Abstract
Objective: The primary objective of this research is to conduct a systematic review of the available studies and evidence to determine if there is a significant relationship between otosclerosis and psychiatric disorders. By critically evaluating the existing data, this study aims to provide insights into the potential interplay between these medical conditions. Data Sources: PubMed, Embase, Ebsco, Proquest, and Web of Science Review Methods: PubMed, Embase, Ebsco, Proquest, and Web of Science databases were queried for original English articles from 1950 to 2023. This review was conducted in accordance with the 2020 PRISMA guidelines. The publications were screened by two independent viewers. The Newcastle–Ottawa Scale quality instrument was used to assess the quality of studies. Results: Initially, 153 abstracts were screened for eligibility. After a rigorous selection process, five studies met the criteria, collectively encompassing 262 patients diagnosed with otosclerosis. The reported mean ages ranged from 25 to 52 years. A combined assessment of psychiatric disorder rates among otosclerosis patients revealed a rate of 36%. Depression, anxiety, and schizophrenia were the most common mental illnesses reported in all six studies. One of the studies specifically examined psychiatric disorder rates before and after stapedectomy, revealing a statistically significant decrease in depressive and anxiety-related symptoms following the surgical intervention. Conclusions: This systematic review emphasizes the emerging evidence connecting otosclerosis with psychiatric disorders and underscores the importance of adopting a multidisciplinary approach to assess and manage otosclerosis patients.
1. Introduction
Otosclerosis (oto, meaning “of the ear”, and sclerosis, referring to “abnormal hardening of body tissue”), also known as otospongiosis, is a condition unique to humans. It is characterized by abnormal bone remodeling in the middle ear. This condition involves the replacement of the normal dense endochondral layer of the bony otic capsule in the labyrinth with irregular spongy bone, which ultimately leads to the fixation of the stapes [1,2,3]. Otosclerosis typically manifests as an early adult-onset disease, with women being affected more frequently than men, in a ratio of 2:1 [4,5]. Onset commonly occurs in the twenties and thirties, though hearing loss typically does not manifest until after the fourth decade.
The prevalence of otosclerosis is highest in Caucasians, with clinical cases occurring in 0.04% to 1% and histologic cases occurring in as much as 10% of the White population [4,5,6]. The condition is much less common in the Black, Asian, and Native American populations [5]. In the Black population, the prevalence of histological otosclerosis is around 1%, while among Asians, it is approximately 5% [5,6].
The exact etiology of otosclerosis is still unclear. Studies have postulated a number of possible anatomical, genetic, and hereditary etiologies, as well as links to sex, ethnicity, age, pregnancy, and viral infections [7]. The primary presentation in patients with clinical otosclerosis is often hearing loss, accompanied by potential occurrences of tinnitus and vertigo. A thorough patient history is crucial. Typically, patients with otosclerosis present with bilateral hearing loss that gradually worsens over several years. The condition may initially affect only one ear but eventually progress to also involve the contralateral ear [7].
Medical treatment primarily aims to halt or slow the progression of the disease [8,9]. The preferred treatment for otosclerosis is stapedotomy or stapedectomy. Surgical intervention for otosclerosis has demonstrated favorable outcomes, regardless of the specific procedure. More than 90% of patients typically experience a significant improvement in their hearing ability following surgery [8]. However, there is currently no effective cure for the condition.
Tinnitus is a significant and concerning side effect of otosclerosis. Studies indicate that individuals experiencing tinnitus may encounter disruptions in their emotional well-being [10,11]. Individuals with particularly bothersome tinnitus frequently report heightened negative emotions and experience suicidal ideation and attempts at a significantly higher rate than individuals without tinnitus [10]. Emotional changes experienced by individuals with tinnitus may include dissatisfaction with life, difficulties achieving relaxation, anxiety, tension, or stress, all of which have a significant impact on their quality of life [8,9].
The prevalence of psychiatric disorders among individuals with hearing loss is a significant concern, given that hearing impairment is one of the most prevalent conditions experienced by adults, particularly as they age. Studies have consistently shown that the occurrence of psychiatric disorders is higher among those with hearing loss compared to the general population. Specifically, conditions such as schizophrenia, anxiety, and depression are notably associated with hearing impairment [12,13]. For instance, research indicates that the prevalence of depression is more than twice as high in individuals with hearing loss (3.8%) compared to controls (1.8%) [14]. To the best of our knowledge, there is currently no review focused specifically on the prevalence of psychiatric outcomes in patients with hearing loss conditions like otosclerosis. This review aims to fill this gap by examining the existing literature to understand the psychological impact of otosclerosis on affected individuals.
Considering the progressive nature of acquired hearing loss and its potential impact on an individual’s communication and daily interactions, the primary goal of this review is to elucidate the prevalence of psychiatric disorders in patients with otosclerosis and to explore the connection between otosclerosis and psychiatric disorders. As a secondary outcome, it will examine the extent, nature, and potential contributing mechanisms of this association, as well as the effect of otosclerosis treatment in improving psychiatric symptoms. The findings from this investigation will have significant implications for the management and treatment of otosclerosis patients because it underscores the importance of a comprehensive approach that addresses both the auditory and psychological aspects of the condition.
2. Materials and Methods
2.1. Data Sources and Search Strategies
A comprehensive search of Pubmed, Web of Science, ProQuest Central, and Ebsco, starting from each database’s inception until 2023, was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15]. The search strategy was designed and conducted by an experienced librarian. A combination of Medical Subject Headings (MeSH), other controlled vocabulary, and keywords were used to search for “hearing loss”, “mental disorders”, “psychiatric disorders”, and “otosclerosis”. An example of the comprehensive search strategy used to query the databases is described in Supplementary Item S1.
2.2. Study Selection and Eligibility Criteria
Only studies published in English or those available in full-length international journals with English translations were selected for further analysis. Additionally, references from publications underwent review to identify potential inclusion criteria. Eligible studies met the following criteria: (1) the inclusion of participants diagnosed with otosclerosis suffering from psychiatric disorder due to otosclerosis; (2) an investigation of the prevalence of psychiatric disorders in otosclerosis patients; (3) the absence of restrictions on the geographical location or setting of the study. Abstracts, conference abstracts, and articles not reported in English were excluded from the study. Moreover, studies lacking sufficient data on psychiatric disorders or failing to report their findings were excluded. Abstracts were reviewed independently by two reviewers (A.P., S.F.). Full-text articles underwent further screening to determine eligibility for inclusion. A PRISMA flow diagram of this process is presented in Figure 1.
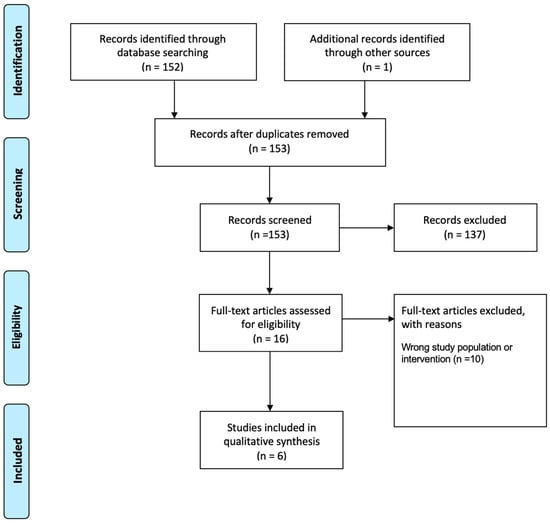
Figure 1.
Preferred Reporting Items for systematic reviews.
2.3. Data Collection and Data Items
The data extracted from each study included (1) the study characteristics, (2) patient characteristics, and (3) the treatments received and the outcome on the patient’s overall health, as shown in Table 1. Study characteristics included the study design, number of patients, average or median reported age, and gender distribution.

Table 1.
Baseline characteristics of included studies.
2.4. Risk of Bias in Individual Studies
The quality of each study was independently evaluated by two authors (SF and AP) using either the Newcastle–Ottawa Scale for case control and cohort studies or the Joanna Briggs Institute Critical Appraisal Tool for case reports [22,23]. Selected studies were examined for their inclusion criteria, sample size, description of study participants, and setting. Two reviewers (SF, NA) independently assessed the methodological quality of each paper. The results of the quality assessment of all included studies are shown in Supplementary Item S2.
3. Results
3.1. Study Characteristics
Of 153 articles initially reviewed by title and/or abstract, we identified 16 for full-text screening, and 6 were included in the study. Among the included studies, three were retrospective cohort studies, and three were case reports [16,19,21] (see Table 1). A total of 262 participants were included in the selected studies. The age of patients included in the study ranged from 25 to 55.
3.2. Risk of Bias within Studies
The average Newcastle–Ottawa Scale (NOS) score for the three included case control studies was 6.7. Two studies were rated 7, indicating good quality. The third study, which the authors felt lacked in follow-up time, was rated a 6, indicating fair quality.
The average Joanna Briggs Critical Appraisal tool score for the three included case reports was 5.7 out of 8. One of the studies scored a 7 out of 8, lacking only in a description of adverse events. One study scored a 6 out of 8, lacking in a description of adverse events and key takeaway points. The third study scored a 4 out of 8 because it did not include an intervention, post-intervention description, adverse outcomes, or key takeaways.
3.3. Clinical Presentation
Across the six studies, an average of 36% of the included otosclerosis patients reported having psychiatric symptoms [16,17,18,19,20,21]. Conversely, the rate of psychiatric disorders in the control groups or in the post-operative status was much lower, at 16%. Across all six studies, depression and anxiety were consistently identified as the most commonly reported mental illnesses [16,17,18,19,20,21].
The retrospective case control by Leposavić et al. reported that the most observed disorders in the preoperative psychiatric assessment were depression (12 cases), anxiety-depressive disorder (10 cases), anxiety (6 cases), hypochondria (4 cases), and conversion disorder (4 cases). Furthermore, they found that patients with hearing impairment caused by otosclerosis had a significantly higher prevalence of psychiatric disorders than the general population. Specifically, rates were reported to be as high as 36 out of 60, as compared to a postoperative psychiatric assessment of 18 out of 60 [20]. The study also emphasized the significance of adaptation style and communication strategies in managing these psychiatric conditions [20].
Mahapatra et al. reported, in their case-control study, that out of 49 patients diagnosed with osteosclerotic deafness, 23 were also diagnosed with psychiatric illnesses. There were 17 with depression, 5 with paranoid schizophrenia, and 1 with anxiety. This incidence was significantly higher than the reported rate in the control group, where 6 out of 40 patients were diagnosed with psychiatric illnesses (p < 0.005) [17]. Similarly, Pizzichetta et al. reported almost twice the rate of depression, 26% vs. 13.3%, in patients with otosclerosis compared to their control counterparts [18].
Three case reports documented patients experiencing auditory hallucinations attributed to otosclerosis. One patient described these hallucinations as the constant repetition of religious hymns. Sometimes, a single melody would persist for half a day before being replaced by another, often comprising old songs from early childhood [16]. In contrast, the second case reported hearing voices of three people urging him to perform actions such as “kill yourself” or “do not touch your wife”, which all resolved after surgical treatment of the patient [19]. The third case report involved a 47-year-old patient who had been suffering from persecutory delusions, withdrawals, as well as severe auditory hallucinations for 15 years. The patient had received a hearing aid with insufficient improvement in his hearing. He underwent direct acoustic cochlear stimulation implant surgery. Immediately after the surgery, his hearing improved, and within two months, the persecutory delusions and withdrawals disappeared. Three years post-implantation surgery, the patient remained free from any psychiatric symptoms [21]. None of the studies could identify an organic cause for the hallucinations.
4. Discussion
The relationship between otosclerosis and psychiatric disorders is a complex issue that requires careful consideration. Otosclerosis can deeply affect individuals’ psychosocial well-being, leading to the onset or worsening of psychiatric disorders [16,17,18,19,20,21]. Hearing loss, such as that resulting from otosclerosis, often leads to social isolation, communication obstacles, and diminished engagement in social interactions. These challenges can serve as catalysts for the emergence of psychiatric disorders, notably depression and anxiety. Moreover, individuals with hearing difficulties may struggle to engage fully in cultural activities and pursue certain professions, affecting their self-esteem, mood, and social connections. This can lead to withdrawal from social life and feelings of helplessness and shame. Additionally, disability may result in patients facing stereotypes and marginalization, which can impact both their personal and professional life [24].
In our review, depression and anxiety consistently emerged as prevalent mental health conditions among individuals with otosclerosis, with a psychiatric disorder prevalence frequency of 36%. This is more than twice that of control groups or post-operative patients, at a rate of 16%.
Both environmental and genetic factors have been implicated in the disease process of otosclerosis; however, its pathogenesis remains poorly understood. To date, several loci have been mapped that indicate an autosomal dominant inheritance with variable penetrance, although no disease-causing mutations have been identified [4,25]. The genetic aspect of otosclerosis could potentially be related to the prevalence of psychiatric disorders in patients with the condition. Indeed, the genetic factors that predispose individuals to otosclerosis might be linked with those implicated in certain psychiatric conditions. However, our current understanding of these genetic correlations is limited, and additional genetic studies are necessary to explore this potential link further.
Tinnitus commonly accompanies otosclerosis, sometimes occurring alongside hearing loss or manifesting several years before it [26]. Together, tinnitus and hearing loss affect approximately 60% of all otosclerosis patients [27]. McKenna et al. discovered that 45% of patients suffering from tinnitus sought psychological assistance. Additionally, they found that 42% of individuals with otoneurological conditions, including tinnitus, hearing impairment (27%), and dizziness (64%), required psychological support [28]. A study by Sullivan et al. demonstrated a prevalence of depression of 7% among healthy individuals versus a striking 60% among those with tinnitus, validating the significant impact of tinnitus on the development of depression [29].
The treatment of otosclerosis, especially surgical intervention, has demonstrated efficacy in improving hearing outcomes. Leposavić et al. reported that an enhancement in hearing can positively impact an individual’s quality of life and potentially alleviate some of the psychiatric symptoms associated with hearing loss [20]. These findings underscore the significance of treatment for patients with otosclerosis and perhaps implicate hearing loss as a primary factor in mental health decline in otosclerosis. A 2014 study by Gevonden et al. demonstrated a hypersensitive dopaminergic system in patients with severe hearing impairment compared with healthy controls, which possibly helps to explain the post-operative resolution of hallucinatory symptoms in the case reports we included [30]. However, the direct influence of surgical treatment for otosclerosis on psychiatric disorders is not thoroughly documented. Furthermore, more research should be conducted to explore otosclerosis-specific factors beyond hearing loss that may contribute to the increased prevalence of psychiatric conditions.
One limitation of the current research is the scarcity of studies specifically investigating the link between otosclerosis and psychiatric disorders. Many studies concentrate on hearing loss in general, without distinguishing the underlying causes. Future research should prioritize longitudinal studies that can shed light on the temporal relationship between otosclerosis and the onset of psychiatric disorders. Additionally, there is a need for research into the effectiveness of various treatment modalities, such as hearing aids, cochlear implants, and stapes surgery, on psychiatric outcomes.
5. Conclusions
This review unveils a growing body of evidence that indicates an increased prevalence of psychiatric disorders, particularly anxiety and depression, among individuals diagnosed with otosclerosis. Furthermore, based on the findings of the included studies, the treatment of otosclerosis was reported to either completely resolve or improve the psychiatric symptoms. Through this systematic review, we emphasize the emerging evidence linking otosclerosis with psychiatric disorders and stress the importance of adopting a multidisciplinary approach in evaluating and treating otosclerosis patients.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ohbm5010007/s1, Supplementary Item S1: Database Search Strategy used for Systematic Review of Examining the Connection Between Otosclerosis and Psychiatric Disorders, Supplementary Item S2: Newcastle-Ottawa Quality Assessment Scale for included studies.
Author Contributions
S.F. and A.N.P., contributed to the data collection, data analysis, and writing and reviewing the final manuscript. E.G. and S.P., contributed to writing and reviewing the final manuscript. D.K., J.D. and R.S., contributed to the conception, data collection, data analysis, and writing and reviewing the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
This systematic review does not require ethical approval.
Data Availability Statement
With the publication, the data set used for this Systematic Review will be shared upon request from the study authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Quesnel, A.M.; Ishai, R.; McKenna, M.J. Otosclerosis: Temporal Bone Pathology. Otolaryngol. Clin. N. Am. 2018, 51, 291–303. [Google Scholar] [CrossRef]
- Babcock, T.A.; Liu, X.Z. Otosclerosis: From Genetics to Molecular Biology. Otolaryngol. Clin. N. Am. 2018, 51, 305–318. [Google Scholar] [CrossRef]
- Rudic, M.; Keogh, I.; Wagner, R.; Wilkinson, E.; Kiros, N.; Ferrary, E.; Sterkers, O.; Grayeli, A.B.; Zarkovic, K.; Zarkovic, N. The pathophysiology of otosclerosis: Review of current research. Hear. Res. 2015, 330, 51–56. [Google Scholar] [CrossRef]
- Crompton, M.; Cadge, B.A.; Ziff, J.L.; Mowat, A.J.; Nash, R.; Lavy, J.A.; Powell, H.R.F.; Aldren, C.P.; Saeed, S.R.; Dawson, S.J. The Epidemiology of Otosclerosis in a British Cohort. Otol. Neurotol. 2019, 40, 22–30. [Google Scholar] [CrossRef]
- Declau, F.; Van Spaendonck, M.; Timmermans, J.P.; Michaels, L.; Liang, J.; Qiu, J.P.; Van de Heyning, P. Prevalence of histologic otosclerosis: An unbiased temporal bone study in Caucasians. Adv. Otorhinolaryngol. 2007, 65, 6–16. [Google Scholar] [CrossRef]
- Markou, K.; Goudakos, J. An overview of the etiology of otosclerosis. Eur. Arch. Otorhinolaryngol. 2009, 266, 25–35. [Google Scholar] [CrossRef]
- Zafar, N.; Hohman, M.H.; Khan, M.A.B. Otosclerosis; StatPearls Publishing: Treasure Island, FL, USA, 2024; NBK560671. [Google Scholar]
- Uppal, S.; Bajaj, Y.; Coatesworth, A.P. Otosclerosis 2: The medical management of otosclerosis. Int. J. Clin. Pract. 2010, 64, 256–265. [Google Scholar] [CrossRef]
- Hentschel, M.A.; Huizinga, P.; van der Velden, D.L.; Wegner, I.; Bittermann, A.J.N.; van der Heijden, G.J.M.; Grolman, W. Limited evidence for the effect of sodium fluoride on deterioration of hearing loss in patients with otosclerosis: A systematic review of the literature. Otol. Neurotol. 2014, 35, 1052–1057. [Google Scholar] [CrossRef]
- Seo, J.H.; Kang, J.M.; Hwang, S.H.; Han, K.D.; Joo, Y.H. Relationship between tinnitus and suicidal behaviour in Korean men and women: A cross-sectional study. Clin. Otolaryngol. 2016, 41, 222–227. [Google Scholar] [CrossRef]
- Hu, J.; Xu, J.; Streelman, M.; Xu, H.; Guthrie, O. The Correlation of the Tinnitus Handicap Inventory with Depression and Anxiety in Veterans with Tinnitus. Int. J. Otolaryngol. 2015, 2015, 689375. [Google Scholar] [CrossRef]
- Saperstein, A.M.; Meyler, S.; Medalia, A. Hearing Loss Among People With Schizophrenia: Implications for Clinical Practice. Psychiatr. Serv. 2023, 74, 543–546. [Google Scholar] [CrossRef]
- Bigelow, R.T.; Reed, N.S.; Brewster, K.K.; Huang, A.; Rebok, G.; Rutherford, B.R.; Lin, F.R. Association of Hearing Loss With Psychological Distress and Utilization of Mental Health Services Among Adults in the United States. JAMA Netw. Open 2020, 3, e2010986. [Google Scholar] [CrossRef]
- Zhou, T.; Wang, J.; Zhang, C.; Zhang, B.; Guo, H.; Yang, B.; Li, Q.; Ge, J.; Li, Y.; Niu, G.; et al. Tracheostomy decannulation protocol in patients with prolonged tracheostomy referred to a rehabilitation hospital: A prospective cohort study. J. Intensive Care. 2022, 10, 34. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Rozanski, J.; Rosen, H. Musical hallucinosis in otosclerosis. Confin. Neurol. 1952, 12, 49–54. [Google Scholar] [CrossRef]
- Mahapatra, S.B. Deafness and mental health: Psychiatric and psychosomatic illness in the deaf. Acta Psychiatr. Scand. 1974, 50, 596–611. [Google Scholar] [CrossRef]
- Pizzichetta, V.; Ferraro, G. The psychic personality in otosclerotic subjects. An. Otorrinolaringol. Ibero Am. 1978, 5, 619–625. [Google Scholar]
- Marneros, A.; Beyenburg, S.; Berghaus, A. Unilateral hallucinations and other psychotic symptoms due to otosclerosis. Psychopathology 1997, 30, 89–92. [Google Scholar] [CrossRef]
- Leposavić, L.; Leposavić, I.; Jasović-Gasić, M.; Milovanović, S.; Nikolić-Balkoski, G. Psychosocial aspects of acquired hearing impairment in the patients with otosclerosis. Psychiatr. Danub. 2006, 18, 30–38. [Google Scholar]
- Rebol, J.; Kravos, M.; Ložar, M. Successful hearing improvement with direct acoustic stimulation in a patient with schizophrenia. J. Laryngol. Otol. 2018, 132, 946–948. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int. J. Evid. Based Healthc. 2015, 13, 163–169. [Google Scholar] [CrossRef]
- Kuchar, I.; Kościelska, O.; Kędziora-Kornatowska, K. Impact of otosclerosis symptoms on patients quality of life before and after surgery—A literature review. J. Educ. Health Sport 2020, 10, 419–427. [Google Scholar] [CrossRef]
- Ealy, M.; Smith, R.J. The genetics of otosclerosis. Hear. Res. 2010, 266, 70–74. [Google Scholar] [CrossRef]
- T G. Chirurgicznego Otosklerozy—Seria. Edited by L K-G. Przypadków. Otolaryngologia 2007. Available online: https://katalogi.bn.org.pl/discovery/fulldisplay/alma9910300518005606/48OMNIS_NLOP:48OMNIS_NLOP (accessed on 24 April 2024).
- Dżaman, K.; Pleskacz, W.A.; Wałkanis, A.; Rapiejko, P.; Jurkiewicz, D. Ocena zmysłu smaku i węchu u pacjentów z polipami nosa. Otolaryngol. Polska. 2007, 61, 831–837. [Google Scholar] [CrossRef]
- McKenna, L.; Hallam, R.S.; Hinchcliffe, R. The prevalence of psychological disturbance in neurotology outpatients. Clin. Otolaryngol. Allied Sci. 1991, 16, 452–456. [Google Scholar] [CrossRef]
- Sullivan, M.D.; Katon, W.; Dobie, R.; Sakai, C.; Russo, J.; Harrop-Griffiths, J. Disabling tinnitus. Association with affective disorder. Gen. Hosp. Psychiatry 1988, 10, 285–291. [Google Scholar] [CrossRef]
- Gevonden, M.; Booij, J.; van den Brink, W.; Heijtel, D.; van Os, J.; Selten, J.P. Increased release of dopamine in the striata of young adults with hearing impairment and its relevance for the social defeat hypothesis of schizophrenia. JAMA Psychiatry 2014, 71, 1364–1372. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).