent me from giving my child medication? | 36 (27.27%) | 16 (12.12%) | 80 (60.61%) | |
| 11 | My child has a history of severe side effects after using ADHD medication. | 26 (19.70%) | 87 (65.91%) | 15 (11.36%) | 4 (3.03%) |
| 12 | Can using ADHD medication for a long period negatively affect my child? | 32 (24.24%) | 32 (24.24%) | 66 (50%) | 2 (1.52%) |
| 13 | I follow non-specialist (friends and relatives) advice and recommendations regarding treatment plans for ADHD. | 13 (9.85%) | 104 (78.79%) | 15 (11.36%) | |
| 14 | 2 (5.56%) NA | 44 (33.33%) S | 16 (12.12%) Mi | 5 (3.79%) | |
| Adolescent | |||||
|---|---|---|---|---|---|
| Agree | Disagree | I Do Not Know | N/A | ||
| 1 | Can diet improve ADHD symptoms? | 61 (53.04%) | 18 (15.65%) | 35 (30.43%) | 1 (0.87%) |
| 2 | Is consuming sugar and candy one of the causes of ADHD? | 79 (68.70%) | 23 (20.0%) | 13 (11.30%) | |
| 3 | Can dietary supplements and vitamins treat ADHD? | 21 (18.26%) | 52 (45.22%) | 42 (36.52%) | |
| 4 | Can electronic devices such as mobiles and tablets cause ADHD? | 18 (15.65%) | 75 (65.22%) | 21 (18.26%) | |
| 5 | Can ADHD medication cause addiction? | 23 (20%) | 71 (61.74%) | 20 (17.39%) | 1 (0.87%) |
| 6 | Is ADHD a form of misbehavior and not a neurodevelopmental disorder? | 61 (53.04%) | 29 (25.22) | 23 (20%) | 2 (1.74%) |
| 7 | Is the parents’ method of raising children a cause of ADHD? | 43 (37.39) | 22 (19.13) | 49 (42.61%) | 1 (0.87%) |
| 8 | Do I prefer behavioral interventions over medication? | 35 (30.43%) | 51 (44.35%) | 25 (21.74%) | 4 (3.48%) |
| 9 | Is the most important factor of having ADHD a genetic factor? | 68 (59.13%) | 23 (20%) | 23 (20%) | 1 (0.87%) |
| 10 | Does the way the media talks about ADHD prevent me from giving my child medication? | 34 (29.57%) | 21 (18.26%) | 58 (50.43%) | 2 (1.74%) |
| 11 | My child has a history of severe side effects after using ADHD medication. | 25 (21.74%) | 70 (60.87%) | 19 (16.52%) | 1 (0.87%) |
| 12 | Can using ADHD medication for a long period negatively affect my child? | 23 (20%) | 30 (26.09%) | 61 (53.04%) | 1 (0.87%) |
| 13 | I follow non-specialist (friends and relatives) advice and recommendations regarding treatment plans for ADHD. | 20 (17.39%) | 85 (73.91%) | 9 (7.83%) | 1 (0.87%) |
| 14 | 47 (40.87%) | 39 (33.92%) | 25 (21.72%) | 4 (3.48%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alrahili, N.; Al Harthi, M.A.; Ababtain, S.J.; Al Sharif, S.S.; Alnuwaysir, M.A.; Al Huzaimi, R.F. Parental Attitudes and Beliefs toward Attention Deficit Hyperactivity Disorder in Prince Sultan Military Medical City, Riyadh City. Psych 2022, 4, 238-246. https://doi.org/10.3390/psych4020020
Alrahili N, Al Harthi MA, Ababtain SJ, Al Sharif SS, Alnuwaysir MA, Al Huzaimi RF. Parental Attitudes and Beliefs toward Attention Deficit Hyperactivity Disorder in Prince Sultan Military Medical City, Riyadh City. Psych. 2022; 4(2):238-246. https://doi.org/10.3390/psych4020020
Chicago/Turabian StyleAlrahili, Nader, Mansour Abdulaziz Al Harthi, Sarah Jassim Ababtain, Salma Saad Al Sharif, Mohammed Abdulaziz Alnuwaysir, and Roaa Fahad Al Huzaimi. 2022. "Parental Attitudes and Beliefs toward Attention Deficit Hyperactivity Disorder in Prince Sultan Military Medical City, Riyadh City" Psych 4, no. 2: 238-246. https://doi.org/10.3390/psych4020020
APA StyleAlrahili, N., Al Harthi, M. A., Ababtain, S. J., Al Sharif, S. S., Alnuwaysir, M. A., & Al Huzaimi, R. F. (2022). Parental Attitudes and Beliefs toward Attention Deficit Hyperactivity Disorder in Prince Sultan Military Medical City, Riyadh City. Psych, 4(2), 238-246. https://doi.org/10.3390/psych4020020






