Is There a Relationship Between Helicobacter pylori Infection and Anthropometric Status?
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Data Collection
2.3. Materials
2.4. Procedings
2.4.1. Fecal Samples
- Test band (T): Indicates the presence of Helicobacter pylori antigens if formed.
- Control band (C): Confirms that the test was performed correctly.
2.4.2. Bioimpedance
- Ensure the scale is calibrated and set to zero; it should be clean and ready for use.
- Enter the patient’s data into the InBody 120 software.
- Request the patient to remove shoes, socks, piercings below the neck, necklaces, rings, bracelets, and any heavy or metallic items.
- The patient is asked to step onto the scale and position their feet on the metallic area in an anatomical stance.
- When prompted by the scale, the patient is handed the device to hold, ensuring that their thumbs make contact with the metallic part while maintaining an anatomical stance. The patient remains in this position until the machine beeps, signaling that the test is complete and they may step off the device.
- The software displays measurements such as fat, muscle, water, bone, proteins, and other parameters. These results are automatically stored in a database.
2.5. Ethical Approval
2.6. Statistical Analysis
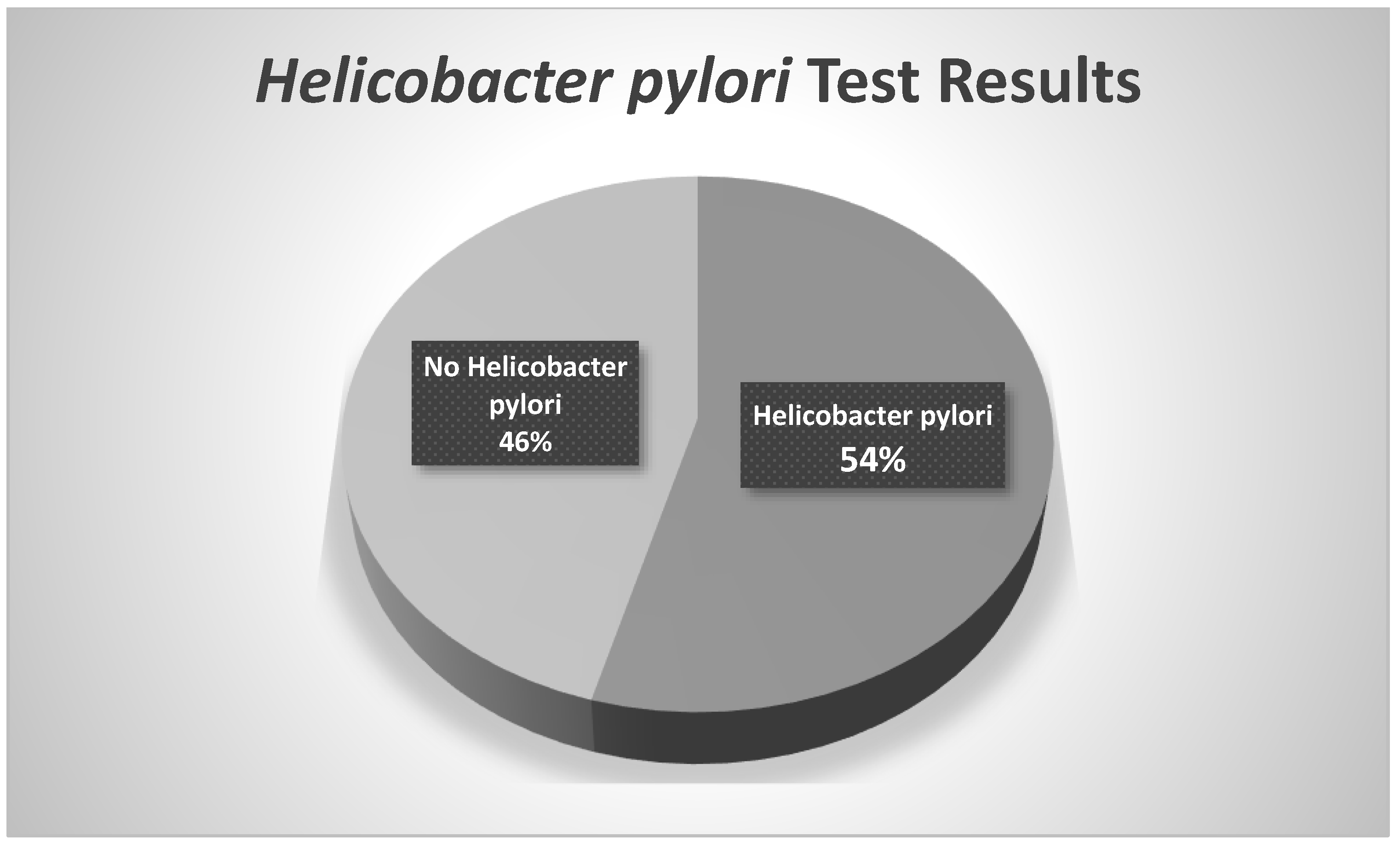
3. Results
3.1. Population
3.2. Body Composition
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aimasso, U.; D’Onofrio, V.; D’Eusebio, C.; Devecchi, A.; Pira, C.; Merlo, F.D.; De Francesco, A. Helicobacter pylori and nutrition: A bidirectional communication. Minerva Gastroenterol. Dietol. 2019, 65, 116–129. [Google Scholar] [CrossRef] [PubMed]
- Su, X.Q.; Yin, Z.Y.; Jin, Q.Y.; Liu, Z.C.; Han, X.; Hu, Z.Q.; Zhang, L.; Ma, J.L.; Li, Z.X.; Zhang, Y.; et al. Allium vegetable intake associated with the risk of incident gastric cancer: A continuous follow-up study of a randomized intervention trial. Am. J. Clin. Nutr. 2023, 117, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Assa, A.; Borrelli, O.; Broekaert, I.; Saccomani, M.D.; Dolinsek, J.; Martin-de-Carpi, J.; Mas, E.; Miele, E.; Sila, S.; Thomson, M.; et al. Helicobacter pylori-negative Chronic Gastritis in Children: A Systematic Review. J. Pediatr. Gastroenterol. Nutr. 2022, 74, 956–967. [Google Scholar] [CrossRef] [PubMed]
- Carlosama-Rosero, Y.H.; Acosta-Astaiza, C.P.; Sierra-Torres, C.H.; Bolaños-Bravo, H.J. Helicobacter pylori genotypes associated with gastric cancer and dysplasia in Colombian patients. Rev. Gastroenterol. México Engl. Ed. 2022, 87, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Di Mario, F.; Crafa, P.; Barchi, A.; Franzoni, L.; Franceschi, M.; Russo, M.; Bricca, L.; Brozzi, L.; Rodriguez Castro, K.; Rugge, M. Pepsinogen II in gastritis and Helicobacter pylori infection. Helicobacter 2022, 27, e12872. [Google Scholar] [CrossRef] [PubMed]
- Hernández, K.d.C.D.; Tejedor, O.J.G. Frecuencia de Helicobacter pylori en pacientes que asisten al hospital militar de la ciudad de Loja-Ecuador. Rev. Clín. Int. Tecnol. Intercont ARANDI-UTIC 2024, 11, 984–994. [Google Scholar] [CrossRef]
- Murillo Zavala, A.; Campos Pachito, M.J.; Moreira Rivadeneira, K.M. Helicobacter pylori y su asociación con hábitos alimenticios en adolescentes de la parroquia San Mateo ciudad Esmeraldas. Polo Conoc. 2021, 6, 150–163. [Google Scholar]
- Aroca Albiño, J.M.; Vélez Zamora, L. Prevalencia de Helicobacter pylori en pacientes asintomáticos en Ecuador. RevVive 2021, 4, 193–202. [Google Scholar] [CrossRef]
- Fajardo, E.G.S.; del Roscio Urrutia, L.; Jiménez, D.G.S.; Granoble, G.Y.M. Incidence of Helicobacter pylori in the Generation of Colon Cancer, at the National Cancer Institute “Dr. Juan Tanca Marengo” “SOLCA” Guayaquil 2019; Incidencia del Helicobacter pylori en la Generación del Cáncer de Colon, en el Instituto Oncológico Naci. 2021. Available online: https://www.cabidigitallibrary.org/doi/full/10.5555/20220400685 (accessed on 9 September 2024).
- Mora-Verdugo, M.; Duque-Proaño, G.; Villagran, F.; Otzen, T. Analysis the General Obesity Trends in Ecuador in the Period 2014–2016; Análisis de la Tendencia de la Obesidad General en Ecuador en los años 2014 a 2016. 2022. Available online: https://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0717-95022022000501268 (accessed on 9 September 2024).
- Vázquez-Jiménez, J.G.; Casillas-Armenta, O.E.; Cortéz, M.I.O.; Romero-García, T. Comprehending Metabolic Syndrome in Children and Adolescents: Cardiometabolic Outcomes in Response to Exercise; Comprendiendo el Síndrome Metabólico en Niños y Adolescentes: Efectos Cardiometabólicos en Respuesta al Ejercicio. 2025. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=9790615 (accessed on 18 September 2024).
- Caballero, B. Humanos Contra la Obesidad: ¿Quién Ganará? Nutr. Av. 2019, 10, S4–S9. [Google Scholar] [CrossRef]
- INEC IN de E y C. Encuesta Nacional de Salud y Nutrición.Quito: INEC. 2018. Available online: https://www.ecuadorencifras.gob.ec/documentos/web-inec/Estadisticas_Sociales/ENSANUT/ENSANUT_2018/Principales%20resultados%20ENSANUT_2018.pdf (accessed on 18 September 2024).
- OMS. La OMS Insta a los Gobiernos a Fomentar la Alimentación Saludable en los Establecimientos Públicos [Internet]. 2021. Available online: https://www.who.int/es/news/item/12-01-2021-who-urges-governments-to-promote-healthy-food-in-public-facilities#:~:text=limitarelconsumodeazúcares,legumbresyfrutossecos%3By (accessed on 12 October 2024).
- Trini, F.A.; Dency, R.D.; Elena, T.T.M.; Mercedes, C.B.; Félix MPR, R.M. Characterization of Helicobacter pylori infection in children and adolescents in an ambulatory service. Rev. Cubana Pediatr. 2018, 90, 1–10. Available online: http://scielo.sld.cu (accessed on 18 October 2024).
- Díaz, O.O.G.; Valentine, O.D.; Martínez, V.R.; Verenice, G.M.; Michaud, D.A.L.; Semper, C.J.; Acosta, J.A.P. Verenice González Mejia1, Dally Anne Lesly Michaud1 CJSJAPA. Factores Sociodemográficos, de Estilo de Vida, Antecedentes e Indicadores Metabólicos Específicos Asociados a Helicobacter pylorien Empleados de una Universidad Privada Mexicana. Rev. Científica Cienc. Salud 2024, 17, 1–10. Available online: https://rccs.upeu.edu.pe/index.php/rc_salud/article/view/2098/2159 (accessed on 20 October 2024). [CrossRef]
- Ostos, O. Relación Entre la Presencia de Helicobacter pylori con el Desarrollo de la Insulinorresistencia y Enfermedades asociadas. Biociencias 2022, 6, 69–92. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=9210502 (accessed on 20 October 2024).
- Instituto Nacional del Cáncer de Estados Unidos. Helicobacter pylori y el Cáncer [Internet]. Instituto Nacional del Cáncer de Estados Unidos. 2023. Available online: https://www.cancer.gov/espanol/cancer/causas-prevencion/riesgo/germenes-infecciosos/hoja-informativa-h-pylori (accessed on 20 November 2024).
- Malfertheiner, P.; Camargo, M.C.; El-Omar, E.; Liou, J.M.; Peek, R.; Schulz, C.; Smith, S.I.; Suerbaum, S. Helicobacter pylori infection. Nat. Rev. Dis. Prim. 2023, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Diana Eugenia Guaya Iñiguez. Determinación del Antígeno Helicobacter pylori por el Método de Inmunocromatografía en los Estudiantes del Instituto Tecnológico 12 de Febrero de Zamora y su Relación con los Factores de Riesgo. 2015. Available online: https://dspace.unl.edu.ec/jspui/bitstream/123456789/13551/1/DIANA%20GUAYA-TESIS.pdf (accessed on 22 October 2024).
- Escudero Silva, N. Incidencia de Gastritis por Helicobacter Pylori en personas Atendidas en la Clinica San Pablo de Trujillo en Enero a Junio del 2018; Pedro Ruíz Gallo: Leganes, Spain, 2019. [Google Scholar]
- Thrastardottir, T.O.; Copeland, V.J.; Constantinou, C. The Association Between the Gut Microbiome, Nutritional Habits, Antibiotics, and Gastric Cancer: A Scoping Review. Curr. Nutr. Rep. 2022, 11, 19–38. Available online: https://pubmed.ncbi.nlm.nih.gov/35020173/ (accessed on 22 October 2024). [CrossRef] [PubMed]
- Korotkaya, Y.; Shores, D. Helicobacter pylori in pediatric patients. Pediatr. Rev. 2020, 41, 585–592. Available online: https://pubmed.ncbi.nlm.nih.gov/33139411/ (accessed on 28 October 2024). [CrossRef] [PubMed]
- Assaad, S.; Chaaban, R.; Tannous, F.; Costanian, C. Dietary Habits and Helicobacter pylori Infection: A Cross Sectional Study at a Lebanese Hospital. 2018. Available online: https://pubmed.ncbi.nlm.nih.gov/29661143/ (accessed on 28 October 2024).
- Baradaran, A.; Dehghanbanadaki, H.; Sara Naderpour, L.M.P. Asociación Entre Helicobacter pylori y Obesidad: Una Revisión Sistemática y Metanálisis de Estudios de Casos y Controles. Diabetes Clínica y Endocrinol. 2021. Available online: https://pubmed.ncbi.nlm.nih.gov/34243821/ (accessed on 29 October 2024).
- Estrada-Cherres, J.P.; Murillo-Zavala, A.M.; Viñanzaca-López, J.P.; Reivan-Ortiz, G.G. Helicobacter pylori y su Relación con Trastornos de la Conducta Alimentaria en Adultos Atendidos en Gastroenterología del Hospital Universitario Católico. 2024. Available online: https://www.investigarmqr.com/ojs/index.php/mqr/article/view/929 (accessed on 29 October 2024).
- Aguilar Gamboa, A.A. Prevalencia de Enteroparasitosis y Helicobacter pylori en Niños del Distrito de Santa Rosa, La Mar—Ayacucho 2022. Repos Univ Nac San Cris Huamanga. 2024. Available online: https://repositorio.unsch.edu.pe/handle/20.500.14612/6799 (accessed on 29 October 2024).
- López Peñas, D.; Naranjo Rodríguez, A.; Muñoz Molinero, J.; Rodríguez López, F.; Gálvez Calderón, C.; Chicano Gallardo, M.; Gallardo, M.C.; Fugarolas, G.M. Eficacia de la determinación fecal de Helicobacter pylori mediante la técnica HpSA en enfermos con hemorragia digestiva alta. Gastroenterol. Hepatol. 2001, 24, 5–8. [Google Scholar] [PubMed]
- Gildner, T.E.; Urlacher, S.S.; Nemeth, K.L.; Beauregard, J.A.; Pfaff Nash, M.; Zhang, A.; Waimon, S.; Cepon-Robins, T.J. Dual burden of infectious and chronic disease in low-resource U.S. communities: Examining relationships between infection, adiposity, and inflammation. Ann. Hum. Biol. 2024, 51, 2368851. Available online: https://www.researchgate.net/publication/381772430_Dual_burden_of_infectious_and_chronic_disease_in_low-resource_US_communities_examining_relationships_between_infection_adiposity_and_inflammation (accessed on 29 October 2024). [CrossRef] [PubMed]
- Sun, M.; Zhang, Z.; Zhang, J.; Zhang, J.; Jia, Z.; Zhao, L.; Han, X.; Sun, X.; Zong, J.; Zhu, Y.; et al. Causal relationships of Helicobacter pylori and related gastrointestinal diseases on Type 2 diabetes: Univariable and Multivariable Mendelian randomization. PLoS ONE 2024, 19, e0300835. Available online: https://pubmed.ncbi.nlm.nih.gov/38652719/ (accessed on 30 October 2024). [CrossRef] [PubMed]
- Kløve, S.; Stinson, S.E.; Romme, F.O.; Butt, J.; Graversen, K.B.; Lund, M.A.V.; Fonvig, C.E.; Waterboer, T.; Perez-Perez, G.I.; Hansen, T.; et al. Helicobacter pylori seropositivity associates with hyperglycemia, but not obesity, in Danish children and adolescents. BMC Med. 2024, 22, 379. Available online: https://pubmed.ncbi.nlm.nih.gov/39256870/ (accessed on 30 October 2024). [CrossRef] [PubMed]
- Farazmand, B.; Shahsavan, M.; Eghbali, F.; Pazouki, A.; Kermansaravi, M. Comparison of Weight Loss after Roux-en-Y Gastric Bypass in Helicobacter pylori-Negative and Helicobacter pylori Eradicated Patients During Five Years Follow-Ups. 2024. Available online: https://pubmed.ncbi.nlm.nih.gov/38082012/ (accessed on 30 October 2024).
- Iqbal, N.T.; Syed, S.; Sadiq, K.; Khan, M.N.; Iqbal, J.; Ma, J.Z.; Umrani, F.; Ahmed, S.; Maier, E.A.; Denson, L.A.; et al. Study of Environmental Enteropathy and Malnutrition (SEEM) in Pakistan: Protocols for Biopsy Based Biomarker Discovery and Validation. 2019. Available online: https://pubmed.ncbi.nlm.nih.gov/31331393/ (accessed on 30 October 2024).
- Sharma, P.; Singh, S.; Das, K.; Mahant, S.; Das, R. Dysbiosis of gut microbiota due to diet, alcohol intake, body mass index, and gastrointestinal diseases in India. Appl. Microbiol. Biotechnol. 2023, 107, 2547–2560. Available online: https://pubmed.ncbi.nlm.nih.gov/36929191/ (accessed on 30 October 2024). [CrossRef] [PubMed]
- Xu, X.; Qian, Y.; Jin, K.; Chen, J.; Fu, J.; Chen, C.; Zhu, Z. The Impact of Helicobacter pylori Infection on Low Skeletal Muscle Mass Risk in Chinese Women over 40: A Cross-Sectional Analysis. 2023. Available online: https://pubmed.ncbi.nlm.nih.gov/38235492/ (accessed on 31 October 2024).

| Mean | Standard Deviation | |
|---|---|---|
| Height (centimeters) | 159.82 | ±9.6 |
| Weight (kilograms) | 64.22 | ±17.35 |
| IMC (kilograms/square meter) | 24.9 | ±5.20 |
| Mean | Standard Deviation | |
|---|---|---|
| Protein | 8.67 | ± 2.26 |
| Minerals | 3.01 | ± 0.72 |
| Body Fat Mass (BFM, kilograms) | 20.53 | ±9.85 |
| Skeletal Muscle Mass (SMM, kilograms) | 24.13 | ±6.81 |
| Percent Body Fat (PBF; percentage) | 31.19 | ±8.91 |
| Target Weight | 56.73 | ±10.40 |
| Waist–Hip Ratio (WHR, centimeters) | 0.90 | ±0.057 |
| P (Significance) Spearman Test | |
|---|---|
| Age | 0.4 |
| Sex | 0.068 |
| Skeletal Muscle Mass | 1.00 |
| Body Mass Index | 0.609 |
| Percentage Body Fat | 0.773 |
| Waist–Hip Ratio | 0.393 |
| Helicobacter pylori | Gender | |
|---|---|---|
| Chi-Square | 3.667 | 2.455 |
| Significance | 0.055 | 0.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camaño Carballo, L.; Lorenzo Hidalgo, A.E.; Romero Riaño, P.A.; Martínez-Rodríguez, A.; Loaiza Martínez, D.A. Is There a Relationship Between Helicobacter pylori Infection and Anthropometric Status? Gastrointest. Disord. 2025, 7, 21. https://doi.org/10.3390/gidisord7010021
Camaño Carballo L, Lorenzo Hidalgo AE, Romero Riaño PA, Martínez-Rodríguez A, Loaiza Martínez DA. Is There a Relationship Between Helicobacter pylori Infection and Anthropometric Status? Gastrointestinal Disorders. 2025; 7(1):21. https://doi.org/10.3390/gidisord7010021
Chicago/Turabian StyleCamaño Carballo, Lilian, Alejandro Ernesto Lorenzo Hidalgo, Paola Andrea Romero Riaño, Alejandro Martínez-Rodríguez, and Daniela Alejandra Loaiza Martínez. 2025. "Is There a Relationship Between Helicobacter pylori Infection and Anthropometric Status?" Gastrointestinal Disorders 7, no. 1: 21. https://doi.org/10.3390/gidisord7010021
APA StyleCamaño Carballo, L., Lorenzo Hidalgo, A. E., Romero Riaño, P. A., Martínez-Rodríguez, A., & Loaiza Martínez, D. A. (2025). Is There a Relationship Between Helicobacter pylori Infection and Anthropometric Status? Gastrointestinal Disorders, 7(1), 21. https://doi.org/10.3390/gidisord7010021







