Prenatal and Postnatal Disparities in Very-Preterm Infants in a Study of Infections between 2018–2023 in Southeastern US
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Maternal Morbidities
3.2. Infant Infections
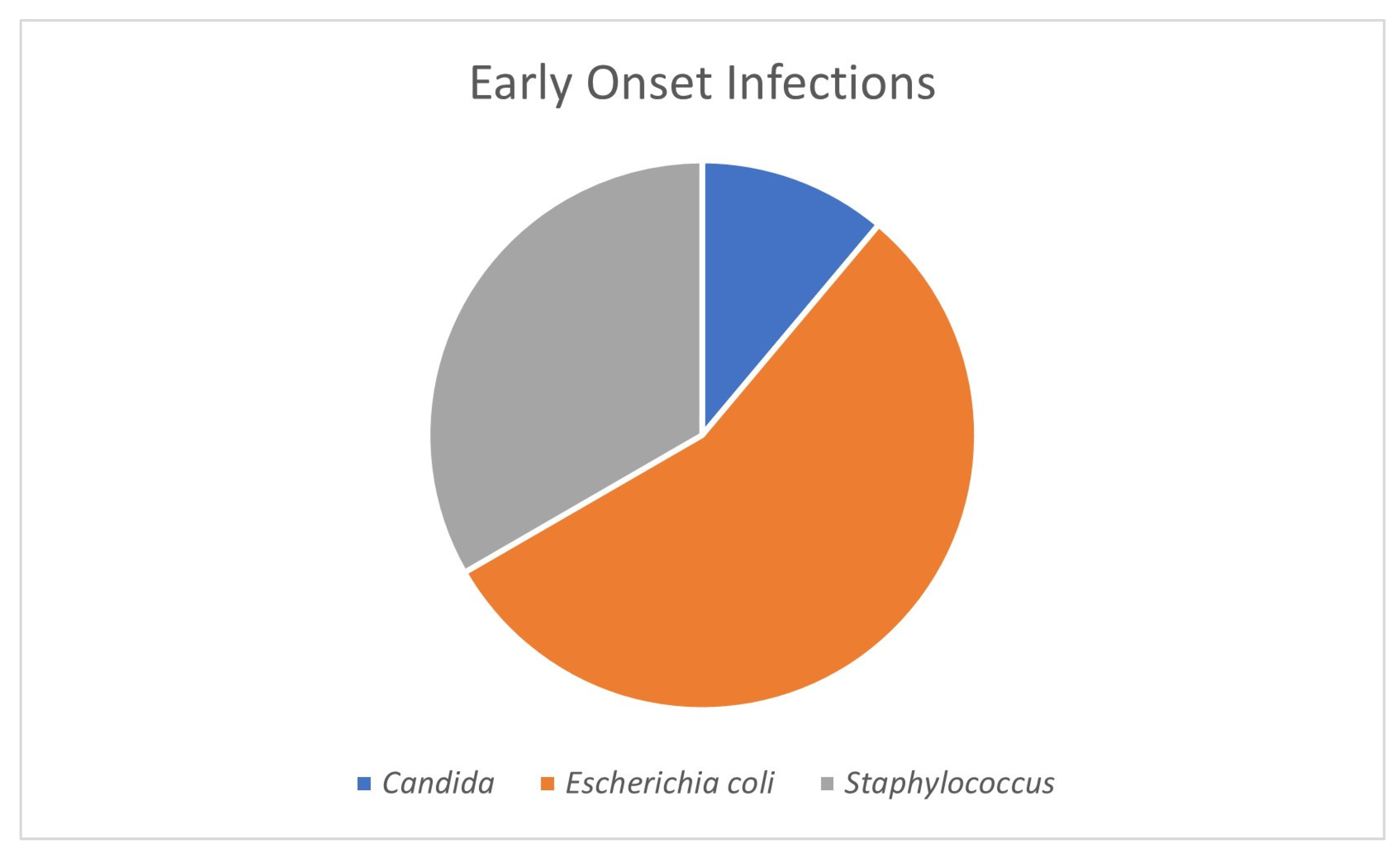
3.2.1. Early-Onset Sepsis
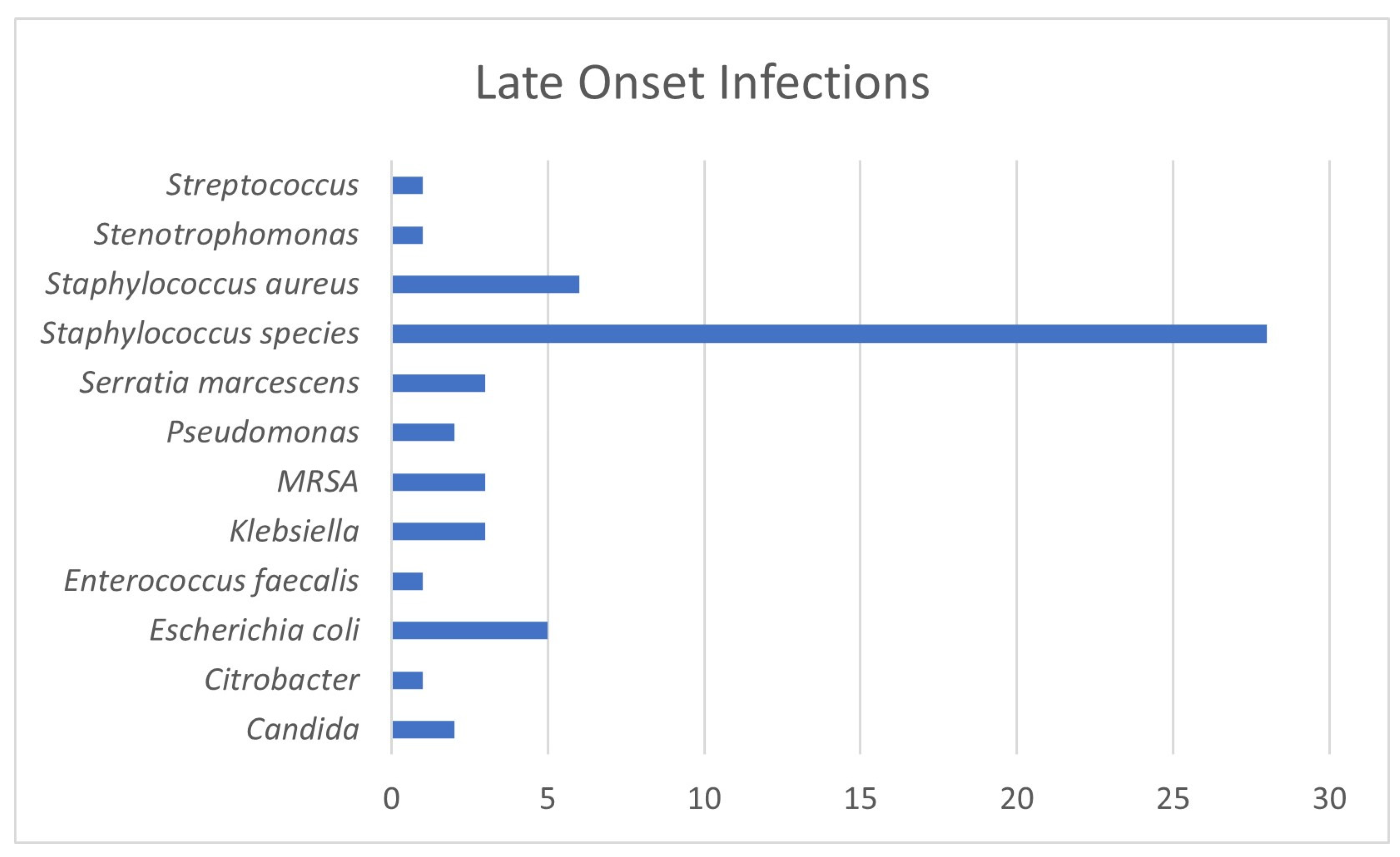
3.2.2. Late-Onset Sepsis
3.2.3. Gram-Positive versus Gram-Negative Infections
3.2.4. Urinary Tract Infections
3.2.5. Respiratory Tract Infections
3.2.6. Cerebral Spinal Fluid Infections
3.2.7. Necrotizing Enterocolitis
3.2.8. Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hamilton, B.E.; Martin, J.A.; Osterman, M.H.S.; Curtin, S.C.; Mathews, T.J.; Division of Vital Statistics. Births: Final Data for 2014. Natl. Vital Stat. Rep. 2015, 64, 1–64. [Google Scholar] [PubMed]
- Martin, J.A.O.M. Exploring the Decline in the Singleton Preterm Birth Rate in the United States, 2019–2020; Centers for Disease Control and Prevention (CDC), Statistics NCFH: Hyattsville, MD, USA, 2022.
- Matthews, T.J.; MacDorman, M.F.; Thoma, M.E. Infant Mortality Statistics from the 2013 Period Linked Birth/Infant Death Data Set. Natl. Vital Stat. Rep. 2015, 64, 1–30. [Google Scholar] [PubMed]
- Fanaroff, A.; Hack, M.; Walsh, M. The NICHD neonatal reseach network: Changes in practic adn outcomes during the first 15 years. Semin. Neonatol. 2003, 27, 281–287. [Google Scholar]
- Ertugrul, S.; Aktar, F.; Yolbas, I.; Yilmaz, A.; Elbey, B.; Yildirim, A.; Yilmaz, K.; Tekin, R. Risk Factors for Health Care-Associated Bloodstream Infections in a Neonatal Intensive Care Unit. Iran. J. Pediatr. 2016, 26, e5213. [Google Scholar] [CrossRef] [PubMed]
- Kurek Eken, M.; Tuten, A.; Ozkaya, E.; Karatekin, G.; Karateke, A. Major determinants of survival and length of stay in the neonatal intensive care unit of newborns from women with premature preterm rupture of membranes. J. Matern.-Fetal Neonatal Med. 2017, 30, 1972–1975. [Google Scholar] [CrossRef] [PubMed]
- Janevic, T.; Zeitlin, J.; Auger, N.; Egorova, N.N.; Hebert, P.; Balbierz, A.; Howell, E.A. Association of Race/Ethnicity With Very Preterm Neonatal Morbidities. JAMA Pediatr. 2018, 172, 1061–1069. [Google Scholar] [CrossRef]
- Assari, S. Social Epidemiology of Perceived Discrimination in the United States: Role of Race, Educational Attainment, and Income. Int. J. Epidemiol. Res. 2020, 7, 136–141. [Google Scholar] [CrossRef]
- Millender, E.; Barile, J.P.; Bagneris, J.R.; Harris, R.M.; De Faria, L.; Wong, F.Y.; Crusto, C.A.; Taylor, J.Y. Associations between social determinants of health, perceived discrimination, and body mass index on symptoms of depression among young African American mothers. Arch. Psychiatr. Nurs. 2021, 35, 94–101. [Google Scholar] [CrossRef]
- Travers, C.P.; Carlo, W.A.; McDonald, S.A.; Das, A.; Ambalavanan, N.; Bell, E.F.; Sánchez, P.J.; Stoll, B.J.; Wyckoff, M.H.; Laptook, A.R.; et al. Racial/Ethnic Disparities Among Extremely Preterm Infants in the United States from 2002 to 2016. JAMA Netw. Open 2020, 3, e206757. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes. The National Academies Collection: Reports funded by National Institutes of Health. In Preterm Birth: Causes, Consequences, and Prevention; Behrman, R.E., Butler, A.S., Eds.; National Academies Press: Washington, DC, USA, 2007. [Google Scholar]
- Xu, X.; Grigorescu, V.; Siefert, K.A.; Lori, J.R.; Ransom, S.B. Cost of racial disparity in preterm birth: Evidence from Michigan. J. Health Care Poor Underserved. 2009, 20, 729–747. [Google Scholar] [CrossRef]
- Sheikh, F.; Douglas, W.; Catenacci, V.; Machon, C.; Fox-Robichaud, A.E. Social Determinants of Health Associated with the Development of Sepsis in Adults: A Scoping Review. Crit. Care Explor. 2022, 4, e0731. [Google Scholar] [CrossRef]
- Greenberg, R.G.; Kandefer, S.; Do, B.T.; Smith, P.B.; Stoll, B.J.; Bell, E.F.; Carlo, W.A.; Laptook, A.R.; Sánchez, P.J.; Shankaran, S.; et al. Late-onset Sepsis in Extremely Premature Infants: 2000–2011. Pediatr. Infect. Dis. J. 2017, 36, 774–779. [Google Scholar] [CrossRef] [PubMed]
- Flannery, D.D.; Edwards, E.M.; Coggins, S.A.; Horbar, J.D.; Puopolo, K.M. Late-Onset Sepsis among Very Preterm Infants. Pediatrics 2022, 150, e2022058813. [Google Scholar] [CrossRef]
- Cohen, R.; Romain, O.; Tauzin, M.; Gras-Leguen, C.; Raymond, J.; Butin, M. Neonatal bacterial infections: Diagnosis, bacterial epidemiology and antibiotic treatment. Infect. Dis. Now. 2023, 53, 104793. [Google Scholar] [CrossRef] [PubMed]
- Puopolo, K.M.; Benitz, W.E.; Zaoutis, T.E. Management of Neonates Born at ≤34 6/7 Weeks’ Gestation with Suspected or Proven Early-Onset Bacterial Sepsis. Pediatrics 2018, 142, e20182896. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Puopolo, K.M.; Hansen, N.I.; Sánchez, P.J.; Bell, E.F.; Carlo, W.A.; Cotten, C.M.; D’angio, C.T.; Kazzi, S.N.J.; Poindexter, B.B.; et al. Early-Onset Neonatal Sepsis 2015 to 2017, the Rise of Escherichia coli, and the Need for Novel Prevention Strategies. JAMA Pediatr. 2020, 174, e200593. [Google Scholar] [CrossRef] [PubMed]
- Dey, A.C.; Hossain, M.I.; Afroze, S.; Dey, S.K.; Mannan, M.A.; Shahidullah, M. A Survey on Current Practice of Management of Early Onset Neonatal Sepsis. Mymensingh Med. J. 2016, 25, 243–247. [Google Scholar]
- Guo, L.; Han, W.; Su, Y.; Wang, N.; Chen, X.; Ma, J.; Liang, J.; Hao, L.; Ren, C. Perinatal risk factors for neonatal early-onset sepsis: A meta-analysis of observational studies. J. Matern.-Fetal Neonatal Med. 2023, 36, 2259049. [Google Scholar] [CrossRef]
- Boghossian, N.S.; Page, G.P.; Bell, E.F.; Stoll, B.J.; Murray, J.C.; Cotten, C.M.; Shankaran, S.; Walsh, M.C.; Laptook, A.R.; Newman, N.S.; et al. Late-onset sepsis in very low birth weight infants from singleton and multiple-gestation births. J. Pediatr. 2013, 162, 1120–1124.e1. [Google Scholar] [CrossRef] [PubMed]
- Köstlin-Gille, N.; Härtel, C.; Haug, C.; Göpel, W.; Zemlin, M.; Müller, A.; Poets, C.F.; Herting, E.; Gille, C. Epidemiology of early and late onset neonatal sepsis in very low birthweight infants: Data from the German neonatal network. Pediatr. Infect. Dis. J. 2021, 40, 255–259. [Google Scholar] [CrossRef]
- Dong, Y.; Speer, C.P. Late-onset neonatal sepsis: Recent developments. Arch. Dis. Child. Fetal Neonatal Ed. 2015, 100, F257–F263. [Google Scholar] [CrossRef] [PubMed]
- Coggins, S.A.; Glaser, K. Updates in late-onset sepsis: Risk assessment, therapy, and outcomes. Neoreviews 2022, 23, 738–755. [Google Scholar] [CrossRef] [PubMed]
- Dail, R.B.; Everhart, K.C.; Hardin, J.W.; Chang, W.; Kuehn, D.; Iskersky, V.; Fisher, K.; Murphy, H.J. Predicting infection in very preterm infants: A study protocol. Nurs. Res. 2021, 70, 142–149. [Google Scholar] [CrossRef]
- Nist, M.D.; Casavant, S.G.; Dail, R.B.; Everhart, K.C.; Sealschott, S.; Cong, X.S. Conducting neonatal intensive care unit research during a pandemic: Challenges and lessons learned. Nurs. Res. 2022, 71, 147–152. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, R.; Boutzoukas, A.E.; Chan, E.; Girgis, V.; Kinduelo, V.; Kwabia, S.A.; Yan, J.; Clark, R.H.; Zimmerman, K.O.; Greenberg, R.G. Urinary Tract Infection Epidemiology in NICUs in the United States. Am. J. Perinatol. 2023. [Google Scholar] [CrossRef] [PubMed]
- Horbar, J.D.; Greenberg, L.T.; Buzas, J.S.; Ehret, D.E.Y.; Soll, R.F.; Edwards, E.M. Trends in mortality and morbidities for infants born 24 to 28 weeks in the US: 1997–2021. Pediatrics 2024, 153, e2023064153. [Google Scholar] [CrossRef]
- Tham, N.; Fazio, T.; Johnson, D.; Skandarajah, A.; Hayes, I.P. Hospital Acquired infections in surgical patients: Impact of COVID-19-related infection prevention measures. World J. Surg. 2022, 46, 1249–1258. [Google Scholar] [CrossRef]
- Abubakar, U.; Awaisu, A.; Khan, A.H.; Alam, K. Impact of COVID-19 Pandemic on healthcare-associated infections: A systematic review and meta-analysis. Antibiotics 2023, 12, 1600. [Google Scholar] [CrossRef]
- Jung, E.; Romero, R.; Suksai, M.; Gotsch, F.; Chaemsaithong, P.; Erez, O.; Conde-Agudelo, A.; Gomez-Lopez, N.; Berry, S.M.; Meyyazhagan, A.; et al. Clinical chorioamnionitis at term: Definition, pathogenesis, microbiology, diagnosis, and treatment. Am. J. Obstet. Gynecol. 2024, 230, S807–S840. [Google Scholar] [CrossRef]
- Boghossian, N.S.; Geraci, M.; Lorch, S.A.; Phibbs, C.S.; Edwards, E.M.; Horbar, J.D. Racial and ethnic differences over time in outcomes of infants born less than 30 weeks’ gestation. Pediatrics 2019, 144, e20191106. [Google Scholar] [CrossRef] [PubMed]
- Manuck, T.A. Racial and ethnic differences in preterm birth: A complex, multifactorial problem. Semin. Perinatol. 2017, 41, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.; Dominguez, T.P.; Burke, W.; Dolan, S.M.; Stevenson, D.K.; Jackson, F.M.; Collins, J.W.; Driscoll, D.A.; Haley, T.; Acker, J.; et al. Explaining the black-white disparity in preterm birth: A consensus statement from a multi-disciplinary scientific work group convened by the March of Dimes. Front. Reprod. Health 2021, 3, 684207. [Google Scholar] [CrossRef] [PubMed]
- Diamond-Smith, N.; Baer, R.J.; Jelliffe-Pawlowski, L. Impact of being underweight before pregnancy on preterm birth by race/ethnicity and insurance status in California: An analysis of birth records. J. Matern.-Fetal Neonatal Med. 2024, 37, 2321486. [Google Scholar] [CrossRef] [PubMed]
- Han, Z.; Mulla, S.; Beyene, J.; Liao, G.; McDonald, S.D. Maternal underweight and the risk of preterm birth and low birth weight: A systematic review and meta-analyses. Int. J. Epidemiol. 2011, 40, 65–101. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.-Y.; Zhu, Y.; Wu, F.; Mao, J.; Liu, L.; Zhang, R.; Chang, Y.-M.; Shen, W.; Tang, L.-X.; Ye, X.-Z.; et al. The role of nutrition in analysis of risk factors and short-term outcomes for late-onset necrotizing enterocolitis among very preterm infants: A nationwide, multicenter study in China. BMC Pediatr. 2024, 24, 172. [Google Scholar] [CrossRef]
- Wang, W.; Jiang, T.; Zhang, W.; Li, C.; Chen, J.; Xiang, D.; Cao, K.; Qi, L.-W.; Li, P.; Zhu, W.; et al. Predictors of mortality in bloodstream infections caused by multidrug-resistant gram-negative bacteria: 4 years of collection. Am. J. Infect. Control 2017, 45, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Bock, A.; Hanson, B.M.; Ruffin, F.; Parsons, J.B.; Park, L.P.; Sharma-Kuinkel, B.; Mohnasky, M.; Arias, C.A.; Fowler Jr, V.G.; Thaden, J.T. Clinical and molecular analyses of recurrent gram-negative bloodstream infections. Clin. Infect. Dis. 2023, 76, e1285–e1293. [Google Scholar] [CrossRef]
- McGrath, C.L.; Bettinger, B.; Stimpson, M.; Bell, S.L.; Coker, T.R.; Kronman, M.P.; Zerr, D.M. Identifying and mitigating disparities in central line-associated bloodstream infections in minoritized racial, ethnic, and language groups. JAMA Pediatr. 2023, 177, 700–709. [Google Scholar] [CrossRef]
- Zhu, M.; Wang, L.; Zhuge, Z.; Li, W.; Zheng, Y.; Mai, J.; Lin, Z.; Lin, J. Risk factors associated with multi-drug resistance in neonatal sepsis caused by Escherichia coli. Infect. Drug Resist. 2023, 16, 2097–2106. [Google Scholar] [CrossRef] [PubMed]
- Malaure, C.; Geslain, G.; Birgy, A.; Bidet, P.; Poilane, I.; Allain, M.; Liberge, M.; Khattat, N.; Sikias, P.; Bonacorsi, S. Early-onset infection caused by Escherichia coli sequence Type 1193 in late preterm and full-term neonates. Emerg. Infect. Dis. 2024, 30, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Yuan, J.M.; Nugent, C.; Wilson, A.; Verlander, N.Q.; Alexander, E.; Fleming, P.; Modi, N.; Oughham, K.; Ratnaraja, N.; Wan, Y.; et al. Clinical outcomes of Staphylococcus capitis isolation from neonates, England, 2015–2021: A retrospective case-control study. Arch. Dis. Child. Fetal Neonatal Ed. 2024, 109, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Chavignon, M.; Coignet, L.; Bonhomme, M.; Bergot, M.; Tristan, A.; Verhoeven, P.; Josse, J.; Laurent, F.; Butin, M. Environmental persistence of Staphylococcus capitis NRCS-A in neonatal intensive care units: Role of biofilm formation, desiccation, and disinfectant tolerance. Microbiol. Spectr. 2022, 10, e0421522. [Google Scholar] [CrossRef] [PubMed]
- Yonghui, Y.; Bingjin, Z. A multicenter prospective cohort study of late-onset sepsis and its poor prognosis in very low birth weight infants. Zhonghua Er Ke Za Zhi 2023, 61, 228–234. [Google Scholar]
- Janardhan, S.; Kim, S.; Cukovic, B.; Demissie, S.; Roth, P.; Blau, J. Urinary tract infections in low birth weight neonates. Am. J. Perinatol. 2022. [Google Scholar] [CrossRef]
- Mohseny, A.B.; van Velze, V.; Steggerda, S.J.; Smits-Wintjens, V.; Bekker, V.; Lopriore, E. Late-onset sepsis due to urinary tract infection in very preterm neonates is not uncommon. Eur. J. Pediatr. 2018, 177, 33–38. [Google Scholar] [CrossRef]
- Szczerbiec, D.; Słaba, M.; Torzewska, A. Substances secreted by Lactobacillus spp. from the urinary tract microbiota play a protective role against Proteus mirabilis infections and their complications. Int. J. Mol. Sci. 2023, 25, 103. [Google Scholar]
- Gobec, K.; Mukenauer, R.; Keše, D.; Erčulj, V.; Grosek, Š.; Perme, T. Association between colonization of the respiratory tract with Ureaplasma species and bronchopulmonary dysplasia in newborns with extremely low gestational age: A retrospective study. Croat. Med. J. 2023, 64, 75–83. [Google Scholar] [CrossRef]
- Imanishi, Y.; Hirata, K.; Nozaki, M.; Mochizuki, N.; Hirano, S.; Wada, K. The Association between early gram-negative bacteria in tracheal aspirate cultures and severe bronchopulmonary dysplasia among extremely preterm infants requiring prolonged ventilation. Am. J. Perinatol. 2023, 40, 1321–1327. [Google Scholar] [CrossRef]
- Hunt, B.; Rogers, C.; Blais, R.M.; Adachi, K.; Sathyavagiswaran, L. Paenibacillus sepsis and meningitis in a premature infant: A case Report. Am. J. Forensic Med. Pathol. 2021, 42, 96–98. [Google Scholar] [CrossRef]
- DeLeon, S.D.; Welliver, R.C., Sr. Paenibacillus alvei sepsis in a neonate. Pediatr. Infect. Dis. J. 2016, 35, 358. [Google Scholar] [CrossRef]
- Hu, X.; Liang, H.; Li, F.; Zhang, R.; Zhu, Y.; Zhu, X.; Xu, Y. Necrotizing enterocolitis: Current understanding of the prevention and management. Pediatr. Surg. Int. 2024, 40, 32. [Google Scholar] [CrossRef] [PubMed]
- Cuna, A.; Sampath, V.; Khashu, M. Racial disparities in necrotizing enterocolitis. Front. Pediatr. 2021, 9, 633088. [Google Scholar] [CrossRef] [PubMed]
- Ree, I.M.; Smits-Wintjens, V.E.; Rijntjes-Jacobs, E.G.; Pelsma, I.C.; Steggerda, S.J.; Walther, F.J.; Lopriore, E. Necrotizing enterocolitis in small-for-gestational-age neonates: A matched case-control study. Neonatology 2014, 105, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Petersen, J.; Abusnina, W.; Beesabathina, S.; Desu, S.S.; Walters, R.W.; Alla, V.M. Racial disparities in outcomes of delivery and cardiac complications among pregnant women with congenital heart disease. J. Racial Ethn. Health Disparities 2024. [Google Scholar] [CrossRef]
- Sweeney, L.; Lundsberg, L.S.; Culhane, J.F.; Partridge, C.; Moeun, S. Co-existing chronic hypertension and hypertensive disorders of pregnancy and associated adverse pregnancy outcomes. J. Matern.-Fetal Neonatal Med. 2024, 37, 2305675. [Google Scholar] [CrossRef]
| Positive Blood Cultures | Black Preterms | White Preterms | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | BW Mean | BW SD | GA Mean | GA SD | N | BW Mean | BW SD | GA Mean | GA SD | |
| Early Onset Sepsis (7) | 5 | 1002.4 | 340.22 | 26.38 | 2.28 | 1 | 745 | NA | 26 | NA |
| Late Onset Sepsis (39) | 27 | 773.44 | 200.54 | 26.26 | 1.99 | 10 | 788.2 | 178.5 | 26.2 | 1.48 |
| Infants without LOS (323) | 199 | 996.7 | 252.69 | 27.87 | 2.02 | 97 | 1028.73 | 254.79 | 27.81 | 2.01 |
| Gram Positive Bacteria (35) | 22 | 828.67 | 226.14 | 26.33 | 1.17 | 8 | 787.67 | 188.48 | 26.22 | 1.56 |
| Gram Negative Bacteria (16) | 9 | 747.62 | 229.24 | 25.92 | 2.47 | 3 | 767.67 | 43.06 | 25.67 | 0.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dail, R.B.; Everhart, K.C.; Iskersky, V.; Chang, W.; Fisher, K.; Warren, K.; Steflik, H.J.; Hardin, J.W. Prenatal and Postnatal Disparities in Very-Preterm Infants in a Study of Infections between 2018–2023 in Southeastern US. Trop. Med. Infect. Dis. 2024, 9, 70. https://doi.org/10.3390/tropicalmed9040070
Dail RB, Everhart KC, Iskersky V, Chang W, Fisher K, Warren K, Steflik HJ, Hardin JW. Prenatal and Postnatal Disparities in Very-Preterm Infants in a Study of Infections between 2018–2023 in Southeastern US. Tropical Medicine and Infectious Disease. 2024; 9(4):70. https://doi.org/10.3390/tropicalmed9040070
Chicago/Turabian StyleDail, Robin B., Kayla C. Everhart, Victor Iskersky, Weili Chang, Kimberley Fisher, Karen Warren, Heidi J. Steflik, and James W. Hardin. 2024. "Prenatal and Postnatal Disparities in Very-Preterm Infants in a Study of Infections between 2018–2023 in Southeastern US" Tropical Medicine and Infectious Disease 9, no. 4: 70. https://doi.org/10.3390/tropicalmed9040070
APA StyleDail, R. B., Everhart, K. C., Iskersky, V., Chang, W., Fisher, K., Warren, K., Steflik, H. J., & Hardin, J. W. (2024). Prenatal and Postnatal Disparities in Very-Preterm Infants in a Study of Infections between 2018–2023 in Southeastern US. Tropical Medicine and Infectious Disease, 9(4), 70. https://doi.org/10.3390/tropicalmed9040070






