Assessing the Adoption of One Health Approaches in National Plans to Combat Health Threats: The Pilot of a One Health Conceptual Framework in Armenia
Abstract
1. Introduction
2. Materials and Methods
2.1. The One Health Conceptual Framework (OHCF)
2.2. Study Design
- Describe how the collection, analysis and dissemination of information is organized within and between relevant sectors involved in the surveillance systems.
- Discuss the main challenges and enabling factors in establishing a functional inter-sectoral utilization of the information collected across sectors.
- Assess gaps and opportunities in the adoption of OH approaches in prevention and preparedness strategies with the support of the OHCF.
- Identify key actions to enhance OH integration and assess their feasibility.
3. Results
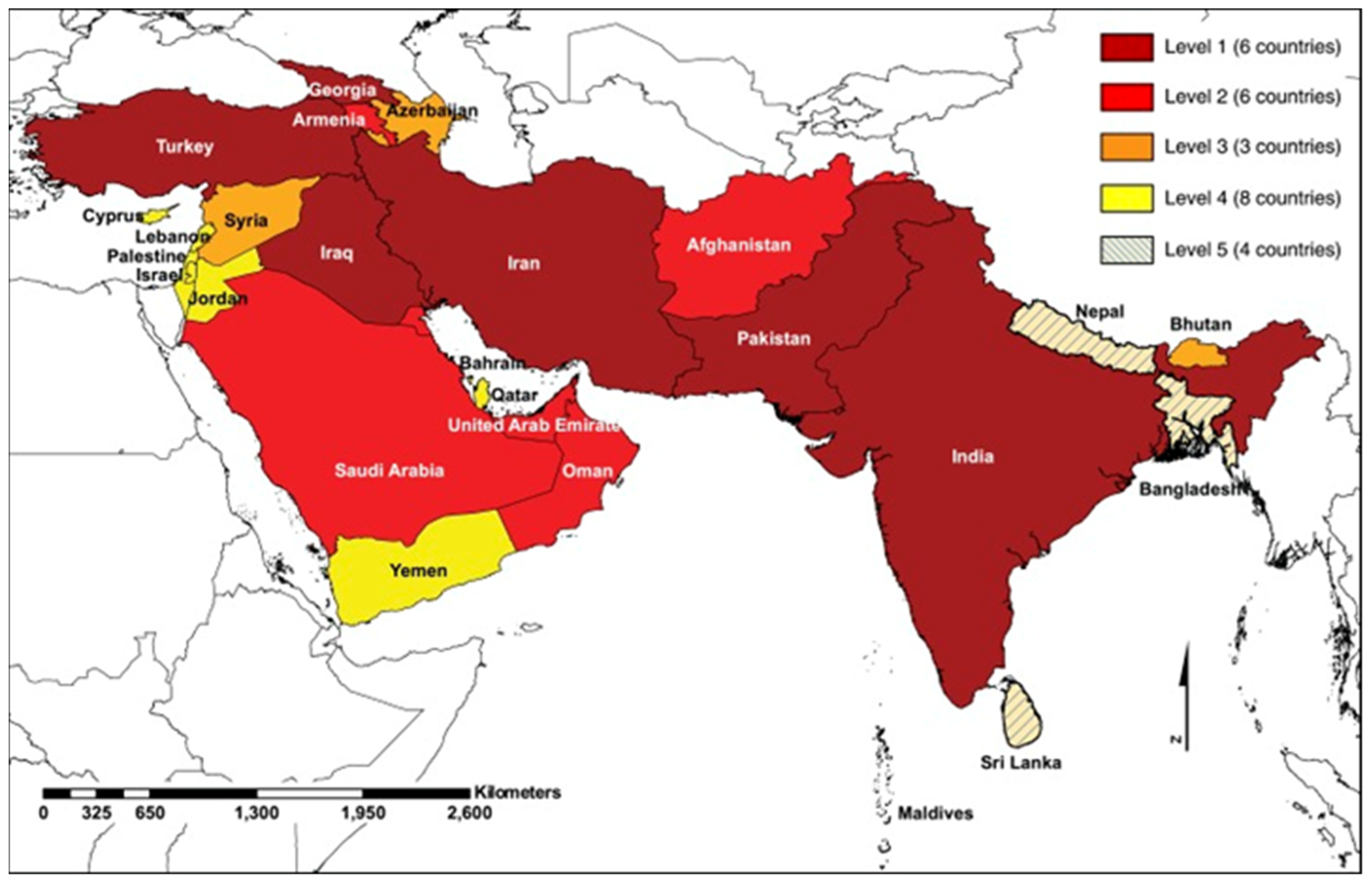
3.1. Preparatory Phase
- -
- Emerging or re-emerging threat with a changing of pattern distribution.
- -
- Emerging or re-emerging threat at the human–animal–environment interface requiring a multisectoral action (OH approach).
- -
- Available surveillance system or/and plans or/and recent response actions to the threat.
- Threat which has activated a recent response action to contain a potential outbreak of the disease.
- Threat for which an OH preparedness/surveillance plan is available.
- Threat detected or caused outbreaks/epidemics in the past ten years.
- Threat affecting food safety and/or food security.
- Threat benefitting the most from the integration of environmental and climatic data in its/their surveillance.
- Threat benefitting the most from the integration of OH in preparedness/surveillance/response.
- Threat greatly impacting socio-economic aspects in case of an outbreak.
- Threat detected in a new location or population in the country or neighbouring countries in the past ten years.
- Threat whose animal host (domestic or wild) is/are in close proximity to humans.
- Threat whose related vector/s’ presence and abundance are increasing due to anthropogenic, climatic and environmental factors.
- Threat with an integrated data collection and analysis system.
3.2. The First Workshop: Prioritization of Pathogens
- Seeking consensus about criteria and indicators for the prioritization of the selected pathogens;
- Ranking the pathogens on the basis of the agreed prioritization indicators.
3.3. The Second Workshop: Framing the OH System
3.3.1. The Surveillance Systems
- (1)
- CCHFV surveillance system in Armenia
- (2)
- Anthrax surveillance system in Armenia
3.3.2. The OH Assessment through the OHCF
3.4. The Third Workshop: Strengthening the OH System
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McMichael, A.J.; Woodruff, R.E.; Hales, S. Climate change and human health: Present and future risks. Lancet 2006, 367, 859–869. [Google Scholar] [CrossRef]
- Van de Vuurst, P.; Escobar, L.E. Climate change and infectious disease: A review of evidence and research trends. Infect. Dis. Poverty 2023, 12, 51. [Google Scholar] [CrossRef] [PubMed]
- Samson, J.; Berteaux, D.; McGill, B.J.; Humphries, M.M. Geographic disparities and moral hazards in the predicted impacts of climate change on human populations. Glob. Ecol. Biogeogr. 2011, 20, 532–544. [Google Scholar] [CrossRef]
- Kakkar, M.; Chauhan, A.S.; Bahl, T.; Rahi, M. Opportunities for one health policies to reduce poverty. Rev. Sci. Tech. l’OIE 2019, 38, 135–144. [Google Scholar] [CrossRef]
- Amuasi, J.H.; Walzer, C.; Heymann, D.; Carabin, H.; Huong, L.T.; Haines, A.; Winkler, A.S. Calling for a COVID-19 One Health Research Coalition. Lancet 2020, 395, 1543–1544. [Google Scholar] [CrossRef] [PubMed]
- Lefrançois, T.; Malvy, D.; Atlani-Duault, L.; Benamouzig, D.; Druais, P.-L.; Yazdanpanah, Y.; Delfraissy, J.-F.; Lina, B. After 2 years of the COVID-19 pandemic, translating one health into action is urgent. Lancet 2022, 401, 789–794. [Google Scholar] [CrossRef]
- Adisasmito, W.B.; Almuhairi, S.; Behravesh, C.B.; Bilivogui, P.; Bukachi, S.A.; Casas, N.; Becerra, N.C.; Charron, D.F.; Chaudhary, A.; Zanella, J.R.C.; et al. One health: A new definition for a sustainable and Healthy Future. PLoS Pathog. 2022, 18, e1010537. [Google Scholar]
- Sinclair, J.R. Importance of a one health approach in advancing global health security and the Sustainable Development goals. Rev. Sci. Tech. l’OIE 2019, 38, 145–154. [Google Scholar] [CrossRef]
- Dye, C. One health as a catalyst for sustainable development. Nat. Microbiol. 2022, 7, 467–468. [Google Scholar] [CrossRef] [PubMed]
- Bhadoria, P.; Gupta, G.; Agarwal, A. Viral Pandemics in the Past Two Decades: An Overview. J. Fam. Med. Prim. Care 2021, 10, 2745–2750. [Google Scholar] [CrossRef]
- WHO; FAO; OIE. Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries. Available online: https://apps.who.int/iris/handle/10665/325620 (accessed on 18 January 2023).
- Berthe, F.C.J.; Bouley, T.; Karesh, W.B.; Le Gall, F.G.; Machalaba, C.C.; Plante, C.A.; Seifman, R.M. Operational Framework for Strengthening Human, Animal and Environmental Public Health Systems at Their Interface; World Bank: Washington, DC, USA, 2018. [Google Scholar]
- He, J.; Guo, Z.; Yang, P.; Cao, C.; Xu, J.; Zhou, X.; Li, S. Social insights on the implementation of One Health in zoonosis prevention and control: A scoping review. Infect. Dis. Poverty 2022, 11, 48. [Google Scholar] [CrossRef] [PubMed]
- Kimani, T.; Kiambi, S.; Eckford, S.; Njuguna, J.; Makonnen, Y.; Rugalema, G.; Morzaria, S.P.; Lubroth, J.; Fasina, F.O. Expanding beyond zoonoses: The benefits of a national one health coordination mechanism to address antimicrobial resistance and other shared health threats at the human–animal–environment interface in Kenya. Rev. Sci. Tech. l’OIE 2019, 38, 155–171. [Google Scholar] [CrossRef] [PubMed]
- WHO; OIE; FAO. Quadripartite Memorandum of Understanding (MoU) Signed for a New Era of One Health Collaboration. UN Environment Program. Available online: https://www.fao.org/3/cb9403en/cb9403en.pdf (accessed on 18 January 2023).
- Defilippo, F.; Dottori, M.; Lelli, D.; Chiari, M.; Cereda, D.; Farioli, M.; Chianese, R.; Cerioli, M.P.; Faccin, F.; Canziani, S.; et al. Assessment of the Costs Related to West Nile Virus Monitoring in Lombardy Region (Italy) between 2014 and 2018. Int. J. Environ. Res. Public Health 2022, 19, 5541. [Google Scholar] [CrossRef] [PubMed]
- Cringoli, G.; Pepe, P.; Bosco, A.; Maurelli, M.P.; Baldi, L.; Ciaramella, P.; Musella, V.; Buonanno, M.L.; Capuano, F.; Corrado, F.; et al. An integrated approach to control Cystic Echinococcosis in southern Italy. Vet. Parasitol. 2021, 290, 109347. [Google Scholar] [CrossRef]
- Riccardo, F.; Bolici, F.; Fafangel, M.; Jovanovic, V.; Socan, M.; Klepac, P.; Plavsa, D.; Vasic, M.; Bella, A.; Diana, G.; et al. West Nile virus in Europe: After action reviews of preparedness and response to the 2018 transmission season in Italy, Slovenia, Serbia and Greece. Glob. Health 2020, 16, 47, Erratum in Glob. Health 2020, 16, 55. [Google Scholar] [CrossRef]
- Paternoster, G.; Babo Martins, S.; Mattivi, A.; Cagarelli, R.; Angelini, P.; Bellini, R.; Santi, A.; Galletti, G.; Pupella, S.; Marano, G.; et al. Economics of One Health: Costs and benefits of integrated West Nile virus surveillance in Emilia-Romagna. PLoS ONE 2017, 12, e0188156. [Google Scholar] [CrossRef]
- Häsler, B.; Hiby, E.; Gilbert, W.; Obeyesekere, N.; Bennani, H.; Rushton, J. A one health framework for the evaluation of rabies control programmes: A case study from Colombo City, Sri Lanka. PLoS Negl. Trop. Dis. 2014, 8, e3270. [Google Scholar] [CrossRef]
- Mindekem, R.; Lechenne, M.S.; Naissengar, K.S.; Oussiguéré, A.; Kebkiba, B.; Moto, D.D.; Alfaroukh, I.O.; Ouedraogo, L.T.; Salifou, S.; Zinsstag, J. Cost Description and Comparative Cost Efficiency of Post-Exposure Prophylaxis and Canine Mass Vaccination against Rabies in N’Djamena, Chad. Front. Vet. Sci. 2017, 4, 38. [Google Scholar] [CrossRef]
- Babo Martins, S.; Rushton, J.; Stärk, K.D. Economics of zoonoses surveillance in a ‘One Health’ context: An assessment of Campylobacter surveillance in Switzerland. Epidemiol. Infect. 2017, 145, 1148–1158. [Google Scholar] [CrossRef]
- Robbiati, C.; Milano, A.; Declich, S.; Di Domenico, K.; Mancini, L.; Pizzarelli, S.; D’Angelo, F.; Riccardo, F.; Scavia, G.; Dente, M.G. One health adoption within prevention, preparedness and response to health threats: Highlights from a scoping review. One Health 2023, 17, 100613. [Google Scholar] [CrossRef]
- Dente, M.G.; Riccardo, F.; Van Bortel, W.; Marrama, L.; Mollet, T.; Derrough, T.; Sudre, B.; Calistri, P.; Nacca, G.; Ranghiasci, A.; et al. Enhancing preparedness for arbovirus infections with a one health approach: The development and implementation of multisectoral risk assessment exercises. BioMed Res. Int. 2020, 2020, 4832360. [Google Scholar] [CrossRef] [PubMed]
- Yasobant, S.; Saxena, D.; Bruchhausen, W.; Memon, F.Z.; Falkenberg, T. Multi-sectoral prioritization of Zoonotic Diseases: One Health Perspective from Ahmedabad, India. PLoS ONE 2019, 14, e0220152. [Google Scholar] [CrossRef] [PubMed]
- WHO; OIE; FAO. Joint Risk Assessment Operational Tool (JRA OT) An Operational Tool of the Tripartite Zoonoses Guide Taking a Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries. Available online: https://apps.who.int/iris/handle/10665/340005 (accessed on 18 January 2023).
- Dente, M.G.; Riccardo, F.; Declich, S.; Milano, A.; Robbiati, C.; Agrimi, U.; Mantovani, A.; Morabito, S.; Scavia, G.; Cubadda, F.; et al. Strengthening preparedness against global health threats: A paradigm shift based on one health approaches. One Health 2022, 14, 100396. [Google Scholar] [CrossRef]
- News [Internet]. MediLabSecure. Available online: https://www.medilabsecure.com/ (accessed on 18 January 2023).
- Statistical Committee of the Republic of Armenia. Social Snapshot and Poverty in Armenia. Available online: https://www.armstat.am/file/doc/99534298.pdf (accessed on 18 January 2023).
- National Adaptation Programme. Armenia. Green Climate Fund, UNDP. Available online: https://unfccc.int/sites/default/files/resource/NAP_Armenia.pdf (accessed on 18 January 2023).
- UNDP; GEF. Third National Communication on Climate Change under the United Nations Framework Convention on Climate Change. Available online: https://unfccc.int/resource/docs/natc/armnc3.pdf (accessed on 18 January 2023).
- FAO. Agriculture Strategy of Armenia 2020–2030 Razmavarutyun_Hamarotagir_Angleren.pdf. Available online: https://unfccc.int/sites/default/files/resource/NAP_Armenia.pdf (accessed on 18 January 2023).
- Harutyunyan, T.; Hayrumyan, V. Public opinion about the health care system in Armenia: Findings from a cross-sectional telephone survey. BMC Health Serv. Res. 2020, 20, 1005. [Google Scholar] [CrossRef] [PubMed]
- Kricorian, K.; Khoshnood, K.; Chekijian, S. Hybrid warfare and public health: Conflicts in Ukraine and Nagorno-Karabakh raise the alarm. Public Health Pract. 2022, 4, 100342. [Google Scholar] [CrossRef]
- Hirschfeld, K.; de Beurs, K.; Brayfield, B.; Melkonyan, A. Ethnic Conflict as a Risk Amplifier for Resurgent P. vivax Malaria in Temperate Zones: A Case Study from the Caucasus Region. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Health System in Action. Armenia. WHO, European Observatory on Health Systems and Policies. Available online: https://apps.who.int/iris/rest/bitstreams/1463761/retrieve (accessed on 18 January 2023).
- Joint External Evaluation of IHR Core Capacities of the Republic of Armenia; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/publications/i/item/WHO-WHE-CPI-2017.14 (accessed on 18 January 2023).
- WHO; OIE. National Bridging Workshop on the International Health Regulations (IHR) and the OIE Performance of Veterinary Services (PVS) Pathway. Armenia. 2019. Available online: https://rr-europe.woah.org/wp-content/uploads/2020/05/nbw-report_arm_final2_en.pdf (accessed on 18 January 2023).
- Breen, R.W.B.; Ghazaryan, A.; Paronyan, L.; Gevorgyan, K.; Gevorgyan, H.; Shcherbakov, O.; Olival, K.J. One Health Armenia: An Assessment of One Health Operations and Capacities. EcoHealth Alliance 2023. [Google Scholar] [CrossRef]
- Agrimi, U.; Carere, M.; Cubadda, F.; Dar, O.; Declich, S.; Dente, M.G.; Farina, M.; Ihekweazy, C.; Lavazza, A.; Mancini, L.; et al. One Health—Based Conceptual Frameworks for Comprehensive and Coordinated Prevention and Preparedness Plans Addressing Global Health Threats. 2021. Available online: https://www.t20italy.org/wp-content/uploads/2021/09/TF1_PB05_LM02.pdf (accessed on 18 January 2023).
- G20—Italian Presidency [Internet]. Ministry of Economic Development. Available online: https://www.mise.gov.it/index.php/en/g20-en/g20-italian-presidency (accessed on 18 January 2023).
- Dente, M.G.; Riccardo, F.; Bolici, F.; Colella, N.A.; Jovanovic, V.; Drakulovic, M.; Vasic, M.; Mamlouk, H.; Maazaoui, L.; Bejaoui, M.; et al. Implementation of the one health approach to fight arbovirus infections in the Mediterranean and Black Sea Region: Assessing integrated surveillance in Serbia, Tunisia and Georgia. Zoonoses Public Health 2019, 66, 276–287. [Google Scholar] [CrossRef]
- WHO. Setting Priorities in Communicable Disease Surveillance. 2006. Available online: https://apps.who.int/iris/handle/10665/69332 (accessed on 18 January 2023).
- Rao, S.; Traxler, R.; Napetavaridze, T.; Asanishvili, Z.; Rukhadze, K.; Maghlakelidze, G.; Geleishvili, M.; Broladze, M.; Kokhreidze, M.; Reynolds, D.; et al. Risk factors associated with the occurrence of anthrax outbreaks in livestock in the country of Georgia: A case-control investigation 2013–2015. PLoS ONE 2019, 14, e0215228. [Google Scholar] [CrossRef]
- Shahhosseini, N.; Wong, G.; Babuadze, G.; Camp, J.V.; Ergonul, O.; Kobinger, G.P.; Chinikar, S.; Nowotny, N. Crimean-Congo hemorrhagic fever virus in Asia, Africa and Europe. Microorganisms 2021, 9, 1907. [Google Scholar] [CrossRef]
- Gevorgyan, H.; Grigoryan, G.G.; Atoyan, H.A.; Rukhkyan, M.; Hakobyan, A.; Zakaryan, H.; Aghayan, S.A. Evidence of crimean-congo haemorrhagic fever virus occurrence in ixodidae ticks of Armenia. J. Arthropod-Borne Dis. 2019, 13, 9–16. [Google Scholar]
- Blair, P.W.; Kuhn, J.H.; Pecor, D.B.; Apanaskevich, D.A.; Kortepeter, G.; Cardile, A.P.; Ramos, A.P.; Keshtkar-Jahromi, M. An emerging biothreat: Crimean-Congo hemorrhagic fever virus in southern and western Asia. Am. J. Trop. Med. Hyg. 2019, 100, 16–23. Available online: https://pubmed.ncbi.nlm.nih.gov/30652673/ (accessed on 18 January 2023). [CrossRef] [PubMed]
- Spengler, J.R.; Bergeron, É.; Rollin, P.E. Seroepidemiological studies of Crimean-Congo hemorrhagic fever virus in domestic and wild animals. PLoS Neglected Trop. Dis. 2016, 10, e0004210. [Google Scholar] [CrossRef] [PubMed]
- Commission Implementing Decision (EU) 2018/945 of 22 June 2018 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions. Off. J. Eur. Union 2018. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32018D0945&from=EN#page=50 (accessed on 18 January 2023).
- Centers for Disease Control and Prevention. What Is Anthrax? [Internet]. 2022. Available online: https://www.cdc.gov/anthrax/basics/index.html#:~:text=Anthrax%20is%20a%20serious%20infectious,animals%20or%20contaminated%20animal%20products (accessed on 3 February 2023).
- Paronyan, L.; Zardaryan, E.; Bakunts, V.; Gevorgyan, Z.; Asoyan, V.; Apresyan, H.; Hovhannisyan, A.; Palayan, K.; Bautista, C.T.; Kuchuloria, T.; et al. A retrospective chart review study to describe selected zoonotic and arboviral etiologies in hospitalized febrile patients in the Republic of Armenia. BMC Infect. Dis. 2016, 16, 445. [Google Scholar] [CrossRef]
- Apresyan, H.; Davidyants, M.; Atoyan, L.; Asoyan, V.; Mkrtchyan, A.; Hovhannisyan, A. The most common epidemiological, clinical and laboratory characteristics of patients with anthrax in Armenia. Int. J. Infect. Dis. 2016, 53, 72. [Google Scholar] [CrossRef]
- Eremenko, E.; Pechkovskii, G.; Pisarenko, S.; Ryazanova, A.; Kovalev, D.; Semenova, O.; Aksenova, L.; Timchenko, L.; Golovinskaya, T.; Bobrisheva, O.; et al. Phylogenetics of bacillus anthracis isolates from Russia and bordering countries. Infect. Genet. Evol. 2021, 92, 104890. [Google Scholar] [CrossRef]
- Ryazanova, A.G.; Skudareva, O.N.; Gerasimenko, D.K.; Logvin, F.V.; Chmerenko, D.K.; Semenova, O.V.; Aksenova, L.Y.; Eremenko, I.; Buravtseva, N.P.; Golovinskaya, T.M.; et al. Epidemiological and epizootiological situation on anthrax around the world in 2021, the forecast for 2022 in the Russian Federation. Probl. Part. Danger. Infect. 2022, 64–70. [Google Scholar] [CrossRef]
- Ryazanova, A.G.; Skudareva, O.N.; Gerasimenko, D.K.; Semenova, O.V.; Aksenova, L.Y.; Eremenko, E.I.; Buravtseva, N.P.; Golovinskaya, T.M.; Varfolomeeva, N.G.; Pechkovsky, G.A.; et al. Analysis of the situation on anthrax in 2019, the forecast for 2020. Probl. Part. Danger. Infect. 2020, 57–61. [Google Scholar] [CrossRef]
| Scope: to Facilitate OH Operationalization and Implementation for the Prevention and Preparedness for Threats at the Human–Animal–Environment Interface. | ||||||
|---|---|---|---|---|---|---|
| Targets | ||||||
| National Level | International Level | |||||
| Target 1 | Target 2 | Target 3 | Target 4 | Target 5 | Target 1 | Target 2 |
| governance | prevention and preparedness | data collection and analysis | capacity building | consolidation and evaluation of the system in place | harmonisation of plans and cross-border collaborations | harmonised capacity building |
| National legislative and procedural framework that allows/imposes mainstream OH approaches in all the prevention and preparedness strategies and allocates the necessary resources. One Health national centers. | Prevention and preparedness plans developed, implemented and monitored with an OH approach, including community empowerment strategies, for the prevention and containment of health threats | National sector-driven database interoperable and accessible to all the institutions/sectors involved in the One Health team | National training plan on OH strategies agreed upon between institutions and integrated into the relevant national plans | Evaluation plans to assess the effectiveness of OH in reducing the risks of potential epidemics (prevention); supporting the early identification of epidemic risks (alerting); and contributing to a reduction in impact (mitigation) | International Framework enabling harmonized integration of OH strategies in all relevant regulations and communications | International training plans and tools aimed at facilitating OH training at national and cross-country levels |
| Priorities for Action | ||||||
| National level | International level | |||||
| Priority 1 | Priority 2 | Priority 3 | Priority 4 | Priority 5 | Priority 1 | Priority 2 |
| governance | prevention and preparedness | data collection and analysis | capacity building | consolidation and evaluation of the system in place | harmonisation of plans and cross-border collaborations | harmonised capacity building |
| Establishing a national multisectoral and multistakeholder team to set principles, rules and procedures to allow operationalization of OH strategies Assessing the opportunity and benefits of setting up an OH national center Enacting laws and identifying resources for OH operationalization | Connecting OH strategies to prevention and preparedness plans by establishing a multisectoral team (OH team) in charge of the development, implementation and monitoring of plans | Identification of national priority areas to be monitored and related monitoring indicators/metrics Verifying available sources of information and data Development of an integrated and interoperable database connected with early warning and surveillance systems | Development of training curricula on OH prevention and preparedness Training of staff involved in activities including OH strategies Piloting and exercising | Identifying monitoring and impact indicators Assessing level of implementation of OH indications in prevention and pandemic plans Assessing added value of OH in prevention and preparedness | Developing and updating guidance and regulations to integrate OH strategies in prevention and preparedness plans and international early warning systems Identification of OH preparedness indicators/metrics in collaboration with national OH teams Establishing Quadripartite-collaborating centers at national OH centers Facilitating networking opportunities between OH national centers | Integration of OH principles in international training for preparedness and in tools aimed at assessing the level of capacities Promoting harmonized and multicounty exercises |
| Preparatory phase—Involved stakeholders: Armenian context experts from the NCDC and the Ministry of Economy | |
| Methods/Tools | Outcomes |
| Desk review | Preliminary picture of the OH system in Armenia |
| Analysis of outcomes provided by previous assessments (e.g., WHO JEE of IHR Core Capacities in 2016 and the National Bridging Workshop on IHR and PVS Pathway in 2019) | |
| Stakeholders mapping | |
| Consultation with Armenian context experts | List of priority zoonotic and vector-borne pathogens |
| Identification of criteria and indicators for the prioritization | |
| Workshops—Involved stakeholders: Experts from all the institutions identified with the stakeholder mapping | |
| Methods/Tools | Outcomes |
| 1st workshop: prioritization | |
| Consensus on criteria and indicators for the prioritization of zoonotic and vector-borne pathogens | Priority pathogens to be addressed during the study |
| Prioritization as per set criteria and indicators | |
| 2nd workshop: framing the OH system | |
| Description of the surveillance systems for the selected pathogens | Status of integration between sectors |
| Analysis of the integration of OH approaches in prevention, surveillance, and preparedness plans of the selected pathogens through the OHCF | Strategies and procedures in place and areas of improvement |
| 3rd workshop: strengthening the OH system | |
| Discussion about the available opportunities and their feasibility for the enhancement of the OH system in Armenia | Priority actions to be implemented and their perceived feasibility |
| Arbovirus (Focus of the MLS Project) | Other Identified Pathogens | ||
|---|---|---|---|
| Virus | Virus | Parasites | Bacteria |
| Crimean–Congo hemorrhagic fever | Tick-borne encephalitis | Leishmaniosis | Anthrax |
| West Nile fever | |||
| Rift Valley fever | Rabies | Dirofilariasis | Brucellosis |
| # of Representatives | Institution |
|---|---|
| 1 | National Center for Disease Control and Prevention/Ministry of Health—Direction |
| 1 | National Center for Disease Control and Prevention/Ministry of Health—Zoonotic and Parasitic Diseases Epidemiology Department |
| 2 | National Center for Disease Control and Prevention/Ministry of Health—Reference Virology Laboratory |
| 1 | National Center for Disease Control and Prevention/Ministry of Health—Laboratory of Episootology, Ectoparasitology and Entomology |
| 1 | Regional branch of National Center for Disease Control and Prevention in Shirak Province |
| 6 | Veterinary Inspectorate, Food Safety Inspection/Ministry of Economy |
| 1 | Risk Assessment Research Center/Ministry of Economy |
| 1 | Reference Laboratory of Especially Dangerous Pathogens, Republican Veterinary and Phytosanitary Laboratory Services Center |
| 1 | Incident Management Support Officer, WHO Armenia Country Office |
| 2 | CH2M [Engineering company named from the initials of its four founders. In 2017, CH2M became part of Jacobs Engineering Group Inc. (Welcome to Jacobs|Jacobs)]—Jacobs Armenia Branch Office |
| 1 | Center for Ecological-Noosphere Studies, National Academy of Sciences |
| 1 | Ministry of Environment |
| Questions | CCHFV | RVFV | WNV | Do Not Know | Total |
|---|---|---|---|---|---|
| Select pathogen/s which have activated a recent response action to contain a potential outbreak of this disease | 0 | 0 | 0 | 4 | 4 |
| Select the pathogen/s for which an OH preparedness/surveillance plan is available in Armenia | 0 | 0 | 0 | 5 | 5 |
| Select the pathogen/s which have been detected or caused outbreaks/epidemics in the past 10 years in Armenia | 0 | 0 | 0 | 0 | 0 |
| Select the pathogen/s that can affect food safety or/and food security | 3 | 1 | 4 | 3 | 11 |
| Select the pathogen/s which can benefit the most from the integration of environmental and climatic data in its surveillance | 3 | 2 | 4 | 1 | 10 |
| Select the pathogen/s which can benefit the most from integration of OH approach in preparedness/surveillance/response in Armenia | 7 | 1 | 4 | 1 | 13 |
| Select the pathogen/s which can have a big impact on economic and social aspects in case of outbreak in Armenia | 7 | 5 | 6 | 1 | 19 |
| Select the pathogen/s that have been detected in a new location or population (human or animal) in the country or neighboring countries in the past 10 years | 5 | 0 | 3 | 0 | 8 |
| Select the pathogen/s whose animal host (domestic or wild) is in close proximity to humans in Armenia | 4 | 2 | 2 | 2 | 10 |
| Select the pathogen/s whose related vector/s’ presence and abundance are increasing in Armenia due to anthropogenic, climatic and environmental factors | 5 | 1 | 2 | 3 | 11 |
| Select the pathogen/s with an integrated (human, veterinarian, environmental) data collection and analysis system in Armenia | 1 | 1 | 1 | 2 | 5 |
| Total | 35 | 13 | 26 | 22 | 96 |
| Questions | Anthrax | Brucellosis | Dirofilariosis | Leishmaniosis | Rabies | TBE | Do Not Know | Total |
|---|---|---|---|---|---|---|---|---|
| Select pathogen/s which have activated a recent response action to contain a potential outbreak of this disease | 5 | 3 | 0 | 1 | 1 | 0 | 0 | 10 |
| Select the pathogen/s for which an OH preparedness/surveillance plan is available in Armenia | 1 | 2 | 0 | 1 | 1 | 1 | 2 | 8 |
| Select the pathogen/s which have been detected or caused outbreaks/epidemics in the past 10 years in Armenia | 3 | 3 | 1 | 1 | 1 | 0 | 1 | 10 |
| Select the pathogen/s that can affect food safety or/and food security | 8 | 8 | 0 | 0 | 1 | 1 | 0 | 18 |
| Select the pathogen/s which can benefit the most from the integration of environmental and climatic data in its surveillance | 2 | 1 | 2 | 3 | 0 | 2 | 0 | 10 |
| Select the pathogen/s that can benefit the most from integration of OH approach in preparedness/surveillance/response in Armenia | 6 | 6 | 2 | 3 | 3 | 1 | 0 | 21 |
| Select the pathogen/s which can have a big impact on economic and social aspects in case of outbreak in Armenia | 6 | 6 | 0 | 0 | 2 | 1 | 0 | 15 |
| Select the pathogen/s that have been detected in a new location or population (human or animal) in the country or neighboring countries in the past 10 years | 2 | 1 | 1 | 3 | 1 | 1 | 1 | 10 |
| Select the pathogen/s whose animal host (domestic or wild) is in close proximity to humans in Armenia | 5 | 5 | 4 | 4 | 1 | 1 | 20 | |
| Select the pathogen/s whose related vector/s’ presence and abundance are increasing in Armenia due to anthropogenic, climatic and environmental factors | 1 | 3 | 2 | 5 | 0 | 1 | 0 | 12 |
| Select the pathogen/s with an integrated (human, veterinarian, environmental) data collection and analysis system in Armenia | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| Total | 39 | 38 | 8 | 21 | 14 | 9 | 7 | 136 |
| Identified Actions towards OH Integration in Armenia | ||
|---|---|---|
| Targets as Per OHCF | Areas to Be Addressed | Actions and Procedures in Place |
| Governance | National procedures and mechanisms enabling intersectoral activities are not fully in place. | Under the International Health Regulations (IHR-2005), there are two multisectoral groups: 1. The high-level intersectoral steering committee. 2. The expert group under the MoH. Under the guidance of WHO, NCDC is developing an OH framework for the implementation of the tripartite guide, starting with legislation aspects. |
| Prevention and preparedness | Specific preparedness plans for pathogens are not available, only a generic preparedness one. Prevention and preparedness plans with an OH approach were reportedly under development but are not yet available. | After a WHO workshop (March 2022) on the control and prevention of zoonotic diseases, an OH national plan was developed and its operationalization was under discussion among the relevant stakeholders during the assessment. |
| Data collection and analysis | Data are not shared regularly between sectors. | The Electronic Diseases Surveillance System (EDSS) for human and animal infectious diseases has been developed but not operationalized at the time of the assessment. |
| Capacity building | A specific intersectoral training curriculum on OH is not available. | In 2021, training was organized by the NCDC, with WHO support, for different disciplines and sectors. US Defense Threat Reduction Agency (DTRA) supports frontline field epidemiology training with epidemiologists from public and animal health. In March 2022, the WHO country office implemented a training workshop focused on the operationalization of the tripartite action plan. |
| Consolidation and evaluation of the system in place | Specific evaluation/s of the national OH system are not available. | Assessments of collaboration capacities were implemented: the WHO Joint External Evaluation in 2016 [34], the National Bridging Workshop on the International Health Regulations (IHR) and the WOAH Performance of Veterinary Services (PVS) Pathway in 2019 [35]. |
| National actions supporting international harmonization and cross-border collaboration | Cross-border collaborations. | MoH has a Memorandum of Understanding with Iran and Georgia for information sharing. |
| Areas of Improvement | CCHFV Prevention and Preparedness | Feasibility Score |
|---|---|---|
| Human and animal surveillance | Cross-sectional serological surveys on domestic animals (especially ruminants) to define areas exposed to virus infections | 4.5 |
| Surveillance of tick infestations in domestic animals in at-risk areas | 4 | |
| Vector mapping | Consolidated maps of the distribution of ticks in the country and identification of priority areas to be monitored | 4.5 |
| Risk assessment | Serological surveys on at-risk groups to define areas exposed to the virus | 4.8 |
| Collection and analysis of data to monitor at-risk groups, areas and events | 4.3 |
| Areas of Improvement | Anthrax Prevention and Preparedness | Feasibility Score |
|---|---|---|
| Identification of drivers | Studies on drivers of anthrax in order to guide prevention actions | 4.5 |
| Community engagement | Communitarian vets more involved in preparedness and prevention actions | 4.5 |
| Intersectorality | Feasibility Score | |
|---|---|---|
| Governance | Leveraging on WHO IHR-2005 requirements to enhance intersectoral activities at national level | 3.8 |
| Preparedness plans with an OH approach | 4 | |
| Multisectoral training curriculum on One Health | 3.8 | |
| OH operationalization (enactment of national laws and procedures) | 3.8 | |
| Include climate and environmental data and identify trends and drivers | 3.8 | |
| Prioritize training on the Electronic Diseases Surveillance System (EDSS) for all the sectors involved at national and peripheral levels | 3.8 | |
| Education and awareness campaigns for communities involving all sectors | 3.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Milano, A.; Robbiati, C.; Declich, S.; Calistri, P.; Pediconi, O.; Amato, L.; Paronyan, L.; Avetisyan, L.; Manucharyan, A.; Avetisyan, G.; et al. Assessing the Adoption of One Health Approaches in National Plans to Combat Health Threats: The Pilot of a One Health Conceptual Framework in Armenia. Trop. Med. Infect. Dis. 2024, 9, 22. https://doi.org/10.3390/tropicalmed9010022
Milano A, Robbiati C, Declich S, Calistri P, Pediconi O, Amato L, Paronyan L, Avetisyan L, Manucharyan A, Avetisyan G, et al. Assessing the Adoption of One Health Approaches in National Plans to Combat Health Threats: The Pilot of a One Health Conceptual Framework in Armenia. Tropical Medicine and Infectious Disease. 2024; 9(1):22. https://doi.org/10.3390/tropicalmed9010022
Chicago/Turabian StyleMilano, Alessia, Claudia Robbiati, Silvia Declich, Paolo Calistri, Ombretta Pediconi, Laura Amato, Lusine Paronyan, Lilit Avetisyan, Arsen Manucharyan, Georgi Avetisyan, and et al. 2024. "Assessing the Adoption of One Health Approaches in National Plans to Combat Health Threats: The Pilot of a One Health Conceptual Framework in Armenia" Tropical Medicine and Infectious Disease 9, no. 1: 22. https://doi.org/10.3390/tropicalmed9010022
APA StyleMilano, A., Robbiati, C., Declich, S., Calistri, P., Pediconi, O., Amato, L., Paronyan, L., Avetisyan, L., Manucharyan, A., Avetisyan, G., Yesayan, T., Gevorgyan, A., Markosyan, T., & Dente, M. G. (2024). Assessing the Adoption of One Health Approaches in National Plans to Combat Health Threats: The Pilot of a One Health Conceptual Framework in Armenia. Tropical Medicine and Infectious Disease, 9(1), 22. https://doi.org/10.3390/tropicalmed9010022







