Abstract
Social jetlag is associated with physical and mental health problems. With the increased popularity of telework, we investigated a specific form of social jetlag that we termed “telework jetlag”. This study aimed to clarify the relationship between telework jetlag—the difference in sleep and wake-up times between in-office and telework days—and mental health problems among Japanese hybrid workers. A cross-sectional study was conducted with 1789 participants from October to December 2021 using an online-based questionnaire. Telework jetlag, defined as the difference in the midsleep point between in-office and telework days, was investigated using two groups according to telework jetlag—those lagging <1 h versus ≥1 h. We used the six-item Kessler Scale as a nonspecific psychological distress scale for the outcome. Telework jetlag was significantly associated with psychological distress, and the ≥1 h group had a higher risk (odds ratio: 1.80) of developing high psychological distress (HPD) than the <1 h group in the multivariate analysis. Since most teleworkers are forced to have a hybrid work style that mixes going to work and teleworking, telework jetlag must be addressed to maintain the health of teleworkers.
Keywords:
telework; social jetlag; sleep; midsleep point; psychological distress; mental health; Japanese 1. Introduction
Social jetlag refers to the difference in sleep timing (the times of going to bed and waking up) between duty days (days when individuals must go to school or work) and free days when the two alternate [1]. On free days, people usually wake up at the time of their choice, while on duty days, they must wake up according to work or school start times. In particular, those who live far from their workplace or school wake up earlier to accommodate travel time. Besides that, social jetlag is also associated with various lifestyle factors such as smoking, caffeine intake, alcohol consumption, and exercise [1,2], as industrialized countries, more than 70% of the population has over 1 h of social jetlag [1,3,4]. Social jetlag is associated with physical and mental health problems such as obesity, metabolic diseases, malignant tumors, and psychiatric disorders resulting from the disruption of circadian rhythms [4,5,6,7,8,9,10,11]. These mechanisms involve abnormal rhythms of glucocorticoid secretion and postprandial glucose response during the internal desynchronization of circadian rhythms [12], abnormal diurnal rhythms of gene expression [13], stress responses, such as elevated blood cortisol levels and resting heart rate [2], and mood instability [14].
A new way of working has become popular since the outbreak of the COVID-19 pandemic in 2020: teleworking. Telework eliminates commuting time and thus decreases social jetlag [15,16,17,18,19]. Telework is expected to contribute to not only convenience, but also the prevention of social jetlag.
However, there is concern that those who partake in teleworking, a phenomenon which spread rapidly after the COVID-19 pandemic, have inadequate knowledge of how to maintain good health [20,21]. Some studies have reported that teleworking could have various effects on mental health, such as increased stress due to the difficulty of separating work and personal life and social isolation due to the lack of face-to-face interactions [22,23,24,25,26,27,28]. Individual differences in the benefits and harms of telework have also been reported, and various work conditions such as telework frequency, location, social support, etc., may cause them [29].
In addition to those issues, we are concerned about the potential for new work styles, including telework, to cause a new jetlag. Few jobs can be completed entirely via telework, and almost all people must visit the workplace several times each week or month. Therefore, most teleworkers have a hybrid work style that combines going to the workplace and teleworking. We named the resulting difference in sleep timing between in-office and telework days “telework jetlag”. If social jetlag can cause health problems, perhaps telework jetlag can as well.
To our knowledge, no studies have investigated the relationship between telework jetlag and mental health problems among teleworkers. In the period when early telework studies were reported, the Wi-Fi environment was not as prevalent as it is today, and the telework environment could be quite different [25,30,31]. In Japan, especially, teleworking was not widespread before the COVID-19 pandemic, and there are a few studies on sleep problems and mental health among Japanese teleworkers. We hypothesize that mental health problems for workers with a hybrid work style, mixing going to work with telework (hybrid workers), are associated with telework jetlag. This study aimed to clarify the relationship between telework jetlag and mental health problems among Japanese hybrid workers.
2. Results
2.1. Participant Characteristics
Responses were obtained from 2032 participants. Of these, 11 individuals who did not consent to participate in the study, 8 who had been on leave within the past month, and 224 who had not teleworked within the past month were excluded, leaving 1789 (1231 men and 558 women; mean age, 43.2 years; standard deviation, 11.3) individuals who were included in the analysis. The valid response rate was 60.2%. Table 1, Table 2 and Table 3 present the participants’ characteristics. There were 232 participants (13.0%) with a telework jetlag of 1 h or longer. Regarding psychological distress, 1524 (85.2%) patients were classified as having non-high psychological distress (NHPD), and 265 (14.8%) were classified as having high psychological distress (HPD).

Table 1.
Characteristics of participants regarding basic attributes.

Table 2.
Characteristics of participants regarding telework jetlag and various telework statuses.

Table 3.
Characteristics of participants regarding each scale.
2.2. Prevalence of HPD for Telework Jetlag
Table 4 shows the aggregate results based on psychological distress and telework jetlag. A higher percentage of HPD (22.0) was found in participants with ≥1 h of telework jetlag, and there was a significant difference in the χ2 test.

Table 4.
Cross-tabulation and χ2 test based on psychological distress and telework jetlag.
2.3. Characteristics of Participants Divided by Telework Jetlag
Figure 1 shows the median times of going to bed and waking up on telework and in-office days for two groups based on telework jetlag. Both groups slept longer on the telework days; however, the <1 h group went to bed 1 h earlier, while the ≥1 h group woke up 2 h later.
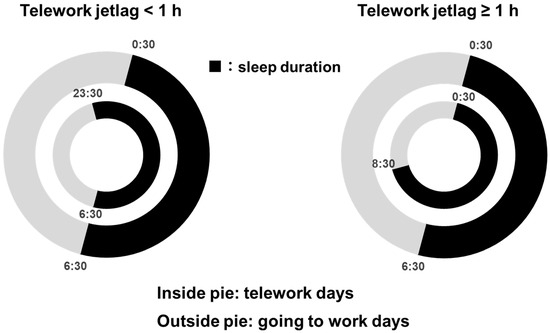
Figure 1.
Median times of going to bed and waking up for telework and in-office days divided by telework jetlag.
2.4. Odds Ratio of HPD in Telework Jetlag
The multivariate regression results are presented in Table 5. The input covariates in each model were as follows: Model 1: sex, age, living alone, telework frequency, telework location, and telework duration; Model 2: occupation, employment position, work hours in the past month, job demands, job control, supervisor support, coworker support, and all covariates of Model 1; Model 3: commuting time, means of commuting, exercise habits, drinking alcohol, consuming caffeine, current smoking status, using electronic terminal outside work, enjoying leisure time, and all covariates of Model 2; and Model 4: sleep duration, Athens Insomnia Scale score, and all covariates of Model 3. In all of the analysis models, the results of the suitability tests were good (i.e., omnibus test: p < 0.05; Hosmer–Lemeshow test: p ≥ 0.05). Telework jetlag was significantly associated with psychological distress, and the ≥1 h group had a higher risk of developing HPD than the <1 h group in all analysis models. The results for other covariates (p-value and 95% CI) are presented in the Supplementary Material (Table S1).

Table 5.
Multivariate regression analysis including variables related to telework and psychological distress.
3. Discussion
In order to establish telework as a sustainable work style, many research studies and policies that contribute to the reduction in health risks due to telework and the promotion of workers’ health are required [32,33]. This study examined the relationship between various telework jetlag and psychological distress among hybrid workers. Telework jetlag was significantly associated with psychological distress even after adjusting for confounding factors such as telework status, lifestyle habits, job stress, and sleep duration. The strength of this study is that it defined the concept of telework jetlag and found that different times of going to bed and waking up on in-office and telework days are associated with psychological distress. Telework jetlag may be a risk factor for mental health problems among hybrid workers, which is important to consider when promoting health management and health promotion among hybrid workers.
First, we discuss the characteristics of the sample population based on the outcome variables. While 10.3% of those aged 20 or above in the 2019 Comprehensive Survey of Living Conditions had six-item Kessler Scale (K6) scores ≥ 10, the percentage was 14.8% for the participants in this study [34]. Thus, the results of this study indicate a higher rate than the national average. However, as 2019 was before the COVID-19 pandemic, it is difficult to compare the results.
Next, for the results of multivariate regression, in Model 1, telework jetlag was found to be significantly associated with psychological distress, even after adjusting for telework frequency, location, and duration. This means that hybrid workers should be aware of the presence of telework jetlag regardless of these various telework statuses. Since telework jetlag is an original conception defined in this study, the factors associated with it are not clear; nevertheless, it is possible that the likelihood and influence of telework jetlag may differ depending on the occupation and work environment (job demand, job control, and social support). The results of Model 2, however, showed that there was still an association between telework jetlag and psychological distress even after adjusting for the occupation and work environment. These findings mean that telework jetlag should be noted regardless of occupation or work environment for the management of mental health in hybrid workers. Furthermore, in Model 3, telework jetlag was significantly associated with psychological distress, even after adjustment for various lifestyle factors. As mentioned earlier, social jetlag is associated with various lifestyle habits, which are also risk factors for mental health problems [35,36,37]. Therefore, the results of Model 3 suggest that telework jetlag is associated with psychological distress independently of such lifestyle habits. On the other hands, since it was pointed out that social jetlag is affected by a lack of sleep, it is recommended to correct for sleep duration [38,39,40]. However, the results of the multivariate analysis showed that the 95% CI range of Model 4 (adjusted for sleep duration) and Model 3 (unadjusted for sleep duration) remained stable. Therefore, the effect of sleep duration on telework jetlag was considered to be small. Okajima et al. stated that although social jetlag and sleep deprivation are positively correlated, their association is small and they are separate concepts [41]. The results of this study on telework jetlag also support their findings.
We also discuss the possible biological mechanisms by which telework jetlag is associated with psychological distress. It has been reported that in social jetlag, the delayed onset of melatonin causes fatigue and drowsiness that persist for several days [42]. Therefore, the disturbance of the melatonin secretion rhythm may also occur in telework jetlag, which may be related to mental condition. A meta-analysis of prospective studies showed an increase in depression among shift workers with disrupted circadian rhythms [43]. A disruption of the circadian rhythm is an important risk factor for mental disorders such as depression [44,45]. The biological mechanism is that irregular sleep timing alters the secretion patterns of hormones, such as melatonin, cortisol, and noradrenaline, which contribute to the development of depressive symptoms [12,46,47,48,49]. In particular, the wake-up times differed by 2 h between the in-office and telework days in the ≥1 h group. Since morning sunlight upon waking is a major synaptic signal for circadian rhythms, changes in wake-up times could greatly affect circadian rhythms [50,51]. However, the participants in the <1 h group woke up at the same time on in-office and telework days and went to bed 1 h earlier. Therefore, they were able to obtain sleep duration with less impact on their circadian rhythms than the ≥1 h group.
However, there is a major limitation to our discussion. If the K6 score is ≥10, a pathological mental disorder that requires medical attention is suspected. Abnormal deep body temperature rhythms and the over-secretion of cortisol, melatonin, and so on often appear in patients with depression [52,53,54,55,56,57]. Therefore, it is possible that telework jetlag is caused by symptoms of mental illness. Since this was a cross-sectional study, it was not possible to prove the temporality of the association. A longitudinal analysis is needed in the future.
Other limitations of this study are as follows: First, there is a possible selection bias because the study only included workers of companies in Tokyo, the capital of Japan. Given Tokyo’s high population density and advanced communications technology, it may have a different telework environment than rural areas. Second, because the survey was entirely self-reported and subjective, possible information bias may have made the responses less objective. Finally, there could be confounding bias due to factors that were not entered as covariates, such as household income and medication history. In particular, those with restricted employment may disproportionately belong to the HPD type.
4. Conclusions
We defined telework jetlag, which is a new concept that differs from social jetlag, as the difference in sleep timing between in-office and telework days. This study showed that telework jetlag of 1 h or more was significantly associated with mental health problems. Telework jetlag may be a risk factor for mental health problems among hybrid workers, which is important to consider when promoting health management and health promotion among hybrid workers. Since most teleworkers are forced to have a hybrid work style that mixes going to work and teleworking, telework jetlag must be addressed to maintain their health. In particular, the delay in wake-up time may need to be focused on.
Our study will contribute substantially to improving the health of teleworkers and making this work style sustainable. However, future longitudinal studies are needed to establish a causal relationship between telework jetlag and mental health problems.
5. Materials and Methods
5.1. Study Design, Participants, and Ethical Considerations
A cross-sectional study using an online-based questionnaire was conducted from October to December 2021. The participants were 2971 day shift workers employed by four companies in Tokyo who consented to participate in the survey. Since the population of Tokyo is approximately 10 million, we considered a sample size of at least 1067 persons to be sufficient, assuming a 95% confidence level, a 3% margin of error, and a population ratio of 0.5. The purpose and procedures of the study were explained to the employees. Participation was voluntary, and we explained that no disadvantages would arise from not participating in the study and that the data obtained would not be used for any purpose other than the study.
Consent for participation was obtained through a web-based response before participation, and those who did not agree were not able to access or respond to any of the research items. Since this was an anonymous study with a substitute employee ID number, they were also told that it was possible to withdraw consent after answering the study and that the responses would be deleted if consent was withdrawn. This study was conducted in accordance with the Declaration of Helsinki and its current amendments. It was approved by the Ethics Committee of the Nihon University School of Medicine (approval no. 2021-02).
5.2. Telework Jetlag and Other Telework Status
To calculate telework jetlag, we referred to the social jetlag calculation method [1]. We first determined the midsleep points on in-office and telework days. The midsleep point is the median value between the times of going to bed and waking up (e.g., if a person goes to bed at midnight and wakes up at 6:00 am, the midsleep point is 3:00 am). The items regarding the times of going to bed and waking up were phrased as follows: “What time did you (go to bed/wake up) on (in-office/telework days) in the past month?” The difference in midsleep points between in-office and telework days was defined as telework jetlag. Since social jetlag of 1 h or more was reported to be associated with health problems [6], participants in this study were also classified according to telework jetlag as <1 h or ≥1 h.
The item regarding teleworking frequency was “How much did you telework in the past month?” The choices were categorized using a five-answer method: (1) not teleworking, (2) 1 to 3 times per month, (3) 1 to 2 times per week, (4) 3 to 4 times per week, and (5) ≥5 times per week. The item regarding telework location was “Please select one location where you telework most frequently”. The choices were categorized using a four-answer method: (1) living room, (2) private room, (3) bedroom, and (4) other. The item regarding teleworking duration was “How long have you been teleworking?” The choices were categorized using a three-answer method: (1) <1 y; (2) ≥1 y and <1.5 y, and (3) ≥1.5 y. These telework statuses were entered as covariates when performing the multivariate analysis.
5.3. Psychological Distress (Outcome)
We used the K6 as a nonspecific psychological distress scale for outcomes [58]. The K6 was developed to screen for depression, anxiety disorders, and other mental health conditions, and the reliability and validity of the Japanese version were established [59,60]. It can be used in surveys of the general population and is widely used as an indicator of the degree of psychological stress. The cutoff values of the K6 are 4/5 and 9/10 points. In this study, a score of ≤9 was defined as indicating NHPD, and a score of ≥10 was defined as indicating HPD.
5.4. Other Covariates
Basic attributes, lifestyle habits, occupational stress, and insomnia were entered as covariates. The basic attributes included sex, age, presence of a roommate, occupation, employment position, commuting time, means of commuting, and work hours in the past month. Lifestyle habits included exercise, alcohol consumption, caffeine intake, current smoking habits, use of electronic terminals outside of work, enjoyment of leisure time, and sleep duration. Occupational-stress-related factors were adapted from the Brief Job Stress Questionnaire and included job demands, job control, supervisor support, and coworker support [61]. Insomnia was measured using the Athens Insomnia Scale (AIS). The AIS was developed in accordance with the diagnostic criteria for insomnia in the International Classification of Disorders, and its Japanese version was verified and validated by Okajima et al. [62,63]. The questionnaire consists of eight items with a score range of 0–24 points. The cutoff value is 5/6 points, with higher scores indicating stronger insomnia symptoms.
5.5. Statistical Analysis
The χ2 test was used for univariate analysis in cross tabulations. Multiple logistic regression was used for multivariate analysis, and odds ratios and 95% confidence intervals were calculated using the direct method. Omnibus and Hosmer–Lemeshow tests were used to assess the suitability of the analysis model. Statistical analyses were performed using SPSS for Windows Version 28.0. All tests were two-tailed with p-values < 0.05 noting statistical significance.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/2624-5175/5/4/40/s1, Table S1: 95%CI and P values of all covariates in the results of multivariate regression analysis.
Author Contributions
Conceptualization, Y.M.; methodology, Y.M., A.H. and K.K.; software, Y.M., O.I. and Y.O.; validation, Y.M. and Y.K.; formal analysis, Y.M., A.H. and Y.O.; investigation, Y.M., A.H. and K.K.; resources, Y.M. and O.I.; data curation, Y.M., A.H. and Y.O.; writing—original draft preparation, Y.M.; writing—review and editing, Y.M., A.H., K.K., O.I., Y.O. and Y.K. visualization, Y.M.; supervision, Y.M.; project administration, Y.M. and Y.K.; funding acquisition, Y.M. All authors have read and agreed to the published version of the manuscript.
Funding
Y.M. received a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology (URL: https://kaken.nii.ac.jp/en/ (accessed on 13 August 2023)) to conduct this research (no. 21K10507).
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and its current amendments. This study was approved by the Ethics Committee of the Nihon University School of Medicine (approval no. 2021-02).
Informed Consent Statement
Consent for participation was obtained through a web-based response, and those who did not agree were not able to access or respond to any research items. Since this was an anonymous study with the use of substitute employee ID numbers, participants were also told that it was possible to withdraw consent after completing the study and that the responses would be deleted if consent was withdrawn.
Data Availability Statement
The data underlying this article will be shared upon reasonable request from the corresponding authors.
Acknowledgments
We wish to thank the participants of this study and the support staff who made it possible.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Rutters, F.; Lemmens, S.G.; Adam, T.C.; Bremmer, M.A.; Elders, P.J.; Nijpels, G.; Dekker, J.M. Is social jetlag associated with an adverse endocrine, behavioral, and cardiovascular risk profile? J. Biol. Rhythms 2014, 29, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Wirz-Justice, A.; Merrow, M. Life between clocks: Daily temporal patterns of human chronotypes. J. Biol. Rhythms 2003, 18, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Allebrandt, K.V.; Merrow, M.; Vetter, C. Social jetlag and obesity. Curr. Biol. 2012, 22, 939–943. [Google Scholar] [CrossRef] [PubMed]
- Caliandro, R.; Streng, A.A.; van Kerkhof, L.W.M.; van der Horst, G.T.J.; Chaves, I. Social jetlag and related risks for human health: A timely review. Nutrients 2021, 13, 4543. [Google Scholar] [CrossRef]
- Islam, Z.; Akter, S.; Kochi, T.; Hu, H.; Eguchi, M.; Yamaguchi, M.; Kuwahara, K.; Kabe, I.; Mizoue, T. Association of social jetlag with metabolic syndrome among Japanese working population: The Furukawa Nutrition and Health Study. Sleep Med. 2018, 51, 53–58. [Google Scholar] [CrossRef]
- Hu, L.; Harper, A.; Heer, E.; McNeil, J.; Cao, C.; Park, Y.; Martell, K.; Gotto, G.; Shen-Tu, G.; Peters, C.; et al. Social jetlag and prostate cancer incidence in Alberta’s Tomorrow Project: A prospective cohort study. Cancers 2020, 12, 3873. [Google Scholar] [CrossRef]
- Islam, Z.; Hu, H.; Akter, S.; Kuwahara, K.; Kochi, T.; Eguchi, M.; Kurotani, K.; Nanri, A.; Kabe, I.; Mizoue, T. Social jetlag is associated with an increased likelihood of having depressive symptoms among the Japanese working population: The Furukawa Nutrition and Health Study. Sleep 2020, 43, zsz204. [Google Scholar] [CrossRef]
- Mota, M.C.; Silva, C.M.; Balieiro, L.C.T.; Fahmy, W.M.; Marqueze, E.C.; Moreno, C.R.C.; Crispim, C.A. Social jetlag is associated with impaired metabolic control during a 1-year follow-up. Front. Physiol. 2021, 12, 702769. [Google Scholar] [CrossRef]
- Kim, J.H.; Lyu, Y.S.; Kim, S.Y. Impact of social jetlag on weight change in adults: Korean National Health and Nutrition Examination Survey 2016–2017. Int. J. Environ. Res. Public Health 2020, 17, 4383. [Google Scholar] [CrossRef]
- Kelly, R.M.; McDermott, J.H.; Coogan, A.N. Differences in sleep offset timing between weekdays and weekends in 79,161 Adult Participants in the UK Biobank. Clocks Sleep 2020, 4, 658–674. [Google Scholar] [CrossRef] [PubMed]
- Scheer, F.A.; Hilton, M.F.; Mantzoros, C.S.; Shea, S.A. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc. Natl. Acad. Sci. USA 2009, 106, 4453–4458. [Google Scholar] [CrossRef] [PubMed]
- Archer, S.N.; Laing, E.E.; Möller-Levet, C.S.; van der Veen, D.R.; Bucca, G.; Lazar, A.S.; Santhi, N.; Slak, A.; Kabiljo, R.; von Schantz, M.; et al. Mistimed sleep disrupts circadian regulation of the human transcriptome. Proc. Natl. Acad. Sci. USA 2014, 111, E682–E691. [Google Scholar] [CrossRef] [PubMed]
- Wehr, T.A.; Wirz-Justice, A.; Goodwin, F.K.; Duncan, W.; Gillin, J.C. Phase advance of the circadian sleep-wake cycle as an antidepressant. Science 1979, 206, 710–713. [Google Scholar] [CrossRef]
- Korman, M.; Tkachev, V.; Reis, C.; Komada, Y.; Kitamura, S.; Gubin, D.; Kumar, V.; Roenneberg, T. COVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Sci. Rep. 2020, 10, 22225. [Google Scholar] [CrossRef]
- Leone, M.J.; Sigman, M.; Golombek, D.A. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr. Biol. 2020, 30, R930–R931. [Google Scholar] [CrossRef]
- Blume, C.; Schmidt, M.H.; Cajochen, C. Effects of the COVID-19 lockdown on human sleep and rest–activity rhythms. Curr. Biol. 2020, 30, R795–R797. [Google Scholar] [CrossRef]
- Bottary, R.; Fields, E.C.; Ugheoke, L.; Denis, D.; Mullington, J.M.; Cunningham, T.J. Changes in sleep regularity and perceived life stress across the COVID-19 Pandemic: A Longitudinal Analysis of a Predominately Female United States Convenience Sample. Clocks Sleep 2022, 5, 1–9. [Google Scholar] [CrossRef]
- Benedict, C.; Brandão, L.E.M.; Merikanto, I.; Partinen, M.; Bjorvatn, B.; Cedernaes, J. Meal and sleep timing before and during the COVID-19 pandemic: A cross-sectional anonymous survey study from Sweden. Clocks Sleep 2021, 3, 251–258. [Google Scholar] [CrossRef]
- Knight, C.; Olaru, D.; Lee, J.; Parker, S. The Loneliness of the Hybrid Worker. MIT Sloan Management Review. 2022. Available online: https://sloanreview.mit.edu/article/the-loneliness-of-the-hybrid-worker/ (accessed on 13 August 2023).
- Buomprisco, G.; Ricci, S.; Perri, R.; De Sio, S. Health and telework: New challenges after COVID-19 pandemic. Eur. J. Public Health 2021, 5, em0073. [Google Scholar] [CrossRef]
- Tavares, A.I. Telework and health effects review. Int. J. Health Care 2017, 3, 30–36. [Google Scholar] [CrossRef]
- Vander Elst, T.; Verhoogen, R.; Sercu, M.; Van den Broeck, A.; Baillien, E.; Godderis, L. Not extent of telecommuting, but job characteristics as proximal predictors of work-related well-being. J. Occup. Environ. Med. 2017, 59, e180–e186. [Google Scholar] [CrossRef] [PubMed]
- Evanoff, B.A.; Strickland, J.R.; Dale, A.M.; Hayibor, L.; Page, E.; Duncan, J.G.; Kannampallil, T.; Gray, D.L. Work-related and personal factors associated with mental well-being during the COVID-19 response: Survey of health care and other workers. J. Med. Internet Res. 2020, 22, e21366. [Google Scholar] [CrossRef] [PubMed]
- Mann, S.; Holdsworth, L. The psychological impact of teleworking: Stress, emotions and health. New Technol. Work Employ. 2003, 18, 196–211. [Google Scholar] [CrossRef]
- Niu, Q.; Nagata, T.; Fukutani, N.; Tezuka, M.; Shimoura, K.; Nagai-Tanima, M.; Aoyama, T. Health effects of immediate telework introduction during the COVID-19 era in Japan: A cross-sectional study. PLoS ONE 2021, 16, e0256530. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.; Hauret, L.; Fuhrer, C. Digitally transformed home office impacts on job satisfaction, job stress and job productivity. COVID-19 findings. PLoS ONE 2022, 17, e0265131. [Google Scholar] [CrossRef]
- Carillo, K.; Cachat-Rosset, G.; Marsan, J.; Saba, T.; Klarsfeld, A. Adjusting to epidemic-induced telework: Empirical insights from teleworkers in France. Eur. J. Inf. Syst. 2021, 30, 69–88. [Google Scholar] [CrossRef]
- Anderson, A.J.; Kaplan, S.A.; Vega, R.P. The impact of telework on emotional experience: When, and for whom, does telework improve daily affective well-being? Eur. J. Work Organ. Psychol. 2015, 24, 882–897. [Google Scholar] [CrossRef]
- Bailey, D.E.; Kurland, N.B. A review of telework research: Findings, new directions, and lessons for the study of modern work. J. Organ. Behav. 2002, 23, 383–400. [Google Scholar] [CrossRef]
- Shin, B.; El Sawy, O.A.; Sheng, O.R.L.; Higa, K. Telework: Existing research and future directions. J. Organ Comput. Electron. Commer 2000, 10, 85–101. [Google Scholar] [CrossRef]
- Chirico, F.; Zaffina, S.; Di Prinzio, R.R.; Girogi, G.; Ferrari, G.; Capitanelli, I.; Sacco, A.; Szarpak, L.; Nucera, G.; Taino, G.; et al. Working from home in the context of COVID-19: A systematic review of physical and mental health effects on teleworkers. J. Health Soc. Behav. 2021, 6, 319–332. [Google Scholar] [CrossRef]
- Moglia, M.; Hopkins, J.; Bardoel, A. Telework, hybrid work and the United Nation’s Sustainable Development Goals: Towards policy coherence. Sustainability 2021, 13, 9222. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Comprehensive Survey of Living Conditions in 2019. Available online: https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa19/index.html (accessed on 13 August 2023). (In Japanese).
- Breslau, N.; Peterson, E.L.; Schultz, L.R.; Chilcoat, H.D.; Andreski, P. Major depression and stages of smoking. A longitudinal investigation. Arch Gen Psychiatry 1998, 55, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Churchill, S.A.; Farrell, L. Alcohol and depression: Evidence from the 2014 health survey for England. Drug Alcohol Depend. 2017, 180, 86–92. [Google Scholar] [CrossRef]
- Gordon, B.R.; McDowell, C.P.; Lyons, M.; Herring, M.P. The effects of resistance exercise training on anxiety: A meta-analysis and meta-regression analysis of randomized controlled trials. Sports Med. 2017, 47, 2521–2532. [Google Scholar] [CrossRef]
- Roenneberg, T.; Kuehnle, T.; Juda, M.; Kantermann, T.; Allebrandt, K.; Gordijn, M.; Merrow, M. Epidemiology of the human circadian clock. Sleep Med. Rev. 2007, 11, 429–438. [Google Scholar] [CrossRef]
- Roenneberg, T.; Pilz, L.K.; Zerbini, G.; Winnebeck, E.C. Chronotype and social jetlag: A (self-) critical review. Biology 2019, 8, 54. [Google Scholar] [CrossRef]
- Jankowski, K.S. Social jet lag: Sleep-corrected formula. Chronobiol. Int. 2017, 34, 531–535. [Google Scholar] [CrossRef]
- Okajima, I.; Komada, Y.; Ito, W.; Inoue, Y. Sleep debt and social jetlag associated with sleepiness, mood, and work performance among workers in Japan. Int. J. Environ. Res. Public. Health 2021, 18, 2908. [Google Scholar] [CrossRef]
- Taylor, A.; Wright, H.R.; Lack, L.C. Sleeping-in on the weekend delays circadian phase and increases sleepiness the following week. Sleep Biol. Rhythm. 2008, 6, 172–179. [Google Scholar] [CrossRef]
- Lee, A.; Myung, S.K.; Cho, J.J.; Jung, Y.J.; Yoon, J.L.; Kim, M.Y. Night shift work and risk of depression: Meta-analysis of observational studies. J. Korean Med. Sci. 2017, 32, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Kuehnle, T.; Pramstaller, P.P.; Ricken, J.; Havel, M.; Guth, A.; Merrow, M. A marker for the end of adolescence. Curr. Biol. 2004, 14, R1038–R1039. [Google Scholar] [CrossRef] [PubMed]
- Germain, A.; Kupfer, D.J. Circadian rhythm disturbances in depression. Hum. Psychopharmacol. 2008, 23, 571–585. [Google Scholar] [CrossRef] [PubMed]
- Salgado-Delgado, R.; Tapia Osorio, A.; Saderi, N.; Escobar, C. Disruption of circadian rhythms: A crucial factor in the etiology of depression. Depress. Res. Treat. 2011, 2011, 839743. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.J.; Purvis, T.E.; Hu, K.; Scheer, F.A. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc. Natl. Acad. Sci. USA 2016, 113, E1402–E1411. [Google Scholar] [CrossRef]
- Moret, C.; Briley, M. The importance of norepinephrine in depression. Neuropsychiatr. Dis. Treat. 2011, 7, 9–13. [Google Scholar] [CrossRef]
- Herbert, J. Cortisol and depression: Three questions for psychiatry. Psychol. Med. 2013, 43, 449–469. [Google Scholar] [CrossRef]
- Roenneberg, T.; Merrow, M. The circadian clock and human health. Curr. Biol. 2016, 26, R432–R443. [Google Scholar] [CrossRef]
- Kronfeld-Schor, N.; Visser, M.E.; Salis, L.; van Gils, J.A. Chronobiology of interspecific interactions in a changing world. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2017, 372, 20160248. [Google Scholar] [CrossRef]
- Souetre, E.; Salvati, E.; Wehr, T.A.; Sack, D.A.; Krebs, B.; Darcourt, G. Twenty-four-hour profiles of body temperature and plasma TSH in bipolar patients during depression and during remission and in normal control subjects. Am. J. Psychiatry 1988, 145, 1133–1137. [Google Scholar] [CrossRef]
- Steiner, M.; Brown, G.M.; Goldman, S. Nocturnal melatonin and cortisol secretion in newly admitted psychiatric inpatients. Eur. Arch. Psychiatry Clin. Neurosci. 1990, 240, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Peeters, F.; Berkhof, J.; Delespaul, P.; Rottenberg, J.; Nicolson, N.A. Diurnal mood variation in major depressive disorder. Emotion 2006, 6, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Buhr, E.D.; Yoo, S.H.; Takahashi, J.S. Temperature as a universal resetting cue for mammalian circadian oscillators. Science 2010, 330, 379–385. [Google Scholar] [CrossRef] [PubMed]
- McClung, C.A. Circadian genes, rhythms and the biology of mood disorders. Pharmacol. Ther. 2007, 114, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Tsang, A.H.; Barclay, J.L.; Oster, H. Interactions between endocrine and circadian systems. J. Mol. Endocrinol. 2014, 52, R1–R16. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kessler, R.C.; Andrews, G.; Colpe, L.; Hiripi, È.; Mroczek, D.K.; Normand, S.-L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, T.A.; Kawakami, N.; Saitoh, M.; Ono, Y.; Nakane, Y.; Nakamura, Y.; Tachimori, H.; Iwata, N.; Uda, H.; Nakane, H.; et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 2008, 17, 152–158. [Google Scholar] [CrossRef]
- Sakurai, K.; Nishi, A.; Kondo, K.; Yanagida, K.; Kawakami, N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin. Neurosci. 2011, 65, 434–441. [Google Scholar] [CrossRef]
- Shimomitsu, T. The Final Development of the Brief Job Stress Questionnaire Mainly Used for Assessment of the Individuals. In Ministry of Labour Sponsored Grant for the Prevention of Work-Related Illness: The 1999 Report; CiNii Research: Tokyo, Japan, 2000; pp. 126–164. (In Japanese) [Google Scholar]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]
- Okajima, I.; Nakajima, S.; Kobayashi, M.; Inoue, Y. Development and validation of the Japanese version of the Athens Insomnia Scale. Psychiatry Clin. Neurosci. 2013, 67, 420–425. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).