The Trend, Characteristics and Treatment Outcomes in Patients with Tuberculosis Undergoing Thoracic Surgery in the Kyrgyz Republic between 2017 and 2021
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.2.1. General Setting
2.2.2. National TB Epidemiology
2.2.3. National TB Control
2.2.4. Surgery for TB in the Kyrgyz Republic
2.3. Study Population
2.4. Data Variables, Sources of Data and Data Collection
2.4.1. For Objective 1 (Trend in TB Cases and TB Surgeries between 2017 and 2021)
2.4.2. For Objective 2 (TB Patients Who Received Surgical Treatment in 2021)
2.5. Analysis and Statistics
3. Results
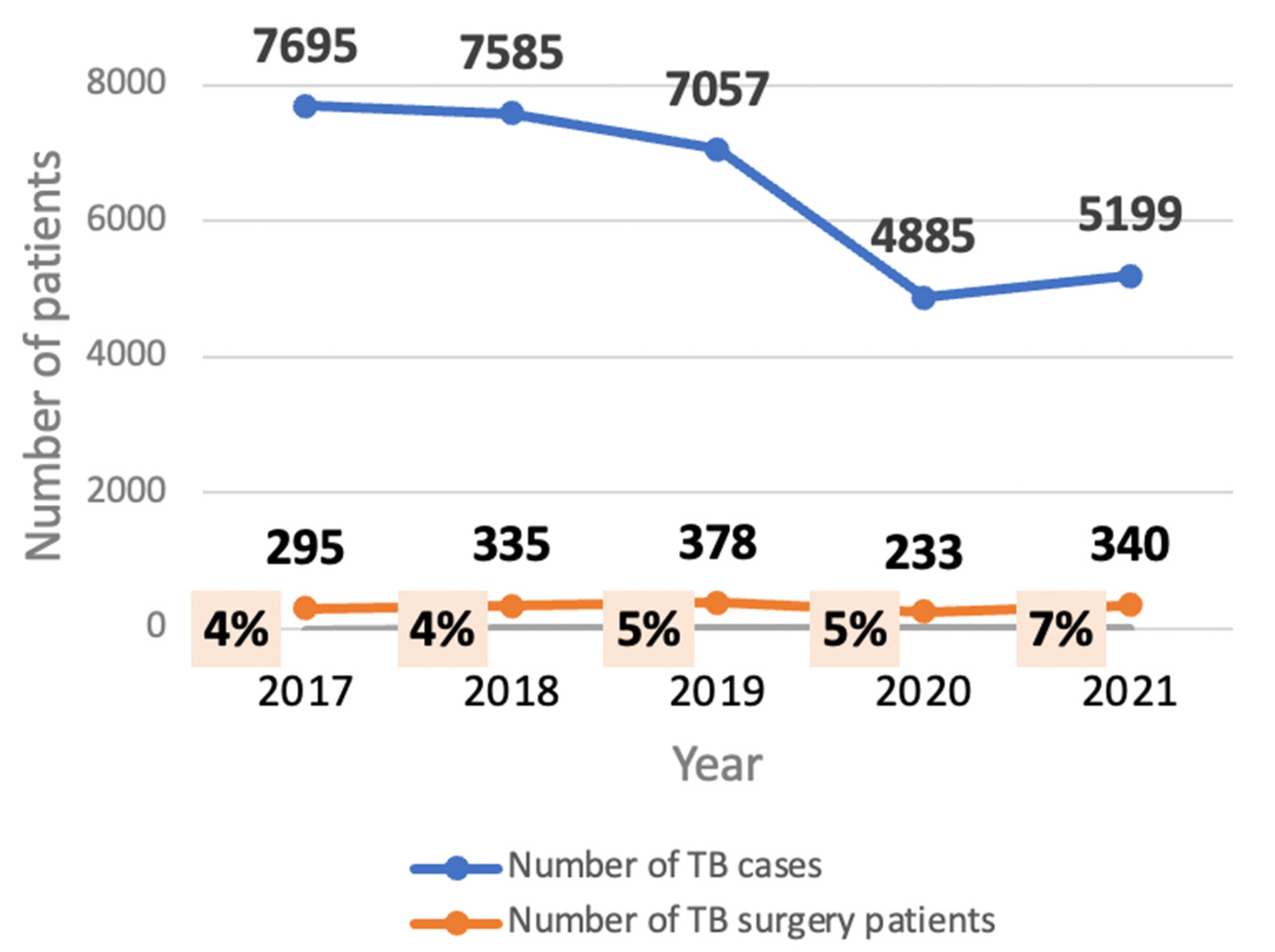
3.1. The Trend in TB Cases and TB Surgery in the Kyrgyz Republic, 2017–2021
3.2. Characteristics of TB Patients Undergoing Thoracic Surgery in 2021
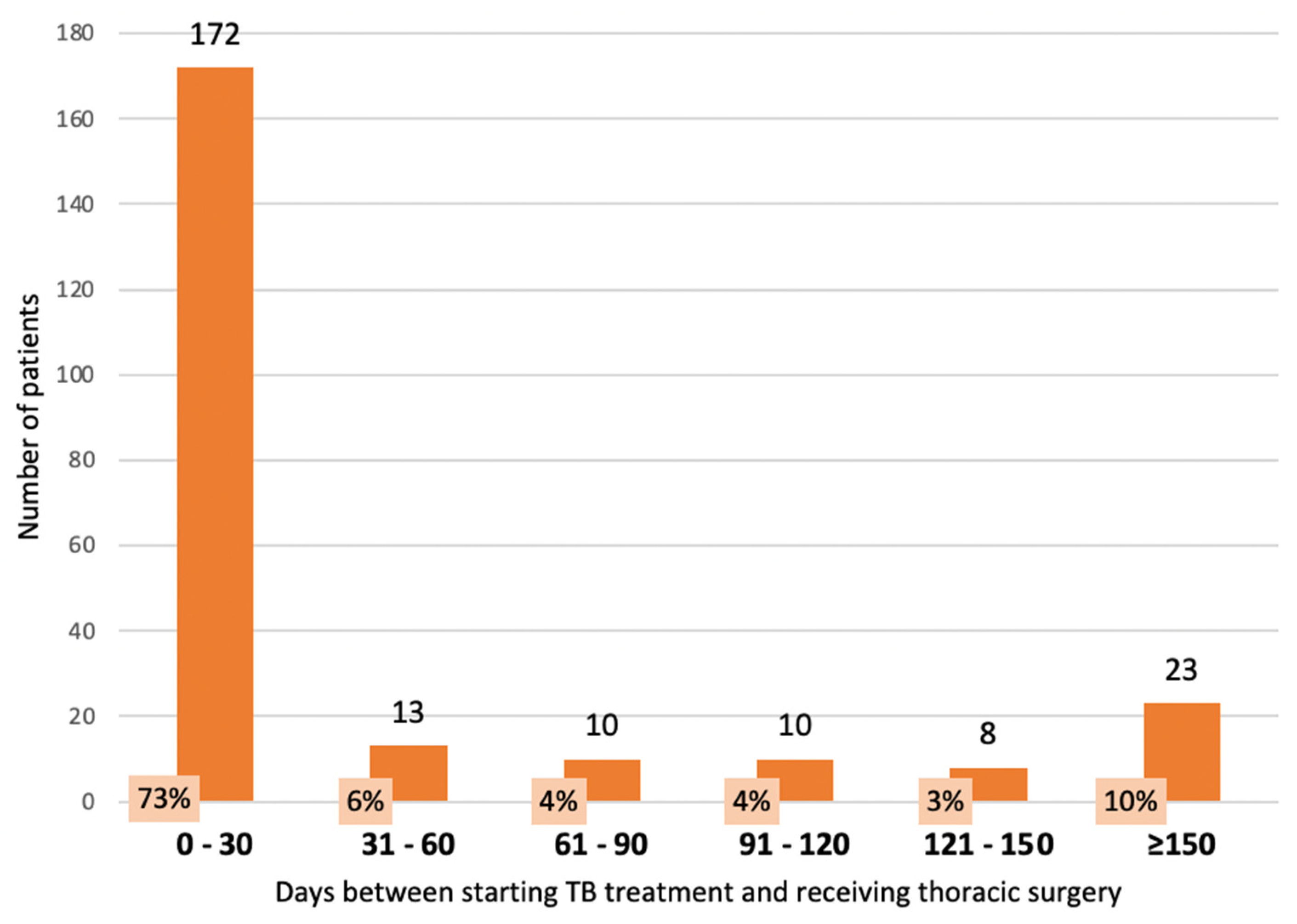
3.3. Timing of TB Treatment with Respect to Thoracic Surgery in TB Patients in 2021
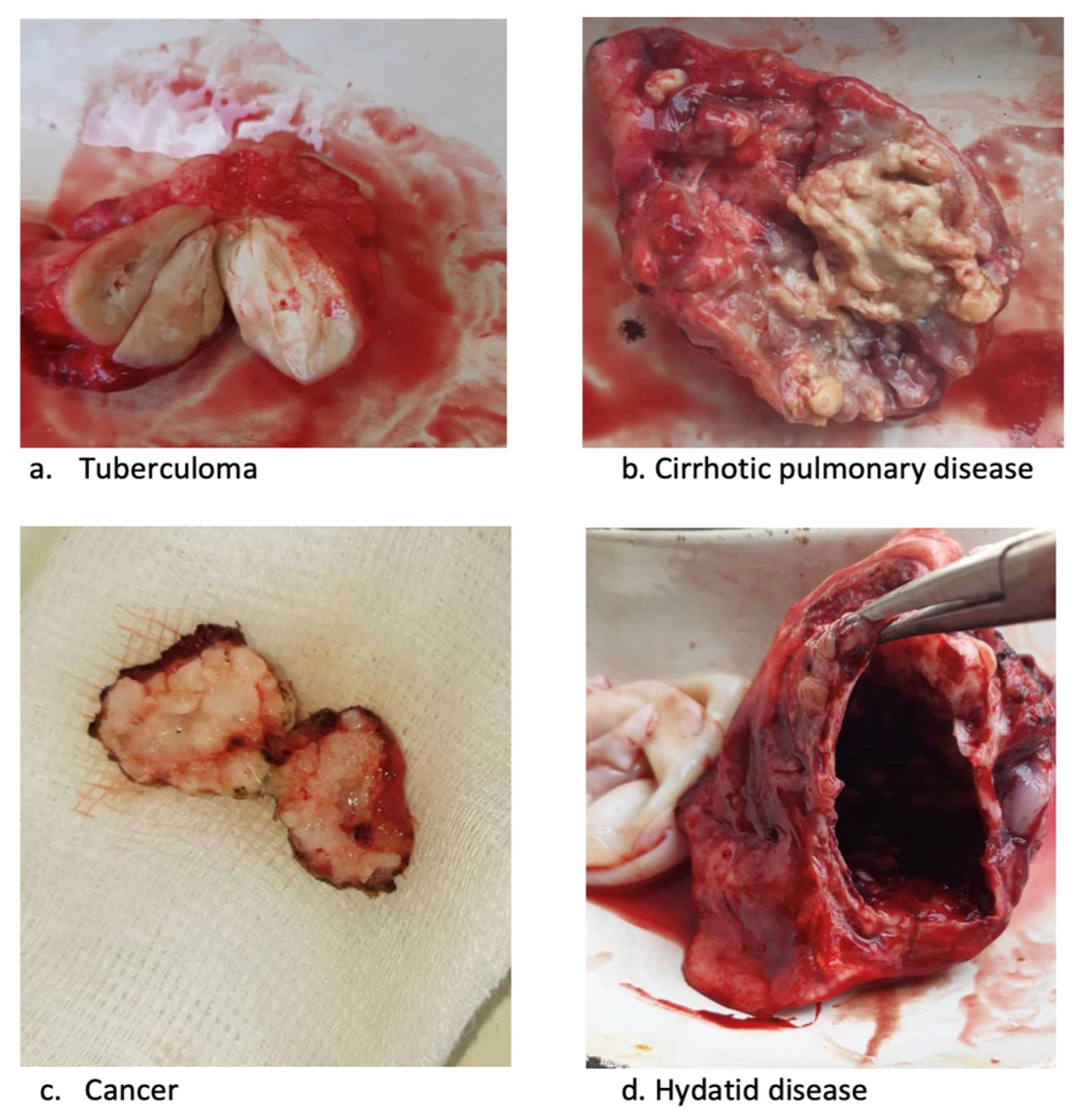
3.4. Details of Thoracic Surgery in TB Patients in 2021
3.5. TB Treatment Outcomes and Factors Associated with Treatment Success
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Open-Access Statement and Disclaimer
References
- World Health Organization. Annual Global TB Report of WHO; WHO: Geneva, Switzerland, 2022; Volume 8, pp. 1–68. [Google Scholar]
- Subotic, D.; Yablonskiy, P.; Sulis, G.; Cordos, I.; Petrov, D.; Centis, R.; D’Ambrosio, L.; Sotgiu, G.; Migliori, G.B. Surgery and Pleuro-Pulmonary Tuberculosis: A Scientific Literature Review. J. Thorac. Dis. 2016, 8, E474–E485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garzon, A.A.; Gourin, A. Surgical Management of Massive Hemoptysis. A Ten-Year Experience. Ann. Surg. 1978, 187, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.C.; Khan, M.S.; Martin, L.J.; Allen, V.; Moore, D.A.J.; Fielding, K.; Grandjean, L.; Amini, A.; Buchanan, R.; Krutikov, M. The Effect of Surgery on the Outcome of Treatment for Multidrug-Resistant Tuberculosis: A Systematic Review and Meta-Analysis. BMC Infect. Dis. 2016, 16, 262. [Google Scholar] [CrossRef] [Green Version]
- Yablonskii, P.K.; Kudriashov, G.G.; Avetisyan, A.O. Surgical Resection in the Treatment of Pulmonary Tuberculosis. Thorac. Surg. Clin. 2019, 29, 37–46. [Google Scholar] [CrossRef]
- Vashakidze, S.; Gogishvili, S.; Nikolaishvili, K.; Dzidzikashvili, N.; Tukvadze, N.; Blumberg, H.M.; Kempker, R.R. Favorable Outcomes for Multidrug and Extensively Drug Resistant Tuberculosis Patients Undergoing Surgery. Ann. Thorac. Surg. 2013, 95, 1892–1898. [Google Scholar] [CrossRef] [Green Version]
- Vashakidze, S.; Despuig, A.; Gogishvili, S.; Nikolaishvili, K.; Shubladze, N.; Avaliani, Z.; Tukvadze, N.; Casals, M.; Caylà, J.A.; Cardona, P.J.; et al. Retrospective Study of Clinical and Lesion Characteristics of Patients Undergoing Surgical Treatment for Pulmonary Tuberculosis in Georgia. Int. J. Infect. Dis. 2017, 56, 200–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riskiyev, A.; Ciobanu, A.; Hovhannesyan, A.; Akopyan, K.; Gadoev, J.; Parpieva, N. Characteristics and Treatment Outcomes of Patients with Tuberculosis Receiving Adjunctive Surgery in Uzbekistan. Int. J. Environ. Res. Public Health 2021, 18, 6541. [Google Scholar] [CrossRef]
- Dadu, A.; Hovhannesyan, A.; Ahmedov, S.; van der Werf, M.J.; Dara, M. Drug-Resistant Tuberculosis in Eastern Europe and Central Asia: A Time-Series Analysis of Routine Surveillance Data. Lancet Infect. Dis. 2020, 20, 250–258. [Google Scholar] [CrossRef]
- Data for Lower Middle Income, Kyrgyz Republic|Data. Available online: https://data.worldbank.org/?locations=XN-KG (accessed on 6 May 2023).
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis Module 4: Treatment Drug-Susceptible Tuberculosis Treatment; WHO: Geneva, Switzerland, 2022; pp. 1–72. [Google Scholar]
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis. Module 4: Treatment—Drug-Resistant Tuberculosis Treatment; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Zhdanova, E.; Goncharova, O.; Davtyan, H.; Alaverdyan, S.; Sargsyan, A.; Harries, A.D.; Maykanaev, B. 9-12 Months Short Treatment for Patients with MDR-TB Increases Treatment Success in Kyrgyzstan. J. Infect. Dev. Ctries. 2021, 15, 66S–74S. [Google Scholar] [CrossRef]
- Definitions and Reporting Framework for Tuberculosis—2013 Revision: Updated December 2014 and January 2020. Available online: https://www.who.int/publications/i/item/9789241505345 (accessed on 6 May 2023).
- Mbithi, I.; Thekkur, P.; Chakaya, J.M.; Onyango, E.; Owiti, P.; Njeri, N.C.; Kumar, A.M.V.; Satyanarayana, S.; Shewade, H.D.; Khogali, M.; et al. Assessing the Real-Time Impact of COVID-19 on TB and HIV Services: The Experience and Response from Selected Health Facilities in Nairobi, Kenya. Trop. Med. Infect. Dis. 2021, 6, 74. [Google Scholar] [CrossRef]
- Thekkur, P.; Tweya, H.; Phiri, S.; Mpunga, J.; Kalua, T.; Kumar, A.M.V.; Satyanarayana, S.; Shewade, H.D.; Khogali, M.; Zachariah, R.; et al. Assessing the Impact of COVID-19 on TB and HIV Programme Services in Selected Health Facilities in Lilongwe, Malawi: Operational Research in Real Time. Trop. Med. Infect. Dis. 2021, 6, 81. [Google Scholar] [CrossRef]
- Thekkur, P.; Takarinda, K.C.; Timire, C.; Sandy, C.; Apollo, T.; Kumar, A.M.V.; Satyanarayana, S.; Shewade, H.D.; Khogali, M.; Zachariah, R.; et al. Operational Research to Assess the Real-Time Impact of COVID-19 on TB and HIV Services: The Experience and Response from Health Facilities in Harare, Zimbabwe. Trop. Med. Infect. Dis. 2021, 6, 94. [Google Scholar] [CrossRef]
- Calligaro, G.L.; Moodley, L.; Symons, G.; Dheda, K. The Medical and Surgical Treatment of Drug-Resistant Tuberculosis. J. Thorac. Dis. 2014, 6, 186–195. [Google Scholar] [CrossRef]
- Dewan, R.K.; Pezzella, A.T. Surgical Aspects of Pulmonary Tuberculosis: An Update. Asian Cardiovasc. Thorac. Ann. 2016, 24, 835–846. [Google Scholar] [CrossRef]
- Molnar, T.F. Tuberculosis: Mother of Thoracic Surgery Then and Now, Past and Prospectives: A Review. J. Thorac. Dis. 2018, 10, S2628–S2642. [Google Scholar] [CrossRef]
- Clinical Diagnosis of Smear-Negative Pulmonary Tuberculosis: An Audit of Diagnostic Practice in Hospitals in Malawi. Available online: https://pubmed.ncbi.nlm.nih.gov/11769773/ (accessed on 6 May 2023).
- Kang, M.W.; Kim, H.K.; Choi, Y.S.; Kim, K.; Shim, Y.M.; Koh, W.J.; Kim, J. Surgical Treatment for Multidrug-Resistant and Extensive Drug-Resistant Tuberculosis. Ann. Thorac. Surg. 2010, 89, 1597–1602. [Google Scholar] [CrossRef]
- Wang, L.; Xia, F.; Li, F.; Qian, X.; Zhu, Y.; Chen, H.; Bian, A.; Wang, J.; Zhang, M.; Li, H.; et al. Pulmonary Resection in the Treatment of Multidrug-Resistant Tuberculosis: A Case Series. Medicine 2017, 96, e9109. [Google Scholar] [CrossRef] [PubMed]
- Roh, H.F.; Kim, J.; HyukNam, S.; Kim, J.M. Pulmonary Resection for Patients with Multidrug-Resistant Tuberculosis Based on Survival Outcomes: A Systematic Review and Meta-Analysis. Eur. J. Cardiothorac. Surg. 2017, 52, 673–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giller, D.B.; Giller, B.D.; Giller, G.V.; Shcherbakova, G.V.; Bizhanov, A.B.; Enilenis, I.I.; Glotov, A.A. Treatment of Pulmonary Tuberculosis: Past and Present. Eur. J. Cardiothorac. Surg. 2018, 53, 967–972. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, H.B.; Jiang, R.H.; Li, L. Pulmonary Resection for Patients with Multidrug-Resistant Tuberculosis: Systematic Review and Meta-Analysis. J. Antimicrob. Chemother. 2011, 66, 1687–1695. [Google Scholar] [CrossRef] [PubMed]
- Fox, G.J.; Mitnick, C.D.; Benedetti, A.; Chan, E.D.; Becerra, M.; Chiang, C.Y.; Keshavjee, S.; Koh, W.J.; Shiraishi, Y.; Viiklepp, P.; et al. Surgery as an Adjunctive Treatment for Multidrug-Resistant Tuberculosis: An Individual Patient Data Metaanalysis. Clin. Infect. Dis. 2016, 62, 887–895. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, E.Y.; Arrazola, R.A.; Mathema, B.; Ahluwalia, I.B.; Mase, S.R. The Impact of Smoking on Tuberculosis Treatment Outcomes: A Meta-Analysis. Int. J. Tuberc. Lung Dis. 2020, 24, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Ragan, E.J.; Kleinman, M.B.; Sweigart, B.; Gnatienko, N.; Parry, C.D.; Horsburgh, C.R.; LaValley, M.P.; Myers, B.; Jacobson, K.R. The Impact of Alcohol Use on Tuberculosis Treatment Outcomes: A Systematic Review and Meta-Analysis. Int. J. Tuberc. Lung Dis. 2020, 24, 73–82. [Google Scholar] [CrossRef]
- Outcome of Patients with Tuberculosis Who Transfer between Reporting Units in Malawi. Available online: https://pubmed.ncbi.nlm.nih.gov/12150477/ (accessed on 6 May 2023).
- Tang, J.; Tang, Z.; Feng, C.; Tang, Q. Efficacy and Safety of Video-Assisted Thoracoscopic Surgery for Pulmonary TB. Int. J. Tuberc. Lung Dis. 2023, 27, 387–394. [Google Scholar] [CrossRef]
| Category | Variable | Number | (%) |
|---|---|---|---|
| Total | Total | 264 | |
| Gender | Male | 161 | (61) |
| Female | 103 | (39) | |
| Age in years | 0–18 | 16 | (6) |
| 19–39 | 163 | (62) | |
| 40–59 | 54 | (20) | |
| ≥60 | 21 | (8) | |
| Not recorded | 10 | (4) | |
| Alcohol use—self-reported | Yes | 20 | (8) |
| No | 227 | (86) | |
| Not recorded | 17 | (6) | |
| Smoking status—self-reported | Yes | 20 | (8) |
| No | 232 | (88) | |
| Not recorded | 12 | (4) | |
| Migration status | Internal/cross-border A | 14 | (5) |
| Not migrant | 250 | (95) | |
| Body mass index (BMI) | Undernutrition (BMI < 18.5) | 28 | (11) |
| Normal (BMI 18.5–24.9) | 139 | (53) | |
| Overweight (BMI 25.0–29.9) | 36 | (14) | |
| Obese (BMI ≥ 30.0) | 10 | (4) | |
| Not recorded | 51 | (18) | |
| HIV status | Positive | 0 | - |
| Negative | 247 | (94) | |
| Not recorded | 17 | (6) | |
| Hepatitis B status | Positive serology | 2 | (1) |
| Negative serology | 238 | (90) | |
| Not recorded | 24 | (9) | |
| Hepatitis C status | Positive serology | 13 | (5) |
| Negative serology | 228 | (86) | |
| Not recorded | 23 | (9) | |
| Category of TB | New | 161 | (61) |
| Previously treated | 103 | (39) | |
| Bacteriological status | Bacteriologically confirmed | 55 | (21) |
| Clinically diagnosed | 209 | (79) | |
| Drug susceptible status A | Susceptible | 26 | (47) |
| Resistant | 29 | (53) | |
| Type of drug resistance B | Isoniazid monoresistance | 4 | (14) |
| Polyresistance | 2 | (7) | |
| RR/MDR | 20 | (69) | |
| Pre-XDR/XDR | 3 | (10) | |
| Disease location | Left unilateral | 105 | (40) |
| Right unilateral | 132 | (50) | |
| Bilateral | 27 | (10) |
| Category | Variable | Number | (%) |
|---|---|---|---|
| Total | Total | 264 | |
| Presenting indications for surgery | Tuberculoma | 85 | (32) |
| Pleural exudate | 82 | (31) | |
| Pleural empyema | 35 | (13) | |
| Cirrhotic pulmonary/pleural disease | 22 | (9) | |
| Fibro-cavitary/cavernous pulmonary | 19 | (7) | |
| Haemoptysis | 14 | (5) | |
| Persistent bacterial expectoration | 5 | (2) | |
| Caseous pneumonia | 2 | (1) | |
| Type of surgical procedure A | Radical | 179 | (68) |
| Minimally invasive surgery | 82 | (31) | |
| Extra-pleural thoracoplasty | 3 | (1) | |
| Number of surgical operations | 1 | 252 | (95) |
| 2 | 11 | (4) | |
| 3 | 1 | (1) | |
| Post-operative complications B | Yes | 21 | (8) |
| No | 243 | (92) | |
| Diagnosis after surgery | TB only | 189 | (72) |
| TB and non-TB together | 12 | (5) | |
| Non-TB only | 63 | (23) | |
| Non-TB only C | Lung cancer | 15 | (24) |
| Hydatid disease of the lung | 6 | (10) | |
| Miscellaneous D | 42 | (66) | |
| Surgical outcome | Discharged | 263 | (99) |
| Died | 1 | (1) | |
| Discharge status | Good outcome after surgery | 260 | (99) |
| No improvement after surgery | 3 | (1) |
| Category | Variable | Number | (%) |
|---|---|---|---|
| Confirmed TB | 201 | ||
| Treatment outcomes | Treatment success | 163 | (81) |
| Died | 1 | (<1) | |
| Lost to follow-up | 5 | (3) | |
| Failed treatment | 4 | (2) | |
| Not evaluated | 28 | (14) | |
| Category | Variable | Confirmed TB Patients | Treatment Success | RR | (95% CI) | p-Value | |
|---|---|---|---|---|---|---|---|
| n | N | (%) | |||||
| Total | 201 | 163 | (81) | ||||
| Gender | Male | 130 | 107 | (82) | 1.04 | (0.9–1.3) | 0.55 |
| Female | 71 | 56 | (79) | ref | |||
| Age group years A | Age < 60 | 185 | 150 | (81) | 1.22 | (0.8–1.9) | 0.50 |
| Age ≥ 60 | 9 | 6 | (67) | ref | |||
| Alcohol use B | Yes | 15 | 13 | (87) | 1.08 | (0.9–1.3) | 0.85 |
| No | 173 | 139 | (80) | ref | |||
| Smoking status C | Yes | 17 | 13 | (76) | 0.94 | (0.7–1.2) | 0.85 |
| No | 175 | 142 | (81) | ref | |||
| Migrant status | Yes | 9 | 7 | (78) | 0.96 | (0.7–1.4) | 0.99 |
| No | 192 | 156 | (81) | ref | |||
| Body Mass Index (BMI) D | Undernutrition (BMI < 18.5) | 22 | 20 | (91) | 1.11 | (0.9–1.3) | 0.30 |
| Normal (BMI 18.5–24.9) | 105 | 86 | (82) | ref | |||
| Overweight (BMI 25.0–29.9) | 26 | 19 | (73) | 0.89 | (0.7–1.1) | 0.31 | |
| Obese (BMI ≥ 30.0) | 6 | 5 | (83) | 1.02 | (0.7–1.5) | 0.99 | |
| Hepatitis C status E | Hepatitis C-positive | 12 | 9 | (75) | 0.92 | (0.7–1.3) | 0.79 |
| Hepatitis C-negative | 175 | 143 | (82) | ref | |||
| Category of TB | New TB | 104 | 83 | (80) | 0.97 | (0.8–1.1) | 0.63 |
| Previously treated TB | 97 | 80 | (82) | ref | |||
| Bacteriological status | Bacteriological confirmed | 51 | 39 | (76) | ref | ||
| Clinically diagnosed | 150 | 124 | (83) | 1.08 | (0.9–1.3) | 0.33 | |
| Drug susceptible status | Drug susceptible | 24 | 17 | (71) | ref | ||
| Drug resistant | 27 | 22 | (81) | 1.15 | (0.8–1.6) | 0.57 | |
| Timing of anti-TB treatment | <2 months before surgery | 132 | 102 | (77) | ref | ||
| ≥2 months before surgery | 51 | 44 | (86) | 1.12 | (0.9–1.3) | 0.17 | |
| Before surgery | 183 | 146 | (78) | ref | |||
| After surgery | 18 | 17 | (94) | 1.18 | (1.0–1.4) | 0.22 | |
| Presenting surgical indications | Tuberculoma | 72 | 68 | (94) | 1.69 | (1.3–2.2) | <0.001 |
| Pleural exudate | 43 | 24 | (56) | ref | |||
| Pleural empyema | 27 | 20 | (74) | 1.33 | (0.9–1.9) | 0.12 | |
| Cirrhotic pulmonary/pleural | 22 | 22 | (100) | 1.75 | (1.3–2.3) | <0.001 | |
| Fibro-cavitary pulmonary | 18 | 14 | (78) | 1.39 | (0.9–2.0) | 0.18 | |
| Haemoptysis | 12 | 12 | (100) | 1.72 | (1.3–2.3) | 0.01 | |
| Persistent expectoration | 5 | 2 | (40) | 0.72 | (0.2–2.2) | 0.54 | |
| Caseous pneumonia | 2 | 1 | (50) | 0.90 | (0.2–3.7) | 0.99 | |
| Disease location | Unilateral | 184 | 152 | (83) | ref | ||
| Bilateral | 17 | 11 | (65) | 0.78 | (0.5–1.1) | 0.07 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakmamatov, K.; Kuznetsova, Y.; Istamov, K.; Shauer, D.; Tripathy, J.P.; Harries, A.D.; Osmonaliev, K.; Goncharova, O. The Trend, Characteristics and Treatment Outcomes in Patients with Tuberculosis Undergoing Thoracic Surgery in the Kyrgyz Republic between 2017 and 2021. Trop. Med. Infect. Dis. 2023, 8, 393. https://doi.org/10.3390/tropicalmed8080393
Sakmamatov K, Kuznetsova Y, Istamov K, Shauer D, Tripathy JP, Harries AD, Osmonaliev K, Goncharova O. The Trend, Characteristics and Treatment Outcomes in Patients with Tuberculosis Undergoing Thoracic Surgery in the Kyrgyz Republic between 2017 and 2021. Tropical Medicine and Infectious Disease. 2023; 8(8):393. https://doi.org/10.3390/tropicalmed8080393
Chicago/Turabian StyleSakmamatov, Konushbek, Yulia Kuznetsova, Kylychbek Istamov, Daniil Shauer, Jaya Prasad Tripathy, Anthony D. Harries, Kudaibergen Osmonaliev, and Olga Goncharova. 2023. "The Trend, Characteristics and Treatment Outcomes in Patients with Tuberculosis Undergoing Thoracic Surgery in the Kyrgyz Republic between 2017 and 2021" Tropical Medicine and Infectious Disease 8, no. 8: 393. https://doi.org/10.3390/tropicalmed8080393
APA StyleSakmamatov, K., Kuznetsova, Y., Istamov, K., Shauer, D., Tripathy, J. P., Harries, A. D., Osmonaliev, K., & Goncharova, O. (2023). The Trend, Characteristics and Treatment Outcomes in Patients with Tuberculosis Undergoing Thoracic Surgery in the Kyrgyz Republic between 2017 and 2021. Tropical Medicine and Infectious Disease, 8(8), 393. https://doi.org/10.3390/tropicalmed8080393









