The diagnosis and treatment of oral erosion/ulceration is often challenging due to the clinician’s limited exposure to the conditions that may cause the lesions and their similar appearances. While many oral ulcers and erosions are the result of chronic trauma, some may indicate an underlying systemic condition such as a gastrointestinal dysfunction, malignancy, immunologic abnormality, or cutaneous disease. Correctly establishing a definitive diagnosis is of major importance to clinicians who manage patients with oral mucosal disease [
1].
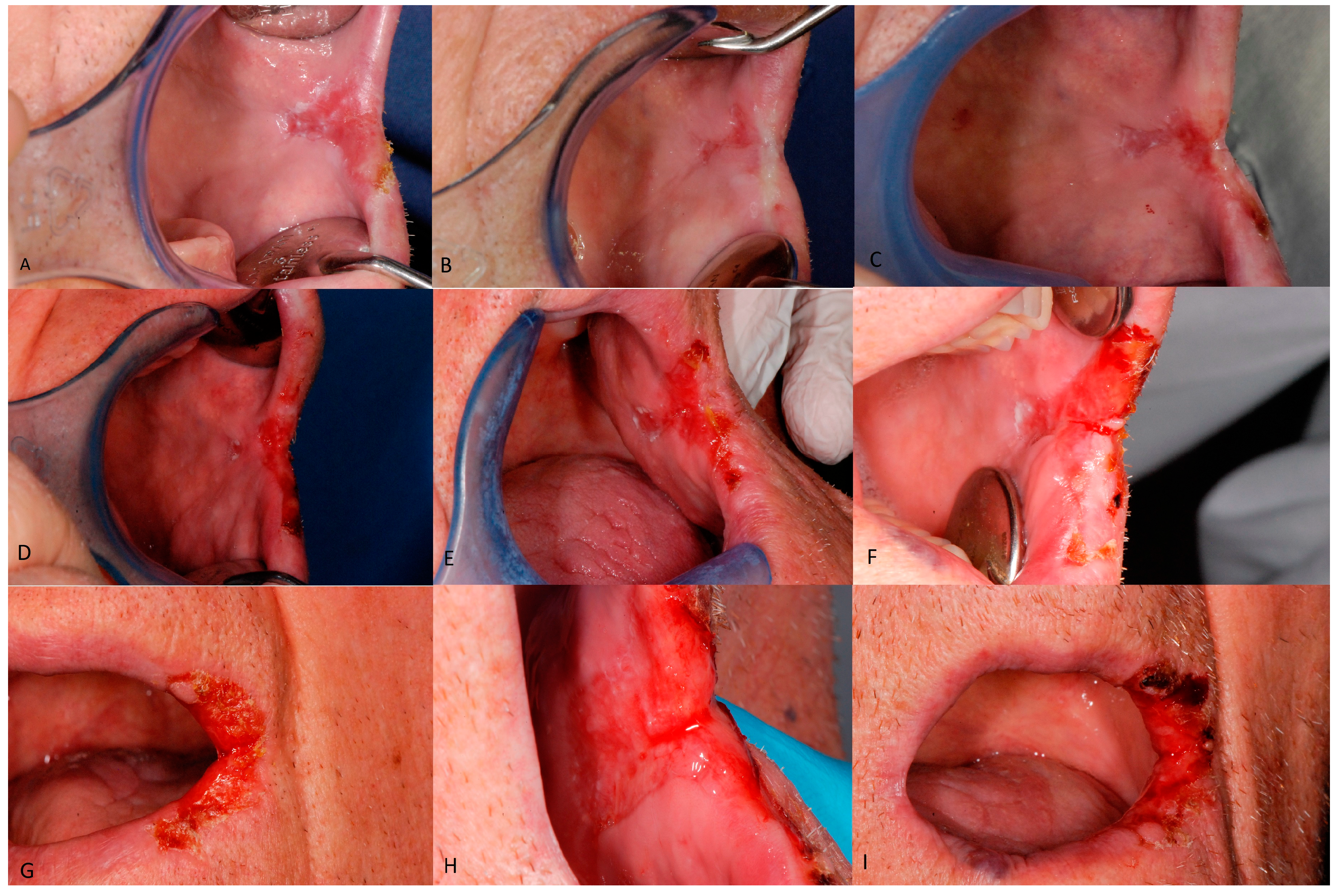
A 77-year-old male edentulous former smoker (stopped in 1962) suffering of hypertension, angina and glaucoma in pharmacological treatment, was admitted to our Oral Medicine and Oral Oncology Clinic on January 2010 with severe and persistent eroded lesions noticed 3 months prior to his visit (
Figure 1A). Lesions involved the left buccal mucosa; extending to left labial commissure and the vermillion. No other lesions could be detected at an oral and cutaneous examination. Map biopsies under Velscope
® guide were performed but the pathological assessment didn’t highlight any alteration in the oral mucosa. Miconazole 2% gel (3 applications per day per 15 days) and Chlortetracycline 3% ointment (3 applications per day per 15 days) treatment improved the clinical aspect of the lesion. After 3 months since the erosion didn’t show up any more improvement, the patient underwent cryosurgery. A nearly complete regression of the erosion was obtained (
Figure 1B). On March 2011, meanwhile two new denture were performed, a worsening of the clinical aspect and of the symptoms had led to the execution of new biopsy samples, which highlighted the presence of mild-moderate dysplasia (
Figure 1C). The patient decided to do not perform the excision, so a new biopsy was performed on November 2011(
Figure 1D). The pathological assessment showed the presence of an in situ carcinoma. The patient underwent photodynamic therapy in 2012. During the follow-up on March 2013 (
Figure 1E) a new severe worsening appeared, with the involvement of the buccal mucosa and also of the skin of the labial commissure by erosion with scabs. The histologic examination ruled out a relapse. Until 2016 the erosion changed several time his clinical aspect. Hematological and Quantiferon exams were required, but they excluded a Tuberculosis infection and a lymphoproliferative disorder. Several pharmacological treatments (antimicotic and antibiotic topical use) couldn’t heal the lesion, biopsies were repeated in the years (September 2013 (
Figure 1F,G), March 2014) until April 2016 (
Figure 1H,I) when the pathological assessment disclosed a mild dysplasia. Because of the worsening of the systemic condition of the patient (since 2015 the patient was suffering of Alzheimer disease), according with the son of the patient, was decided to keep only clinical follow-up. On August 2017 the patient died due to a complication of senile dementia.
Diagnosis of oral erosion-ulceration can be challenging and requires careful clinical examination and history taking. Persistent oral ulcerations can result from a variety of disparate etiologies and, therefore, may pose a diagnostic challenge. Historically, the diagnosis of many of these conditions has been made based only on clinical presentation, sometimes along with tissue biopsy [
2]. However, not every case will present the typical clinical or histological features associated with a certain condition. The management of many of these conditions has been similarly nonspecific, often involving non-targeted anti-inflammatory or immunosuppressive agents.