Traumatic Brain Injury, Sleep, and Melatonin—Intrinsic Changes with Therapeutic Potential
Abstract
1. Introduction
2. Results
3. Discussion
3.1. Traumatic Brain Injury and Sleep Disorders
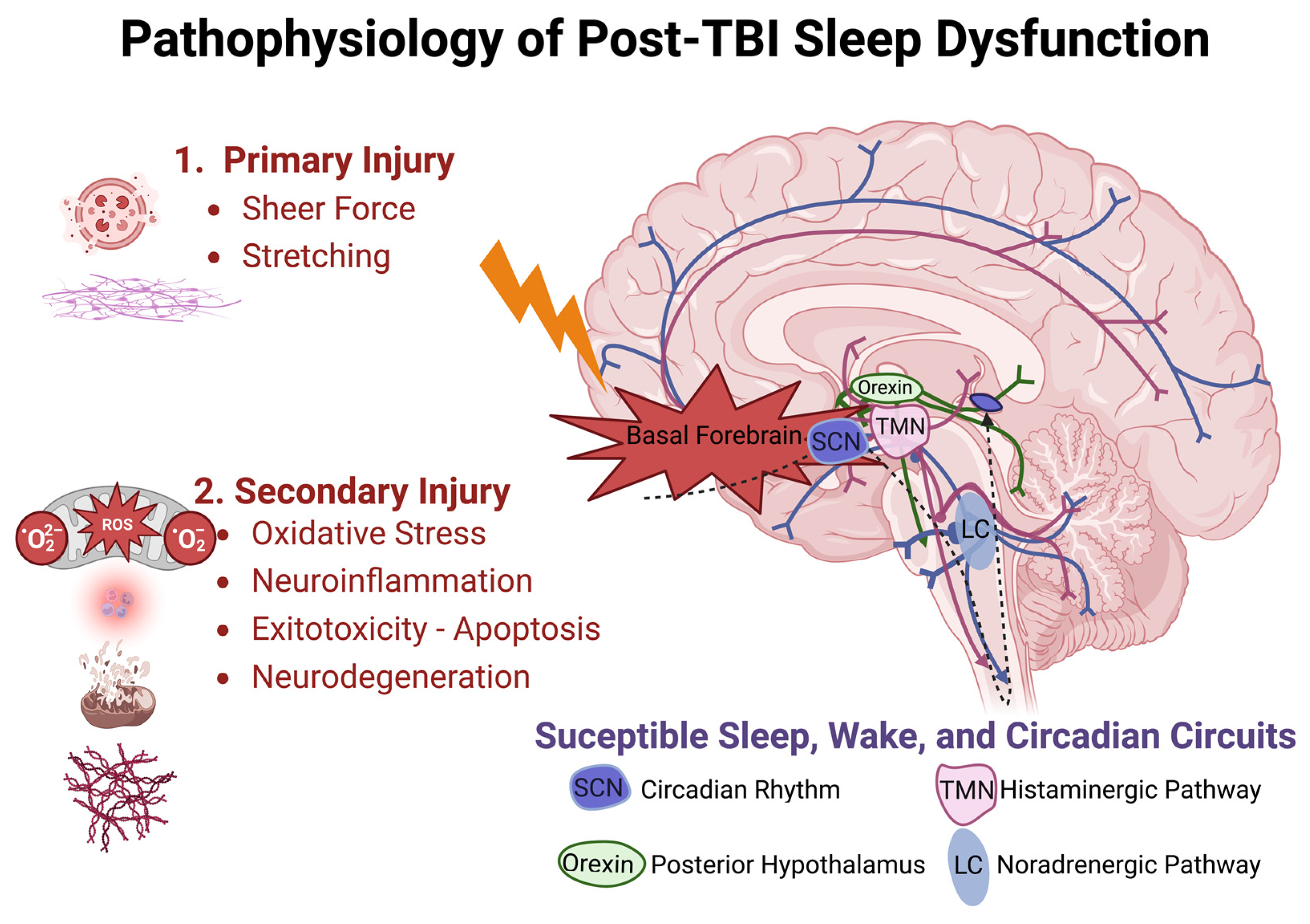
3.2. Pathophysiology of TBI Associated Sleep Dysfunction
3.2.1. Primary Injury
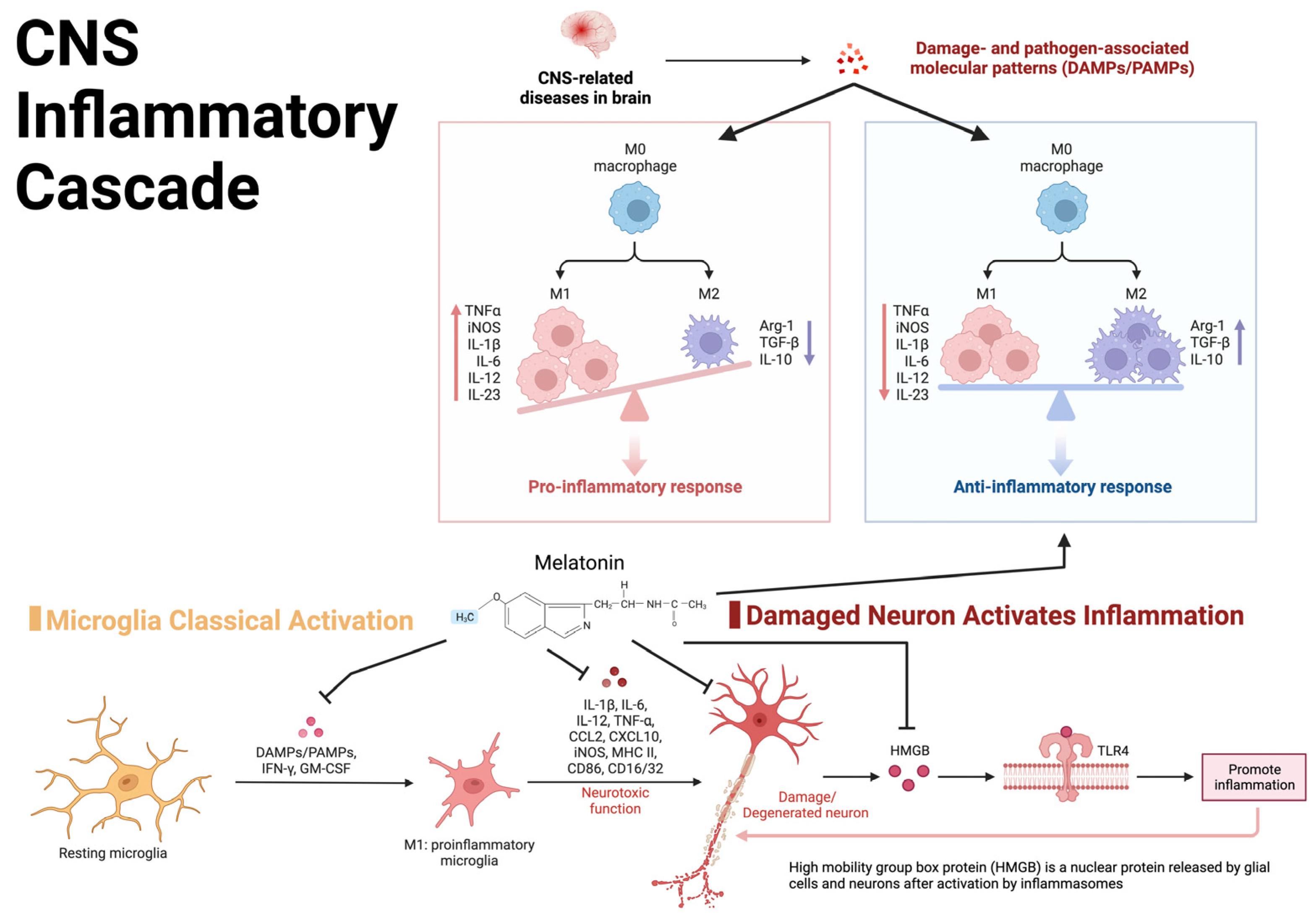
3.2.2. Secondary Injury
3.2.3. Injury Severity
3.2.4. Genetic Risk
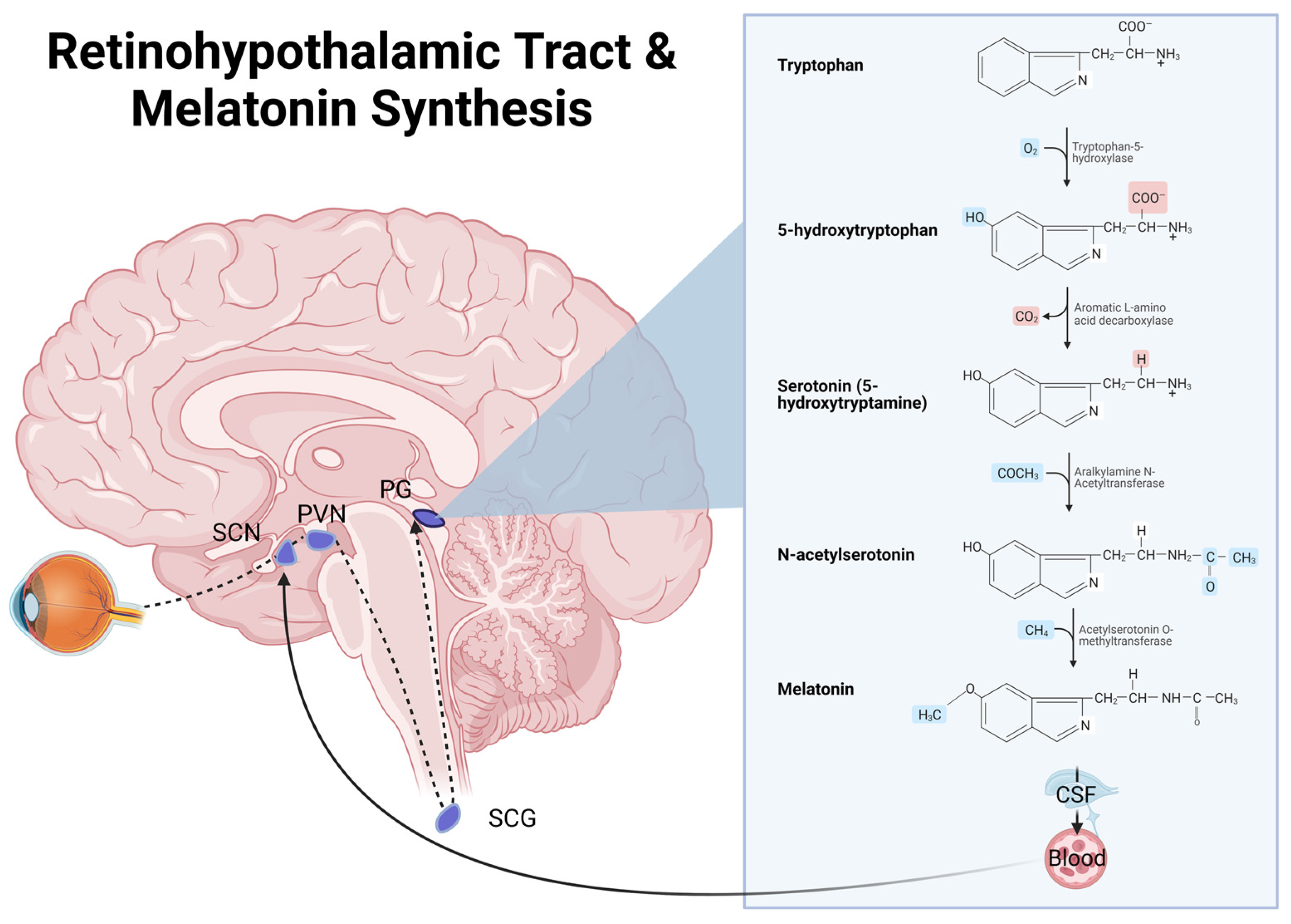
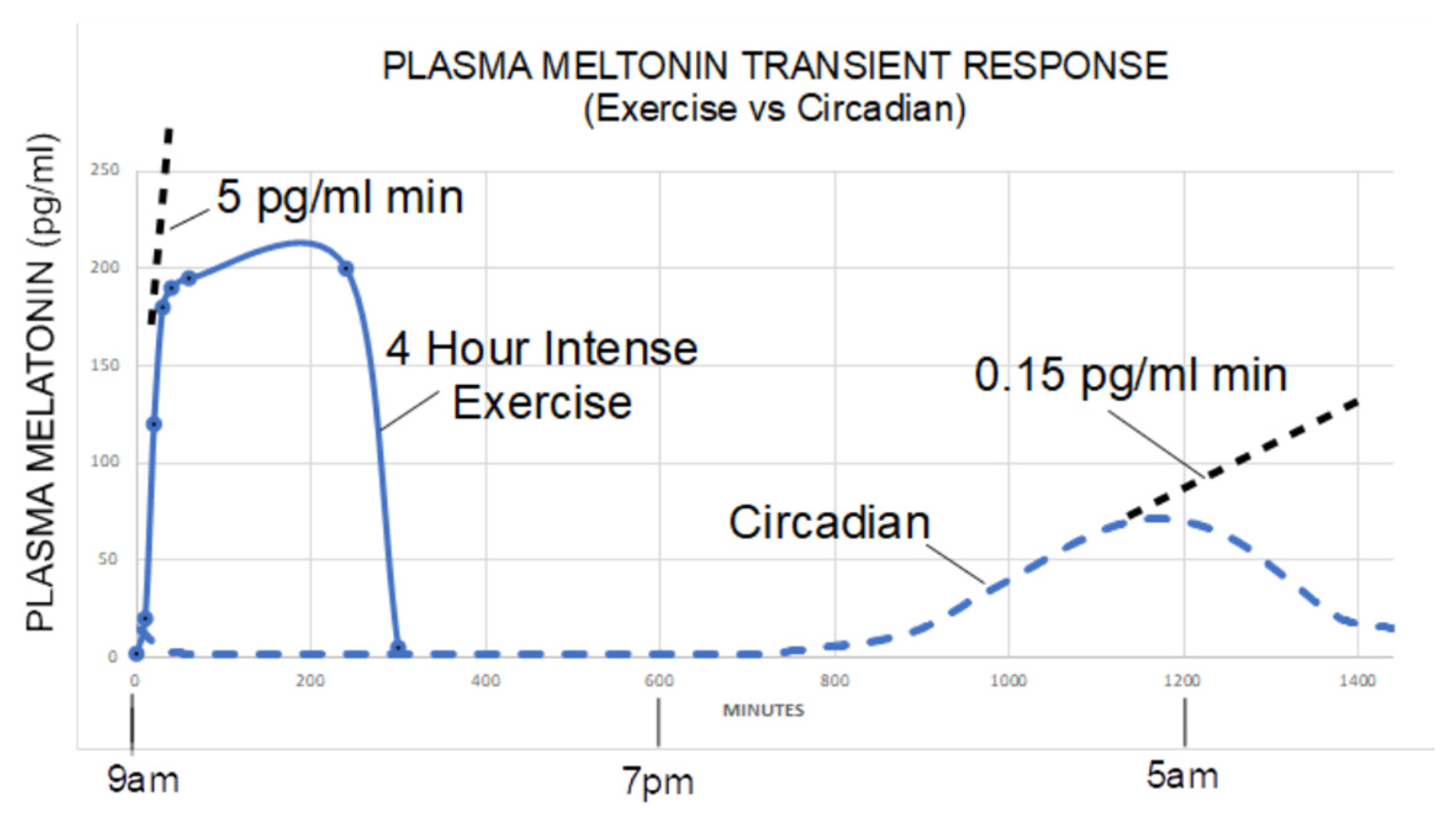
3.3. Melatonin Physiology
3.3.1. TBI Effect on Melatonin Synthesis
3.3.2. TBI Effect on Melatonin Receptor Expression
3.4. Therapeutic Potential of Melatonin
3.4.1. Melatonin’s TBI Therapeutic Potential—Circadian and Sleep-Wake Disorders
3.4.2. Melatonin’s TBI Therapeutic Potential—Antioxidant/Anti-Inflammatory
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclosures
Appendix A
| Citation | Design | Title |
|---|---|---|
| Rehman et al., 2019 [178] | RCT Mice | Neurological Enhancement Effects of Melatonin Against Brain Injury-Induced Oxidative Stress, Neuroinflammation, and Neurodegeneration via Ampk/Creb Signaling |
| Naeser et al., 2016 [179] | LED Human | Transcranial, Red/Near-Infrared Light-Emitting Diode Therapy to Improve Cognition in Chronic Traumatic Brain Injury |
| Ge et al., 2020 [180] | Rats | Effect of Melatonin on Regeneration of Cortical Neurons in Rats with Traumatic Brain Injury |
| Ozdemir et al., 2005 [181] | Rats | Protective Effect of Melatonin Against Head Trauma-Induced Hippocampal Damage and Spatial Memory Deficits in Immature Rats |
| Bao et al., 2019 [182] | Rats | Silencing of A20 Aggravates Neuronal Death and Inflammation After Traumatic Brain Injury: A Potential Trigger of Necroptosis |
| Osier et al., 2017 [18] | RCT Rats | Brain Injury Results in Lower Levels of Melatonin Receptors’ Subtypes MT1 and MT2 |
| Wang et al., 2012 [183] | Model | Melatonin Activates the NRF2-Are Pathway When It Protects Against Early Brain Injury in a Subarachnoid Hemorrhage Model |
| Ding et al., 2014 [156] | Model | Melatonin Stimulates Antioxidant Enzymes and Reduces Oxidative Stress in Experimental Traumatic Brain Injury: The NRF2-Are Signaling Pathway as a Potential Mechanism |
| Senol et al., 2014 [184] | Rats | Melatonin Reduces Traumatic Brain Injury-Induced Oxidative Stress in the Cerebral Cortex and Blood of Rats |
| Ding et al., 2015 [185] | Rats | Melatonin Protects the Brain from Apoptosis by Enhancement of Autophagy After Traumatic Brain Injury in Mice |
| Ates et al., 2006 [186] | Rats | Effect of Pinealectomy and Melatonin Replacement on Morphological and Biochemical Recovery After Traumatic Brain Injury |
| Beni et al., 2004 [187] | Rats | Melatonin-Induced Neuroprotection after Closed Head Injury is Associated with Increased Brain Antioxidants and Attenuated Late-Phase Activation of Nf-кB and Ap-1 |
| Campolo et al., 2013 [102] | Rats | Combination Therapy with Melatonin and Dexamethasone in a Mouse Model of Traumatic Brain Injury |
| Dehghan et al., 2013 [188] | Rats | Effect of Melatonin on Intracranial Pressure and Brain Edema Following Traumatic Brain Injury: Role of Oxidative Stresses |
| Ding et al., 2014 [189] | Rats | Melatonin Reduced Microglial Activation and Alleviated Neuroinflammation Induced Neuron Degeneration in Experimental Traumatic Brain Injury: Possible Involvement of Mtor Pathway |
| Ding et al., 2015 [185] | Rats | Melatonin Protects the Brain from Apoptosis by Enhancement of Autophagy After Traumatic Brain Injury in Mice |
| Kabadi et al., 2010 [190] | Rats | Posttreatment With Uridine and Melatonin Following Traumatic Brain Injury Reduces Edema in Various Brain Regions in Rats |
| Kelso et al., 2011 [191] | Rats | Melatonin and Minocycline for Combinatorial Therapy to Improve Functional and Histopathological Deficits Following Traumatic Brain Injury |
| Lin et al., 2016 [192] | Rats | Melatonin Attenuates Traumatic Brain Injury-Induced Inflammation: A Possible Role for Mitophagy |
| Mesenge et al., 1998 [193] | Rats | Protective Effect of Melatonin in a Model of Traumatic Brain Injury in Mice |
| Sarrafzadeh et al., 2000 [194] | Rats | Neuroprotective Effect of Melatonin on Cortical Impact Injury in the Rat |
| Wu et al., 2016 [195] | Rats | Melatonin Attenuates Neuronal Apoptosis Through Up-Regulation of K(+)-Cl(−) Cotransporter KCC2 Expression Following Traumatic Brain Injury in Rats |
| Yamakawa et al., 2017 [196] | Rats | Manipulating Cognitive Reserve: Pre-injury Environmental Conditions Influence the Severity of Concussion Symptomology, Gene Expression, and Response to Melatonin Treatment in Rats |
| Ran et al., 2021 [160] | Rats | Melatonin Protects Against Ischemic Brain Injury by Modulating pi3K/Akt Signaling Pathway via Suppression of Pten |
| Wang et al., 2022 [159] | Rats | Melatonin Protected Against Myocardial Infarction Injury in Rats Through a SIRT6-Dependent Antioxidant Pathway |
| Rui et al., 2021 [19] | Mice | Deletion of Ferritin H in Neurons Counteracts the Protective Effect of Melatonin Against Traumatic Brain Injury-induced Ferroptosis |
References
- Feigin, V.L.; Theadom, A.; Barker-Collo, S.; Starkey, N.J.; McPherson, K.; Kahan, M.; Dowell, A.; Brown, P.; Parag, V.; Kydd, R.; et al. Incidence of traumatic brain injury in New Zealand: A population-based study. Lancet Neurol. 2013, 12, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.-C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 2019, 130, 1080–1097. [Google Scholar] [CrossRef]
- Johnson, V.E.; Stewart, J.E.; Begbie, F.D.; Trojanowski, J.Q.; Smith, D.H.; Stewart, W. Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Brain 2013, 136, 28–42. [Google Scholar] [CrossRef] [PubMed]
- Kempf, J.; Werth, E.; Kaiser, P.R.; Bassetti, C.L.; Baumann, C.R. Sleep-wake disturbances 3 years after traumatic brain injury. J. Neurol. Neurosurg. Psychiatry 2010, 81, 1402–1405. [Google Scholar] [CrossRef]
- Ouellet, M.-C.; Beaulieu-Bonneau, S.; Morin, C.M. Sleep-wake disturbances after traumatic brain injury. Lancet Neurol. 2015, 14, 746–757. [Google Scholar] [CrossRef] [PubMed]
- Mathias, J.; Alvaro, P. Prevalence of sleep disturbances, disorders, and problems following traumatic brain injury: A meta-analysis. Sleep Med. 2012, 13, 898–905. [Google Scholar] [CrossRef]
- Sandsmark, D.K.; Elliott, J.; Lim, M.M. Sleep-Wake Disturbances After Traumatic Brain Injury: Synthesis of Human and Animal Studies. Sleep 2017, 40, zsx044. [Google Scholar] [CrossRef]
- Fichtenberg, N.L.; Zafonte, R.D.; Putnam, S.; Mann, N.R.; Millard, A.E. Insomnia in a post-acute brain injury sample. Brain Inj. 2002, 16, 197–206. [Google Scholar] [CrossRef]
- Gottshall, J.L.; Agyemang, A.A.; O’Neil, M.; Wei, G.; Presson, A.; Hewins, B.; Fisher, D.; Mithani, S.; Shahim, P.; Pugh, M.J.; et al. Sleep quality: A common thread linking depression, post-traumatic stress, and post-concussive symptoms to biomarkers of neurodegeneration following traumatic brain injury. Brain Inj. 2022, 36, 633–643. [Google Scholar] [CrossRef]
- Wolfe, L.F.; Sahni, A.S.; Attarian, H. Sleep disorders in traumatic brain injury. Neurorehabilitation 2018, 43, 257–266. [Google Scholar] [CrossRef]
- Mckee, A.C.; Daneshvar, D.H. The Neuropathology of Traumatic Brain Injury. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2015; Volume 127, pp. 45–66. [Google Scholar] [CrossRef]
- Hemphill, M.A.; Dauth, S.; Yu, C.J.; Dabiri, B.E.; Parker, K.K. Traumatic Brain Injury and the Neuronal Microenvironment: A Potential Role for Neuropathological Mechanotransduction. Neuron 2015, 85, 1177–1192. [Google Scholar] [CrossRef] [PubMed]
- Seifman, M.A.; Adamides, A.A.; Nguyen, P.N.; Vallance, A.S.; Cooper, D.J.; Kossmann, T.; Rosenfeld, J.V.; Morganti-Kossmann, M.C. Endogenous Melatonin Increases in Cerebrospinal Fluid of Patients after Severe Traumatic Brain Injury and Correlates with Oxidative Stress and Metabolic Disarray. J. Cereb. Blood Flow Metab. 2008, 28, 684–696. [Google Scholar] [CrossRef] [PubMed]
- Marseglia, L.; D’Angelo, G.; Manti, S.; Rulli, I.; Salvo, V.; Buonocore, G.; Reiter, R.J.; Gitto, E. Melatonin Secretion Is Increased in Children with Severe Traumatic Brain Injury. Int. J. Mol. Sci. 2017, 18, 1053. [Google Scholar] [CrossRef] [PubMed]
- Lorente, L.; Martín, M.M.; Abreu-González, P.; Pérez-Cejas, A.; Ramos, L.; Argueso, M.; Solé-Violán, J.; Cáceres, J.J.; Jiménez, A.; García-Marín, V. Serum melatonin levels in survivor and non-survivor patients with traumatic brain injury. BMC Neurol. 2017, 17, 138. [Google Scholar] [CrossRef]
- Duclos, C.; Dumont, M.; Paquet, J.; Blais, H.; Van Der Maren, S.; Menon, D.K.; Bernard, F.; Gosselin, N. Sleep-wake disturbances in hospitalized patients with traumatic brain injury: Association with brain trauma but not with an abnormal melatonin circadian rhythm. Sleep 2019, 43, zsz191. [Google Scholar] [CrossRef]
- Lorente, L.; Martín, M.M.; Ruiz, C.; Abreu-González, P.; Ramos-Gómez, L.; Argueso, M.; Sole-Violan, J.; Cáceres, J.J.; Jiménez, A. Serum melatonin levels in predicting mortality in patients with severe traumatic brain injury. Anaesth. Crit. Care Pain Med. 2021, 40, 100966. [Google Scholar] [CrossRef]
- Osier, N.D.; Pham, L.; Pugh, B.J.; Puccio, A.; Ren, D.; Conley, Y.P.; Alexander, S.; Dixon, C.E. Brain injury results in lower levels of melatonin receptors subtypes MT1 and MT2. Neurosci. Lett. 2017, 650, 18–24. [Google Scholar] [CrossRef]
- Rui, T.; Wang, H.; Li, Q.; Cheng, Y.; Gao, Y.; Fang, X.; Ma, X.; Chen, G.; Gao, C.; Gu, Z.; et al. Deletion of ferritin H in neurons counteracts the protective effect of melatonin against traumatic brain injury-induced ferroptosis. J. Pineal Res. 2020, 70, e12704. [Google Scholar] [CrossRef]
- Choi, K.; Lee, Y.J.; Park, S.; Je, N.K.; Suh, H.S. Efficacy of melatonin for chronic insomnia: Systematic reviews and meta-analyses. Sleep Med. Rev. 2022, 66, 36179487. [Google Scholar] [CrossRef]
- McGowan, N.M.; Kim, D.S.; Crespo, M.D.A.; Bisdounis, L.; Kyle, S.D.; Saunders, K.E.A. Hypnotic and Melatonin/Melatonin-Receptor Agonist Treatment in Bipolar Disorder: A Systematic Review and Meta-Analysis. CNS Drugs 2022, 36, 345–363. [Google Scholar] [CrossRef]
- Marupuru, S.; Arku, D.; Campbell, A.M.; Slack, M.K.; Lee, J.K. Use of Melatonin and/on Ramelteon for the Treatment of Insomnia in Older Adults: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 5138. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.-L.; Ye, X.; Wang, S.; Zhang, D. Melatonin Application in Assisted Reproductive Technology: A Systematic Review and Meta-Analysis of Randomized Trials. Front. Endocrinol. 2020, 11, 160. [Google Scholar] [CrossRef]
- Ghaderi, A.; Banafshe, H.R.; Mirhosseini, N.; Motmaen, M.; Mehrzad, F.; Bahmani, F.; Aghadavod, E.; Mansournia, M.A.; Reiter, R.J.; Karimi, M.-A.; et al. The effects of melatonin supplementation on mental health, metabolic and genetic profiles in patients under methadone maintenance treatment. Addict. Biol. 2018, 24, 754–764. [Google Scholar] [CrossRef] [PubMed]
- González-Candia, A.; Veliz, M.; Araya, C.; Quezada, S.; Ebensperger, G.; Serón-Ferré, M.; Reyes, R.V.; Llanos, A.J.; Herrera, E.A. Potential adverse effects of antenatal melatonin as a treatment for intrauterine growth restriction: Findings in pregnant sheep. Am. J. Obstet. Gynecol. 2016, 215, 245.e1–245.e7. [Google Scholar] [CrossRef]
- Colmenero, M.; Diaz, B.; Miguel, J.; González, M.; Esquifino, A.; Marin, B. Melatonin administration during pregnancy retards sexual maturation of female offspring in the rat. J. Pineal Res. 1991, 11, 23–27. [Google Scholar] [CrossRef]
- Luboshitzky, R.; Shen-Orr, Z.; Nave, R.; Lavi, S.; Lavie, P. Melatonin administration alters semen quality in healthy men. J. Androl. 2002, 23, 572–578. [Google Scholar] [PubMed]
- Erland, L.; Saxena, P.K. Melatonin Natural Health Products and Supplements: Presence of Serotonin and Significant Variability of Melatonin Content. J. Clin. Sleep Med. 2017, 13, 275–281. [Google Scholar] [CrossRef]
- Sun, S.-Y.; Chen, G.-H. Treatment of Circadian Rhythm Sleep–Wake Disorders. Curr. Neuropharmacol. 2021, 20, 1022–1034. [Google Scholar] [CrossRef]
- Kaleyias, J.; Kothare, S.V. Sleep Disorders in Traumatic Brain Injury. J. Clin. Neurophysiol. 2022, 39, 356–362. [Google Scholar] [CrossRef]
- Naseem, M.; Parvez, S. Role of Melatonin in Traumatic Brain Injury and Spinal Cord Injury. Sci. World J. 2014, 2014, 1–13. [Google Scholar] [CrossRef]
- Stewart, K.; Shakarishvili, N.; Michalak, A.; Maschauer, E.L.; Jenkins, N.; Riha, R.L. Treating sleep disorders following traumatic brain injury in adults: Time for renewed effort? Sleep Med. Rev. 2022, 63, 101631. [Google Scholar] [CrossRef] [PubMed]
- Gagner, C.; Landry-Roy, C.; Lainé, F.; Beauchamp, M.H. Sleep-Wake Disturbances and Fatigue after Pediatric Traumatic Brain Injury: A Systematic Review of the Literature. J. Neurotrauma 2015, 32, 1539–1552. [Google Scholar] [CrossRef] [PubMed]
- Driver, S.; Stork, R. Pharmacological management of sleep after traumatic brain injury. Neurorehabilitation 2018, 43, 347–353. [Google Scholar] [CrossRef]
- Osier, N.; McGreevy, E.; Pham, L.; Puccio, A.; Ren, D.; Conley, Y.P.; Alexander, S.; Dixon, C.E. Melatonin as a Therapy for Traumatic Brain Injury: A Review of Published Evidence. Int. J. Mol. Sci. 2018, 19, 1539. [Google Scholar] [CrossRef] [PubMed]
- Barlow, K.; Esser, M.M.J.; Veidt, M.; Boyd, R. Melatonin as a Treatment after Traumatic Brain Injury: A Systematic Review and Meta-Analysis of the Pre-Clinical and Clinical Literature. J. Neurotrauma 2019, 36, 523–537. [Google Scholar] [CrossRef] [PubMed]
- Blum, B.; Kaushal, S.; Khan, S.; Kim, J.H.; Villalba, C.L.A. Melatonin in Traumatic Brain Injury and Cognition. Cureus 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, C.; Carr, C.; Zemek, R.; Yeates, K.O.; Master, C.; Schneider, K.; Bell, M.J.; Wisniewski, S.; Mannix, R. Association of Pharmacological Interventions with Symptom Burden Reduction in Patients With Mild Traumatic Brain Injury. JAMA Neurol. 2021, 78, 596–608. [Google Scholar] [CrossRef]
- Ali, A.M.; Morfin, J.B.; Mills, J.A.; Pasipanodya, E.C.; Maas, Y.J.M.; Huang, E.; Dirlikov, B.M.; Englander, J.; Zedlitz, A. Fatigue After Traumatic Brain Injury: A Systematic Review. J. Head Trauma Rehabil. 2021, 37, E249–E257. [Google Scholar] [CrossRef]
- Samantaray, S.; Das, A.; Thakore, N.P.; Matzelle, D.D.; Reiter, R.J.; Ray, S.K.; Banik, N.L. Therapeutic potential of melatonin in traumatic central nervous system injury. J. Pineal Res. 2009, 47, 134–142. [Google Scholar] [CrossRef]
- Reiter, R.J.; Mayo, J.C.; Tan, D.-X.; Sainz, R.M.; Alatorre-Jimenez, M.; Qin, L. Melatonin as an antioxidant: Under promises but over delivers. J. Pineal Res. 2016, 61, 253–278. [Google Scholar] [CrossRef]
- Cassimatis, M.; Browne, G.; Orr, R. The Utility of Melatonin for the Treatment of Sleep Disturbance After Traumatic Brain Injury: A Scoping Review. Arch. Phys. Med. Rehabil. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kemp, S.; Biswas, R.; Neumann, V.; Coughlan, A. The value of melatonin for sleep disorders occurring post-head injury: A pilot RCT. Brain Inj. 2004, 18, 911–919. [Google Scholar] [CrossRef] [PubMed]
- Grima, N.A.; Rajaratnam, S.M.W.; Mansfield, D.; Sletten, T.L.; Spitz, G.; Ponsford, J.L. Efficacy of melatonin for sleep disturbance following traumatic brain injury: A randomised controlled trial. BMC Med. 2018, 16, 1–10. [Google Scholar] [CrossRef]
- Lequerica, A.; Jasey, N.; Tremont, J.N.P.; Chiaravalloti, N.D. Pilot Study on the Effect of Ramelteon on Sleep Disturbance After Traumatic Brain Injury: Preliminary Evidence from a Clinical Trial. Arch. Phys. Med. Rehabil. 2015, 96, 1802–1809. [Google Scholar] [CrossRef]
- Iyer, K.K.; Zalesky, A.; Cocchi, L.; Barlow, K.M. Neural Correlates of Sleep Recovery following Melatonin Treatment for Pediatric Concussion: A Randomized Controlled Trial. J. Neurotrauma 2020, 37, 2647–2655. [Google Scholar] [CrossRef] [PubMed]
- Barlow, K.M.; Brooks, B.L.; Esser, M.J.; Kirton, A.; Mikrogianakis, A.; Zemek, R.L.; MacMaster, F.P.; Nettel-Aguirre, A.; Yeates, K.O.; Kirk, V.; et al. Efficacy of Melatonin in Children with Post-concussive Symptoms: A Randomized Clinical Trial. Pediatrics 2020, 145, e20192812. [Google Scholar] [CrossRef]
- Kuczynski, A.; Crawford, S.; Bodell, L.; Dewey, D.; Barlow, K.M. Characteristics of post-traumatic headaches in children following mild traumatic brain injury and their response to treatment: A prospective cohort. Dev. Med. Child Neurol. 2013, 55, 636–641. [Google Scholar] [CrossRef]
- Grima, D.N.A.; Rajaratnam, S.M.; Mansfield, D.; McKenzie, D.; Ponsford, J.L. Poorer sleep quality predicts melatonin response in patients with traumatic brain injury: Findings from a randomized controlled trial. J. Clin. Sleep Med. 2021, 17, 1545–1551. [Google Scholar] [CrossRef]
- Dominguez-Rodriguez, A.; Abreu-Gonzalez, P.; de la Torre-Hernandez, J.M.; Consuegra-Sanchez, L.; Piccolo, R.; Gonzalez-Gonzalez, J.; Garcia-Camarero, T.; Garcia-Saiz, M.D.M.; Aldea-Perona, A.; Reiter, R.J.; et al. Usefulness of Early Treatment With Melatonin to Reduce Infarct Size in Patients With ST-Segment Elevation Myocardial Infarction Receiving Percutaneous Coronary Intervention (From the Melatonin Adjunct in the Acute Myocardial Infarction Treated With Angioplasty Trial). Am. J. Cardiol. 2017, 120, 522–526. [Google Scholar] [CrossRef]
- Domínguez-Rodríguez, A.; Hernández-Vaquero, D.; Abreu-González, P.; Báez-Ferrer, N.; Díaz, R.; Avanzas, P.; Simko, F.; Domínguez-González, V.; Sharma, R.; Reiter, R.J. Early Treatment of Acute Myocardial Infarction with Melatonin: Effects on MMP-9 and Adverse Cardiac Events. J. Clin. Med. 2022, 11, 1909. [Google Scholar] [CrossRef]
- Ekeloef, S.; Halladin, N.; Fonnes, S.; Jensen, S.E.; Zaremba, T.; Rosenberg, J.; Jonsson, G.; Aarøe, J.; Gasbjerg, L.S.; Rosenkilde, M.M.; et al. Effect of Intracoronary and Intravenous Melatonin on Myocardial Salvage Index in Patients with ST-Elevation Myocardial Infarction: A Randomized Placebo Controlled Trial. J. Cardiovasc. Transl. Res. 2017, 10, 470–479. [Google Scholar] [CrossRef]
- Dwaich, K.H.; Al-Amran, F.G.; Al-Sheibani, B.I.; Al-Aubaidy, H.A. Melatonin effects on myocardial ischemia–reperfusion injury: Impact on the outcome in patients undergoing coronary artery bypass grafting surgery. Int. J. Cardiol. 2016, 221, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Auger, R.R.; Burgess, H.J.; Emens, J.S.; Deriy, L.V.; Thomas, S.M.; Sharkey, K.M. Clinical Practice Guideline for the Treatment of Intrinsic Circadian Rhythm Sleep-Wake Disorders: Advanced Sleep-Wake Phase Disorder (ASWPD), Delayed Sleep-Wake Phase Disorder (DSWPD), Non-24-Hour Sleep-Wake Rhythm Disorder (N24SWD), and Irregular Sleep-Wake Rhythm Disorder (ISWRD). An Update for 2015. J. Clin. Sleep Med. 2015, 11, 1199–1236. [Google Scholar] [CrossRef] [PubMed]
- Morgenthaler, T.I.; Lee-Chiong, T.; Alessi, C.; Friedman, L.; Aurora, R.N.; Boehlecke, B.; Brown, T.; Chesson, A.L.; Kapur, V.; Maganti, R.; et al. Practice Parameters for the Clinical Eval-uation and Treatment of Circadian Rhythm Sleep Disorders. Sleep 2007, 30, 1445–1459. [Google Scholar] [CrossRef]
- Riemann, D.; Baglioni, C.; Bassetti, C.; Bjorvatn, B.; Groselj, L.D.; Ellis, J.G.; Espie, C.A.; Garcia-Borreguero, D.; Gjerstad, M.; Gonçalves, M.; et al. European guideline for the diagnosis and treatment of insomnia. J. Sleep Res. 2017, 26, 675–700. [Google Scholar] [CrossRef] [PubMed]
- Sateia, M.J.; Buysse, D.J.; Krystal, A.D.; Neubauer, D.N.; Heald, J.L. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 307–349. [Google Scholar] [CrossRef]
- Qaseem, A.; Kansagara, D.; Forciea, M.A.; Cooke, M.; Denberg, T.D.; Clinical Guidelines Committee of the American College of Physicians. Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline from the American College of Physicians. Ann. Intern. Med. 2016, 165, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Barlow, K.M.; Brooks, B.L.; MacMaster, F.P.; Kirton, A.; Seeger, T.; Esser, M.; Crawford, S.; Nettel-Aguirre, A.; Zemek, R.; Angelo, M.; et al. A double-blind, placebo-controlled intervention trial of 3 and 10 mg sublingual melatonin for post-concussion syndrome in youths (PLAYGAME): Study protocol for a randomized controlled trial. Trials 2014, 15, 271. [Google Scholar] [CrossRef]
- Leng, Y.; Byers, A.L.; Barnes, D.E.; Peltz, C.B.; Li, Y.; Yaffe, K. Traumatic Brain Injury and Incidence Risk of Sleep Disorders in Nearly 200,000 US Veterans. Neurology 2021, 96, e1792–e1799. [Google Scholar] [CrossRef]
- Baumann, C.; Werth, E.; Stocker, R.; Ludwig, S.; Bassetti, C.L. Sleep-wake disturbances 6 months after traumatic brain injury: A prospective study. Brain 2007, 130, 1873–1883. [Google Scholar] [CrossRef]
- Mollayeva, T.; Mollayeva, S.; Colantonio, A. The Risk of Sleep Disorder Among Persons with Mild Traumatic Brain Injury. Curr. Neurol. Neurosci. Rep. 2016, 16, 27079955. [Google Scholar] [CrossRef] [PubMed]
- Castriotta, R.J.; Murthy, J.N. Sleep Disorders in Patients with Traumatic Brain Injury. CNS Drugs 2011, 25, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Ouellet, M.-C.; Beaulieu-Bonneau, S.; Morin, C.M. Insomnia in Patients with Traumatic Brain Injury. J. Head Trauma Rehabil. 2006, 21, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Rao, V.; Spiro, J.; Vaishnavi, S.; Rastogi, P.; Mielke, M.; Noll, K.; Cornwell, E.; Schretlen, D.; Makley, M. Prevalence and types of sleep disturbances acutely after traumatic brain injury. Brain Inj. 2008, 22, 381–386. [Google Scholar] [CrossRef]
- Verma, A.; Anand, V.; Verma, N. Verma Sleep Disorders. J. Clin. Sleep Med. 2007, 3, 357–362. [Google Scholar] [CrossRef]
- Chaput, G.; Giguère, J.-F.; Chauny, J.-M.; Denis, R.; Lavigne, G. Relationship among subjective sleep complaints, headaches, and mood alterations following a mild traumatic brain injury. Sleep Med. 2009, 10, 713–716. [Google Scholar] [CrossRef]
- Theadom, A.; Cropley, M.; Parmar, P.; Barker-Collo, S.; Starkey, N.; Jones, K.; Feigin, V.L. Sleep difficulties one year following mild traumatic brain injury in a population-based study. Sleep Med. 2015, 16, 926–932. [Google Scholar] [CrossRef]
- Haboubi, N.H.J.; Long, J.; Koshy, M.; Ward, A.B. Short-term sequelae of minor head injury (6 years experience of minor head injury clinic). Disabil. Rehabil. 2001, 23, 635–638. [Google Scholar] [CrossRef]
- Mac Donald, C.L.; Barber, J.; Patterson, J.; Johnson, A.M.; Dikmen, S.; Fann, J.R.; Temkin, N. Association between 5-Year Clinical Outcome in Patients with Nonmedically Evacuated Mild Blast Traumatic Brain Injury and Clinical Measures Collected within 7 Days Postinjury in Combat. JAMA Netw. Open 2019, 2, e186676. [Google Scholar] [CrossRef]
- Wickwire, E.M.; Albrecht, J.S.; Capaldi, V.F.; Jain, S.O.; Gardner, R.C.; Werner, J.K.; Mukherjee, P.; McKeon, A.B.; Smith, M.T.; Giacino, J.T.; et al. Trajectories of Insomnia in Adults After Traumatic Brain Injury. JAMA Netw. Open 2022, 5, e2145310. [Google Scholar] [CrossRef]
- Nakase-Richardson, R.; McNamee, S.; Howe, L.L.; Massengale, J.; Peterson, M.; Barnett, S.D.; Harris, O.; McCarthy, M.; Tran, J.; Scott, S.; et al. Descriptive Characteristics and Rehabilitation Outcomes in Active Duty Military Personnel and Veterans With Disorders of Consciousness With Combat- and Noncombat-Related Brain Injury. Arch. Phys. Med. Rehabil. 2013, 94, 1861–1869. [Google Scholar] [CrossRef] [PubMed]
- Baumann, C.R.; Werner, J. TBI and Sleep–Wake Disorders: Pathophysiology, Clinical Management, and Moving towards the Future. Semin. Neurol. 2017, 37, 419–432. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Yue, S.; Wang, P.; Wen, B.; Zhang, X. Systemic inflammation in traumatic brain injury predicts poor cognitive function. Immun. Inflamm. Dis. 2021, 10, 8926513. [Google Scholar] [CrossRef] [PubMed]
- Corps, K.N.; Roth, T.; McGAVERN, D.B. Inflammation and Neuroprotection in Traumatic Brain Injury. JAMA Neurol. 2015, 72, 355–362. [Google Scholar] [CrossRef]
- Esposito, E.; Cuzzocrea, S. Antiinflammatory Activity of Melatonin in Central Nervous System. Curr. Neuropharmacol. 2010, 8, 228–242. [Google Scholar] [CrossRef]
- Ikram, M.; Park, H.Y.; Ali, T.; Kim, M.O. Melatonin as a Potential Regulator of Oxidative Stress, and Neuroinflammation: Mechanisms and Implications for the Management of Brain Injury-Induced Neurodegeneration. J. Inflamm. Res. 2021, 14, 6251–6264. [Google Scholar] [CrossRef]
- Valko, P.O.; Gavrilov, Y.V.; Yamamoto, M.; Finn, K.; Reddy, H.; Haybaeck, J.; Weis, S.; Scammell, T.E.; Baumann, C.R. Damage to histaminergic tuberomammillary neurons and other hypothalamic neurons with traumatic brain injury. Ann. Neurol. 2014, 77, 177–182. [Google Scholar] [CrossRef]
- Prins, M.; Greco, T.; Alexander, D.; Giza, C.C. The pathophysiology of traumatic brain injury at a glance. Dis. Model. Mech. 2013, 6, 1307–1315. [Google Scholar] [CrossRef]
- Schuch, J.B.; Genro, J.P.; Bastos, C.R.; Ghisleni, G.; Tovo-Rodrigues, L. The role of CLOCK gene in psychiatric disorders: Evidence from human and animal research. Am. J. Med Genet. Part B Neuropsychiatr. Genet. 2017, 177, 181–198. [Google Scholar] [CrossRef]
- Hong, C.-T.; Wong, C.-S.; Ma, H.-P.; Wu, D.; Huang, Y.-H.; Wu, C.-C.; Lin, C.-M.; Su, Y.-K.; Liao, K.-H.; Ou, J.-C.; et al. PERIOD3 polymorphism is associated with sleep quality recovery after a mild traumatic brain injury. J. Neurol. Sci. 2015, 358, 385–389. [Google Scholar] [CrossRef]
- Lerner, A.B.; Case, J.D.; Takahashi, Y.; Lee, T.H.; Mori, W. ISOLATION OF MELATONIN, THE PINEAL GLAND FACTOR THAT LIGHTENS MELANOCYTEs. J. Am. Chem. Soc. 1958, 80, 2587. [Google Scholar] [CrossRef]
- Suofu, Y.; Li, W.; Jean-Alphonse, F.G.; Jia, J.; Khattar, N.K.; Li, J.; Baranov, S.V.; Leronni, D.; Mihalik, A.C.; He, Y.; et al. Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proc. Natl. Acad. Sci. USA 2017, 114, E7997–E8006. [Google Scholar] [CrossRef]
- Rosengarten, H.; Meller, E.; Friedhoff, A.J. In vitro enzymatic formation of melatonin by human erythrocytes. Res. Commun. Chem. Pathol. Pharmacol. 1972, 4, 457–465. [Google Scholar]
- Bubenik, G.A. Gastrointestinal Melatonin Localization, Function, and Clinical Relevance. Dig. Dis. Sci. 2002, 47, 2336–2348. [Google Scholar] [CrossRef] [PubMed]
- Amaral, F.G.D.; Cipolla-Neto, J. A brief review about melatonin, a pineal hormone. Arq. Bras. de Endocrinol. Metabol. 2018, 62, 472–479. [Google Scholar] [CrossRef]
- Tan, D.-X.; Reiter, R.J.; Zimmerman, S.; Hardeland, R. Melatonin: Both a Messenger of Darkness and a Participant in the Cellular Actions of Non-Visible Solar Radiation of Near Infrared Light. Biology 2023, 12, 89. [Google Scholar] [CrossRef]
- Kim, T.-K.; Lin, Z.; Tidwell, W.J.; Li, W.; Slominski, A.T. Melatonin and its metabolites accumulate in the human epidermis in vivo and inhibit proliferation and tyrosinase activity in epidermal melanocytes in vitro. Mol. Cell. Endocrinol. 2014, 404, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, S.; Reiter, R.J. Transient responses of melatonin to stress. Melatonin Res. 2022, 5, 295–303. [Google Scholar] [CrossRef]
- Tan, D.-X.; Manchester, L.C.; Liu, X.; Rosales-Corral, S.A.; Acuna-Castroviejo, D.; Reiter, R.J. Mitochondria and chloroplasts as the original sites of melatonin synthesis: A hypothesis related to melatonin’s primary function and evolution in eukaryotes. J. Pineal Res. 2012, 54, 127–138. [Google Scholar] [CrossRef]
- Reiter, R.J.; Tan, D.X.; Galano, A. Melatonin: Exceeding Expectations. Physiology 2014, 29, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Allegra, M.; Reiter, R.; Tan, D.-X.; Gentile, C.; Tesoriere, L.; Livrea, M. The chemistry of melatonin’s interaction with reactive species. J. Pineal Res. 2002, 34, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rosen, J.; Ni Than, N.; Koch, D.; Poeggeler, B.; Laatsch, H.; Hardeland, R. Interactions of melatonin and its metabolites with the ABTS cation radical: Extension of the radical scavenger cascade and formation of a novel class of oxidation products, C2-substituted 3-indolinones. J. Pineal Res. 2006, 41, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, C.; Mayo, J.C.; Sainz, R.M.; Antolin, I.; Herrera, F.; Martin, V.; Reiter, R.J. Regulation of antioxidant enzymes: A significant role for melatonin. J. Pineal Res. 2004, 36, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.-X.; Manchester, L.C.; Esteban-Zubero, E.; Zhou, Z.; Reiter, R.J. Melatonin as a Potent and Inducible Endogenous Antioxidant: Synthesis and Metabolism. Molecules 2015, 20, 18886–18906. [Google Scholar] [CrossRef]
- Castroviejo, D.A.; Lopez, L.C.; Escames, G.; Lopez, A.; Garcia, J.A.; Reiter, R.J. Melatonin-mitochondria Interplay in Health and Disease. Curr. Top. Med. Chem. 2011, 11, 221–240. [Google Scholar] [CrossRef] [PubMed]
- Acuña-Castroviejo, D.; Escames, G.; León, J.; Carazo, A.; Khaldy, H. Mitochondrial regulation by melatonin And its metabolites. Adv. Exp. Med. Biol. 2003, 527, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Leon, J.; Acuna-Castroviejo, D.; Escames, G.; Tan, D.-X.; Reiter, R.J. Melatonin mitigates mitochondrial malfunction. J. Pineal Res. 2004, 38, 1–9. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, Z.; Liu, Y.; Pan, S.; Zhang, H.; Fang, M.; Jiang, H.; Yin, J.; Zou, S.; Li, Z.; et al. Melatonin reduces hypoxic-ischaemic (HI) induced autophagy and apoptosis: An in vivo and in vitro investigation in experimental models of neonatal HI brain injury. Neurosci. Lett. 2017, 653, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.-J.; Wu, C.; Niu, H.-J.; Wang, K.; Mo, L.-J.; Shao, A.-W.; Dixon, B.J.; Zhang, J.-M.; Yang, S.-X.; Wang, Y.-R. Neuroprotective Mechanisms of Melatonin in Hemorrhagic Stroke. Cell. Mol. Neurobiol. 2017, 37, 1173–1185. [Google Scholar] [CrossRef]
- Das, A.; McDowell, M.; Pava, M.J.; Smith, J.A.; Reiter, R.J.; Woodward, J.J.; Varma, A.K.; Ray, S.K.; Banik, N.L. The inhibition of apoptosis by melatonin in VSC4.1 motoneurons exposed to oxidative stress, glutamate excitotoxicity, or TNF-α toxicity involves membrane melatonin receptors. J. Pineal Res. 2010, 48, 157–169. [Google Scholar] [CrossRef]
- Campolo, M.; Ahmad, A.; Crupi, R.; Impellizzeri, D.; Morabito, R.; Esposito, E.; Cuzzocrea, S. Combination therapy with melatonin and dexamethasone in a mouse model of traumatic brain injury. J. Endocrinol. 2013, 217, 291–301. [Google Scholar] [CrossRef]
- Villapol, S.; Fau, S.; Renolleau, S.; Biran, V.; Charriaut-Marlangue, C.; Baud, O. Melatonin Promotes Myelination by Decreasing White Matter Inflammation After Neonatal Stroke. Pediatr. Res. 2011, 69, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.C.; Chen, W.J.; Ching, C.H.; Chuang, J.I. Melatonin attenuates brain contusion-induced oxidative insult, inactivation of signal transducers and activators of transcription 1, and upregulation of suppressor of cytokine signaling-3 in rats. J. Pineal Res. 2011, 51, 233–245. [Google Scholar] [CrossRef]
- Jung-Hynes, B.; Schmit, T.L.; Reagan-Shaw, S.R.; Siddiqui, I.A.; Mukhtar, H.; Ahmad, N. Melatonin, a novel Sirt1 inhibitor, imparts antiproliferative effects against prostate cancer in vitro in culture and in vivo in TRAMP model. J. Pineal Res. 2010, 50, 140–149. [Google Scholar] [CrossRef]
- Cheng, Y.; Cai, L.; Jiang, P.; Wang, J.; Gao, C.; Feng, H.; Wang, C.; Pan, H.; Yang, Y. SIRT1 inhibition by melatonin exerts antitumor activity in human osteosarcoma cells. Eur. J. Pharmacol. 2013, 715, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Scott, F.F.; Belle, M.; Delagrange, P.; Piggins, H.D. Electrophysiological Effects of Melatonin on Mouse Per1 and non-Per1 Suprachiasmatic Nuclei Neurones In Vitro. J. Neuroendocr. 2010, 22, 1148–1156. [Google Scholar] [CrossRef]
- Lima, A.C.P.; Louzada, P.R.; De Mello, F.G.; Ferreira, S.T. Neuroprotection Against Aβ and Glutamate Toxicity by Melatonin: Are GABA Receptors Involved? Neurotox. Res. 2003, 5, 323–328. [Google Scholar] [CrossRef]
- Matsuta, Y.; Yusup, A.; Tanase, K.; Ishida, H.; Akino, H.; Yokoyama, O. Melatonin Increases Bladder Capacity via GABAergic System and Decreases Urine Volume in Rats. J. Urol. 2010, 184, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Andrews-Zwilling, Y.; Bien-Ly, N.; Xu, Q.; Li, G.; Bernardo, A.; Yoon, S.Y.; Zwilling, D.; Yan, T.X.; Chen, L.; Huang, Y. Apolipoprotein E4 Causes Age- and Tau-Dependent Impairment of GABAergic Interneurons, Leading to Learning and Memory Deficits in Mice. J. Neurosci. 2010, 30, 13707–13717. [Google Scholar] [CrossRef]
- Hardeland, R. Melatonin and the theories of aging: A critical appraisal of melatonin’s role in antiaging mechanisms. J. Pineal Res. 2013, 55, 325–356. [Google Scholar] [CrossRef] [PubMed]
- Sansoni, P.; Vescovini, R.; Fagnoni, F.; Biasini, C.; Zanni, F.; Zanlari, L.; Telera, A.; Lucchini, G.; Passeri, G.; Monti, D.; et al. The immune system in extreme longevity. Exp. Gerontol. 2008, 43, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Ponnappan, S.; Ponnappan, U.; Zheng, Y.; Joyce, B.T.; Colicino, E.; Liu, L.; Zhang, W.; Dai, Q.; Shrubsole, M.J.; Kibbe, W.A.; et al. Aging and Immune Function: Molecular Mechanisms to Interventions. Antioxid. Redox Signal. 2011, 14, 1551–1585. [Google Scholar] [CrossRef]
- Candore, G.; Colonna-Romano, G.; Balistreri, C.R.; Di Carlo, D.; Grimaldi, M.P.; Listì, F.; Nuzzo, D.; Vasto, S.; Lio, D.; Caruso, C. Biology of Longevity: Role of the Innate Immune System. Rejuvenation Res. 2006, 9, 143–148. [Google Scholar] [CrossRef]
- Bouatia-Naji, N.; Bonnefond, A.; Cavalcanti-Proença, C.; Sparsø, T.; Holmkvist, J.; Marchand, M.; Delplanque, J.; Lobbens, S.; Rocheleau, G.; Durand, E.; et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat. Genet. 2008, 41, 89–94. [Google Scholar] [CrossRef]
- Lyssenko, V.; Nagorny, C.L.; Erdos, M.R.; Wierup, N.; Jonsson, A.; Spégel, P.; Bugliani, M.; Saxena, R.; Fex, M.; Pulizzi, N.; et al. Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat. Genet. 2009, 41, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Prokopenko, I.; Langenberg, C.; Florez, J.C.; Saxena, R.; Soranzo, N.; Thorleifsson, G.; Loos, R.J.F.; Manning, A.K.; Jackson, A.U.; Aulchenko, Y.; et al. Variants in MTNR1B influence fasting glucose levels. Nat. Genet. 2008, 41, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Tarnowski, M.; Malinowski, D.; Safranow, K.; Dziedziejko, V.; Pawlik, A. MTNR1A and MTNR1B gene polymorphisms in women with gestational diabetes. Gynecol. Endocrinol. 2017, 33, 395–398. [Google Scholar] [CrossRef]
- Yang, P.; Liu, H.; Lin, J.; Yang, H. The Association of rs4753426 Polymorphism in the Melatonin Receptor 1B (MTNR1B) Gene and Susceptibility to Adolescent Idiopathic Scoliosis: A Systematic Review and Meta-analysis. Pain Physician 2015, 18, 419–431. [Google Scholar] [CrossRef]
- Li, C.; Shi, Y.; You, L.; Wang, L.; Chen, Z.-J. Melatonin Receptor 1A Gene Polymorphism Associated with Polycystic Ovary Syndrome. Gynecol. Obstet. Investig. 2011, 72, 130–134. [Google Scholar] [CrossRef]
- Su, S.-C.; Ho, Y.-C.; Liu, Y.-F.; Reiter, R.J.; Chou, C.-H.; Yeh, C.-M.; Lee, H.-L.; Chung, W.-H.; Hsieh, M.-J.; Yang, S.-F. Association of melatonin membrane receptor 1A/1B gene polymorphisms with the occurrence and metastasis of hepatocellular carcinoma. Oncotarget 2017, 8, 85655–85669. [Google Scholar] [CrossRef]
- Mestre, H.; Hablitz, L.M.; Xavier, A.L.; Feng, W.; Zou, W.; Pu, T.; Monai, H.; Murlidharan, G.; Rivera, R.M.C.; Simon, M.J.; et al. Aquaporin-4-dependent glymphatic solute transport in the rodent brain. Elife 2018, 7, 30561329. [Google Scholar] [CrossRef] [PubMed]
- Lindblad, C.; Nelson, D.W.; Zeiler, F.A.; Ercole, A.; Ghatan, P.H.; von Horn, H.; Risling, M.; Svensson, M.; Agoston, D.V.; Bellander, B.-M.; et al. Influence of Blood–Brain Barrier Integrity on Brain Protein Biomarker Clearance in Severe Traumatic Brain Injury: A Longitudinal Prospective Study. J. Neurotrauma 2020, 37, 1381–1391. [Google Scholar] [CrossRef]
- Olczak, M.; Niderla-Bielińska, J.; Kwiatkowska, M.; Samojłowicz, D.; Tarka, S.; Wierzba-Bobrowicz, T. Tau protein (MAPT) as a possible biochemical marker of traumatic brain injury in postmortem examination. Forensic Sci. Int. 2017, 280, 1–7. [Google Scholar] [CrossRef]
- Sullan, M.J.; Asken, B.M.; Jaffee, M.S.; DeKosky, S.T.; Bauer, R.M. Glymphatic system disruption as a mediator of brain trauma and chronic traumatic encephalopathy. Neurosci. Biobehav. Rev. 2018, 84, 316–324. [Google Scholar] [CrossRef]
- Xie, L.; Kang, H.; Xu, Q.; Chen, M.J.; Liao, Y.; Thiyagarajan, M.; O’Donnell, J.; Christensen, D.J.; Nicholson, C.; Iliff, J.J.; et al. Sleep Drives Metabolite Clearance from the Adult Brain. Science 2013, 342, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.-X.; Manchester, L.C.; Reiter, R.J. CSF generation by pineal gland results in a robust melatonin circadian rhythm in the third ventricle as an unique light/dark signal. Med. Hypotheses 2015, 86, 3–9. [Google Scholar] [CrossRef]
- Hashimoto, P.H.; Sun, S.-Q. Venous Microvasculature of the Pineal Body and Choroid Plexus in the Rat. J. Electron Microsc. 1991, 40, 29–33. [Google Scholar] [CrossRef]
- Reiter, R.J.; Sharma, R.; Cucielo, M.S.; Tan, D.X.; Rosales-Corral, S.; Gancitano, G.; de Almeida Chuffa, L.G. Brain washing and neural health: Role of age, sleep, and the cerebrospinal fluid melatonin rhythm. Cell. Mol. Life Sci. 2023, 80, 88. [Google Scholar] [CrossRef]
- Grima, N.A.; Ponsford, J.L.; Hilaire, M.A.S.; Mansfield, D.; Rajaratnam, S.M. Circadian Melatonin Rhythm Following Traumatic Brain Injury. Neurorehabilit. Neural Repair 2016, 30, 972–977. [Google Scholar] [CrossRef]
- Seifman, M.A.; Gomes, K.; Nguyen, P.N.; Bailey, M.; Rosenfeld, J.V.; Cooper, D.J.; Morganti-Kossmann, M.C. Measurement of Serum Melatonin in Intensive Care Unit Patients: Changes in Traumatic Brain Injury, Trauma, and Medical Conditions. Front. Neurol. 2014, 5, 237. [Google Scholar] [CrossRef]
- Jang, S.H.; Kwon, H.G. Injury of the Ascending Reticular Activating System in Patients with Fatigue and Hypersomnia Following Mild Traumatic Brain Injury. Medicine 2016, 95, e2628. [Google Scholar] [CrossRef] [PubMed]
- Espino, J.; Pariente, J.A.; Rodríguez, A.B. Oxidative Stress and Immunosenescence: Therapeutic Effects of Melatonin. Oxidative Med. Cell. Longev. 2012, 2012, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yaeger, K.; Alhilali, L.; Fakhran, S. Evaluation of Tentorial Length and Angle in Sleep-Wake Disturbances After Mild Traumatic Brain Injury. Am. J. Roentgenol. 2014, 202, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Rasmussen, L.; Saraswati, M.; Koehler, R.C.; Robertson, C.; Kannan, S.; Missault, S.; Anckaerts, C.; Blockx, I.; Deleye, S.; et al. Traumatic Injury Leads to Inflammation and Altered Tryptophan Metabolism in the Juvenile Rabbit Brain. J. Neurotrauma 2019, 36, 74–86. [Google Scholar] [CrossRef]
- Paparrigopoulos, T.; Melissaki, A.; Tsekou, H.; Efthymiou, A.; Kribeni, G.; Baziotis, N.; Geronikola, X. Melatonin secretion after head injury: A pilot study. Brain Inj. 2006, 20, 873–878. [Google Scholar] [CrossRef]
- Shekleton, J.A.; Parcell, D.L.; Redman, J.R.; Phipps-Nelson, J.; Ponsford, J.L.; Rajaratnam, S.M.W. Sleep disturbance and melatonin levels following traumatic brain injury. Neurology 2010, 74, 1732–1738. [Google Scholar] [CrossRef]
- Rzepka-Migut, B.; Paprocka, J. Melatonin-Measurement Methods and the Factors Modifying the Results. A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 1916. [Google Scholar] [CrossRef]
- Benloucif, S.; Burgess, H.J.; Klerman, E.B.; Lewy, A.J.; Middleton, B.; Murphy, P.J.; Parry, B.L.; Revell, V.L. Measuring Melatonin in Humans. J. Clin. Sleep Med. 2008, 4, 66–69. [Google Scholar] [CrossRef]
- Ramakrishnan, K.; Scheid, D.C. Treatment options for insomnia. Am. Fam. Physician 2007, 76, 517–526. [Google Scholar]
- Savage, R.A.; Zafar, N.; Yohannan, S.; Miller, J.-M.M. Melatonin. In StatPearls; StatPearls: Tampa, FA, USA, 2022. [Google Scholar]
- Vural, E.; Munster, B.; Rooij, S. Optimal dosages for melatonin supplementation therapy in older adults: A systematic review of current literature. Drugs Aging 2014, 31, 441–451. [Google Scholar] [CrossRef]
- Besag, F.M.C.; Vasey, M.J.; Lao, K.S.J.; Wong, I.C.K. Adverse Events Associated with Melatonin for the Treatment of Primary or Secondary Sleep Disorders: A Systematic Review. CNS Drugs 2019, 33, 1167–1186. [Google Scholar] [CrossRef] [PubMed]
- Brzezinski, A.; Vangel, M.G.; Wurtman, R.J.; Norrie, G.; Zhdanova, I.; Ben-Shushan, A.; Ford, I. Effects of exogenous melatonin on sleep: A meta-analysis. Sleep Med. Rev. 2005, 9, 41–50. [Google Scholar] [CrossRef]
- Gao, C.; Nie, M.; Huang, J.; Tian, Y.; Wang, D.; Zhang, J.; Jiang, R. Pharmacotherapy for mild traumatic brain injury: An overview of the current treatment options. Expert Opin. Pharmacother. 2022, 23, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Minkel, J.; Krystal, A.D. Optimizing the Pharmacologic Treatment of Insomnia: Current Status and Future Horizons. Sleep Med. Clin. 2013, 8, 333–350. [Google Scholar] [CrossRef] [PubMed]
- Hardeland, R.; Poeggeler, B.; Srinivasan, V.; Trakht, I.; Pandi-Perumal, S.R.; Cardinali, D.P. Melatonergic drugs in clinical practice. Arzneimittel-Forschung 2008, 58, 1–10. [Google Scholar] [CrossRef]
- Liu, J.; Clough, S.J.; Hutchinson, A.J.; Adamah-Biassi, E.B.; Popovska-Gorevski, M.; Dubocovich, M.L. MT1 and MT2 Melatonin Receptors: A Therapeutic Perspective. Annu. Rev. Pharmacol. Toxicol. 2016, 56, 361–383. [Google Scholar] [CrossRef]
- Zarezadeh, M.; Barzegari, M.; Aghapour, B.; Adeli, S.; Khademi, F.; Musazadeh, V.; Jamilian, P.; Jamilian, P.; Fakhr, L.; Chehregosha, F.; et al. Melatonin effectiveness in amelioration of oxidative stress and strengthening of antioxidant defense system: Findings from a systematic review and dose–response meta-analysis of controlled clinical trials. Clin. Nutr. ESPEN 2022, 48, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Herrera, E.A.; Macchiavello, R.; Montt, C.; Ebensperger, G.; Díaz, M.; Ramírez, S.; Parer, J.T.; Serón-Ferré, M.; Reyes, R.V.; Llanos, A.J. Melatonin improves cerebrovascular function and decreases oxidative stress in chronically hypoxic lambs. J. Pineal Res. 2014, 57, 33–42. [Google Scholar] [CrossRef]
- Aly, H.; Elmahdy, H.; El-Dib, M.; Rowisha, M.; Awny, M.; El-Gohary, T.; Elbatch, M.; Hamisa, M.; El-Mashad, A.-R. Melatonin use for neuroprotection in perinatal asphyxia: A randomized controlled pilot study. J. Perinatol. 2014, 35, 186–191. [Google Scholar] [CrossRef]
- Chumboatong, W.; Thummayot, S.; Govitrapong, P.; Tocharus, C.; Jittiwat, J.; Tocharus, J. Neuroprotection of agomelatine against cerebral ischemia/reperfusion injury through an antiapoptotic pathway in rat. Neurochem. Int. 2017, 102, 114–122. [Google Scholar] [CrossRef]
- Herrera, F.; Sainz, R.M.; Mayo, J.C.; Martin, V.; Antolin, I.; Rodriguez, C. Glutamate induces oxidative stress not mediated by glutamate receptors or cystine transporters: Protective effect of melatonin and other antioxidants. J. Pineal Res. 2001, 31, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Gajardo, R.; Matamala, J.M.; Carrasco, R.; Gutiérrez, R.; Melo, R.; Rodrigo, R. Novel Therapeutic Strategies for Traumatic Brain Injury: Acute Antioxidant Reinforcement. CNS Drugs 2014, 28, 229–248. [Google Scholar] [CrossRef]
- Leon, J.; Acuña-Castroviejo, D.; Sainz, R.M.; Mayo, J.C.; Tan, D.-X.; Reiter, R.J. Melatonin and mitochondrial function. Life Sci. 2004, 75, 765–790. [Google Scholar] [CrossRef]
- Ding, K.; Wang, H.; Xu, J.; Li, T.; Zhang, L.; Ding, Y.; Zhu, L.; He, J.; Zhou, M. Melatonin stimulates antioxidant enzymes and reduces oxidative stress in experimental traumatic brain injury: The Nrf2–ARE signaling pathway as a potential mechanism. Free Radic. Biol. Med. 2014, 73, 1–11. [Google Scholar] [CrossRef]
- Hardeland, R. Melatonin and Microglia. Int. J. Mol. Sci. 2021, 22, 8296. [Google Scholar] [CrossRef]
- Kilic, E.; Kilic, Ü.; Reiter, R.J.; Bassetti, C.L.; Hermann, D.M. Tissue-plasminogen activator-induced ischemic brain injury is reversed by melatonin: Role of iNOS and Akt. J. Pineal Res. 2005, 39, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, S.; Ma, Y.; Xiang, A.; Sun, H.; Song, J.; Yang, W.; Li, X.; Xu, H. Melatonin protected against myocardial infarction injury in rats through a Sirt6-dependent antioxidant pathway. Adv. Clin. Exp. Med. 2022, 31, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Ran, Y.; Ye, L.; Ding, Z.; Gao, F.; Yang, S.; Fang, B.; Liu, Z.; Xi, J. Melatonin Protects Against Ischemic Brain Injury by Modulating PI3K/AKT Signaling Pathway via Suppression of PTEN Activity. ASN Neuro 2021, 13, 17590914211022888. [Google Scholar] [CrossRef]
- Wang, Z.; Zhou, F.; Dou, Y.; Tian, X.; Liu, C.; Li, H.; Shen, H.; Chen, G. Melatonin Alleviates Intracerebral Hemorrhage-Induced Secondary Brain Injury in Rats via Suppressing Apoptosis, Inflammation, Oxidative Stress, DNA Damage, and Mitochondria Injury. Transl. Stroke Res. 2017, 9, 74–91. [Google Scholar] [CrossRef]
- Jerez-Calero, A.; Salvatierra-Cuenca, M.T.; Benitez-Feliponi, A.; Fernández-Marín, C.E.; Narbona-López, E.; Uberos-Fernández, J.; Muñoz-Hoyos, A. Hypothermia Plus Melatonin in Asphyctic Newborns: A Randomized-Controlled Pilot Study. Pediatr. Crit. Care Med. 2020, 21, 647–655. [Google Scholar] [CrossRef]
- Yıldız, E.P.; Ekici, B.; Tatlı, B. Neonatal hypoxic ischemic encephalopathy: An update on disease pathogenesis and treatment. Expert Rev. Neurother. 2017, 17, 449–459. [Google Scholar] [CrossRef]
- Marseglia, L.; Gitto, E.; Laschi, E.; Giordano, M.; Romeo, C.; Cannavò, L.; Toni, A.L.; Buonocore, G.; Perrone, S. Antioxidant Effect of Melatonin in Preterm Newborns. Oxidative Med. Cell. Longev. 2021, 2021, 1–8. [Google Scholar] [CrossRef]
- Merchant, N.M.; Azzopardi, D.V.; Hawwa, A.F.; McElnay, J.C.; Middleton, B.; Arendt, J.; Arichi, T.; Gressens, P.; Edwards, A.D. Pharmacokinetics of melatonin in preterm infants. Br. J. Clin. Pharmacol. 2013, 76, 725–733. [Google Scholar] [CrossRef]
- McCrory, P.; Meeuwisse, W.; Dvorak, J.; Aubry, M.; Bailes, J.; Broglio, S.; Cantu, R.C.; Cassidy, D.; Echemendia, R.J.; Castellani, R.J.; et al. Consensus statement on concussion in sport—The 5th international conference on concussion in sport held in Berlin, October. Br. J. Sports Med. 2017, 51, 838–847. [Google Scholar] [CrossRef]
- Skolnick, B.E.; Maas, A.I.; Narayan, R.K.; van der Hoop, R.G.; MacAllister, T.; Ward, J.D.; Nelson, N.R.; Stocchetti, N. A Clinical Trial of Progesterone for Severe Traumatic Brain Injury. N. Engl. J. Med. 2014, 371, 2467–2476. [Google Scholar] [CrossRef] [PubMed]
- Arango, M.F.; Bainbridge, D. Magnesium for acute traumatic brain injury. Cochrane Database Syst. Rev. 2008, 4, CD005400. [Google Scholar] [CrossRef]
- Nichol, A.; French, C.; Little, L.; Haddad, S.; Presneill, J.; Arabi, Y.; Bailey, M.; Cooper, D.J.; Duranteau, J.; Huet, O.; et al. Erythropoietin in traumatic brain injury (EPO-TBI): A double-blind randomised controlled trial. Lancet 2015, 386, 2499–2506. [Google Scholar] [CrossRef] [PubMed]
- Robertson, C.S.; Hannay, H.J.; Yamal, J.-M.; Gopinath, S.; Goodman, J.C.; Tilley, B.C.; Baldwin, A.; Rivera-Lara, L.; Saucedo-Crespo, H.; Ahmed, O.; et al. Effect of Erythropoietin and Transfusion Threshold on Neurological Recovery After Traumatic Brain Injury. JAMA 2014, 312, 36–47. [Google Scholar] [CrossRef]
- Bennett, M.H.; Trytko, B.; Jonker, B. Hyperbaric oxygen therapy for the adjunctive treatment of traumatic brain injury. Cochrane Database Syst. Rev. 2012, 12, CD004609. [Google Scholar] [CrossRef] [PubMed]
- Mazzeo, A.T.; Brophy, G.M.; Gilman, C.B.; Scar, O.; Alves, L.; Robles, J.R.; Hayes, R.L.; Povlishock, J.T.; Bullock, M.R. Safety and Tolerability of Cyclosporin A in Severe Traumatic Brain Injury Patients: Results from a Prospective Randomized Trial. J. Neurotrauma 2009, 26, 2195–2206. [Google Scholar] [CrossRef]
- Effect of intravenous corticosteroids on death within 14 days in 10 008 adults with clinically significant head injury (MRC CRASH trial): Randomised placebo-controlled trial. Lancet 2004, 364, 1321–1328. [CrossRef]
- Zetner, D.; Andersen LP, K.; Alder, R.; Jessen, M.L.; Tolstrup, A.; Rosenberg, J. Pharmacokinetics and Safety of Intravenous, Intravesical, Rectal, Transdermal, and Vaginal Melatonin in Healthy Female Volunteers: A Cross-Over Study. Pharmacology 2021, 106, 169–176. [Google Scholar] [CrossRef]
- Dominguez-Rodriguez, A.; Abreu-Gonzalez, P.; de la Torre-Hernandez, J.M.; Gonzalez-Gonzalez, J.; Garcia-Camarero, T.; Consuegra-Sanchez, L.; Garcia-Saiz, M.D.M.; Aldea-Perona, A.; Virgos-Aller, T.; Azpeitia, A.; et al. Effect of intravenous and intracoronary melatonin as an adjunct to primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: Results of the Melatonin Adjunct in the acute myocaRdial Infarction treated with Angioplasty trial. J. Pineal Res. 2016, 62, e12374. [Google Scholar] [CrossRef]
- Flynn Pharma Ltd. Circadin 2 mg Prolonged-Release Tablets Summary of Product Characteristics. 2021. Available online: https://www.medicinesOrgUk/Emc/Medicine/25643#companyDetails (accessed on 2 February 2023).
- Gandolfi, J.V.; Di Bernardo, A.P.A.; Chanes, D.A.V.; Martin, D.F.; Joles, V.B.; Amendola, C.P.; Sanches, L.C.; Ciorlia, G.L.; Lobo, S.M. The Effects of Melatonin Supplementation on Sleep Quality and Assessment of the Serum Melatonin in ICU Patients: A Randomized Controlled Trial. Crit. Care Med. 2020, 48, e1286–e1293. [Google Scholar] [CrossRef]
- Rehman, S.U.; Ikram, M.; Ullah, N.; Alam, S.I.; Park, H.Y.; Badshah, H.; Choe, K.; Kim, M.O. Neurological Enhancement Effects of Melatonin against Brain Injury-Induced Oxidative Stress, Neuroinflammation, and Neurodegeneration via AMPK/CREB Signaling. Cells 2019, 8, 760. [Google Scholar] [CrossRef] [PubMed]
- Naeser, M.A.; Martin, P.I.; Ho, M.D.; Krengel, M.H.; Bogdanova, Y.; Knight, J.A.; Yee, M.K.; Zafonte, R.; Frazier, J.; Hamblin, M.R.; et al. Transcranial, Red/Near-Infrared Light-Emitting Diode Therapy to Improve Cognition in Chronic Traumatic Brain Injury. Photomed. Laser Surg. 2016, 34, 610–626. [Google Scholar] [CrossRef] [PubMed]
- Ge, J.; Chen, D.; Ben, J.; Song, X.; Zou, L.; Yi, X. Effect of melatonin on regeneration of cortical neurons in rats with traumatic brain injury. Clin. Investig. Med. 2020, 43, E8–16. [Google Scholar] [CrossRef]
- Ozdemir, D.; Tugyan, K.; Uysal, N.; Sonmez, U.; Sonmez, A.; Acikgoz, O.; Ozdemir, N.; Duman, M.; Ozkan, H. Protective effect of melatonin against head trauma-induced hippocampal damage and spatial memory deficits in immature rats. Neurosci. Lett. 2005, 385, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Bao, Z.; Fan, L.; Zhao, L.; Xu, X.; Liu, Y.; Chao, H.; Liu, N.; You, Y.; Liu, Y.; Wang, X.; et al. Silencing of A20 Aggravates Neuronal Death and Inflammation After Traumatic Brain Injury: A Potential Trigger of Necroptosis. Front. Mol. Neurosci. 2019, 12, 222. [Google Scholar] [CrossRef]
- Wang, Z.; Ma, C.; Meng, C.-J.; Zhu, G.-Q.; Sun, X.-B.; Huo, L.; Zhang, J.; Liu, H.-X.; He, W.-C.; Shen, X.-M.; et al. Melatonin activates the Nrf2-ARE pathway when it protects against early brain injury in a subarachnoid hemorrhage model. J. Pineal Res. 2012, 53, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Nazıroğlu, M.; Şenol, N. Melatonin reduces traumatic brain injury-induced oxidative stress in the cerebral cortex and blood of rats. Neural Regen. Res. 2014, 9, 1112–1116. [Google Scholar] [CrossRef]
- Ding, K.; Xu, J.; Wang, H.; Zhang, L.; Wu, Y.; Li, T. Melatonin protects the brain from apoptosis by enhancement of autophagy after traumatic brain injury in mice. Neurochem. Int. 2015, 91, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Ates, O.; Çayli, S.; Gurses, I.; Yucel, N.; Iraz, M.; Altinoz, E.; Kocak, A.; Yologlu, S. Effect of pinealectomy and melatonin replacement on morphological and biochemical recovery after traumatic brain injury. Int. J. Dev. Neurosci. 2006, 24, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Beni, S.M.; Kohen, R.; Reiter, R.J.; Tan, D.; Shohami, E. Melatonin-induced neuroprotection after closed head injury is associated with increased brain antioxidants and attenuated late-phase activation of NF-κB and AP-1. FASEB J. 2003, 18, 149–151. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, F.; Hadad, M.K.; Asadikram, G.; Najafipour, H.; Shahrokhi, N. Effect of Melatonin on Intracranial Pressure and Brain Edema Following Traumatic Brain Injury: Role of Oxidative Stresses. Arch. Med Res. 2013, 44, 251–258. [Google Scholar] [CrossRef]
- Ding, K.; Wang, H.; Xu, J.; Lu, X.; Zhang, L.; Zhu, L. Melatonin reduced microglial activation and alleviated neuroinflammation induced neuron degeneration in experimental traumatic brain injury: Possible involvement of mTOR pathway. Neurochem. Int. 2014, 76, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Kabadi, S.V.; Maher, T.J. Posttreatment with uridine and melatonin following traumatic brain injury reduces edema in various brain regions in rats. Ann. N. Y. Acad. Sci. 2010, 1199, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Kelso, M.L.; Scheff, N.N.; Scheff, S.W.; Pauly, J.R. Melatonin and minocycline for combinatorial therapy to improve functional and histopathological deficits following traumatic brain injury. Neurosci. Lett. 2011, 488, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Chao, H.; Li, Z.; Xu, X.; Liu, Y.; Hou, L.; Liu, N.; Ji, J. Melatonin attenuates traumatic brain injury-induced inflammation: A possible role for mitophagy. J. Pineal Res. 2016, 61, 177–186. [Google Scholar] [CrossRef]
- Mésenge, C.; Margaill, I.; Verrecchia, C.; Allix, M.; Boulu, R.G.; Plotkine, M.; Marchand-Leroux, C. Protective effect of melatonin in a model of traumatic brain injury in mice. J. Pineal Res. 1998, 25, 41–46. [Google Scholar] [CrossRef]
- Sarrafzadeh, A.S.; Thomale, U.-W.; Kroppenstedt, S.-N.; Unterberg, A.W. Neuroprotective Effect of Melatonin on Cortical Impact Injury in the Rat. Acta Neurochir. 2000, 142, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Shao, A.; Zhao, M.; Chen, S.; Yu, J.; Zhou, J.; Liang, F.; Shi, L.; Dixon, B.J.; Wang, Z.; et al. Melatonin attenuates neuronal apoptosis through up-regulation of K+-Cl−cotransporter KCC2 expression following traumatic brain injury in rats. J. Pineal Res. 2016, 61, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Yamakawa, G.R.; Salberg, S.; Barlow, K.M.; Brooks, B.L.; Esser, M.J.; Yeates, K.O.; Mychasiuk, R. Manipulating cognitive reserve: Pre-injury environmental conditions influence the severity of concussion symptomology, gene expression, and response to melatonin treatment in rats. Exp. Neurol. 2017, 295, 55–65. [Google Scholar] [CrossRef] [PubMed]
| Citation | Title | Design | Key Findings |
|---|---|---|---|
| Kaleyias and Kothare, 2022 [30] | Sleep Disorders in Traumatic Brain Injury | Literature Review | Factors implicated in sleep disturbance following TBI include reduced hypocretin signaling, damage to histaminergic tuberomammillary neurons, disruption of circadian regulation impairing melatonin synthesis, and parenchymal damage involving the ascending reticular activating system, basal ganglia, and limbic system. Human observational studies implicate substantial loss of histaminergic neurons and impaired melatonin synthesis as significant pathophysiologic contributors up to 6 months after injury. |
| Naseem and Parvez, 2014 [31] | Role of Melatonin in Traumatic Brain Injury and Spinal Cord Injury: A Review | Literature Review 9 Studies | In animal models, melatonin has neuroprotective effects on both TBI and spinal cord injury (SCI). Mechanisms for observed benefit are largely owed to anti-inflammatory and anti-oxidative action leading to a reduction in cerebral edema, decreased NFkB, decreased AP-1, stabilization of Nitric Oxide Species (NOS), increased superoxide dismutase and glutathione peroxidase. Measurements of melatonin in the CSF increase acutely following TBI. |
| Stewart et al., 2022 [32] | Treating Sleep Disorders Following Traumatic Brain Injury in Adults: Time for Renewed Effort? | Systematic Review 18 Articles | Pathophysiology of sleep disruption following TBI remains poorly understood. Circadian rhythm dysfunction was common acutely (10 days), and low melatonin production is found up to a year post injury and associated with reduced sleep quality. Recommendation for clinical use of melatonin to treat sleep dysfunction following TBI is supported but cautioned against given the paucity of published data from human RCTs. |
| Gagner et al., 2015 [33] | Sleep-wake Disturbances and Fatigue after Pediatric Traumatic Brain Injury: A Systematic Review of the Literature. | Systematic Review | From over 20 identified pathologic characteristics from human and animal models from studies investigating neuropathology, only 4 were observed concurrently in both. Shared findings included decreased hypothalamic orexin, increased slow waveform during wakefulness on EEG, increased sleep fragmentation, and increased sleep time, suggesting higher validity and utility for these findings when investigating the pathophysiologic mechanism for sleep dysfunction after TBI. |
| Driver and Stork, 2018 [34] | Pharmacological Management of Sleep After Traumatic Brain Injury | Literature Review | Melatonin administration following TBI may improve subjective daytime alertness, but a comprehensive understanding of its restorative impact on sleep fragmentation is limited by a lack of rigorous RCTs with objective sleep data. In one double-blind placebo-controlled trial of 13 individuals with TBI, the melatonin agonist Ramelteon improved total sleep duration and cognitive performance following the 3-week trial. |
| Osier et al., 2018 [35] | Melatonin as a Therapy for Traumatic Brain Injury: A Review of Published Evidence | Literature Review 22 articles | In animal models, melatonin conferred neuroprotective benefits following TBI via antioxidative action, downregulation of NFkB and AP-1, and decreased apoptosis leading to reduced contusion volume during the evening. Majority of reports support the potential use of melatonin in treating human patients following TBI. |
| Barlow et al., 2019 [36] | Melatonin as a Treatment after Traumatic Brain Injury: A Systematic Review and Meta-Analysis of the Pre-Clinical and Clinical Literature | Meta-analysis 17 studies | From 15 pre-clinical studies, melatonin had an overall beneficial effect on subject outcomes with improvement in cognitive performance and motor function. Pertinent clinical trials included a post-concussive pediatric population that benefited from melatonin supplementation to reduce post-traumatic headaches (N = 12). |
| Blum et al., 2021 [37] | Melatonin in Traumatic Brain Injury and Cognition | Literature Review 11 studies | Murine models continue to demonstrate melatonin exerting potent neuroprotective action via anti-inflammatory and antioxidant functions. Evidence for reduced expression of abnormal proteins, including AB and p-tau, following treatment with melatonin after injury highlight a potential future application in decreasing the risk of neurodegenerative disease for which TBI exposure is a risk factor. Longitudinal data on cognitive performance in a treatment population are lacking; however, some evidence for improvement in memory task function acutely after injury does exist. |
| Feinberg et al., 2021 [38] | Association of Pharmacological Interventions with Symptom Burden Reduction in Patients with Mild Traumatic Brain Injury: A Systematic Review | Systematic Review 23 studies | Review of 23 studies (11 randomized clinical trials, 7 prospective observational studies, 3 retrospective observational studies, and 2 case studies) examining 20 pharmacological interventions; while methylphenidate, sertraline hydrochloride, ondansetron, amitriptyline, and melatonin were adequately represented— consistent symptom burden reduction was limited. |
| Ali et al., 2022 [39] | Fatigue After Traumatic Brain Injury: A Systematic Review | Systematic Review | Review of 37 articles showed methylphenidate and melatonin were the only pharmacological agents associated with decreased fatigue in RCTs. |
| Samantaray et al., 2009 [40] | Therapeutic Potential of Melatonin in Traumatic Central Nervous System Injury | Mini Review | Mini review exploring and summarizing characteristics and benefits of melatonin as neuroprotectant/treatment for acute SCI or traumatic CNS injuries. |
| Reiter et al., 2016 [41] | Melatonin as an Antioxidant: Under Promises but Over Delivers | Literature Review | Review articles summarizing the evolutionary history of melatonin as well as its biochemical pathways and physiological effects in healthy and injured states. |
| Cassimatis et al., 2022 [42] | The Utility of Melatonin for the Treatment of Sleep Disturbance Following Traumatic Brain Injury | Literature Review 9 studies | A total of 5 RCTs on adults and adolescents showed that post-TBI melatonin treatment improved subjective and objective sleep measures as well as mental health symptoms, executive function, and cognition. |
| Citation | Title | Design | Key Findings |
|---|---|---|---|
| Kemp et al., 2004 [43] | The Value of Melatonin for Sleep Disorders Occurring Post-Head Injury: a Pilot RCT | 1 mth, Double blind crossover (N = 7) of TBI patients with insomnia; melatonin 5 mg/d vs. amitriptyline 25 mg/d; 2 wk washout | Melatonin improved daytime alertness compared to baseline (d = 0.42). No treatment effect on insomnia (F (2.48) = 0.98, p > 0.056) was found. |
| Grima et al., 2018 [44] | Efficacy of Melatonin for Sleep Disturbance Following Traumatic Brain Injury: A Randomized Controlled Trial | 4 wk, Double blind crossover (N = 33) of TBI patients with chronic insomnia; melatonin 2 mg/d vs. placebo; 48 h washout | Melatonin improved sleep quality compared to placebo by PSQI (d = 0.46; p < 0.0001). Melatonin improved sleep efficiency (d = 0.28, p = 0.04) but had no effect on sleep onset latency (d = 0.18; p = 0.23). No treatment effect on daytime sleepiness by ESS (d = 0.17, p = 0.15) |
| Lequerica et al., 2015 [45] | Pilot Study on the Effect of Ramelteon on Sleep Disturbance After Traumatic Brain Injury: Preliminary Evidence from a Clinical Trial | 3 wk, Double blind crossover (N = 13) of TBI patients with circadian rhythm disorder | Ramelteon 8 mg nightly improved total sleep time and slightly increased sleep latency. Improvement seen from psychometric tests in executive function. |
| Ilyer et al., 2020 [46] | Neural Correlates of Sleep Recovery following melatonin Treatment for Pediatric Concussion: A Randomized Controlled Trial | Double-blind RCT of pediatric cohort with post-concussion symptoms (N = 62). 3 mg vs. 10 mg melatonin vs. placebo. | fMRI findings show increased connectivity of posterior default mode networks in the melatonin group. |
| Barlow et al., 2020 [47] | Efficacy of Melatonin in Children with Postconcussive Symptoms: A Randomized Clinical Trial | Double-blind RCT of 99 adolescents with PPCS. Placebo vs. 3 mg vs. 10 mg. | No significant difference in outcomes on Post-Concussion Symptom Inventory score measured after 28 days of treatment. However, caveated by wide confidence intervals. |
| Kuczynski et al., 2013 [48] | Characteristics of Post-traumatic Headaches in Children Following Mild Traumatic Brain Injury and their Response to Treatment: A Prospective Cohort. | Prospective pediatric cohort with post-mTBI symptoms (N = 670; 385 males, 285 females) and comparison group with extracranial injury (N = 120; 61 males, 59 females). Retrospective chart review of a separate cohort (treatment cohort) treated for post-traumatic headaches (PTH) with amitriptyline, flunarizine, topiramate, and melatonin, (N = 44; 29 females, 15 males). | Headaches in 9/12 (75%). 13/18 patients (68%) reported a good effect with amitriptyline. |
| Grima et al., 2021 [49] | Poorer Sleep Quality Predicts Melatonin Response in Patients with Traumatic Brain Injury: Findings from a Randomized Controlled Trial | Secondary analysis of phase 3 randomized, placebo-controlled, double-blind, 2-period, 2-treatment crossover clinical trial evaluating the efficacy of melatonin (2 mg, prolonged release) treatment for sleep disturbances in patients with TBI | Severe TBI patients with comorbid insomnia and poorer sleep quality experience most benefit regardless of time since injury, demographics, fatigue, daytimes sleepiness, mood, and anxiety. |
| Dominguez-Rodriguez et al., 2017 [50] | Usefulness of Early Treatment with Melatonin to Reduce Infarct Size in Patients With ST-Segment Elevation Myocardial Infarction Receiving Percutaneous Coronary Intervention (From the Melatonin Adjunct in the Acute Myocardial Infarction Treated With Angioplasty Trial) | Multi-site, double-blind, RCT of STEMI patients in 3 groups. Placebo vs. intracoronary melatonin vs. intravenous melatonin. | Melatonin treatment in STEMI patients who present early after symptom onset was associated with a significant reduction in the infarct size after pPCI. |
| Dominguez-Rodriguez et al., 2022 [51] | Early Treatment of Acute Myocardial Infarction with Melatonin: Effects on MMP-9 and Adverse Cardiac Events | Pilot RCT of melatonin treatment vs. placebo in acute MI patients receiving percutaneous intervention (N = 94). | Melatonin associated with improved outcomes in acute MI patients undergoing primary percutaneous intervention. |
| Ekeloef et al., 2017 [52] | Effect of Intracoronary and Intravenous Melatonin on Myocardial Salvage Index in Patients with ST-Elevation Myocardial Infarction: A Randomized Placebo Controlled Trial. | RCT of STEMI patients in 3 groups. Placebo vs. intracoronary melatonin vs. intravenous melatonin. | No improvement in myocardial salvage index after primary percutaneous coronary intervention in patients with STEMI treated with melatonin vs. placebo. |
| Dwaich et al., 2016 [53] | Melatonin Effects on Myocardial ischemia-reperfusion Injury: Impact on the Outcome in Patients Undergoing Coronary Artery Bypass Grafting Surgery | RCT of 45 patients split into 3 groups: Placebo-controlled group, low dose melatonin group, 10 mg capsule once daily and high dose melatonin group 20 mg capsule once daily. | Dose-dependent melatonin supplementation can ameliorate the degree of myocardial ischemic-reperfusion injury. |
| Indication | Administration | Recommendations |
|---|---|---|
| ASWPD | AASM Consensus panel did not provide a recommendation regarding the use of melatonin for ASWPD [54] | |
| DSWPD | Adult: “Strategically timed,” administration: 0.3–3.0 mg; 1.5–6.5 h prior to DLMO, i.e., 15:00–21:30 for most adult patients Children (6–12 years): 1.5–2.0 h prior to usual sleep time for patients with no comorbidities, with depression, patients without depression; 20–30 min prior to caregivers’ desired bedtime or 18:00, 19:00, for those with comorbid psychiatric disease | AASM Consensus panel, rating in favor of the use of melatonin, as opposed to no treatment. [WEAK] [54] |
| N24SWPD | For “blind adults:” 0.5–10 mg one hour prior to desired bedtime, or consistently at 21:00 | Consensus panel, rating in favor of the use of melatonin, as opposed to no treatment. [WEAK] [54] No recommendation made for sighted adults with N24SWD. |
| Shift work disorder | 1.8–3.0 mg prior to the desired sleep period | Administration of melatonin prior to daytime sleep is indicated to promote daytime sleep among night shift workers. [GUIDELINE] [55] Melatonin improved daytime sleep but did not improve nighttime alertness (work shift alertness). |
| Jetlag | 0.5–10 mg administered at bedtime | Melatonin administered at the appropriate time is indicated to reduce symptoms of jet lag and improve sleep following travel across multiple time zones. [STANDARD] [55] |
| Insomnia | Doses ranging from 0.5–10 mg have been studied for insomnia, but evidence-based guidelines were based on studies using 2 mg | Most evidence-based guidelines recommend against the use of melatonin for insomnia (compared to no treatment), based on low quality evidence, with a limited dose range, failing to demonstrate efficacy). [WEAK] [56,57,58] |
| TBI: misc. sleep dysfunction | 3–10 mg in pediatric and adult patients | Conflicting results, increased daytime alertness, no significant impact on sleep measures [43,59]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bell, A.; Hewins, B.; Bishop, C.; Fortin, A.; Wang, J.; Creamer, J.L.; Collen, J.; Werner, J.K., Jr. Traumatic Brain Injury, Sleep, and Melatonin—Intrinsic Changes with Therapeutic Potential. Clocks & Sleep 2023, 5, 177-203. https://doi.org/10.3390/clockssleep5020016
Bell A, Hewins B, Bishop C, Fortin A, Wang J, Creamer JL, Collen J, Werner JK Jr. Traumatic Brain Injury, Sleep, and Melatonin—Intrinsic Changes with Therapeutic Potential. Clocks & Sleep. 2023; 5(2):177-203. https://doi.org/10.3390/clockssleep5020016
Chicago/Turabian StyleBell, Allen, Bryson Hewins, Courtney Bishop, Amanda Fortin, Jonathan Wang, Jennifer L. Creamer, Jacob Collen, and J. Kent Werner, Jr. 2023. "Traumatic Brain Injury, Sleep, and Melatonin—Intrinsic Changes with Therapeutic Potential" Clocks & Sleep 5, no. 2: 177-203. https://doi.org/10.3390/clockssleep5020016
APA StyleBell, A., Hewins, B., Bishop, C., Fortin, A., Wang, J., Creamer, J. L., Collen, J., & Werner, J. K., Jr. (2023). Traumatic Brain Injury, Sleep, and Melatonin—Intrinsic Changes with Therapeutic Potential. Clocks & Sleep, 5(2), 177-203. https://doi.org/10.3390/clockssleep5020016






