4. Discussion
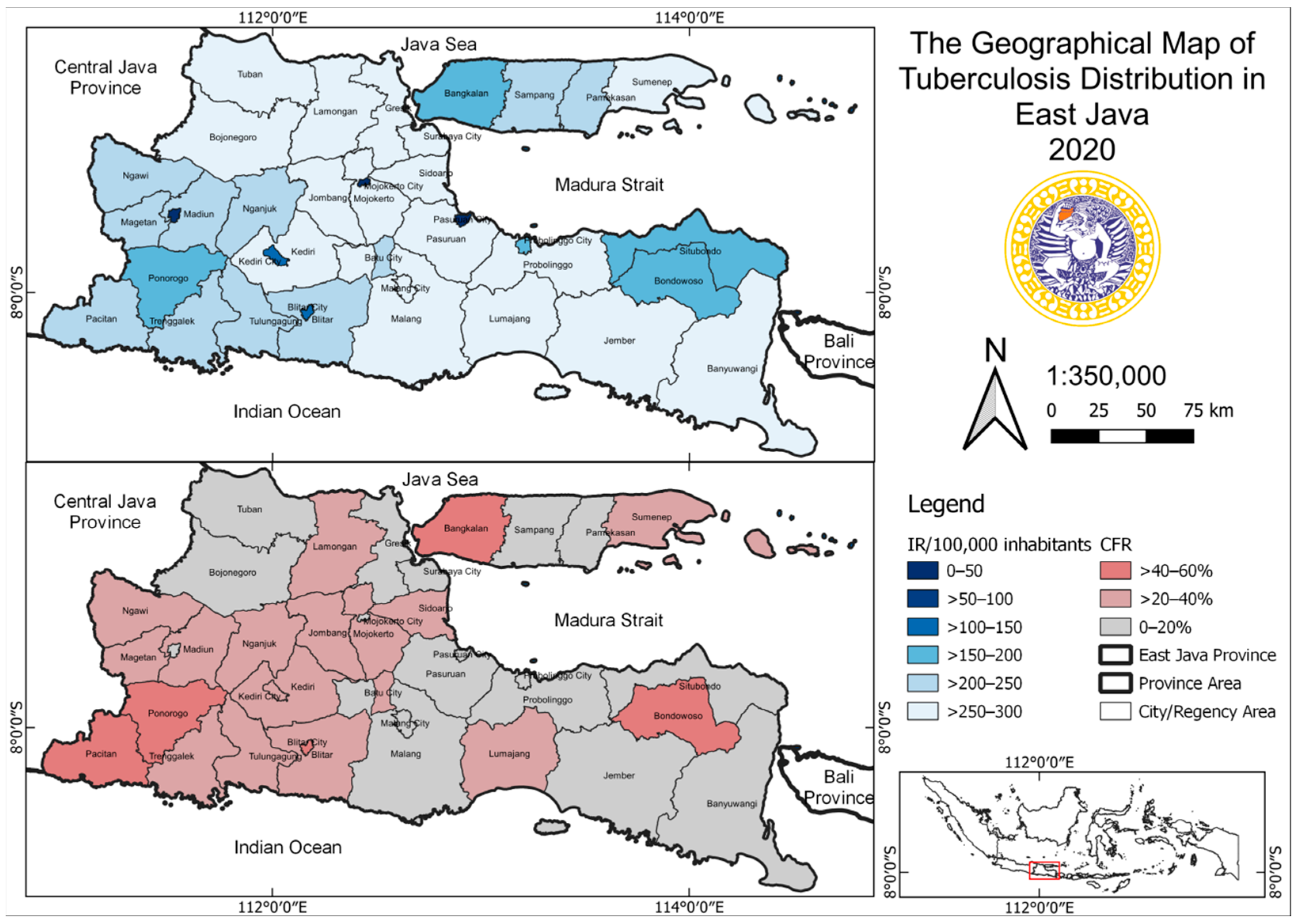
This study showed no significant correlation between the incidence rate and case fatality rate for tuberculosis (
p = 0.912;
p < 0.05). The incidence rate of tuberculosis in East Java Province (586.24/100,000 inhabitants) in 2020 was higher than the national incidence rate (301/100,000 inhabitants). Furthermore, there was a decreasing incidence rate of tuberculosis in 2020 (95.49/100,000 inhabitants) compared to that in 2019 (95.925/100,000 inhabitants) [
7]. The global incidence rate of tuberculosis in 2020 was 127/100,000 inhabitants [
8]. This showed that the incidence rate in East Java needs to be properly managed. Meanwhile, one of the global milestones proposed by the World Health Organization (WHO) in 2020 is the reduction in incidence rate and tuberculosis deaths by 20% and 35%, respectively [
8]. The overall case fatality rate of tuberculosis in East Java Province in 2020 was 3.6/100,000 inhabitants, while in 2019, it was 3.8/100,000 inhabitants [
6].
The decrease in the incidence rate of tuberculosis was also in line with another report, where the global data showed a decline in three of the six WHO regions, namely Southeast Asia, the Eastern Mediterranean, and the Western Pacific. In 2020, Indonesia was one of the eight countries that reported a high TB rate, with an estimated incidence of, (1) India (26%), (2) China (8.5%), (3) Indonesia (8.4%), (4) the Philippines (6.0%), (5) Pakistan (5.8%), (6) Nigeria (4.6%), (7) Bangladesh (3.6%), and (8) South Africa (3.3%). The results showed that the incidence of tuberculosis was higher in men than in women. This is in line with the global data in 2020, which showed a tuberculosis rate of 56% in men, 33% in women, and 11% in children [
8]. Moreover, these values were also obtained in the national tuberculosis survey in Vietnam [
9].
The elimination of tuberculosis depends on the treatment success rate of infected people. In this study, some regencies in East Java with were discovered to have a TSR value below the target (<90%). A total of 20 regencies with a TSR of below 90% need to benefit from public health promotion and sensitize tuberculosis patients to complete their treatment. Indonesia can adopt one of the efforts used to increase the treatment success/completion rate in India through Private Provider Interface Agencies (PPIAs). In India, the effort was effective in increasing tuberculosis notification rates, testing, and treatment success rates [
10,
11]. PPIAs can provide interventions related to patient care, training physicians, tuberculosis diagnostics, treatment monitoring, and tuberculosis medicines [
12].
Tuberculosis and COVID-19 are airborne diseases; the infection affects the lungs and has similar symptoms. Moreover, COVID-19 symptoms include fever or chills, cough, shortness of breath or difficulty breathing, fatigue and headache, muscle or body aches, loss of new taste or smell, sore throat, stuffy or runny nose, nausea, vomiting, and diarrhea. Meanwhile, tuberculosis symptoms are coughing up phlegm or blood, a cough that lasts more than 2 months, appetite and weight loss, chest pain, chills, fever or night sweats, and fatigue [
13]. Previous studies have demonstrated an association between tuberculosis and COVID-19. Both active and a previous history of tuberculosis seem to be related to an increased risk for the development of COVID-19, and aggravate the prognosis of infection [
11,
14,
15,
16,
17,
18]. The damage caused by TB infection in the lungs exacerbates its impact on local immunity and increases the body’s susceptibility to airborne pathogens [
19]. This increases the risk of COVID-19 developing in patients with a current or previous history of TB. Tuberculosis was found to be associated with a 2.10-fold increase in the risk of severe COVID-19 disease. In patients with previous respiratory disease, lung function can be impaired and a low resistance to viral infections can form, which can develop into acute respiratory distress syndrome (ARDS) [
20,
21].
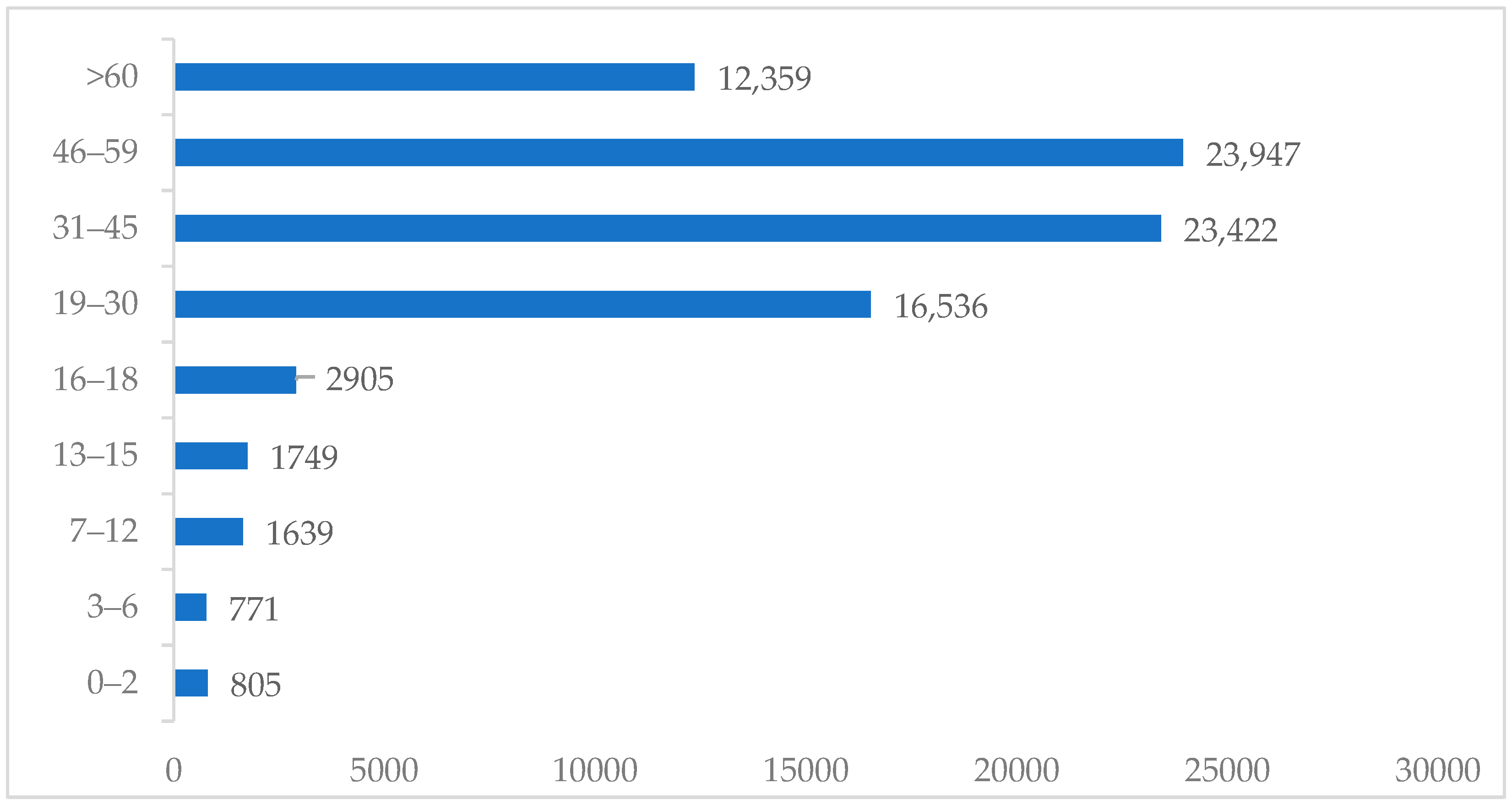
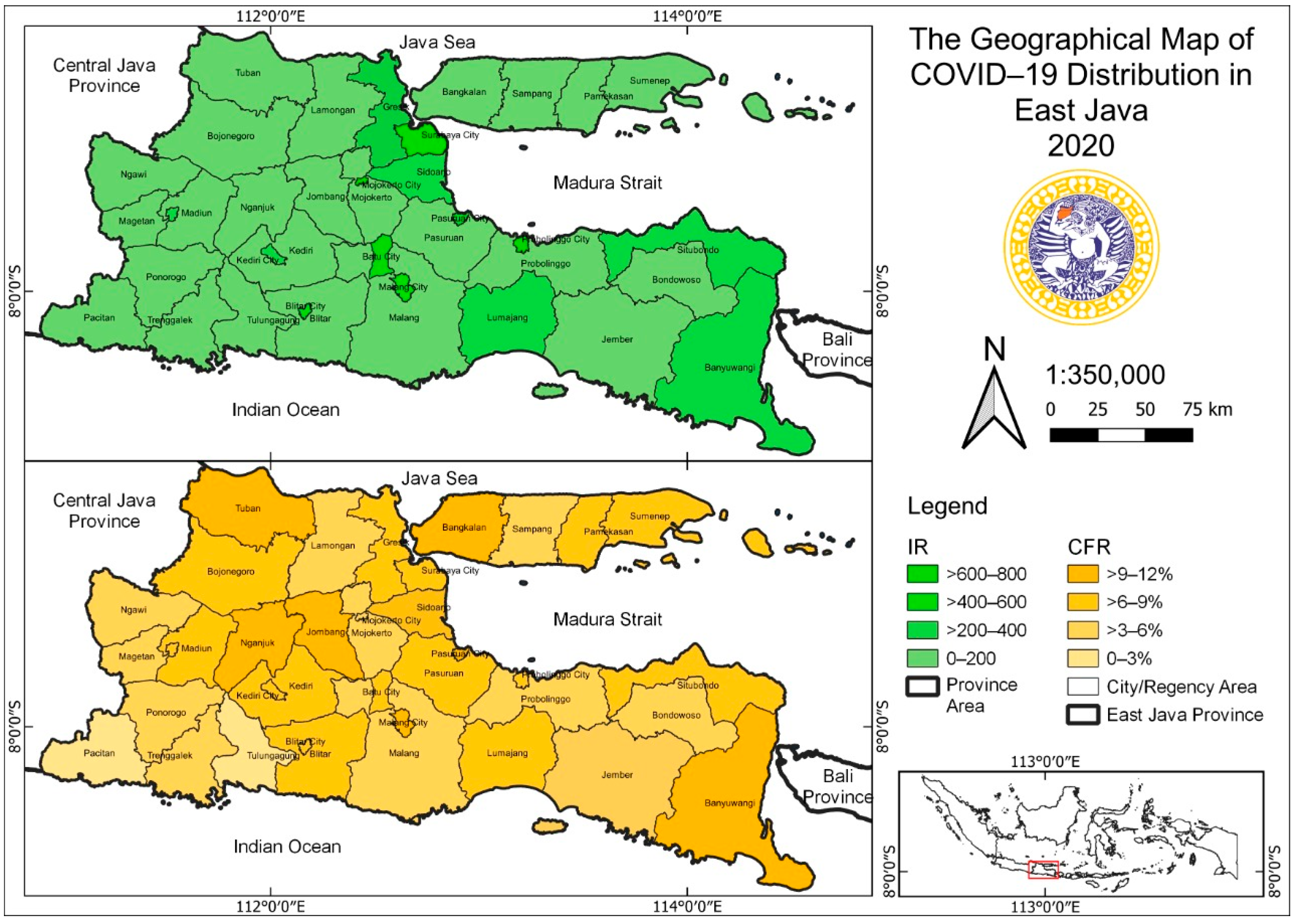
In 2020, when all countries were affected by COVID-19, it was reported that there were 84,140 cases in East Java, Indonesia, where the number of infected females was higher than the number for males. This was not in line with the report from Peru, where the incidence rate in females was higher than in that males. COVID-19 can affect any age group due to its fast transmission rate; however, this study discovered that the highest incidence rate was in the age group between 46 and 59 years old. This was in line with the national survey in Peru, where the highest incidence was in people older than 50 years [
22].
The elimination of tuberculosis has three pillars and components, namely: (1) integrated, patient-centered care, and prevention, (2) bold policies and supportive systems, (3) and intensified research and innovation. The first pillars can be translated into four activities: (a) early diagnosis of tuberculosis, including testing on universal drug susceptibility, screening of close contact groups, (b) treating and supporting people with tuberculosis to complete their treatment, (c) collaborative care that manages the comorbidities, (d) preventive treatment of people at high risk [
8].
COVID-19 and tuberculosis data showed that there is a possibility of coinfection in a patient, where an individual can simultaneously be affected by both illnesses. However, the limitation of this study is its inability to capture co-infected patients or those who are only infected with one of the diseases. Therefore, clinicians should be concerned with chronic diseases in patients, such as coinfection with both COVID-19 and tuberculosis. This is because the coinfection with both diseases was already reported by studies in China [
23,
24], USA [
25], and Italy [
15,
26], with various clinical characteristics.
Coinfection between tuberculosis and COVID-19 could have an important impact on the public health sector. In another case, public health also has an important role in combatting COVID-19 through various interventions, including physical distancing, self-quarantine, travel restrictions, a semi-lockdown, practicing good personal hygiene, eating nutritious food, increasing case-tracking, and vaccine development [
27]. People with underlying respiratory diseases should be considered during the pandemic, to prevent its exacerbation [
28].
Lung macrostructural changes caused by pulmonary tuberculosis affect the function and defence of the lower respiratory tract. This condition can be complicated due to the consequences of the inflammatory response exacerbated by SARS-CoV-2, such as oedema [
18,
29,
30]. The reported complications of tuberculosis with COVID-19 coinfection that are hypoxemia, respiratory failure, acute respiratory distress syndrome (ARDS), the need for non-invasive ventilation, glucose abnormalities, and longer lengths of hospital stay, with a maximum of 130 days, and recurrent or concurrent bacterial infections [
19,
31,
32,
33,
34]. The risk of recovery in COVID-19 patients with tuberculosis is 25% lower [
16]. Meanwhile, the risk of mortality for COVID-19 patients with early treatment of pulmonary tuberculosis is 2.5 times higher, and a previous history of tuberculosis has a 50% higher mortality risk [
17].
Previous studies showed that pulmonary tuberculosis patients had an increased susceptibility to COVID-19 infection and showed an increase in the severity of symptom development [
14]. Cumulative research has reported 80 pulmonary tuberculosis patients with COVID-19 coinfection from China, India, Belgium, Brazil, France, Italy, Russia, Spain, Switzerland and Singapore. The highest case of tuberculosis sufferers presenting with COVID-19 coinfection occurred in Italy [
35].
One of the principal efforts to suppress the transmission of tuberculosis in a community is the active case finding (ACF). Case finding could be deciphering this kind of activity, including house-to-house surveys, massive surveillance, increasing case-finding, and out-patient case detection, specifically in high-risk groups [
36]. Historical results showed that mass radiography could screen 2000 cases in over 2 million individuals [
37]. Sufficient case finding could lead to the successfully treatment of tuberculosis. In certain cases, case-finding could also find HIV-TB-coinfected patients, as mentioned in Nigeria, which could locate 109 HIV-TB infected patients. In Nigeria, successful treatment was proven to be associated with newly registered patients [
38].
Health facilities were also a predictor of the treatment success rate for tuberculosis. According to this, intersectoral collaborations with the private sector should be increased. As in another report, private health facilities had a more successful treatment rate than public health facilities [
39,
40]. The other challenge in tuberculosis management was drug resistance; interestingly, if the treatment success rate reaches 85%, this could lead to a reduction in transmission, drug resistance, TB prevalence, and TB incidence. In East Java Province, the number of health facilities, specifically primary health centers, is 968 units. However, not all primary health centers have the same capacity to tackle tuberculosis, especially during the pandemic, when the all the health facilities were focused on COVID-19. In addition, Indonesia also had an endemic for another tropical disease, which was neglected [
41].
Drug resistance in tuberculosis become a challenge in TB management, due to the increasing number of mechanisms that were involved. This phenomenon led to difficultes in the development of diagnostic procedures. However, whole-genome sequencing (WGS) may can help to identify polymorphisms related to drug resistance. In another case, the capacity of laboratories which can conduct WGS in developing countries is still limited [
42]. During the pandemic, whole-genome sequencing (WGS) was introduced, specifically to understand the new variant of COVID-19, which continuously increased. According to the latest information, the COVID-19 variants can be classified into three groups, namely, variants of concern (VOC), variants of interest (VOI) and high-consequence variants (VOHC). This classification was formulated according to the capacity and the impact on global public health [
41].