A Qualitative Assessment of an Ambient Display to Support In-Home Medication of Older Adults †
Abstract
:1. Introduction
2. Medication Ambient Display (MAD)
2.1. Ambient Modalities
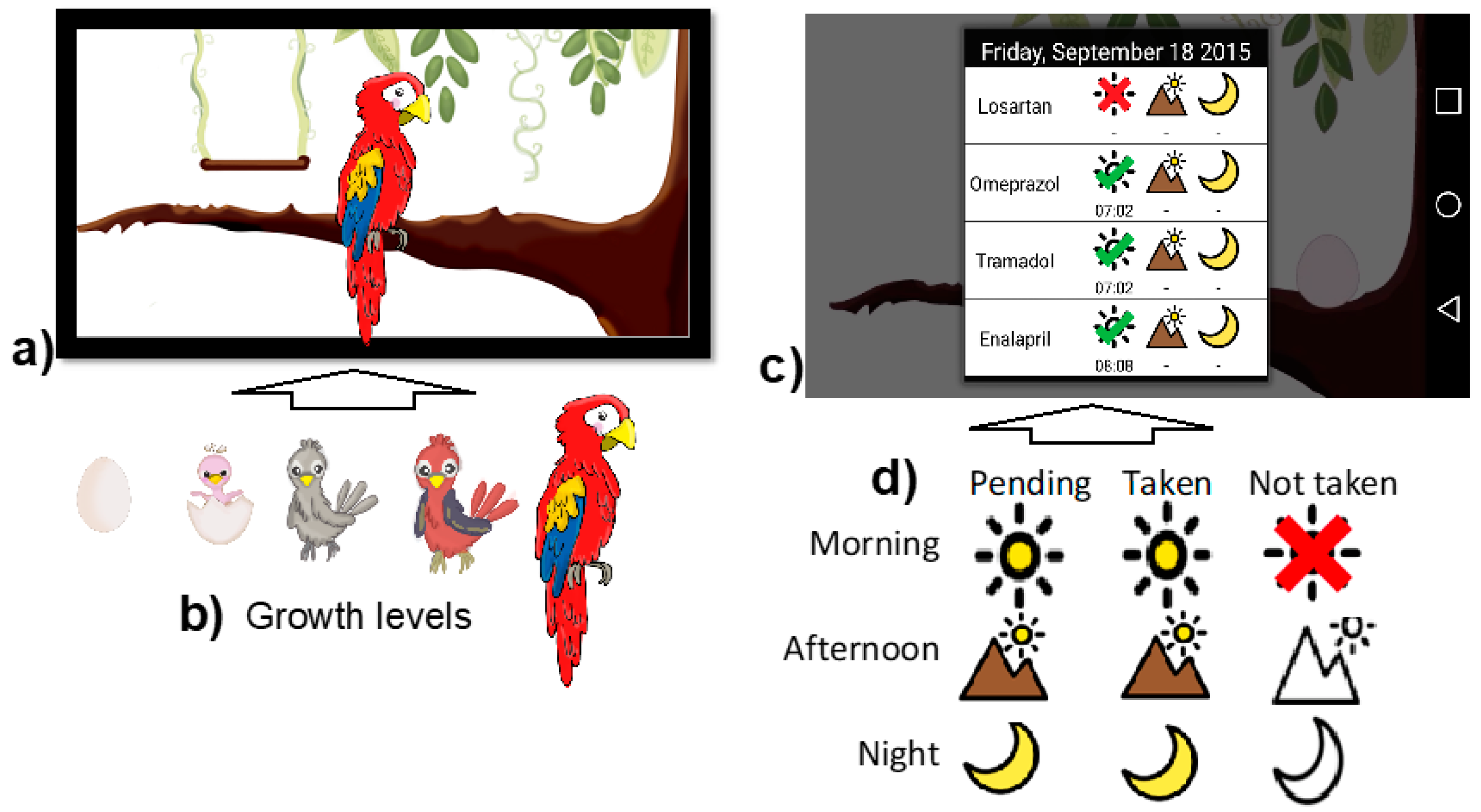
- Abstract representations of the daily medication taking: The MAD implementation shows a virtual bird, which has the aim of raising elders’ consciousness about how they have to take the responsibility for caring for their own health, in a similar way that they gladly take care of their pets. As presented in Figure 1a,b, the abstract representation is an animated parakeet that symbolizes the daily medication adherence. Each day a new pet hatches to represent the medication adherence. Additionally, by touching any point of the virtual parakeet, the MAD presents detailed information of the daily medication adherence by using the notation presented in Figure 1d. For instance, in Figure 1c, MAD shows the 4 medicines that a senior needs to take 3 times a day: during morning, afternoon and night. Additionally, it presents that a morning medicine (e.g., Losartan) was not taken; and that the afternoon and night doses are still pending.
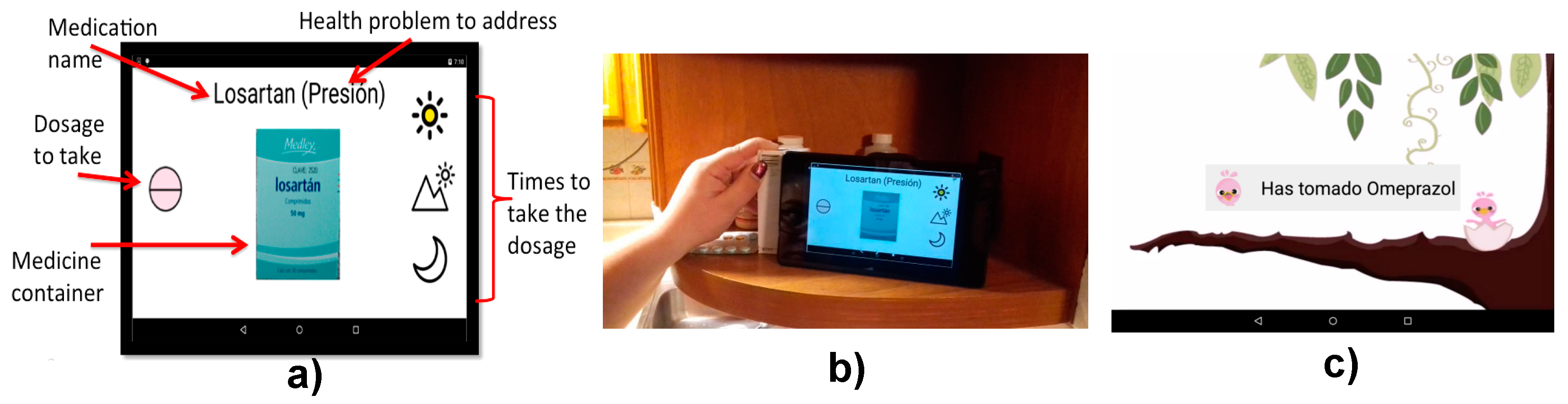
- Auditory and pictograms-based notifications to remind taking medications: The auditory notifications (i.e., a parakeet whistle) call the older adults attention when they have to take medications; while the pictograms-based notifications present critical information to follow the medication regimen as described in Figure 2a).
2.2. MAD Deployment
3. Methods
3.1. Study Aim
3.2. Study Flow
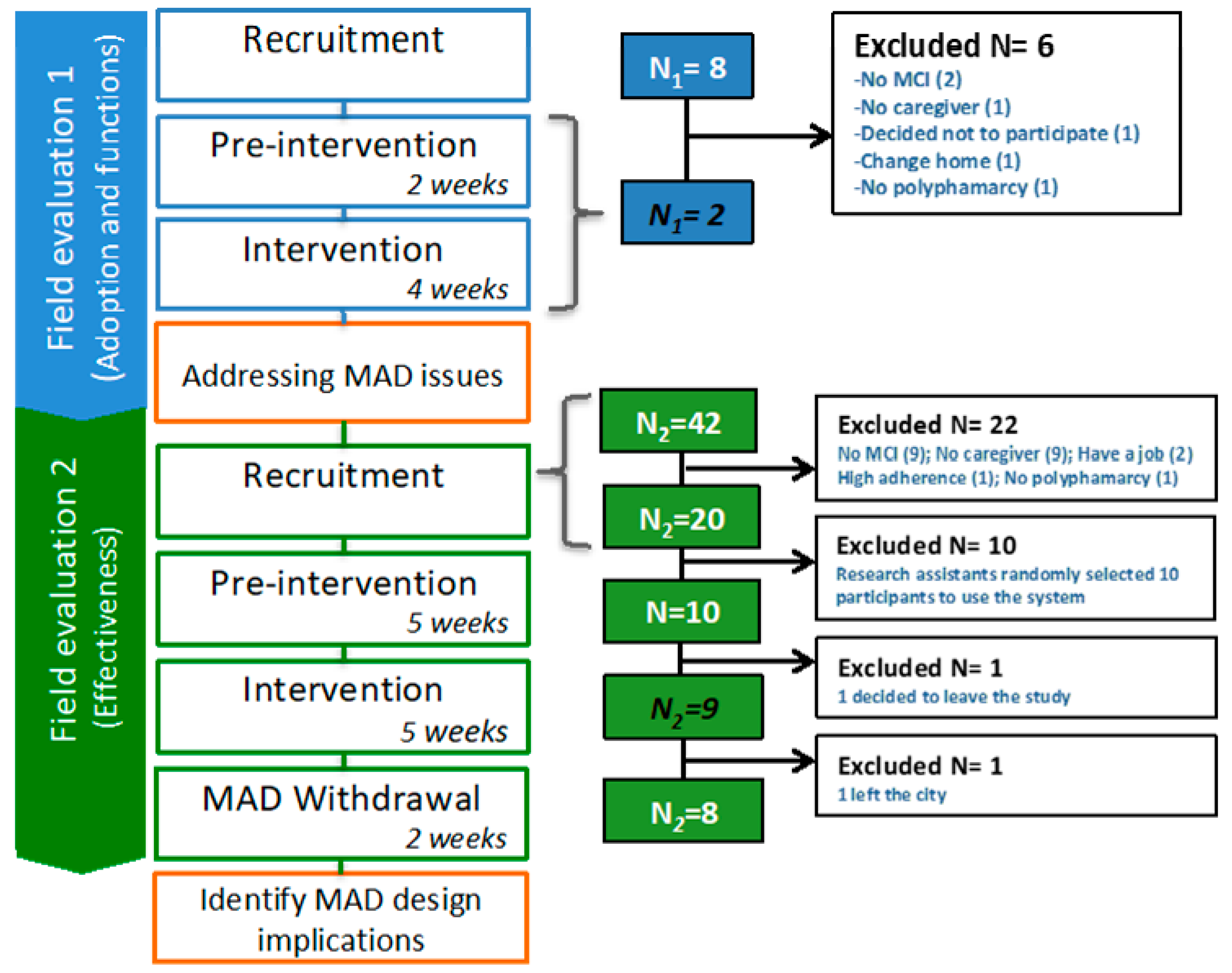
3.2.1. Field Evaluation 1
3.2.2. Field Evaluation 2
3.2.3. Field Evaluations’ Stages
- Recruitment. To be eligible to participate, older adults had to be over 60 years old, live at their homes, present poly-pharmacy, i.e., taking at least three prescribed medications, have mild cognitive impairment (MCI), report medications forgetting events, and have a relative that assists them in following the medication routine, such as reminding to medicate or serving medications. We assessed the eligibility criteria through interviews and by administered validated clinical instruments, which are described in Table 1. Enrolled older adults signed an informed consent form and received roughly $14.00 USD as a weekly economical incentive. To contact potential participants, we used different strategies for each of the evaluations.
- Pre-intervention (baseline). To characterize participants, we conducted a contextual inquiry consisting of semi-structured interviews and observation. We collected data in three major aspects: problems faced in medicating adequately, help received by their relatives, and feelings of the family caregivers.
- Intervention (use of the technology). We visited each of the older adults to introduce MAD in the presence of their caregivers. For this training, we used the “spaced retrieval” approach that consists on the following activities sequence: teach, ask, wait, ask again, wait, ask again [19]. After the training session, which lasted 40 min. approximately, MAD was personalized according to older adults’ prescriptions, and the timetables that they used to medicate. MAD was placed in the home’s room where they usually medicate, mostly it was in the kitchen and living room. Similar to the pre-intervention stage, we conducted the contextual inquiry and centered it to find out if MAD produced changes in older adults’ medication behavior, and caregivers activities and feelings.
3.3. Data Analysis
| Characteristics | N = 11 |
|---|---|
| Age (years) | 69.64 ± 6.71 |
| Cognitive impairment | Mild (MCI) a |
| Formal education completed (years) | 6.73 ± 2.87 |
| Caregiver relationship | Spouse: 4 Child: 6 Grandchild: 1 |
| Medication Adherence (Pill Counting) | 81.04 ± 15.01 b |
| Reported Medication self-efficacy c | 4 reported low adherence 7 reported mild adherence |
3.4. Organizational Setting
4. Findings
4.1. Possitive Effects of MAD
- Reducing instances of forgetting. MAD not only helped older adults remember medicating, but also to recall if medications had been taken. For instance, P1’s wife reported that some risky behaviors diminished, e.g., she stated: “one morning [before using MAD] I found two pills on the bed that he took out from the container and apparently forgot to take them, but now [while using MAD], he is more attentive to taking his pills.” Additionally, MAD helped caregivers ensure that older adults did not forget to take medication; e.g., P9 said: “my children used to forget to remind me to take medications. Now, they hear the parakeet, and then check if I am taking them …”. By calculating the weekly medication adherence of the 9 participants of the second field evaluation, and then the average of these weekly estimations for each evaluation stage, we found that it increased from M = 83.61% (SD = 15) in the pre-intervention to M = 95.97% (SD = 6.08) in the intervention. Nonetheless, with the withdrawal of MAD, it decreased to M = 76.71% (SD = 16.33). By using One-Way ANOVA with repeated measures, we compared the effect of MAD on the group of participants during the three phases. It showed a significant statistical difference between at least two of the phases (F[2, 14] = 6.59, p = 0.0096). With a post-hoc analysis using Tukey’s HSD, we identified that there exists a statistical difference between the pre-intervention and intervention phases (p = 0.02), and between the intervention and post-intervention phases (p = 0.0016); and Cohen’s effect size values (d = 1.35 and d = 1.72, respectively) suggest a high practical significance in both cases. This positive effect on the participants’ behavior is also evident when estimating the cumulative medication adherence, as illustrated in Figure 5. It shows that the participants’ medication adherence improved from 83.61% at the end of the pre-intervention phase, to 87.99% at the end of the intervention; and finally, it diminished during the post-intervention up to 85.82%. We asked older adults to explain their perception of their medication behavior during the post-intervention phase. Seven (7) older adults felt that it had been negatively affected. For instance, the participant P6 stated: “I take them at any time, or until I remember to … Before [during the intervention], when the parakeet sang, then I came [to the kitchen] to take them, and noticed the missed pills”. On the other hand, two participants (P5 and P10) perceived that their medication adherence was not affected; however, their average medication adherence estimated for each phase, dropped from M = 89.10% during the intervention phase to M = 74.29% during the post-intervention for P5, and from M = 92.62% to M = 69.29% for P10.
- Preventing symptom based-medication: We found that for some older adults, symptoms acted as cues for realizing that they had forgotten to take their pills. For participant P1, who took medications for pain relief, the system helped him take them on time and prevent under-medication, which increased his physical pain, or overmedication, which highly worried his wife. Regarding this, he reported: “… I used to skip the doctor instructions, now I obey the system and I feel more supported and responsible”. Similar benefits of using MAD were reported by P9: “[before using MAD] I realized that I have forgotten to take the pills for controlling my blood pressure, until I felt dizzy”.
- Better awareness within informal care network: MAD enhanced the awareness within the informal care network of the care recipient’s day-to-day medication intake. The system changed the patterns of caregiving, which were influenced by the particular family context. For instance, P1 lived with her husband and an adolescent grandchild. However, P1’s daughter was the relative concerned for her medication adherence, who did not live in the same home but used to visit P1 every day to prepare lunch, while checking and advising her to remember medicating. During the intervention phase, P1’s daughter reported consulting the system once a day, every day: “If I don’t check it in the morning, I check it in the afternoon. Now, I don’t have to ask my mom about her medications”. A more relevant result was that the system made P1’s adolescent grandchild get more involved in her medication routine. During the first week, he got familiarized with the system functionality. During the following weeks of the study, the afternoon auditory notification made him aware about helping her apply the glaucoma eye-drops, which was an issue that worried P1’s daughter. Different circumstances influenced the system’s adoption by P9, who lives with her grandchildren. P9 reported: “Before [using the system] I used to forget to take medications, and my children forgot to remind me. Now, when they hear the parakeet whistle, they ask me: ‘Mom, have you taken your pills?’”. Similarly, P8’s husband commented: “When my wife is in the backyard, and the parakeet sings, then I call her, prepare the medications and approach the tablet to register them”.
4.2. Challenges for Adopting MAD
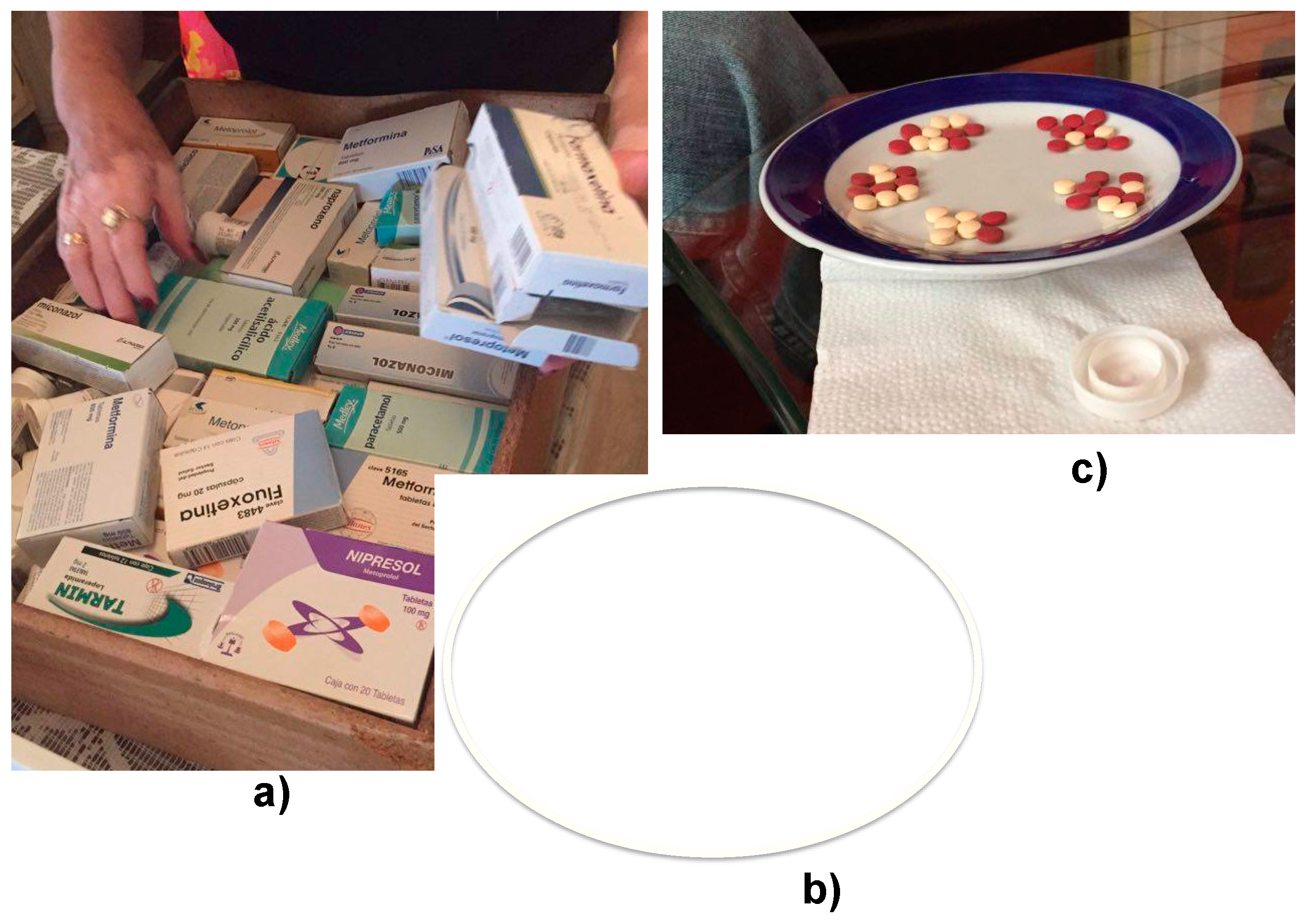
- Accumulation of medications: Four (4) participants reported that physicians authorize medications refilling on each visit, causing them to accumulate medications. For example, one of the participants had an inappropriate control of her medications since she stored and ordered her medications as illustrated in Figure 6a; she was initially reluctant to use the system since she had to adopt a new way to manage her medication, which included to take pills from the containers with the attached NFC.
- Similar medication containers and pills: Participant P3 was illiterate and used to identify medications through the physical appearance of their containers, and pills’ shape and color (see Figure 6b,c). However, she reported that some containers of different medications look alike, and that containers design may change, which incremented her dependency on her husband for recognizing medications.
- Complex medication routines: Additionally, participant P3 had a complex medication routine since she took several (6) medications on different timetables, and decided not to combine any of them. Therefore, she felt that receiving many reminders daily was overwhelming, causing her to decline to use the system at the beginning of the intervention stage as depicted in Figure 4.
5. Discussion
5.1. Design Implications
- Ambient stylized representations encourage relatives to assist older adults: Receiving direct family assistance is the main approach to ensuring that older adults with cognitive decline follow their prescribed medications regimens [27]. On the other side, a related line of research shows that caregivers are slow to assume responsibility for administering patients’ medications and often wait until safety issues are apparent [27]. We found that MAD enhanced the awareness within the family care network of the older adults’ medication intake, which made caregiving patterns change, such as motivating relatives to provide older adults with direct assistance. We attributed this effect to the fact that MAD was designed: (i) to be integrated into the home as an ornament, which attracted the attention of relatives; and (ii) to reveal the older adults’ medication behavior through stylized and dynamic representations. However, MAD did not enable both older adults and relatives, to be aware about the effect of the medication management strategies adopted to cope with specific contextual conditions, such as being illiterate or accumulating medications. Consequently, further design features should be incorporated into MAD. To this end, the following are our recommendations to develop ambient technologies that cope with risky medication-related behaviors of older adults.
- Persuading strategies for supporting the rational use of medications: Technologies may perform a retrospective assessment of the number of doses dispensed over the dispensing period (i.e., medication possession ratio) [28], and used it to persuade older adults about making appropriate utilization and management of medication. For instance, the gamification [29] approach could be implemented to incentive older adults when they have an appropriate control of their medications; or by explicitly informing older adults and family caregivers about the quantity of medications they possess which may help them discuss with their physicians the pertinence of prescriptions refill.
- Intelligent recognition of medications: To enable older adults to identify medication containers with similar appearance, medications technologies may incorporate algorithms to recognize objects. Belongie et al., 2014 [30], proposes the shape matching algorithm to identify correspondence between shapes; however, its computational efficiency may be high since it requires an images database for the algorithm training stage. A more appropriate algorithm to be executed in Tablets PC may be the proposed by Jiang et al., 2014 [31], to recognize the characters of medications’ labels. It uses methods such as contour tracking, projection and back-propagation neural networks for character recognition.
- Knowledge based-systems to adjust the medication regimens to older adults’ daily routine: To cope with the lack of appropriate and regular professional assessment for planning how to follow medication regimens [32], we propose that intelligent agents assist older adults at home to adjust their medication routine to fit into their lifestyles. Agents may propose a medication schedule based on their daily activities; suggest how to pair daily routines with the prescribed medication regimen since routines may act as additional cues for remembering medicating [2,11,32] and finally, recognize potential drugs interactions to assess if they could be combined. To provide this personal assistance, agents need a knowledge base to make inferences and decisions about a medication regimen. In this sense, ontologies can be used to enable agents to accomplish a semantic reasoning about a particular domain. Ontologies have been used for empowering computing systems with ambient intelligence to personalize non-pharmacological interventions for patients with dementia [33]. The advantage of using ontologies is that domain knowledge can be reused; thus, system designers may take advantage of medical ontologies that describe diseases [33], and drug-drug interactions [34].
5.2. Study Limitations
6. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Murray, M.A.; Morrow, D.G.; Winer, M.; Clark, D.O.; Tu, W.; Deer, M.M.; Brater, D.C.; Weinberger, M. Conceptual framework to study medication adherence in older adults. Am. J. Geriatr. Pharmacother. 2004, 2, 36–43. [Google Scholar] [CrossRef]
- Insel, K.; Einstein, G.O.; Morrow, D.G.; Hepworth, J.T. A multifaceted prospective memory intervention to improve medication adherence: Design of a randomized control trial. Contemp. Clin. Trials 2013, 34, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Chasteen, A.L.; Park, D.C.; Schwarz, N. Implementation intentions and facilitation of prospective memory. Psychol. Sci. 2001, 12, 457–461. [Google Scholar] [CrossRef]
- Kang, H.S.; Myung, W.; Na, D.L.; Kim, S.Y.; Lee, J.H.; Han, S.H.; Choi, S.H.; Kim, S.; Kim, S.; Kim, D.K. Factors associated with caregiver burden in patients with Alzheimer’s disease. Psychiatry Investig. 2014, 11, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Vira, T.; Colquhoun, M.; Etchells, E. Reconcilable differences: Correcting medication errors at hospital admission and discharge. Qual. Saf. Health Care 2006, 15, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Wimmer, B.C.; Bell, J.S.; Fastbom, J.; Wiese, M.D.; Johnell, K. Medication regimen complexity and number of medications as factors associated with unplanned hospitalizations in older people: A population-based cohort study. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 831–837. [Google Scholar] [CrossRef]
- Doubova, S.V.; Reyes-Morales, H.; Torres-Arreola, L.P.; Suarez-Ortega, M. Potential drug-drug and drug-disease interactions in prescriptions for ambulatory patients over 50 years of age in family medicine clinics in Mexico City. BMC Health Serv. Res. 2007. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, A.; Elnour, A.A.; Ali, A.A.; Hassan, N.A.; Shehab, A.; Bhagavathula, A.S. Evaluation of rational use of medicines (RUM) in four government hospitals in UAE. Saudi Pharm. J. 2015, 24, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Arriola-Peñalosa, M.A. The role of health regulations in the rational use of medicines. Gac. Med. Mex. 2015, 151, 640–647. (In Spanish) [Google Scholar]
- World Health Organization. WHO Policy Perspectives on Medicines-Promoting Rational Use of Medicines: Core Components. September 2002, Geneva. Available online: http://www.who.int/medicines/publications/policyperspectives/en/ (accessed on 30 May 2016).
- Stawarz., K.; Cox, A.L.; Blandford, A. Don’t forget your pill! designing effective medication reminder apps that support users’ daily routines. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (2014), Toronto, ON, Canada, 26 April–1 May 2014; pp. 2269–2278. [Google Scholar]
- Hayes, T.L.; Cobbinah, K.; Dishongh, T.; Kaye, J.A.; Kimel, J.; Labhard, M.; Leen, T.; Lundell, J.; Ozertem, U.; Pavel, M.; et al. A study of medication-taking and unobtrusive, intelligent reminding. Telemed. J. E Health 2009, 15, 770–776. [Google Scholar] [CrossRef]
- Reeder, B.; Demiris, G.; Marek, K.D. Older adults’ satisfaction with a medication dispensing device in home care. Inform. Health Soc. Care 2013, 38, 211–222. [Google Scholar] [CrossRef]
- Vitality. (n.d.). GlowCaps. Available online: http://www.glowcaps.com/ (accessed on 30 May 2016).
- De Oliveira, R.; Cherubini, M.; Oliver, N. MoviPill: Improving medication compliance for elders using a mobile persuasive social game. In Proceedings of the ACM International Conference on Ubiquitous Computing (2010), Copenhagen, Denmark, 26–29 September 2010; pp. 251–260. [Google Scholar]
- Lee, M.; Dey, A. Real-time feedback for improving medication taking. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (2014), Toronto, ON, Canada, 26 April–1 May 2014; pp. 2259–2268. [Google Scholar]
- Pousman, Z.; Stasko, J. A taxonomy of ambient information systems: Four patterns of design. In Proceedings of the ACM Working Conference on Advanced Visual Interfaces (2006), Venezia, Italy, 23–26 May; pp. 67–74.
- Mankoff, J.; Dey, A.K.; Hsieh, G.; Kientz, J.; Lederer, S.; Ames, M. Heuristic evaluation of ambient displays. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (2003), Fort Lauderdale, FL, USA, 5–10 April 2003; pp. 169–176. [Google Scholar]
- Zárate-Bravo, E.; García-Vázquez, J.P.; Rodríguez, M.D. An ambient medication display to heighten the peace of mind of family caregivers of older adults: A study of feasibility. In Proceedings of the Pervasive Computing Paradigms for Mental Health (MindCare 2015), Milan, Italy, 24–25 September 2015; pp. 274–283. [Google Scholar]
- García-Vazquez, J.P.; Rodríguez, M.D.; Andrade, A.G.; Bravo, J. Supporting the strategies to improve elders’ medication compliance by providing ambient aids. Pers. Ubiquitous Comput. 2011, 15, 389–397. [Google Scholar] [CrossRef]
- Yen, P.Y.; Bakken, S. Review of health information technology usability study methodologies. J. Am. Med. Inform. Assoc. 2012, 19, 413–422. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Folstein, M.F.; Robins, L.N.; Helzer, J.E. The mini-mental state examination. Arch. Gen. Psychiatry 1983, 40, 812. [Google Scholar] [CrossRef] [PubMed]
- De la Iglesia, J.M.; Dueñas, R.; Onis, M.C.; Aguado, C.; Albert, C.; Luque, R. Adaptación y validación al castellano del cuestionario de Pfeiffer (SPMSQ) para detectar la existencia de deterioro cognitivo en personas mayores de 65 años. Med. Clin. 2001, 117, 129–134. [Google Scholar] [CrossRef]
- Risser, J.; Jacobson, T.A.; Kripalani, S. Development and psychometric evaluation of the self-efficacy for appropriate medication use scale (SEAMS) in low- literacy patients with chronic disease. J. Nurs. Meas. 2007, 15, 203–219. [Google Scholar] [CrossRef] [PubMed]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Kaasalainen, S.; Dolovich, L.; Papaioannou, A.; Holbrook, A.; Lau, E.; Ploeg, J.; Levine, M.; Cosby, J.; Emily, A. The process of medication management for older adults with dementia. J. Nurs. Healthc. Chronic Illn. 2011, 3, 407–418. [Google Scholar] [CrossRef]
- Steiner, J.F.; Prochazka, A.V. The assessment of refill compliance using pharmacy records. Methods, validity and applications. J. Clin. Epidemiol. 1997, 50, 105–116. [Google Scholar] [CrossRef]
- Deterding, S.; Dixon, D.; Khaled, R.; Nacke, L. From game design elements to gamefulness: Defining gamification. In Proceedings of the 15th International Academic MindTrek Conference: Envisioning Future Media Environments 2011, Tampere, Finland, 28–30 September 2011; pp. 9–15. [Google Scholar]
- Belongie, S.; Malik, J.; Puzicha, J. Shape matching and object recognition using shape contexts. IEEE Trans. Pattern Anal. Mach. Intell. 2001, 24, 509–522. [Google Scholar] [CrossRef]
- Jiang, Y.; Jin, C.; Gao, H. Study of highly efficient algorithms for the character recognition system of medicine bottle label. J. Softw. 2014, 9, 991–998. [Google Scholar] [CrossRef]
- Cramer, J.A. Optimizing long-term medication compliance. Neurology 1995, 45, S25–S28. [Google Scholar] [PubMed]
- Navarro, R.; Rodríguez, M.D.; Favela, J. Intervention tailoring in augmented cognition systems for elders with dementia. IEEE J. Biomed. Health Inform. 2014, 18, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Doulaverakis, C.; Nikolaidis, G.; Kleontas, A.; Kompatsiaris, I. GalenOWL: Ontology-based drug recommendations discovery. J. Biomed. Semant. 2012, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez, M.D.; Zarate-Bravo, E.; García-Vázquez, J.-P.; Andrade, Á.G.; Navarro, R.F.; Torres-Cervantes, E.; Ponce, G. A Qualitative Assessment of an Ambient Display to Support In-Home Medication of Older Adults. Proceedings 2018, 2, 1248. https://doi.org/10.3390/proceedings2191248
Rodríguez MD, Zarate-Bravo E, García-Vázquez J-P, Andrade ÁG, Navarro RF, Torres-Cervantes E, Ponce G. A Qualitative Assessment of an Ambient Display to Support In-Home Medication of Older Adults. Proceedings. 2018; 2(19):1248. https://doi.org/10.3390/proceedings2191248
Chicago/Turabian StyleRodríguez, Marcela D., Ernesto Zarate-Bravo, Juan-Pablo García-Vázquez, Ángel G. Andrade, René F. Navarro, Engracia Torres-Cervantes, and Gisela Ponce. 2018. "A Qualitative Assessment of an Ambient Display to Support In-Home Medication of Older Adults" Proceedings 2, no. 19: 1248. https://doi.org/10.3390/proceedings2191248
APA StyleRodríguez, M. D., Zarate-Bravo, E., García-Vázquez, J.-P., Andrade, Á. G., Navarro, R. F., Torres-Cervantes, E., & Ponce, G. (2018). A Qualitative Assessment of an Ambient Display to Support In-Home Medication of Older Adults. Proceedings, 2(19), 1248. https://doi.org/10.3390/proceedings2191248







