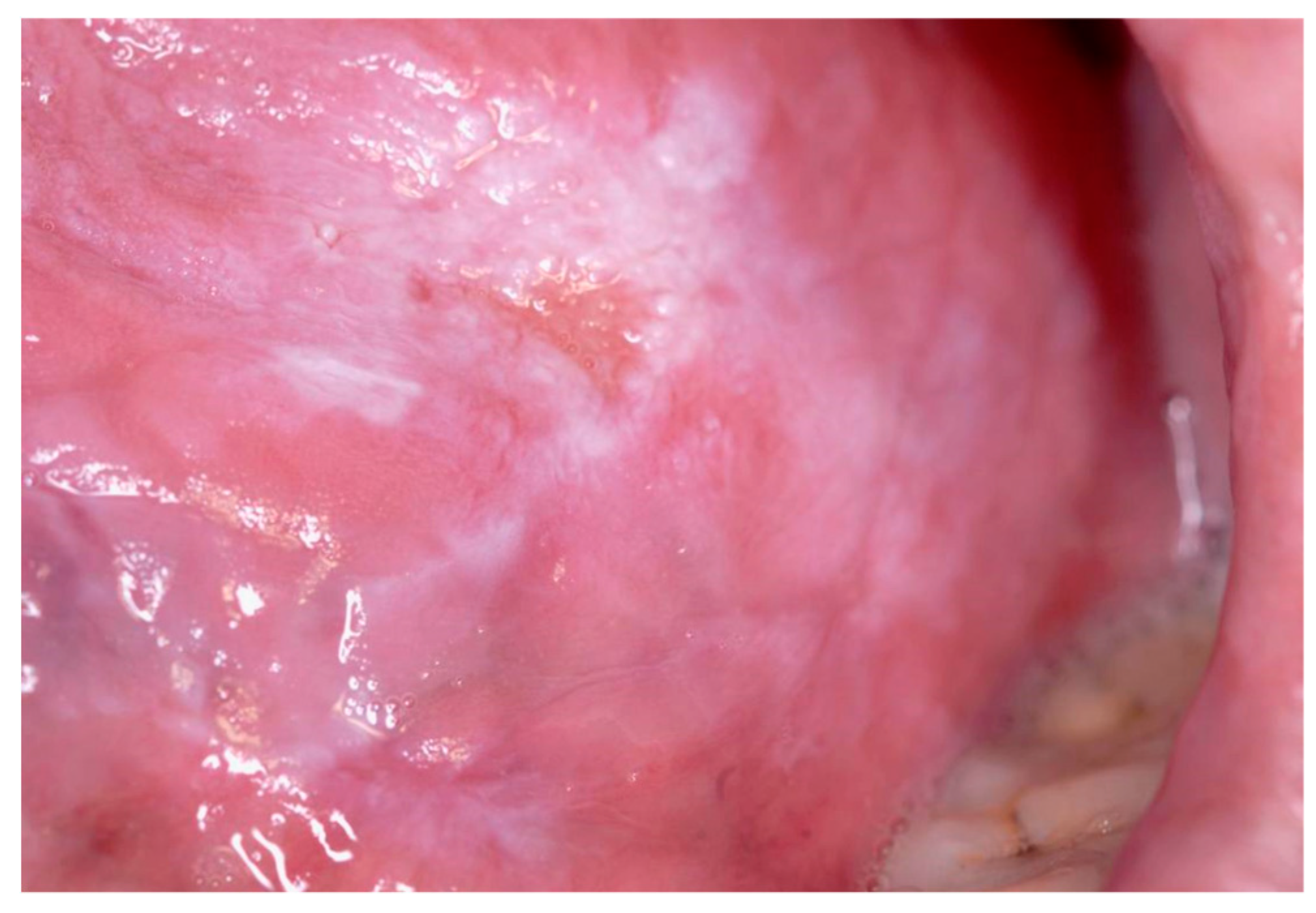
Oral leukoplakia. A More Challenging Disorder than It Seems †
Conflicts of Interest
References
- Holmstrup, P.; Dabelsteen, E. Oral leukoplakia—To treat or not to treat. Oral Dis. 2016, 22, 494–497. [Google Scholar] [CrossRef] [PubMed]
- Van der Waal, I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol. 2009, 45, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Speight, P.M.; Khurram, S.A.; Kujan, O. Oral potentially malignant disorders: Risk of progression to malignancy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, 612–627. [Google Scholar] [CrossRef] [PubMed]
- Brouns, E.R.A.; Baart, J.A.; Bloemena, E.; Karagozoglu, H.; Van der Waal, I. The relevance of uniform reporting in oral leukoplakia: Definition, certainty factor and staging based on experience with 275 patients. Med. Oral Patol. Oral y Cir. Bucal 2013, 18, e19. [Google Scholar] [CrossRef] [PubMed]
- Kuribayashi, Y.; Tsushima, F.; Morita, K.I.; Matsumoto, K.; Sakurai, J.; Uesugi, A.; Sato, K.; Oda, S.; Sakamoto, K.; Harada, H. Long-term outcome of non-surgical treatment in patients with oral leukoplakia. Oral Oncol. 2015, 51, 1020–1025. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tovaru, S.R. Oral leukoplakia. A More Challenging Disorder than It Seems. Proceedings 2019, 35, 9. https://doi.org/10.3390/proceedings2019035009
Tovaru SR. Oral leukoplakia. A More Challenging Disorder than It Seems. Proceedings. 2019; 35(1):9. https://doi.org/10.3390/proceedings2019035009
Chicago/Turabian StyleTovaru, Serban Radu. 2019. "Oral leukoplakia. A More Challenging Disorder than It Seems" Proceedings 35, no. 1: 9. https://doi.org/10.3390/proceedings2019035009
APA StyleTovaru, S. R. (2019). Oral leukoplakia. A More Challenging Disorder than It Seems. Proceedings, 35(1), 9. https://doi.org/10.3390/proceedings2019035009



