A 74-Year-Old Man with Massive Ascites: A Case Report of Yellow Nail Syndrome
Abstract
1. Introduction and Clinical Significance
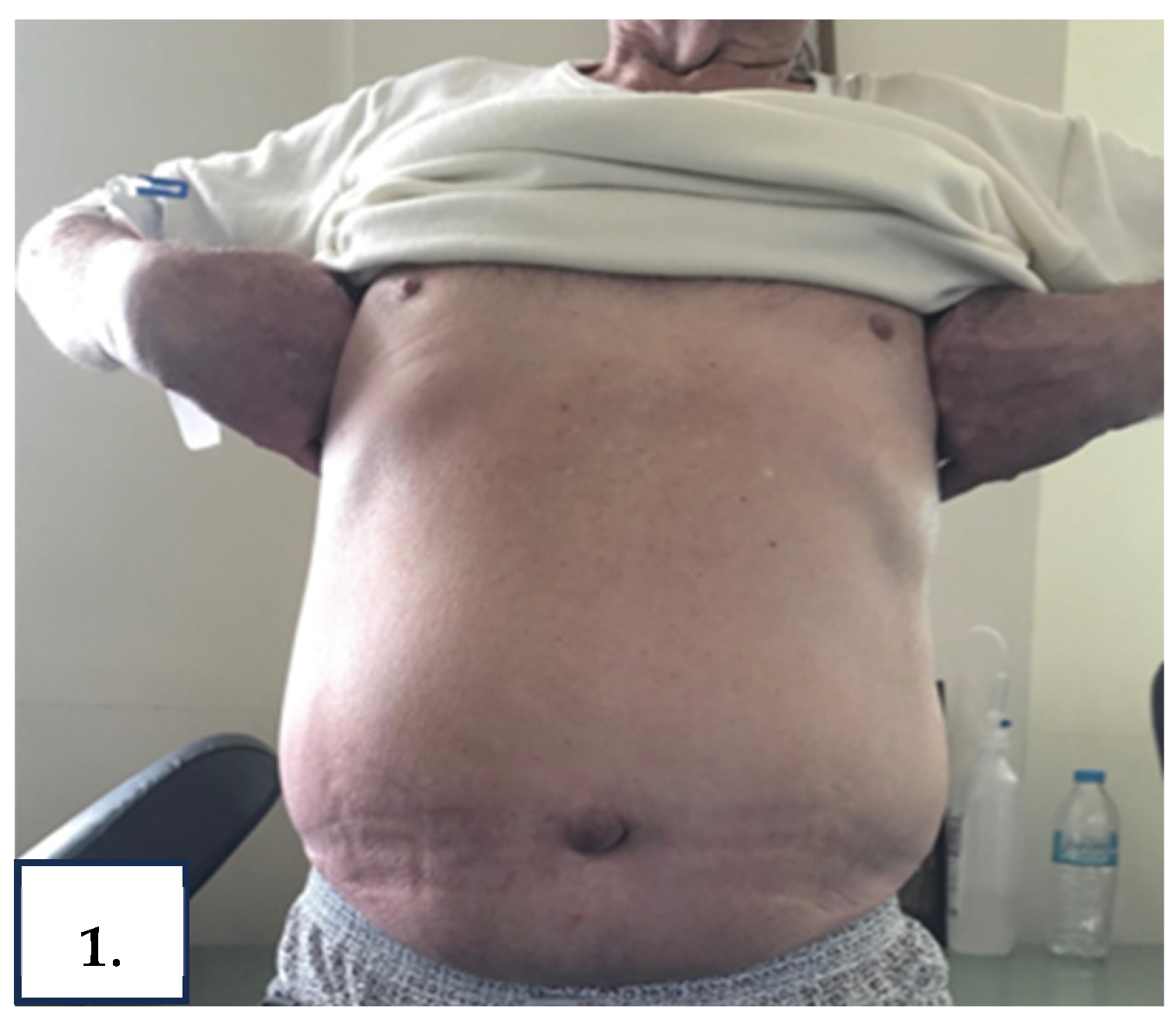
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Vignes, S.; Baran, R. Yellow nail syndrome: A review. Orphanet J. Rare Dis. 2017, 12, 42. [Google Scholar] [CrossRef]
- Maldonado, F.; Tazelaar, H.D.; Wang, C.W.; Ryu, J.H. Yellow nail syndrome: Analysis of 41 consecutive patients. Chest 2008, 134, 375–381. [Google Scholar] [CrossRef]
- Runyon, B.A. Ascites and spontaneous bacterial peritonitis. In Schiff’s Diseases of the Liver, 11th ed.; Schiff, E.R., Madderly, W.C., Sorrell, M.F., Eds.; Wiley-Blackwell: Chisester, UK, 2012; Volume 1, pp. 393–419. [Google Scholar]
- Talluri, S.K.; Nuthakki, H.; Tadakamalla, A.; Talluri, J.; Besur, S. Chylous ascites. N. Am. J. Med. Sci. 2011, 3, 438–440. [Google Scholar] [CrossRef] [PubMed]
- Duhra, P.M.; Quigley, E.M.; Marsh, M.N. Chylous ascites, intestinal lymphangiectasia and the ‘yellow-nail’ syndrome. Gut 1985, 26, 1266–1269. [Google Scholar] [CrossRef]
- Valmary, J.; Delbrouck, P.; Herning, R.; Algayres, J.P.; Fléchaire, A.; Daly, J.P.; Laverdant, C. Yellow nail syndrome with chylous effusions. Rev. Med. Interne 1988, 9, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.C. Dietary treatment of chylous ascites in yellow nail syndrome. Gut 1989, 30, 1622–1623. [Google Scholar] [CrossRef] [PubMed]
- Malek, N.P.; Ocran, K.; Tietge, U.J.; Maschek, H.; Gratz, K.F.; Trautwein, C.; Wagner, S.; Manns, M.P. A case of the yellow nail syndrome associated with massive chylous ascites, pleural and pericardial effusions. Z. Gastroenterol. 1996, 34, 763–766. [Google Scholar]
- Widjaja, A.; Gratz, K.F.; Ockenga, J.; Wagner, S.; Manns, M.P. Octreotide for therapy of chylous ascites in yellow nail syndrome. Gastroenterology 1999, 116, 1017–1018. [Google Scholar] [CrossRef]
- Kuloğlu, Z.; Ustündağ, G.; Kirsaçlioğlu, C.T.; Kansu, A.; Bingol-Kologlu, M.; Vargun, R.; Hazinedaroğlu, S.; Karayalçın, S.; Girgin, N. Successful living-related liver transplantation in a child with familial yellow nail syndrome and fulminant hepatic failure: Report of a case. Pediatr. Transplant. 2008, 12, 906–909. [Google Scholar] [CrossRef]
- Omari, A.K. Management of incarcerated inguinal hernia in a patient with yellow nail syndrome. Singap. Med. J. 2008, 49, 155–157. [Google Scholar]
- Cimini, C.; Giunta, R.; Utili, R.; Durante-Mangoni, E. Yellow nail syndrome as a cause of unexplained edema. Monaldi Arch. Chest Dis. 2009, 71, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Joshi, A.N.; Valliani, T.; Przemioslo, R. Unusual presentation of a man with recurrent chylous ascites. BMJ Case Rep. 2021, 14, e235273. [Google Scholar] [CrossRef] [PubMed]
- Baran, R. Pigmentations of the nails (chromonychia). J. Dermatol. Surg. Oncol. 1978, 4, 250–254. [Google Scholar] [CrossRef]
- Stosiek, N.; Peters, K.P.; Hiller, D.; Riedl, B.; Hornstein, O.P. Yellow nail syndrome in a patient with mycosis fungoides. J. Am. Acad. Dermatol. 1993, 28, 792–794. [Google Scholar] [CrossRef]
- Mishra, A.K.; George, A.A.; George, L. Yellow nail syndrome in rheumatoid arthritis: An aetiology beyond thiol drugs. Oxf. Med. Case Rep. 2016, 2016, 37–40. [Google Scholar] [CrossRef]
- Nordkild, P.; Kromann-Andersen, H.; Struve-Christensen, E. Yellow nail syndrome—The triad of yellow nails, lymphoedema, and pleural effusions. A review of the literature and a case report. Acta Med. Scand. 1986, 219, 221–227. [Google Scholar] [CrossRef]
- Valdés, L.; Huggins, J.T.; Gude, F.; Ferreiro, L.; Alvarez-Dobaño, J.M.; Golpe, A.; Toubes, M.E.; González-Barcala, F.J.; José, E.S.; Sahn, S.A. Characteristics of patients with yellow nail syndrome and pleural effusion. Respirology 2014, 19, 985–992. [Google Scholar] [CrossRef]
- Runyon, B.A.; Forker, E.L.; Sopko, J.A. Pleural-fluid kinetics in a patient with primary lymphedema, pleural effusions, and yellow nails. Am. Rev. Respir. Dis. 1979, 119, 821–825. [Google Scholar]
- Maldonado, F.; Ryu, J.H. Yellow nail syndrome. Curr. Opin. Pulm. Med. 2009, 15, 371–375. [Google Scholar] [CrossRef]
- Szuba, A.; Rockson, S.G. Lymphedema: Classification, diagnosis and therapy. Vasc. Med. 1998, 3, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Baran, R.; Thomas, L. Combination of fluconazole and alpha-tocopherol in the treatment of yellow nail syndrome. J. Drugs Dermatol. 2009, 8, 276–278. [Google Scholar] [PubMed]
- Imadojemu, S.; Rubin, A. Dramatic improvement of yellow nail syndrome with a combination of intralesional triamcinolone, fluconazole, and sinusitis management. Int. J. Dermatol. 2015, 54, e497–e499. [Google Scholar] [CrossRef]
- Hillerdal, G. Yellow nail syndrome: Treatment with octreotide. Clin. Respir. J. 2007, 1, 120–121. [Google Scholar] [CrossRef]
- Makrilakis, K.; Pavlatos, S.; Giannikopoulos, G.; Toubanakis, C.; Katsilambros, N. Successful octreotide treatment of chylous pleural effusion and lymphedema in the yellow nail syndrome. Ann. Intern. Med. 2004, 141, 246–247. [Google Scholar] [CrossRef] [PubMed]
- International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 consensus document of the International Society of Lymphology. Lymphology 2013, 46, 1–11. [Google Scholar]



| Laboratory Parameter | Reference Range | Patient’s Values | ||||
|---|---|---|---|---|---|---|
| D0 | D1 | D3 | D7 † | D45 ‡ | ||
| White cell count (× 109/L) | 4.0–10.0 | 7.04 | 5.92 | 8.67 | 6.40 | 7.04 |
| Hemoglobin (g/L) | 12.0–16.0 | 16.1 | 13.7 | 15.0 | 13.9 | 14.2 |
| Platelet count (× 109/L) | 150–400 | 367 | 333 | 361 | 253 | 313 |
| International normalized ratio (INR) | 0.8–1.2 | 1.15 | 1.09 | 1.16 | 1.13 | 1.10 |
| Albumin (g/dL) | 3.5–5.2 | 3.5 | 3.5 | 3.5 | 3.4 | 3.8 |
| Total Protein (g/dL) | 6.2–8.5 | 6.3 | 6.2 | 5.8 | 5.8 | 6.2 |
| Total Bilirubin (mg/dL) | 0.3–1.2 | 0.5 | 0.45 | 0.5 | 0.4 | 0.5 |
| Alanine aminotransferase (U/L) | 0–35 | 29 | 27 | 25 | 22 | 25 |
| Aspartate aminotransferase (U/L) | 0–40 | 38 | 31 | 35 | 48 | 40 |
| Alkaline phosphatase (U/L) | 30–120 | 66 | 57 | 66 | 48 | 51 |
| Lactate dehydrogenase (U/L) | 140–246 | 181 | 104 | 138 | 216 | 150 |
| Urea (mg/dL) | 15–45 | 56 | 52 | 49 | 66 | 71 |
| Creatinine (mg/dL) | 0.6–1.1 | 1.0 | 0.9 | 1.1 | 1.1 | 1.4 |
| Potassium (mmol/lt) | 3.5–5.1 | 3.8 | 3.4 | 3.8 | 4.1 | 4.1 |
| Natrium (mmol/lt) | 136–146 | 134 | 134 | 136 | 134 | 131 |
| C–reactive protein (mg/dL) | <0.5 | 1.45 | 1.02 | 1.05 | 0.66 | 0.5 |
| Urine, protein | - | - | ||||
| NT–pro BNP * (pg/mL) | <125 | 52.1 | ||||
| Ascitic Fluid Analysis | ||||||
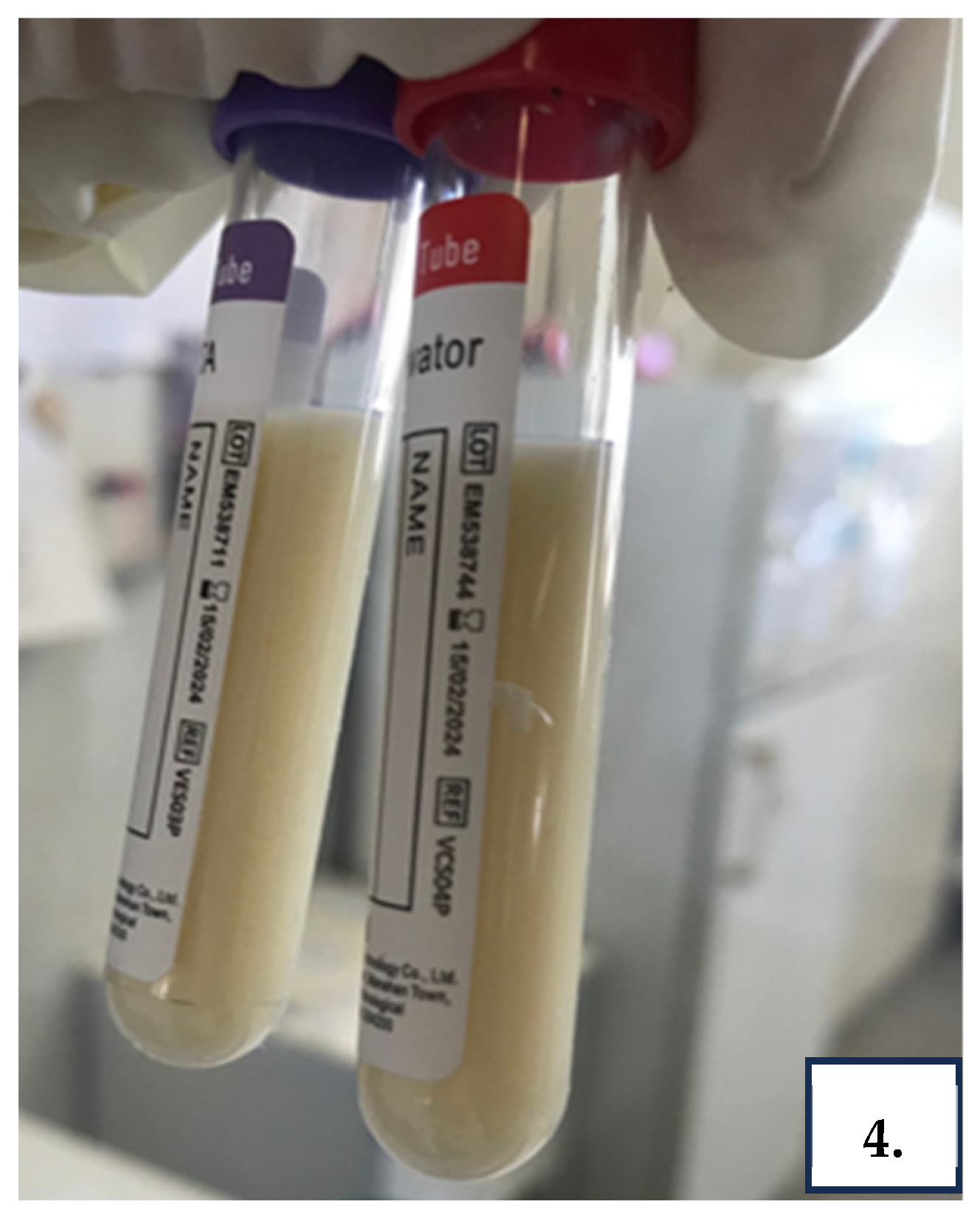
| Gross appearance | clear, light yellow | Cloudy, yellow | Cloudy, white | |||
| Total Protein (g/L) | <4.1 | 3.9 | 3.8 | |||
| Lactate dehydrogenase (U/L) | >Upper limit of serum reference interval | <50 | <50 | |||
| Triglyceride Level (mg/dL) | <200 | 5010 | 3050 | |||
| SAAG ** (g/dL) | </≥1.1 | 0.1 | 0.2 | |||
| Cell counts (cells/µL) | <500 | 574 | 1000 | |||
| Neutrophils, N (%) | <25 | 20 | 23 | |||
| Bacterial culture | Negative | Negative | Negative | |||
| M. Tuberculosis complex RT–PCR *** | Negative | Negative | ||||
| Cytology | Normal | Normal | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stamatiou, I.; Ntoga, M.; Karagiannis, C.; Valsamaki, P.N.; Papazoglou, D.; Rafailidis, P. A 74-Year-Old Man with Massive Ascites: A Case Report of Yellow Nail Syndrome. Reports 2025, 8, 219. https://doi.org/10.3390/reports8040219
Stamatiou I, Ntoga M, Karagiannis C, Valsamaki PN, Papazoglou D, Rafailidis P. A 74-Year-Old Man with Massive Ascites: A Case Report of Yellow Nail Syndrome. Reports. 2025; 8(4):219. https://doi.org/10.3390/reports8040219
Chicago/Turabian StyleStamatiou, Iliana, Melina Ntoga, Christos Karagiannis, Pipitsa N. Valsamaki, Dimitrios Papazoglou, and Petros Rafailidis. 2025. "A 74-Year-Old Man with Massive Ascites: A Case Report of Yellow Nail Syndrome" Reports 8, no. 4: 219. https://doi.org/10.3390/reports8040219
APA StyleStamatiou, I., Ntoga, M., Karagiannis, C., Valsamaki, P. N., Papazoglou, D., & Rafailidis, P. (2025). A 74-Year-Old Man with Massive Ascites: A Case Report of Yellow Nail Syndrome. Reports, 8(4), 219. https://doi.org/10.3390/reports8040219






