Idiopathic Penile Calcinosis Cutis: A Histopathological Case Report
Abstract
1. Introduction and Clinical Significance
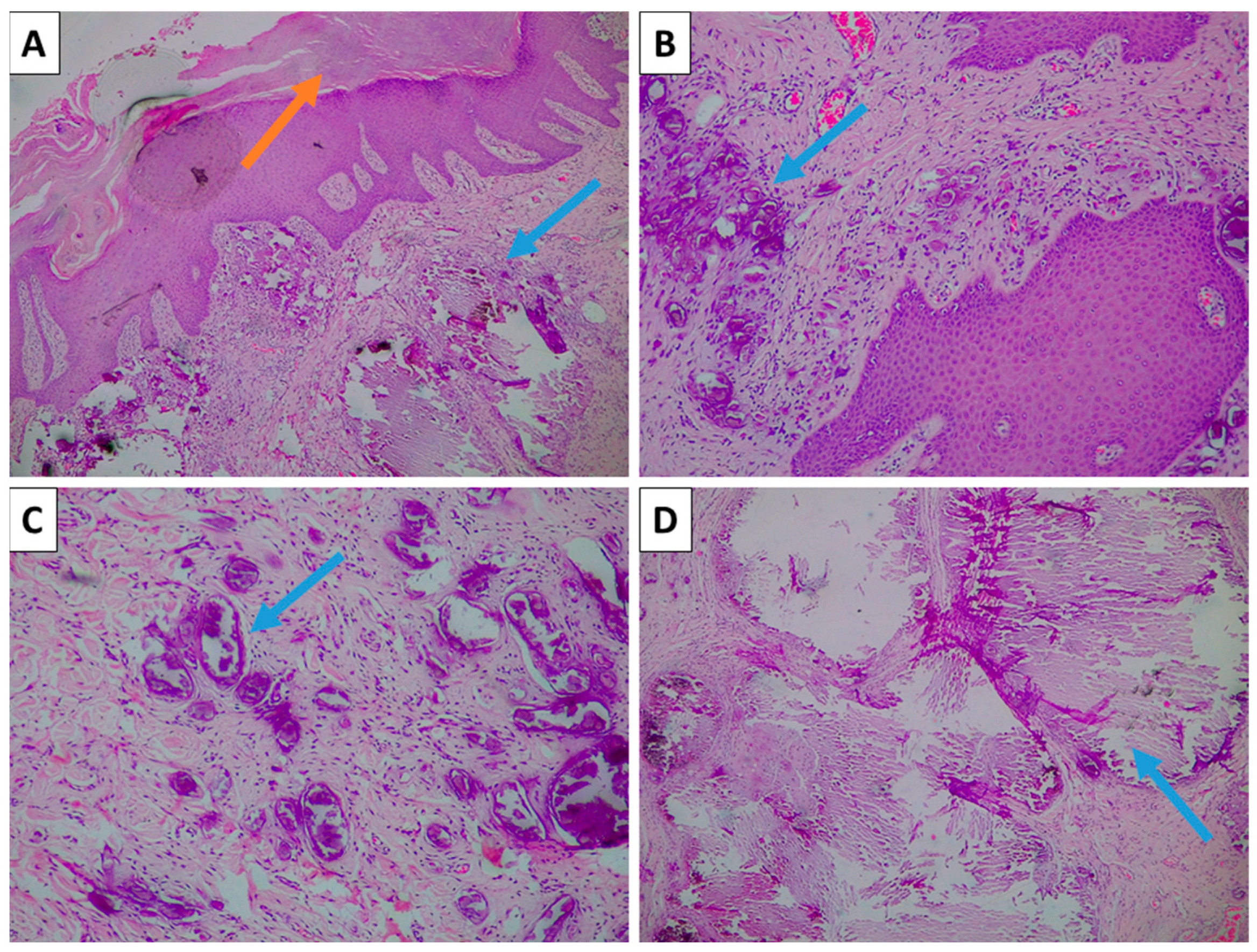
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herrera, M.H.; Díez, E.M.; Martínez, J.M.O. Calcinosis Cutis. Rev. Osteoporos. Metab. Miner. 2023, 15, 160–163. [Google Scholar] [CrossRef]
- Foster, J.; Guerrero, L.; Chong, B.F. Outcome Measures in Dystrophic Calcinosis Cutis: A Systematic Review. JID Innov. 2025, 5, 100368. [Google Scholar] [CrossRef]
- Mehta, N.; Bhoi, A.K.; Khandpur, S. Traumatic Dystrophic Calcinosis Cutis in a Child Successfully Treated with Sodium Metabisulfite Ointment. Indian J. Dermatol. Venereol. Leprol. 2024, 90, 656–658. [Google Scholar] [CrossRef]
- Westphal, S.G.; Plumb, T. Calciphylaxis. Atlas Clin. Vasc. Med. 2023, 114–115. [Google Scholar] [CrossRef]
- García-García, E.; López-López, R.; Álvarez-del-Vayo, C.; Bernabeu-Wittel, J. Iatrogenic Calcinosis Cutis Successfully Treated with Topical Sodium Thiosulfate. Pediatr. Dermatol. 2017, 34, 356–358. [Google Scholar] [CrossRef]
- Rumancik, B.E.; Rahnama-Moghadam, S. Severe Iatrogenic Calcinosis Cutis From Extravasated Calcium Gluconate. Cureus 2020, 12, e9712. [Google Scholar] [CrossRef]
- Róbert, L.; Kuroli, E.; Bottlik, G.; Hidvégi, B. Late-Onset Calcinosis in Burn Scars: A Review of the Literature and Two Case Reports. JDDG J. Dtsch. Dermatol. Gesellschaft 2022, 20, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Al Wadany, M.; Al Wadany, F.; Almousa, A.; Almoussa, F.; Alharbi, A. Idiopathic Calcinosis Cutis in a Child: Report of a Rare Case. Cureus 2023, 15, e34254. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Iqbal, Z.; Mohroo, R.; Khan, S.; Hussain, M. Idiopathic Calcinosis Cutis Presenting as Iliac Region Mass in an Elderly Female: A Rare Entity with Cyto-Histopathological Correlation. Indian J. Dermatopathol. Diagn. Dermatol. 2024, 11, 8–11. [Google Scholar] [CrossRef]
- Crockett, J.L.; Copp, H.L.; Mully, T.W.; Francois, R.A.; Cordoro, K.M. Genital Calcinosis Cutis: Microscopic Evidence Supporting a Dystrophic Origin. Pediatr. Dermatol. 2024, 41, 1188–1192. [Google Scholar] [CrossRef]
- Rout, A.N.; Pradhan, S.; Sirka, C.S. Pinch-Punch Technique for Scrotal Calcinosis Cutis. Indian J. Dermatol. Venereol. Leprol. 2021, 87, 858–860. [Google Scholar] [CrossRef]
- Syed, M.M.A.; Rajbhandari, A.; Paudel, U. Idiopathic Calcinosis Cutis of the Scrotum: A Case Report and Review of the Literature. J. Med. Case Rep. 2018, 12, 366. [Google Scholar] [CrossRef] [PubMed]
- Katoh, N.; Okabayashi, K.; Wakabayashi, S.; Kishimoto, S.; Yasuno, H. Dystrophic Calcinosis of the Penis. J. Dermatol. 1993, 20, 114–117. [Google Scholar] [CrossRef]
- Nigam, J.; Bharti, J.; Nair, V.; Gargade, C.; Deshpande, A.; Dey, B.; Singh, A. Epidermal Cysts: A Clinicopathological Analysis with Emphasis on Unusual Findings. Int. J. Trichology 2017, 9, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Swinehart, J.M.; Golitz, L.E. Scrotal Calcinosis: Dystrophic Calcification of Epidermoid Cysts. Arch. Dermatol. 1982, 118, 985–988. [Google Scholar] [CrossRef]
- Warvi, W.N.; Gates, O. Epithelial Cysts and Cystic Tumors of the Skin. Am. J. Pathol. 1943, 19, 765. [Google Scholar] [PubMed]
- Julian, P.; Krasnaliev, I.; Bakardzhiev, I. Osteoma Cutis—Neoplasia or Paleogenetics? J. Clin. Res. Dermatol. 2019, 6, 1–3. [Google Scholar] [CrossRef]
- Hoang, V.T.; Trinh, C.T.; Nguyen, C.H.; Chansomphou, V.; Chansomphou, V.; Tran, T.T.T. Overview of Epidermoid Cyst. Eur. J. Radiol. Open 2019, 6, 291–301. [Google Scholar] [CrossRef]
- Cohen, P.R.; Tschen, J.A. Idiopathic Calcinosis Cutis of the Penis. J. Clin. Aesthet. Dermatol. 2012, 5, 23. [Google Scholar]
- Cecchi, R.; Giomi, A. Idiopathic Calcinosis Cutis of the Penis. Dermatology 1999, 198, 174–175. [Google Scholar] [CrossRef]
- Sánchez-Merino, J.M.; Bouso-Montero, M.; Fernández-Flores, A.; García-Alonso, J. Idiopathic Calcinosis Cutis of the Penis. J. Am. Acad. Dermatol. 2004, 51, 118–119. [Google Scholar] [CrossRef] [PubMed]
- Cangelosi, J.; Martherne, R.; Sanchez, R. Idiopathic calcinosis cutis of the penis. J. Cutan. Pathol. 2011, 38, 174–175. [Google Scholar]
- Gabel, C.; Chakrala, T.; Shah, R.; Danesh, M.J.; Dobry, A.S.; Garza-Mayers, A.C.; Ko, L.N.; Nguyen, E.; St. John, J.; Walls, A.C.; et al. Penile Calciphylaxis: A Retrospective Case-Control Study. J. Am. Acad. Dermatol. 2021, 85, 1209–1217. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stoyanov, G.; Marchev, D.; Popov, H. Idiopathic Penile Calcinosis Cutis: A Histopathological Case Report. Reports 2025, 8, 248. https://doi.org/10.3390/reports8040248
Stoyanov G, Marchev D, Popov H. Idiopathic Penile Calcinosis Cutis: A Histopathological Case Report. Reports. 2025; 8(4):248. https://doi.org/10.3390/reports8040248
Chicago/Turabian StyleStoyanov, George, Dobri Marchev, and Hristo Popov. 2025. "Idiopathic Penile Calcinosis Cutis: A Histopathological Case Report" Reports 8, no. 4: 248. https://doi.org/10.3390/reports8040248
APA StyleStoyanov, G., Marchev, D., & Popov, H. (2025). Idiopathic Penile Calcinosis Cutis: A Histopathological Case Report. Reports, 8(4), 248. https://doi.org/10.3390/reports8040248





