Approach to Hyperthyroidism
Abstract
1. Case Scenario
- (A)
- Initiate beta-blockade: Symptomatic management is crucial in hyperthyroidism.
- (B)
- Start antithyroid medication: Medications like methimazole or propylthiouracil inhibit thyroid hormone synthesis.
- (C)
- Consider radioactive iodine therapy: This treatment selectively destroys thyroid tissue, reducing hormone production, and is a common approach for definitive treatment of Graves’ disease, especially when medications are contraindicated or ineffective.
- (D)
- Perform thyroidectomy: Surgical removal of part, or all, of the thyroid gland is another definitive treatment option, particularly in cases of large goiters, patient preference, or contraindications to radioactive iodine therapy.
- (E)
- Refer to an endocrinologist: Specialist input is essential for comprehensive management and treatment planning.
2. Initial Approach
2.1. Overview of Hyperthyroidism
2.2. Symptoms and Clinical Presentation of Hyperthyroidism
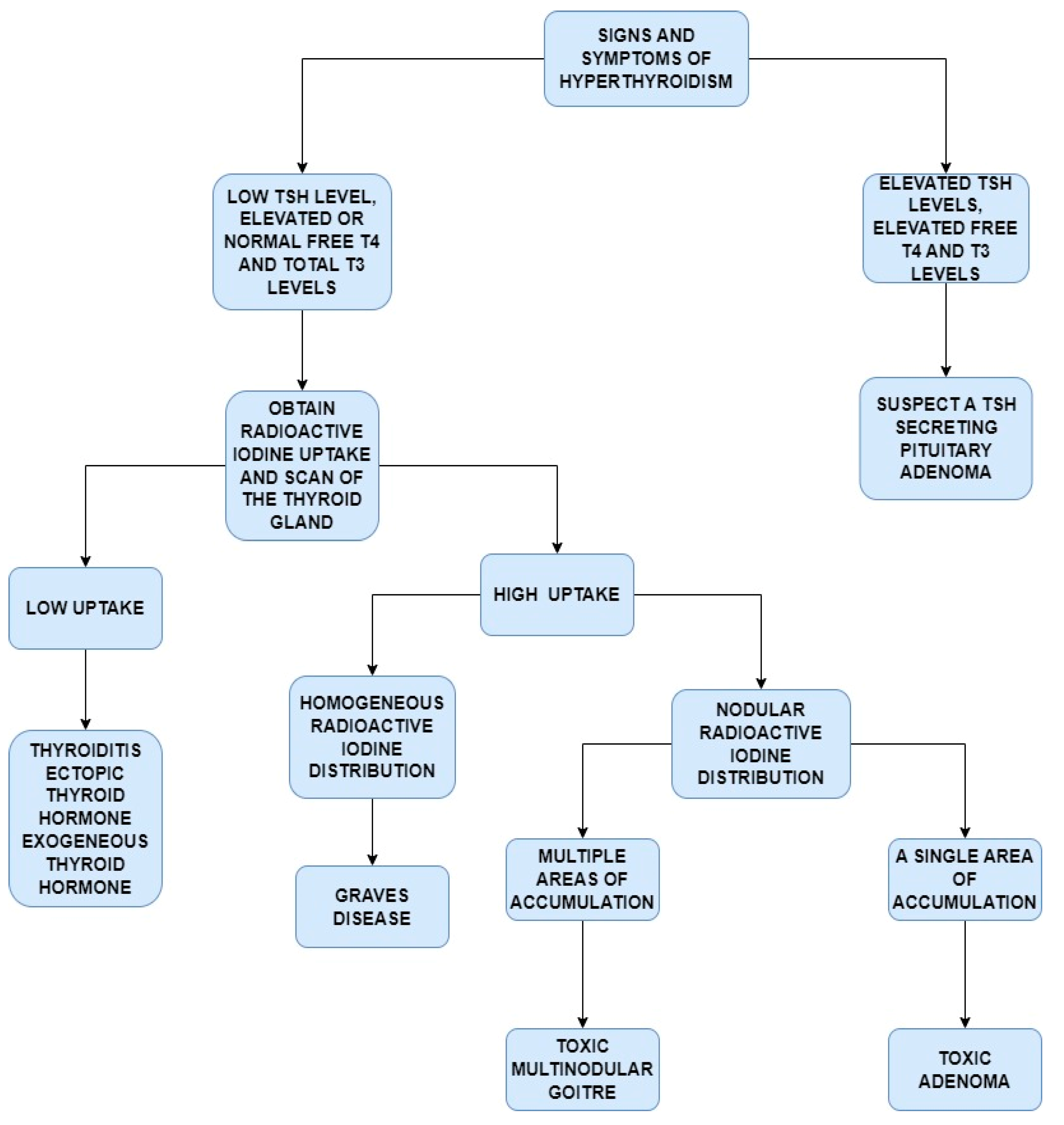
2.3. Laboratory Investigations and Diagnosis of Hyperthyroidism
2.4. Interpretation of TFTs in Hyperthyroidism
2.5. Significance of Thyroid Antibodies in Hyperthyroidism
3. Beyond the Initial Approach
Initial Management Steps
- Beta blockers: Beta-blockers are commonly used to alleviate the symptoms associated with hyperthyroidism. They work by blocking the effects of excess thyroid hormones on the body’s tissues, particularly the heart and nervous system. By antagonizing beta-adrenergic receptors, beta-blockers reduce the impact of adrenaline and other catecholamines, leading to a lower heart rate, reduced blood pressure, and relief from symptoms linked to increased sympathetic activity [17]. These medications effectively manage palpitations, tremors, and anxiety by normalizing the heart rate and counteracting the overstimulation caused by elevated thyroid hormones. Strategic use of beta-blockers significantly enhances the quality of life in individuals dealing with hyperthyroidism [18].
- Antithyroid medications: Medications such as methimazole or propylthiouracil are central to the management of hyperthyroidism as they inhibit thyroid hormone synthesis within the gland. The primary goal is to restore normal thyroid hormone levels, known as euthyroidism, thereby relieving hyperthyroid symptoms and preventing complications associated with excessive hormone production. These medications are often recommended as a first-line therapy, especially in cases of Graves’ disease, aiming to induce remission or prepare the patient for definitive treatments like radioactive iodine or surgery. By restoring the hormonal balance, antithyroid medications play a crucial role in managing hyperthyroidism and laying the groundwork for comprehensive treatment strategies [19].
- Radioactive iodine therapy: Radioactive iodine therapy (RAI) is a well-established treatment option for hyperthyroidism, particularly in conditions such as Graves’ disease, toxic multinodular goiter, and toxic adenoma. RAI works by delivering targeted radiation to the thyroid gland, effectively destroying overactive thyroid tissue. The thyroid absorbs radioactive iodine, which emits beta radiation that disrupts thyroid cells, thereby reducing hormone production [2].
- Thyroidectomy: Thyroidectomy, a surgical treatment for hyperthyroidism, involves the partial or complete removal of the thyroid gland. The extent of the surgery varies, with partial thyroidectomy (lobectomy) often used for solitary toxic nodules and total thyroidectomy for conditions such as Graves’ disease or toxic multinodular goiter. The indications for thyroidectomy include cases where radioactive iodine therapy is not viable or preferred, such as large goiters causing compression, suspected thyroid cancer, those who fail medical therapy, or when patients opt for surgery over other treatments. Thyroidectomy offers a tailored solution for complex cases of hyperthyroidism [20].
- Duration of medical treatment and transition to definitive therapy: The duration of antithyroid medication therapy typically ranges from 12 to 18 months. Remission rates vary, with predictors such as lower TRAb levels and smaller goiter sizes associated with a higher likelihood of success. Definitive treatments, including radioactive iodine therapy or thyroidectomy, are recommended in cases of relapse, intolerance of medications, or patient preference for permanent resolution [21].
- Recent advancements: The role of predictive markers such as TRAb levels in assessing the remission and relapse risk. Additionally, novel therapeutic approaches, including targeted molecular treatments, are emerging as potential alternatives to conventional therapies, particularly in patients with refractory disease. These innovations provide clinicians with tools to individualize treatment further and improve long-term outcomes [22].
- Patient-centered care: Incorporating patient values and preferences is a cornerstone of evidence-based medicine, particularly in chronic conditions such as hyperthyroidism. Patients’ individual circumstances, treatment goals, and concerns about potential side effects or long-term outcomes should guide the selection of management strategies. For example, while some patients may prioritize non-surgical options, others may prefer definitive treatments such as radioactive iodine or thyroidectomy based on their lifestyle, reproductive plans, or tolerance of medication [2]. A patient-centered approach ensures not only adherence to treatment but also improved satisfaction and quality of life.
- Updated controversies in hyperthyroidism management: Recent debates in hyperthyroidism management reflect the complexity of balancing treatment efficacy, safety, and patient-specific factors. For antithyroid drug (ATD) therapy, the optimal duration remains unclear, with guidelines suggesting a typical course of 12–18 months but with variable relapse rates. Radioactive iodine therapy (RAI) continues to raise questions, particularly in patients with large goiters or Graves’ ophthalmopathy, where concerns about worsening eye symptoms or inadequate responses exist. Partial thyroidectomy, though less common, has been revisited as a surgical option for Graves’ disease in select patients, offering the potential to retain partial thyroid function while minimizing long-term hypothyroidism. These controversies underscore the importance of personalized treatment decisions and shared decision-making with patients to optimize outcomes [21,23].
Author Contributions
Funding
Conflicts of Interest
Correction Statement
References
- Mathew, P.; Kaur, J.; Rawla, P. Hyperthyroidism. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://pubmed.ncbi.nlm.nih.gov/30725738/ (accessed on 1 September 2024).
- Doubleday, A.R.; Sippel, R.S. Hyperthyroidism. Gland Surg. 2020, 9, 124–135. [Google Scholar] [CrossRef] [PubMed]
- De Leo, S.; Lee, S.Y.; Braverman, L.E. Hyperthyroidism. Lancet 2016, 388, 906–918. [Google Scholar] [CrossRef] [PubMed]
- McDermott, M.T. Hyperthyroidism. Ann. Intern. Med. 2020, 172, ITC49. [Google Scholar] [CrossRef] [PubMed]
- Maji, D. Hyperthyroidism. J. Indian Med. Assoc. 2006, 104, 563–564, 566–567. [Google Scholar]
- Rashid, M.; Rashid, M.H. Obstetric management of thyroid disease. Obstet. Gynecol. Surv. 2007, 62, 680–688. [Google Scholar] [CrossRef]
- Grebe, S.K.G.; Kahaly, G.J. Laboratory testing in hyperthyroidism. Am. J. Med. 2012, 125, S2. [Google Scholar] [CrossRef]
- D’aurizio, F. The role of laboratory medicine in the diagnosis of the hyperthyroidism. Q. J. Nucl. Med. Mol. Imaging 2021, 65, 91–101. [Google Scholar] [CrossRef]
- Arens, A.M.; Birmingham, M.; McHale, E.; Siegel-Richman, Y.; Driver, B.E. The utility of laboratory testing for suspected hyperthyroidism in the emergency department. Am. J. Emerg. Med. 2022, 54, 76–80. [Google Scholar] [CrossRef]
- Meng, W. Diagnosis of hyperthyroidism. Z. Arztl. Fortbild. Qualitatssich. 2001, 95, 51–60. [Google Scholar]
- Reid, J.R.; Wheeler, S.F. Hyperthyroidism: Diagnosis and treatment. Am. Fam. Physician 2005, 72, 623–630. [Google Scholar]
- Kravets, I. Hyperthyroidism: Diagnosis and treatment. Am. Fam. Physician 2016, 93, 363–370. [Google Scholar] [PubMed]
- Trainer, T.D.; Howard, P.L.; Rock, R.C. Thyroid function tests in thyroid and nonthyroid disease. CRC Crit. Rev. Clin. Lab. Sci. 1983, 19, 135–171. [Google Scholar] [CrossRef] [PubMed]
- Economidou, F.; Douka, E.; Tzanela, M.; Nanas, S.; Kotanidou, A. Thyroid function during critical illness. Hormones 2011, 10, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Khanna, C.M.; Shanker, R.; Magdum, M.; Jain, S.K.; Jaggi, C.B. Prognostic significance of thyroid antibodies in hyperthyroid patients treated with antithyroid drugs. J. Assoc. Physicians India 1998, 46, 176–178. [Google Scholar] [PubMed]
- Vargas-Uricoechea, H.; Nogueira, J.P.; Pinzón-Fernández, M.V.; Schwarzstein, D. The usefulness of thyroid antibodies in the diagnostic approach to autoimmune thyroid disease. Antibodies 2023, 12, 48. [Google Scholar] [CrossRef]
- Feely, J.; Peden, N. Use of β-adrenoceptor blocking drugs in hyperthyroidism. Drugs 1984, 27, 425–446. [Google Scholar] [CrossRef]
- Geffner, D.L.; Hershman, J.M. β-Adrenergic blockade for the treatment of hyperthyroidism. Am. J. Med. 1992, 93, 61–68. [Google Scholar] [CrossRef]
- Hughes, K.; Eastman, C. Thyroid disease: Long-term management of hyperthyroidism and hypothyroidism. Aust. J. Gen. Pract. 2021, 50, 36–42. [Google Scholar] [CrossRef]
- Barczyński, M. Current approach to surgical management of hyperthyroidism. Q. J. Nucl. Med. Mol. Imaging 2021, 65, 124–131. [Google Scholar] [CrossRef]
- Bahn Chair, R.S.; Burch, H.B.; Cooper, D.S.; Garber, J.R.; Greenlee, M.C.; Klein, I.; Laurberg, P.; McDougall, I.R.; Montori, V.M.; Rivkees, S.A.; et al. Hyperthyroidism and other causes of thyrotoxicosis: Management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. Off. J. Am. Thyroid. Assoc. 2011, 21, 593–646. [Google Scholar] [CrossRef]
- Karapanou, O.; Simeakis, G.; Vlassopoulou, B.; Alevizaki, M.; Saltiki, K. Advanced RAI-refractory thyroid cancer: An update on treatment perspectives. Endocr-Relat. Cancer 2022, 29, R57–R66. [Google Scholar] [CrossRef] [PubMed]
- Ross, D.S.; Burch, H.B.; Cooper, D.S.; Greenlee, M.C.; Laurberg, P.; Maia, A.L.; Rivkees, S.A.; Samuels, M.; Sosa, J.A.; Stan, M.N.; et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid. Off. J. Am. Thyroid. Assoc. 2016, 26, 1343–1421. [Google Scholar] [CrossRef] [PubMed]
| Symptoms | Clinical Presentation |
|---|---|
| Weight loss | Unintentional weight loss despite regular or increasing appetite |
| Palpitations | Sensation of rapid or irregular heartbeat |
| Heat intolerance | Inability to tolerate heat, often accompanied by excessive sweating |
| Tremors | Fine tremors, especially noticeable in the hands |
| Anxiety and irritability | Feelings of nervousness, anxiety, and irritability |
| Fatigue | Chronic tiredness and lack of energy |
| Increased bowel movements | Frequent or loose stools |
| Muscle weakness | Generalized muscle weakness or easy fatigability |
| Menstrual changes | Irregular or lighter menstrual periods |
| Goiter | Palpable anterior neck mass at the level of the thyroid gland |
| Management Option | Description | Potential Complications |
|---|---|---|
| Beta-Blockers | Medications that alleviate symptoms (e.g., palpitations, tremors, anxiety) by blocking the effects of thyroid hormones on tissues. | Bradycardia, fatigue, cold extremities |
| Antithyroid Medications | Methimazole or propylthiouracil inhibit thyroid hormone synthesis, aiming to achieve normal hormone levels. | Agranulocytosis, hepatotoxicity, rash |
| Radioactive Iodine Therapy | Delivers targeted radiation to the thyroid gland to destroy overactive tissue, commonly used in Graves’ disease cases. | Hypothyroidism, transient thyroiditis |
| Thyroidectomy | Surgical removal of part, or all, of the thyroid gland, indicated when other therapies are unsuitable or based on patient preference. | Hypocalcaemia, recurrent laryngeal nerve injury, hypothyroidism |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chowdhury, R.; Turkdogan, S.; Silver, J.A.; Hier, J.; Bursey, S.; Quttaineh, D.; Khoury, M.; Himdi, L. Approach to Hyperthyroidism. J. Otorhinolaryngol. Hear. Balance Med. 2024, 5, 20. https://doi.org/10.3390/ohbm5020020
Chowdhury R, Turkdogan S, Silver JA, Hier J, Bursey S, Quttaineh D, Khoury M, Himdi L. Approach to Hyperthyroidism. Journal of Otorhinolaryngology, Hearing and Balance Medicine. 2024; 5(2):20. https://doi.org/10.3390/ohbm5020020
Chicago/Turabian StyleChowdhury, Raisa, Sena Turkdogan, Jennifer A. Silver, Jessica Hier, Stuart Bursey, Danah Quttaineh, Mark Khoury, and Lamiae Himdi. 2024. "Approach to Hyperthyroidism" Journal of Otorhinolaryngology, Hearing and Balance Medicine 5, no. 2: 20. https://doi.org/10.3390/ohbm5020020
APA StyleChowdhury, R., Turkdogan, S., Silver, J. A., Hier, J., Bursey, S., Quttaineh, D., Khoury, M., & Himdi, L. (2024). Approach to Hyperthyroidism. Journal of Otorhinolaryngology, Hearing and Balance Medicine, 5(2), 20. https://doi.org/10.3390/ohbm5020020







