Hard Palate Hyperpigmentation Induced by Chloroquine: A Case Report †
1. Introduction
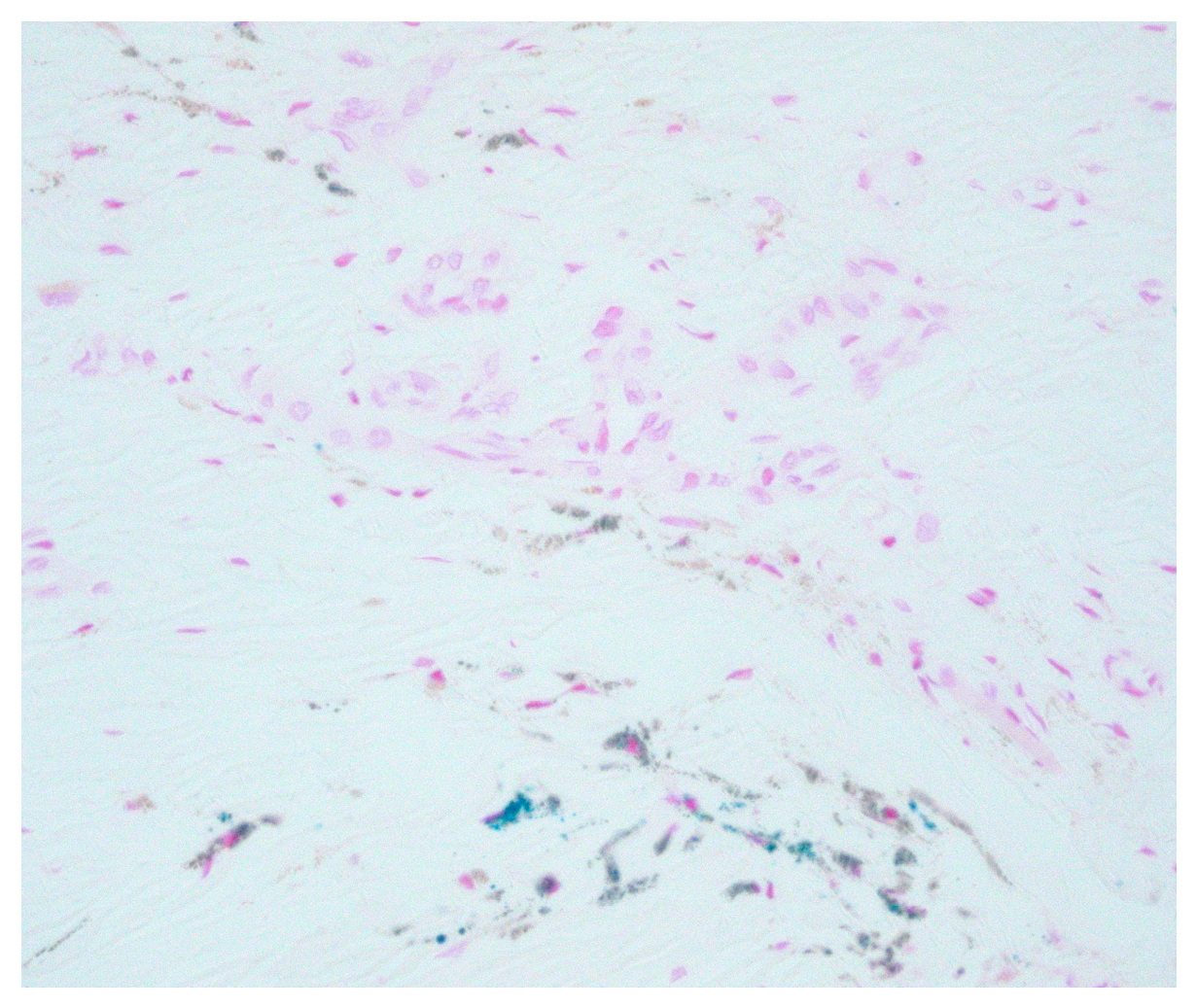
2. Case Report
3. Discussion
Conflicts of Interest
References
- Joseph, A.; Regezi, J.S.; Richard, C.K.; Jordan, A. Oral Pathology: Clinical Pathologic Correlations, 7th ed.; Elsevier-Saunders: Amsterdam, The Netherlands, 2017. [Google Scholar]
- De Andrade, B.A.B.; Padron-Alvarado, N.A.; Muñoz-Campos, E.M.; Morais, T.M.L.; Martinez-Pedraza, R. Hyperpigmentation of hard palate induced by chloroquine therapy. J. Clin. Exp. Dent. 2017, 9, e1487–e1491. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tosios, K.I.; Kalogirou, E.M.; Sklavounou, A. Drug-associated hyperpigmentation of the oral mucosa: report of four cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, e54–e66. [Google Scholar] [CrossRef] [PubMed]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Attuati, S.; Martini, V.; Bonacina, R.; Mariani, U.; Gianatti, A. Hard Palate Hyperpigmentation Induced by Chloroquine: A Case Report. Proceedings 2019, 35, 45. https://doi.org/10.3390/proceedings2019035045
Attuati S, Martini V, Bonacina R, Mariani U, Gianatti A. Hard Palate Hyperpigmentation Induced by Chloroquine: A Case Report. Proceedings. 2019; 35(1):45. https://doi.org/10.3390/proceedings2019035045
Chicago/Turabian StyleAttuati, Sara, Valeria Martini, Riccardo Bonacina, Umberto Mariani, and Andrea Gianatti. 2019. "Hard Palate Hyperpigmentation Induced by Chloroquine: A Case Report" Proceedings 35, no. 1: 45. https://doi.org/10.3390/proceedings2019035045
APA StyleAttuati, S., Martini, V., Bonacina, R., Mariani, U., & Gianatti, A. (2019). Hard Palate Hyperpigmentation Induced by Chloroquine: A Case Report. Proceedings, 35(1), 45. https://doi.org/10.3390/proceedings2019035045



