Isolated Rem Sleep Behavior Disorder: A Model to Assess the Overnight Habituation of Emotional Reactivity
Abstract
1. Introduction
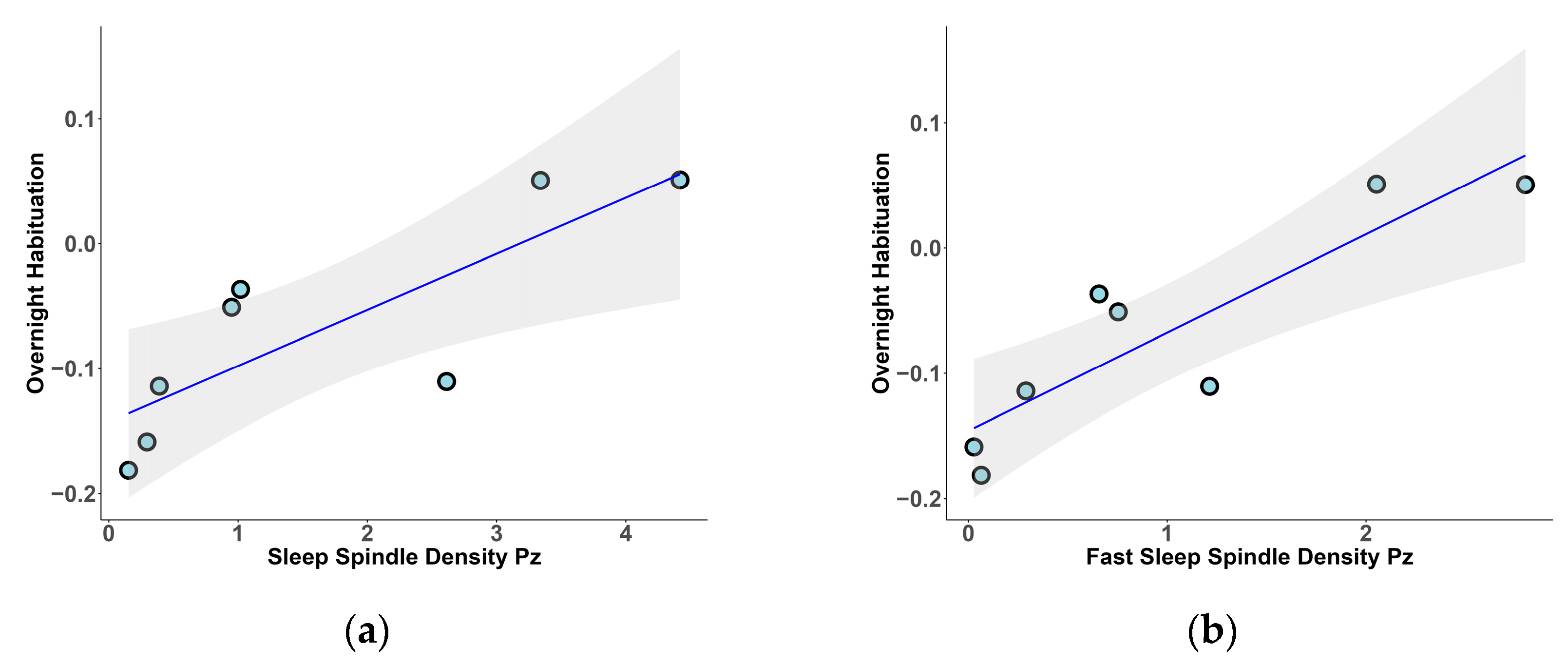
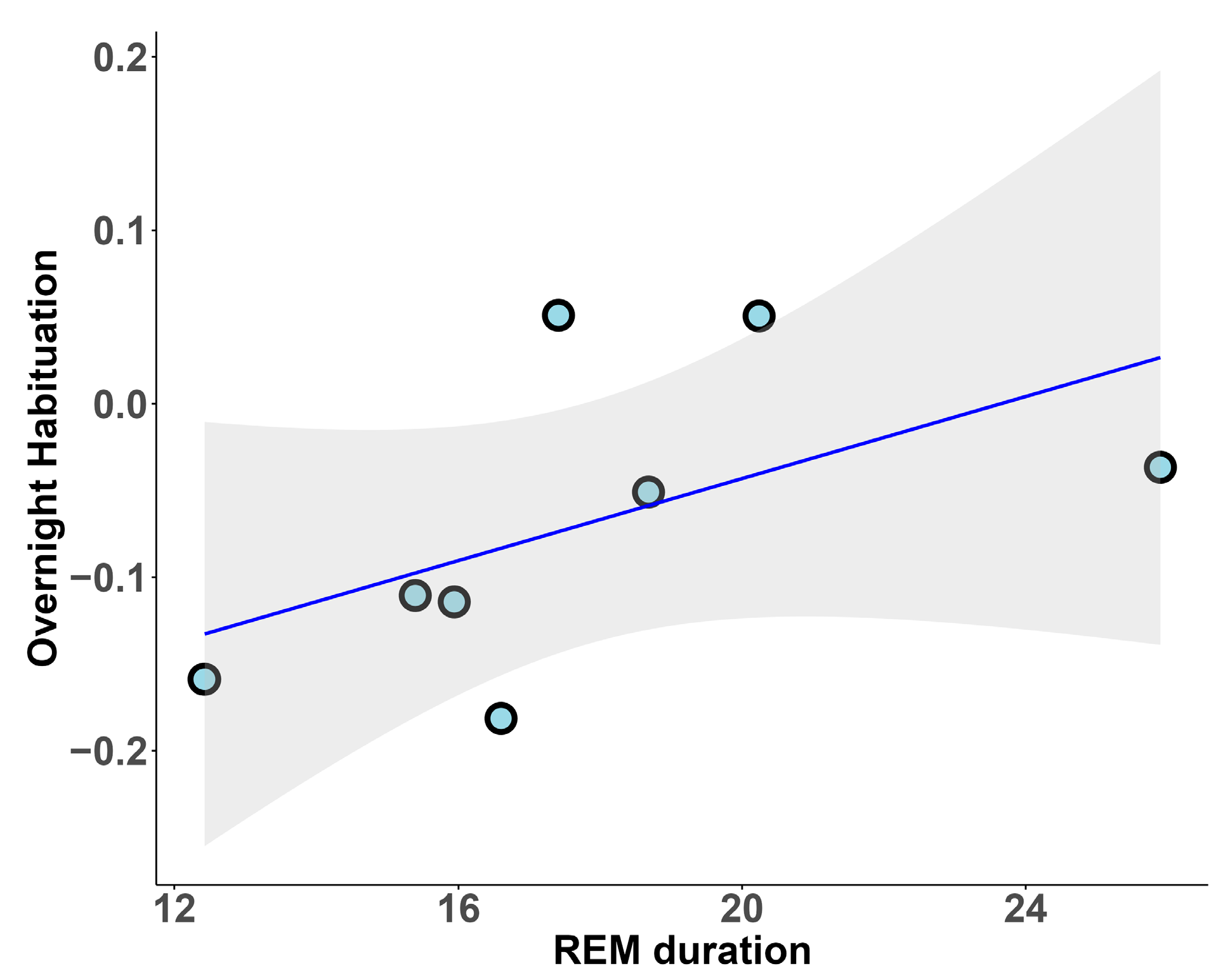
- to explore the relationship between distinct sleep stages, with a particular focus on REM sleep and SSs, and the overnight habituation of emotional reactivity in a sample of elderly individuals, including both HCs and iRBD patients;
- to evaluate the relationship between phasic events in REM sleep and alterations in overnight habituation of emotional reactivity;
- to investigate emotional dysregulation in iRBD patients using questionnaires and an arousal rating task.
2. Results
3. Discussion
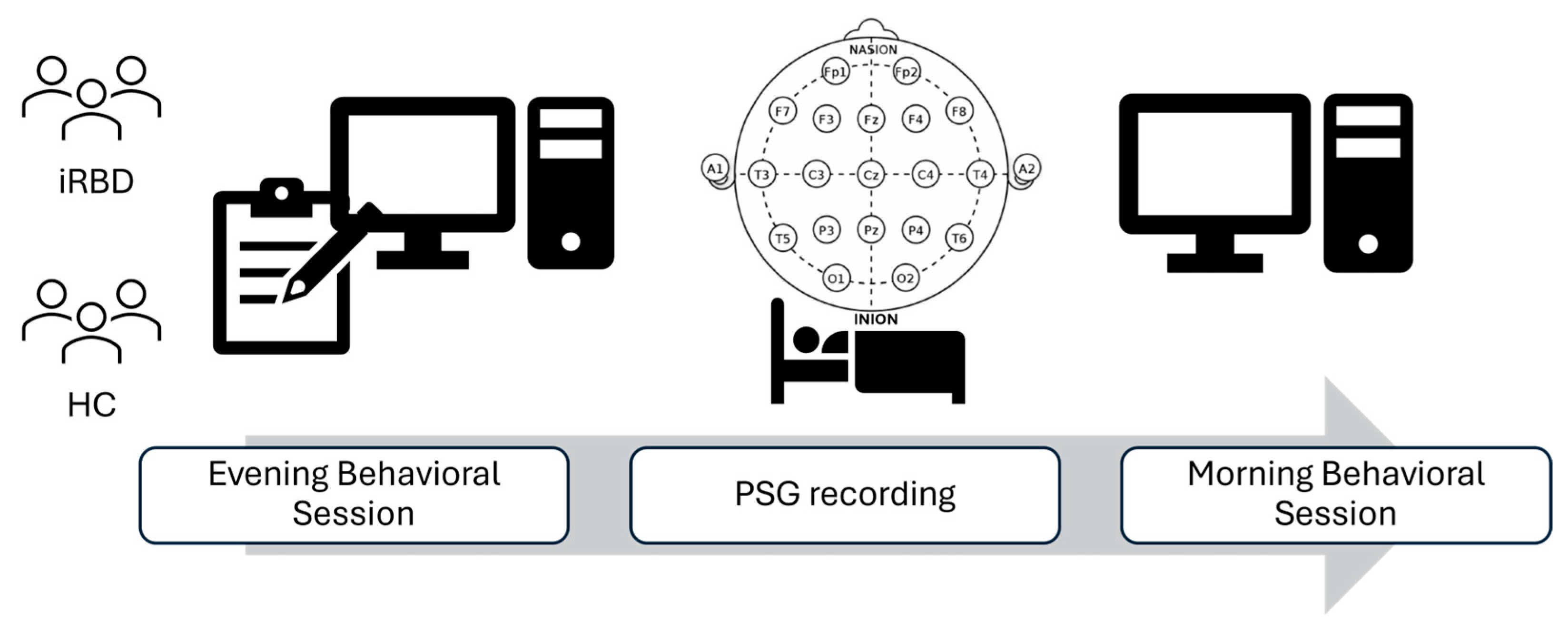
4. Materials and Methods
4.1. Subjects
- No history of psychiatric, neurologic, or sleep disorders (other than iRBD in the pathological group) and no current use of psychoactive drugs or habitual use of marijuana. Not under the influence of any medication or substance that could directly affect sleep;
- Normal or corrected to normal vision and good sleep quality.
4.2. Procedure
4.3. Materials
- Beck Depression Inventory (BDI) for the assessment of depressive symptoms [38]. The BDI is a self-report scale consisting of 21 items on a four-point scale assessing symptoms and attitudes. Higher scores reflect more severe depressive symptomatology;
- State-Trait Anxiety Inventory (STAI) for the assessment of anxiety [39]. The STAI includes two different scales: STAI-Y-1 measuring state anxiety, based on the subject feeling “at that moment”, and STAI-Y-2 measuring trait anxiety, based on the subject’s general feelings. Both scales include 20 items. Higher scores indicate higher levels of anxiety;
- Dimensional Apathy Scale (DAS) for the evaluation of apathy [40]. The DAS is a self-report questionnaire consisting of 24 items rated on a four-point Likert-type scale (from “hardly ever” to “almost always”). The scale assesses three apathy subtypes: (1) executive apathy, characterized by impairments associated with planning, attention, or organization; (2) emotional apathy, defined by difficulties in emotion integration; and (3) initiation apathy, related to the lack of motivation for self-generation of behaviors or cognition;
- DERS for the assessment of emotion dysregulation [41]. The DERS is a self-report inventory including six factors: (1) “non-acceptance of emotional responses”; (2) “difficulties in distracting with emotion and performing alternate behavior”; (3) “lack of confidence in emotional regulation skills”; (4) “difficulties in behavioral control”; (5) “difficulty in recognizing emotions”; and (6) “reduced emotional self-awareness”. Participants are asked to indicate their agreement with 36 items on a five-point Likert-type scale (from “almost never” to “almost always”). Higher scores indicate greater difficulties in regulating emotion.
4.4. PSG Recording
4.5. Sleep Stages
4.5.1. NREM Sleep Microstructure
4.5.2. REM Sleep Microstructure
4.6. Experimental Task
4.7. Statistical Analyses
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tempesta, D.; Socci, V.; De Gennaro, L.; Ferrara, M. Sleep and emotional processing. Sleep Med. Rev. 2018, 40, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Braun, A.R.; Balkin, T.J.; Wesensten, N.J.; Carson, R.E.; Varga, M.; Baldwin, P.; Selbie, S.; Belenky, G.; Herscovitch, P. Regional cerebral blood flow throughout the sleep-wake cycle An H2(15)O PET study. Brain 1997, 120, 1173–1197. [Google Scholar] [CrossRef] [PubMed]
- Dang-Vu, T.T.; Schabus, M.; Desseilles, M.; Sterpenich, V.; Bonjean, M.; Maquet, P. Functional Neuroimaging Insights into the Physiology of Human Sleep. Sleep 2010, 33, 1589–1603. [Google Scholar] [CrossRef] [PubMed]
- Van Der Helm, E.; Walker, M.P. Sleep and emotional memory processing. Sleep Med. Clin. 2011, 6, 31–43. [Google Scholar] [CrossRef]
- Luppi, P.H.; Chancel, A.; Malcey, J.; Cabrera, S.; Fort, P.; Maciel, R.M. Which structure generates paradoxical (REM) sleep: The brainstem, the hypothalamus, the amygdala or the cortex? Sleep Med. Rev. 2024, 74, 101907. [Google Scholar] [CrossRef]
- Rasch, B.; Born, J. Maintaining memories by reactivation. Curr. Opin. Neurobiol. 2007, 17, 698–703. [Google Scholar] [CrossRef]
- Vanderheyden, W.M.; Poe, G.R.; Liberzon, I. Trauma exposure and sleep: Using a rodent model to understand sleep function in PTSD. Exp. Brain Res. 2014, 232, 1575–1584. [Google Scholar] [CrossRef]
- Klinzing, J.G.; Niethard, N.; Born, J. Mechanisms of systems memory consolidation during sleep. Nat. Neurosci. 2019, 22, 1598–1610. [Google Scholar] [CrossRef]
- Walker, M.P. The role of sleep in cognition and emotion. Ann. N. Y. Acad. Sci. 2009, 1156, 168–197. [Google Scholar] [CrossRef]
- Goldstein, A.N.; Walker, M.P. The role of sleep in emotional brain function. Annu. Rev. Clin. Psychol. 2014, 10, 679–708. [Google Scholar] [CrossRef]
- Pace-Schott, E.F.; Shepherd, E.; Spencer, R.M.C.; Marcello, M.; Tucker, M.; Propper, R.E.; Stickgold, R. Napping promotes inter-session habituation to emotional stimuli. Neurobiol. Learn. Mem. 2011, 95, 24–36. [Google Scholar] [CrossRef] [PubMed]
- Werner, G.G.; Schabus, M.; Blechert, J.; Kolodyazhniy, V.; Wilhelm, F.H. Pre- to postsleep change in psychophysiological reactivity to emotional films: Late-night REM sleep is associated with attenuated emotional processing. Psychophysiology 2015, 52, 813–825. [Google Scholar] [CrossRef] [PubMed]
- Deliens, G.; Peigneux, P. One night of sleep is insufficient to achieve sleep-to-forget emotional decontextualisation processes. Cogn. Emot. 2014, 28, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Werner, G.G.; Schabus, M.; Blechert, J.; Wilhelm, F.H. Differential Effects of REM Sleep on Emotional Processing: Initial Evidence for Increased Short-term Emotional Responses and Reduced Long-term Intrusive Memories. Behav. Sleep Med. 2021, 19, 83–98. [Google Scholar] [CrossRef]
- Cairney, S.A.; Durrant, S.J.; Power, R.; Lewis, P.A. Complementary roles of slow-wave sleep and rapid eye movement sleep in emotional memory consolidation. Cereb. Cortex 2015, 25, 1565–1575. [Google Scholar] [CrossRef]
- Wassing, R.; Lakbila-Kamal, O.; Ramautar, J.R.; Stoffers, D.; Schalkwijk, F.; Van Someren, E.J.W. Restless REM Sleep Impedes Overnight Amygdala Adaptation. Curr. Biol. 2019, 29, 2351–2358.e4. [Google Scholar] [CrossRef]
- Cairney, S.A.; Durrant, S.J.; Jackson, R.; Lewis, P.A. Sleep spindles provide indirect support to the consolidation of emotional encoding contexts. Neuropsychologia 2014, 63, 285–292. [Google Scholar] [CrossRef]
- Pillai, V.; Kalmbach, D.A.; Ciesla, J.A. A Meta-Analysis of Electroencephalographic Sleep in Depression: Evidence for Genetic Biomarkers. Biol. Psychiatry 2011, 70, 912–919. [Google Scholar] [CrossRef]
- Baglioni, C.; Nanovska, S.; Regen, W.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Reynolds, C.F.; Riemann, D. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 2016, 142, 969–990. [Google Scholar] [CrossRef]
- Palmer, C.A.; Bower, J.L.; Cho, K.W.; Clementi, M.A.; Lau, S.; Oosterhoff, B.; Alfano, C.A. Sleep Loss and Emotion: A Systematic Review and Meta-Analysis of Over 50 Years of Experimental Research. Psychol. Bull. 2023, 150, 440–463. [Google Scholar] [CrossRef]
- Wittchen, H.U.; Jacobi, F.; Rehm, J.; Gustavsson, A.; Svensson, M.; Jönsson, B.; Olesen, J.; Allgulander, C.; Alonso, J.; Faravelli, C.; et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 655–679. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Krone, L.B.; Wulff, K.; Nissen, C. Sleep, insomnia, and depression. Neuropsychopharmacology 2020, 45, 74–89. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Regen, W.; Teghen, A.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Riemann, D. Sleep changes in the disorder of insomnia: A meta-analysis of polysomnographic studies. Sleep Med. Rev. 2014, 18, 195–213. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders (ICSD-3); American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- Barber, T.R.; Griffanti, L.; Muhammed, K.; Drew, D.S.; Bradley, K.M.; McGowan, D.R.; Crabbe, M.; Lo, C.; Mackay, C.E.; Husain, M.; et al. Apathy in rapid eye movement sleep behaviour disorder is associated with serotonin depletion in the dorsal raphe nucleus. Brain 2018, 141, 2848–2854. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, S.J.; Lee, S.A. Severity of idiopathic rapid eye movement sleep behavior disorder correlates with depression and alexithymia. Sleep Med. 2020, 74, 25–30. [Google Scholar] [CrossRef]
- Högl, B.; Stefani, A.; Videnovic, A. Idiopathic REM sleep behaviour disorder and neurodegeneration—An update. Nat. Rev. Neurol. 2018, 14, 40–56. [Google Scholar] [CrossRef]
- Galbiati, A.; Verga, L.; Giora, E.; Zucconi, M.; Ferini-Strambi, L. The risk of neurodegeneration in REM sleep behavior disorder: A systematic review and meta-analysis of longitudinal studies. Sleep Med. Rev. 2019, 43, 37–46. [Google Scholar] [CrossRef]
- Poewe, W.; Seppi, K.; Tanner, C.M.; Halliday, G.M.; Brundin, P.; Volkmann, J.; Schrag, A.E.; Lang, A.E. Parkinson disease. Nat. Rev. Dis. Primers 2017, 3, 1–21. [Google Scholar] [CrossRef]
- Schapira, A.H.V.; Chaudhuri, K.R.; Jenner, P. Non-motor features of Parkinson disease. Nat. Rev. Neurosci. 2017, 18, 435–450. [Google Scholar] [CrossRef]
- Assogna, F.; Pellicano, C.; Savini, C.; Macchiusi, L.; Pellicano, G.R.; Alborghetti, M.; Caltagirone, C.; Spalletta, G.; Pontieri, F.E. Drug Choices and Advancements for Managing Depression in Parkinson’s Disease. Curr. Neuropharmacol. 2019, 18, 277–287. [Google Scholar] [CrossRef]
- Christensen, J.A.E.; Kempfner, J.; Zoetmulder, M.; Leonthin, H.L.; Arvastson, L.; Christensen, S.R.; Sorensen, H.B.; Jennum, P. Decreased sleep spindle density in patients with idiopathic REM sleep behavior disorder and patients with Parkinson’s disease. Clin. Neurophysiol. 2014, 125, 512–519. [Google Scholar] [CrossRef] [PubMed]
- Sunwoo, J.S.; Cha, K.S.; Byun, J.I.; Jun, J.S.; Kim, T.J.; Shin, J.W.; Lee, S.-T.; Jung, K.-H.; Park, K.-I.; Chu, K.; et al. Nonrapid eye movement sleep electroencephalographic oscillations in idiopathic rapid eye movement sleep behavior disorder: A study of sleep spindles and slow oscillations. Sleep 2021, 44, zsaa160. [Google Scholar] [CrossRef] [PubMed]
- Gorgoni, M.; Galbiati, A. Non-REM sleep electrophysiology in REM sleep behaviour disorder: A narrative mini-review. Neurosci. Biobehav. Rev. 2022, 142, 104909. [Google Scholar] [CrossRef] [PubMed]
- Cairney, S.A.; Guttesen Aá, V.; El Marj, N.; Staresina, B.P. Memory Consolidation Is Linked to Spindle-Mediated Information Processing during Sleep. Curr. Biol. 2018, 28, 948–954.e4. [Google Scholar] [CrossRef]
- Rasch, B.; Born, J. About Sleep’s Role in Memory. Physiol. Rev. 2013, 93, 681–766. [Google Scholar] [CrossRef]
- Hutchison, I.C.; Pezzoli, S.; Tsimpanouli, M.E.; Abdellahi, M.E.A.; Lewis, P.A. Targeted memory reactivation in REM but not SWS selectively reduces arousal responses. Commun. Biol. 2021, 4, 404. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Ball, R.; Ranieri, W.F. Comparison of Beck Depression Inventories-IA and-II in Psychiatric Outpatients. J. Personal. Assess. 1996, 67, 588–597. [Google Scholar] [CrossRef]
- Spielberger, C. Manual for the State-Trait Anxiety Inventory; Spieberger, C.D., Ed.; STAI Manual; Consulting Psychologist Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Radakovic, R.; Abrahams, S. Developing a new apathy measurement scale: Dimensional Apathy Scale. Psychiatry Res. 2014, 219, 658–663. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Frauscher, B.; Iranzo, A.; Gaig, C.; Gschliesser, V.; Guaita, M.; Raffelseder, V.; Ehrmann, L.; Sola, N.; Salamero, M.; Tolosa, E.; et al. Normative EMG values during REM sleep for the diagnosis of REM sleep behavior disorder. Sleep 2012, 35, 835–847. [Google Scholar] [CrossRef]
- Zucconi, M.; Ferri, R.; Allen, R.; Baier, P.C.; Bruni, O.; Chokroverty, S.; Ferinistrambi, L.; Fulda, S.; Garciaborreguero, D.; Hening, W.A.; et al. The official World Association of Sleep Medicine (WASM) standards for recording and scoring periodic leg movements in sleep (PLMS) and wakefulness (PLMW) developed in collaboration with a task force from the International Restless Legs Syndrome Study Group (IRLSSG). Sleep Med. 2006, 7, 175–183. [Google Scholar] [PubMed]
- Berry, R.B.; Brooks, R.; Gamaldo, C.; Harding, S.M.; Lloyd, R.M.; Quan, S.F.; Troester, M.T.; Vaughn, B.V. AASM scoring manual updates for 2017 (version 2.4). J. Clin. Sleep Med. 2017, 13, 665–666. [Google Scholar] [CrossRef] [PubMed]
- Vallat, R.; Walker, M.P. An open-source, high-performance tool for automated sleep staging. eLife 2021, 10, 70092. [Google Scholar] [CrossRef] [PubMed]
- Lang, P.J.; Bradley, M.M.; Cuthbert, B.N. International Affective Picture System (IAPS): Affective Ratings of Pictures and Instruction Manual; Technical Report A-6; The Center for Research in Psychophysiology, University of Florida: Gainesville, FL, USA, 2005. [Google Scholar]
- Bradley, M.M.; Lang, P.J. International Affective Digitized Sounds (IADS): Stimuli, Instruction Manual and Affective Ratings; Technical Report No B-2; The Center for Research in Psychophysiology, University of Florida: Gainesville, FL, USA, 1999. [Google Scholar]



| PSG Parameters | Group | Mean ± SD | Mean Rank | U Statistic | p |
|---|---|---|---|---|---|
| SE | HC | 83.47 ± 13.26 | 9.25 | 26 | 0.574 |
| iRBD | 77.13 ± 18.27 | 7.75 | |||
| TIB | HC | 497.50 ± 41.78 | 10 | 20 | 0.234 |
| iRBD | 469.69 ± 19.25 | 7 | |||
| TST | HC | 417.56 ± 84.76 | 10.50 | 16 | 0.105 |
| iRBD | 358.50 ± 86.79 | 6.50 | |||
| WASO | HC | 68.06 ± 51.39 | 7.38 | 33 | 0.613 |
| iRBD | 98.29 ± 83.38 | 8.71 | |||
| SOL N1 | HC | 4.44 ± 4.13 | 5.44 | 48.50 | 0.014 * |
| iRBD | 10.79 ± 3.59 | 10.93 | |||
| SOL N2 | HC | 16.06 ± 10.83 | 5.88 | 45 | 0.054 |
| iRBD | 41.14 ± 29.89 | 10.43 | |||
| %N1 | HC | 17.08 ± 8.65 | 7.88 | 37 | 0.645 |
| iRBD | 21.77 ± 10.70 | 9.12 | |||
| %N2 | HC | 57.88 ± 8.99 | 10.25 | 18 | 0.161 |
| iRBD | 50.33 ± 9.80 | 6.75 | |||
| %N3 | HC | 7.21 ± 10.26 | 9.25 | 26 | 0.574 |
| iRBD | 5.21 ± 8.67 | 7.75 | |||
| %REM | HC | 17.82 ± 4.00 | 6.88 | 45 | 0.195 |
| iRBD | 22.69 ± 8.33 | 10.12 | |||
| REM latency | HC | 99.50 ± 47.01 | 6.38 | 49 | 0.041 * |
| iRBD | 182.81 ± 102.13 | 10.62 | |||
| REMs density | HC | 3.22 ± 1.46 | 4.50 | 56 | <0.001 * |
| iRBD | 8.19 ± 2.82 | 12 | |||
| REM arousal index | HC | 0.23 ± 0.10 | 6 | 44 | 0.036 * |
| iRBD | 0.35 ± 0.11 | 10.29 | |||
| REM arousal and awakening index | HC | 0.29 ± 0.12 | 6.75 | 38 | 0.281 |
| iRBD | 0.38 ± 0.12 | 9.43 | |||
| SS density N2 Cz | HC | 1.10 ± 1.12 | 9 | 20 | 0.397 |
| iRBD | 0.59 ± 0.64 | 6.86 | |||
| SS density N2 Pz | HC | 1.65 ± 1.60 | 8.62 | 23 | 0.613 |
| iRBD | 1.22 ± 0.98 | 7.29 |
| PSG Parameters | Group | Mean ± SD | Mean Rank | U Statistic | p |
|---|---|---|---|---|---|
| DERS Total | HC | 70.37 ± 17.83 | 7.75 | 38 | 0.574 |
| iRBD | 76.75 ± 17.55 | 9.25 | |||
| DERS Non-Acceptance | HC | 10.00 ± 3.25 | 6.69 | 46.50 | 0.130 |
| iRBD | 13.00 ± 3.89 | 10.31 | |||
| DERS Goals | HC | 13.87 ± 5.38 | 9.56 | 23.50 | 0.382 |
| iRBD | 11.50 ± 2.73 | 7.44 | |||
| DERS Impulsiveness | HC | 9.50 ± 4.21 | 6.75 | 46 | 0.161 |
| iRBD | 13.37 ± 5.10 | 10.25 | |||
| DERS Awareness | HC | 14.62 ± 5.34 | 9.50 | 24 | 0.442 |
| iRBD | 12.12 ± 5.36 | 7.50 | |||
| DERS Strategies | HC | 14.37 ± 4.69 | 6.69 | 46.50 | 0.130 |
| iRBD | 17.75 ± 4.68 | 10.31 | |||
| DERS Clarity | HC | 8.00 ± 2.51 | 8.44 | 32.50 | 1.00 |
| iRBD | 8.87 ± 4.61 | 8.56 | |||
| BDI | HC | 5.37 ± 5.34 | 7.75 | 38 | 0.574 |
| iRBD | 6.00 ± 2.39 | 9.25 | |||
| STAI-Y1 | HC | 29.37 ± 8.42 | 7.50 | 40 | 0.442 |
| iRBD | 34.57 ± 13.38 | 9.50 | |||
| STAI-Y2 | HC | 32.37 ± 12.12 | 7.38 | 41 | 0.382 |
| iRBD | 34.25 ± 7.46 | 9.62 | |||
| DAS Executive | HC | 7.62 ± 4.81 | 10.81 | 13.50 | 0.057 |
| iRBD | 3.62 ± 1.92 | 6.19 | |||
| DAS Emotional | HC | 7.37 ± 4.63 | 8.25 | 34 | 0.878 |
| iRBD | 7.37 ± 3.20 | 8.75 | |||
| DAS Behavior and Cognition | HC | 9.25 ± 3.99 | 9.38 | 25 | 0.505 |
| iRBD | 6.62 ± 4.14 | 7.62 | |||
| DAS Total | HC | 24.25 ± 7.05 | 10.50 | 16 | 0.105 |
| iRBD | 17.62 ± 7.11 | 6.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leitner, C.; Greco, V.; Casoni, F.; Lewis, P.A.; Ferini-Strambi, L.; Galbiati, A. Isolated Rem Sleep Behavior Disorder: A Model to Assess the Overnight Habituation of Emotional Reactivity. Clocks & Sleep 2025, 7, 9. https://doi.org/10.3390/clockssleep7010009
Leitner C, Greco V, Casoni F, Lewis PA, Ferini-Strambi L, Galbiati A. Isolated Rem Sleep Behavior Disorder: A Model to Assess the Overnight Habituation of Emotional Reactivity. Clocks & Sleep. 2025; 7(1):9. https://doi.org/10.3390/clockssleep7010009
Chicago/Turabian StyleLeitner, Caterina, Viviana Greco, Francesca Casoni, Penelope A. Lewis, Luigi Ferini-Strambi, and Andrea Galbiati. 2025. "Isolated Rem Sleep Behavior Disorder: A Model to Assess the Overnight Habituation of Emotional Reactivity" Clocks & Sleep 7, no. 1: 9. https://doi.org/10.3390/clockssleep7010009
APA StyleLeitner, C., Greco, V., Casoni, F., Lewis, P. A., Ferini-Strambi, L., & Galbiati, A. (2025). Isolated Rem Sleep Behavior Disorder: A Model to Assess the Overnight Habituation of Emotional Reactivity. Clocks & Sleep, 7(1), 9. https://doi.org/10.3390/clockssleep7010009







