Community Awareness on Rabies Prevention and Control in Bicol, Philippines: Pre- and Post-Project Implementation
Abstract
1. Introduction
2. Methods
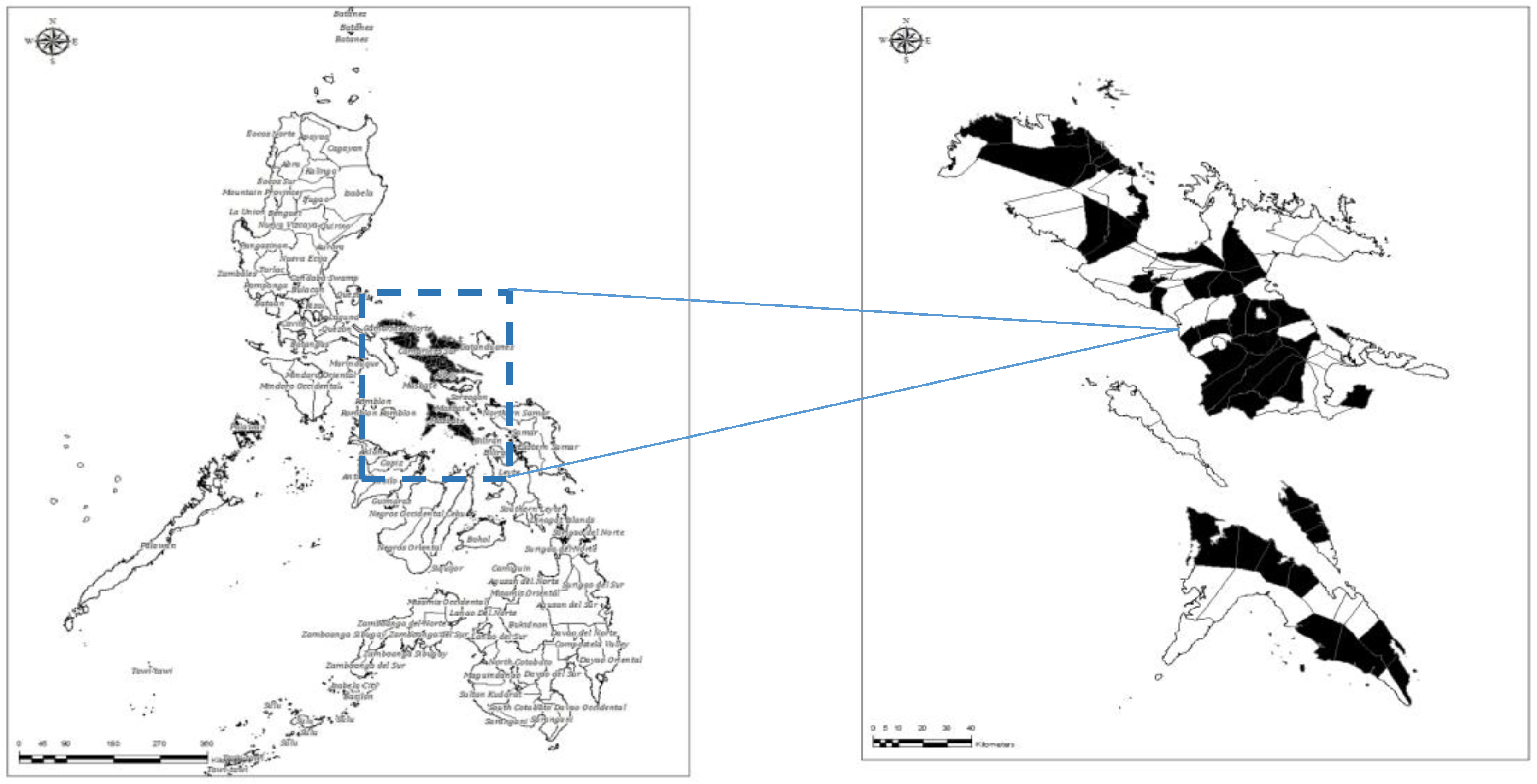
2.1. Study Area
2.2. Study Design and Sample Size
2.3. Data Collection and Analysis
3. Results
3.1. Socio-Demographic Profile of Respondents
3.2. Knowledge on Rabies, Species Affected, and Clinical Signs
3.3. Transmission of Rabies, Its Prevention, and Presence of Government Rabies Programs
3.4. Dog Ownership and Attitude towards Biting Incidents
3.5. Attitude towards Suspect Rabid Animal Sightings
3.6. Duties of Owner towards Pets
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Funding
References
- Hampson, K.; Coudeville, L.; Lembo, T.; Sambo, M.; Kieffer, A.; Attlan, M.; Barrat, J.; Blanton, J.D.; Briggs, D.J.; Cleaveland, S.; et al. Estimating the global burden of endemic canine rabies. PLoS Negl. Trop. Dis. 2015, 9, e0003709. [Google Scholar]
- Salahuddin, N.; Gohar, M.A.; Baig-Ansari, N. Reducing cost of rabies post-exposure prophylaxis: experience of a tertiary care hospital in Pakistan. PLoS Negl. Trop. Dis. 2016, 10, e0004448. [Google Scholar] [CrossRef] [PubMed]
- Lankester, F.; Hampson, K.; Lembo, T.; Palmer, G.; Taylor, L. Infectious diseases: implementing Pasteur’s vision for rabies elimination. Science 2014, 345, 1562–1564. [Google Scholar] [CrossRef] [PubMed]
- Lembo, T.; Hampson, K.; Kaare, M.T.; Ernest, E.; Knobel, D.; Kazwala, R.R.; Haydon, D.T.; Cleaveland, S. The feasibility of canine rabies elimination in Africa: dispelling doubts with data. PLoS Negl. Trop. Dis. 2010, 4, e626. [Google Scholar] [CrossRef] [PubMed]
- OIE ASEAN. Rabies Elimination Strategy. 2015. Available online: http://vncdc.gov.vn/files/article_attachment/2015/3/endorsed-ares-final.pdf (accessed on 13 December 2017).
- Rabies Prevention and Control Program. 2016. Available online: http://www.doh.gov.ph/national-rabies-prevention-and-control-program (accessed on 11 December 2017).
- Republic of the Philippines-13th Congress. 2007. Republic Act 9482: Anti-Rabies Act of 2007. Available online: http://www.officialgazette.gov.ph/downloads/2007/05may/20070525-RA-9482-GMA.pdf (accessed on 12 December 2017).
- World Health Organization. 2012. Strategic Framework for Elimination of Human Rabies Transmitted by Dogs in the South-East Asia Region. Available online: http://www.searo.who.int/entity/emerging_diseases/links/Zoonoses_SFEHRTD-SEAR.pdf (accessed on 11 December 2017).
- World Health Organization. 2001. Strategies for the Control and Elimination of Rabies in Asia. Available online: http://apps.who.int/rabies/en/Strategies_for_the_control_and_elimination_of_rabies_in_Asia.pdf (accessed on 13 December 2017).
- Hergert, M.; Nel, L.H. Dog bite histories and response to incidents in canine rabies-enzootic KwaZulu-Natal, South Africa. PLoS Negl. Trop. Dis. 2013, 7, e2059. [Google Scholar] [CrossRef] [PubMed]
- Herbert, M.; Riyaz Basha, S.; Thangaraj, S. Community perception regarding rabies prevention and stray dog control in urban slums in India. J. Infect. Public Health 2012, 5, 374–380. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Expert Consultation on Rabies: First Report; WHO Technical Report Series 931; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Herzog, H.A. Gender differences in human-animal interactions: A review. Anthropozoos 2007, 20, 7–21. [Google Scholar] [CrossRef]
- Global Alliance for Rabies Control. 2017. Country Support-Philippines. Available online: https://rabiesalliance.org/networks/country-support/philippines (accessed on 14 December 2017).
- Madhusudana, S.N.; Sukumaran, S.M. Antemortem diagnosis and prevention of human rabies. Ann. Indian Acad. Neurol. 2008, 11, 3–12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. 2013. WHO Regional Office for Southeast Asia: Frequently Asked Questions. Available online: https://www.who.int/rabies/resources/SEA_CD_278_FAQs_Rabies.pdf (accessed on 14 December 2017).
- Digafe, R.T.; Kifelew, L.G.; Mechesso, A.F. Knowledge, attitudes and practices towards rabies: Questionnaire survey in rural household heads of Gondar Zuria District, Ethiopia. BMC Res. Notes 2015, 8, 400. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control. 2015. Rabies vaccination. Available online: https://www.cdc.gov/rabies/specific_groups/veterinarians/vaccination.html (accessed on 16 December 2017).
- Morters, M.K.; McNabb, S.; Horton, D.L.; Fooks, A.R.; Schoeman, J.P.; Whay, H.R.; Wood, J.L.N.; Cleaveland, S. Effective vaccination against rabies in puppies in rabies endemic regions. Vet. Rec. 2015, 177, 150. [Google Scholar] [CrossRef] [PubMed]
- Seghaier, C.; Cliquet, F.; Hammami, S.; Aouina, T.; Tlatli, A.; Aubert, M. Rabies mass vaccination campaigns in Tunisia: Are vaccinated dogs correctly immunized? Am. J. Trop. Med. Hyg. 1999, 61, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.; Chowdhury, S.; Haider, N.; Bhowmik, R.K.; Rana, M.D.S.; Prue Marma, A.S.; Hossain, M.B.; Debnath, N.C.; Ahmed, B.-N. Awareness of rabies and response to dog bites in a Bangladesh community. Vet. Med. Sci. 2016, 2, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Li, S.; Xiang, H.; Pang, S.; Xu, G.; Schwebel, D.C. A multi-site study on knowledge, attitudes, beliefs and practice of child-dog interactions in rural China. Int. J. Environ. Res. Public Health 2013, 10, 950–962. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Pre-Implementation N = 1088 (%) | Post-Implementation N = 1380 (%) | p-Value |
|---|---|---|---|
| Profile | |||
| Father | 419 (38.5) | 524 (37.8) | 1.2777 |
| Mother | 453 (41.6) | 691 (50.0) | 0.00003 |
| Son/daughter | 178 (16.4) | 164 (11.8) | 1.9990 |
| Other | 38 (3.5) | 1 (0.07) | 2.0000 |
| Sex | |||
| Male | 464 (42.6) | 624 (45.2) | 0.1965 |
| Female | 624 (57.3) | 756 (54.7) | 1.8035 |
| Civil Status | |||
| Single | 199 (18.3) | 157 (11.3) | 2.0000 |
| Married | 776 (71.3) | 1097 (79.4) | 0.000003 |
| Separated | 11 (1.0) | 19 (1.3) | 0.4995 |
| Widower | 67 (6.2) | 81 (5.8) | 1.3223 |
| Live-in | 35 (3.2) | 26 (1.8) | 1.9739 |
| Educational Attainment | |||
| Did not go to school | 2 (0.2) | 4 (0.2) | 1.0000 |
| Elementary Level | 69 (6.3) | 93 (6.7) | 0.6915 |
| Elementary graduate | 181 (16.6) | 244 (17.6) | 0.5151 |
| High school level | 155 (14.2) | 216 (15.6) | 0.3357 |
| High school graduate | 305 (28.0) | 319 (23.1) | 1.9944 |
| Vocational graduate | 46 (4.1) | 64 (4.6) | 0.5516 |
| College level | 149 (13.7) | 188 (13.6) | 1.0571 |
| College graduate | 164 (15) | 231 (16.7) | 0.2545 |
| Postgraduate | 17 (1.6) | 10 (0.7) | 1.9665 |
| Parameter (Knowledge on Rabies) | Pre-Implementation N = 1088 (%) | Post-Implementation N = 1380 (%) | p-Value |
|---|---|---|---|
| Sources of Knowledge | |||
| Newspaper | 53 (4.9) | 64 (7.5) | 0.0143 |
| Radio | 255 (23.4) | 97 (11.4) | 2.0000 |
| Relatives | 116 (10.7) | 42 (4.9) | 2.0000 |
| Health workers | 205 (18.8) | 117 (13.8) | 1.9973 |
| Veterinarians | 49 (4.5) | 87 (10.2) | 0.0000 |
| TV | 489 (44.9) | 158 (18.6) | 2.0000 |
| Others (seminars, printed materials, barangay officials) | 183 (16.8) | 161 (19.0) | 0.1986 |
| Species affected with Rabies | |||
| Humans | 732 (67.3) | 406 (29.4) | 2.0000 |
| Cats | 264 (24.3) | 260 (19.0) | 2.0000 |
| Dogs | 587 (53.9) | 860 (62.3) | 0.0000 |
| Don’t know | 83 (7.6) | 177 (12.8) | 0.0000 |
| Others | 100 (9.2) | 36 (2.6) | 2.0000 |
| Signs of Rabies in dogs | |||
| Fear of water | 196 (18.0) | 277 (20.1) | 0.1245 |
| Aggressiveness | 174 (16.0) | 289 (20.9) | 0.0003 |
| Paralysis | 15 (1.4) | 36 (2.6) | 0.0135 |
| Convulsion | 17 (1.6) | 49 (3.6) | 0.0003 |
| Restlessness/delirium | 100 (9.2) | 152 (11.0) | 0.0840 |
| Salivation/drooling | 465 (42.7) | 334 (24.2) | 2.0000 |
| Loss of appetite | 73 (6.7) | 72 (5.2) | 1.9373 |
| Do not know | 235 (21.6) | 80 (5.8) | 2.0000 |
| Others | 372 (34.2) | ||
| Signs of rabies in humans | |||
| Fear of water | 277 (25.5) | 243 (17.6) | 2.0000 |
| Aggressiveness | 89 (8.2) | 224 (16.2) | 0.0000 |
| Paralysis | 28 (2.7) | 43 (3.1) | 0.4763 |
| Restlessness/delirium | 39 (3.6) | 279 (20.2) | 0.0000 |
| Salivation/drooling | 236 (21.7) | 250 (18.1) | 1.9919 |
| Loss of appetite | 60 (5.5) | 115 (8.3) | 0.0012 |
| Do not know | 320 (29.4) | 123 (8.9) | 2.0000 |
| Others (crazy, fever, convulsion) | 438 (40.3) | 201 (14.6) | 2.0000 |
| Parameter (Knowledge) | PRI N = 1088 (%) | POI N = 1380 (%) | p-Value |
|---|---|---|---|
| How can dogs acquire rabies? | |||
| Bitten by a rabid dog | 217 (19.9) | 525 (38.0) | 0.0000 |
| Eating dog meat | 14 (1.3) | 106 (7.7) | 0.0000 |
| Licked on broken skin | 29 (2.7) | 54 (3.9) | 0.0819 |
| Scavenging garbage | 256 (23.5) | 469 (34.0) | 0.0000 |
| Do not know | 369 (33.9) | 186 (13.5) | 2.0000 |
| Others (dirty food and environment) | 339 (31.2) | 40 (2.9) | 2.0000 |
| How can a person acquire rabies? | |||
| Bitten by a rabid dog | 704 (64.7) | 1097 (79.5) | 0.0000 |
| Eating dog meat | 52 (4.8) | 96 (7.0) | 0.0194 |
| Licked on broken skin | 27 (2.5) | 20 (1.4) | 1.9578 |
| Scavenging garbage | 30 (2.7) | 47 (3.4) | 0.3095 |
| Do not know | 232 (21.3) | 112 (8.1) | 2.0000 |
| Others (dirty environment) | 95 (8.7) | 8 (0.6) | 2.0000 |
| How to prevent Rabies? | |||
| Vaccination | 672 (61.8) | 1281 (92.8) | 0.0000 |
| Do not allow dogs to roam freely | 178 (16.4) | 84 (6.1) | 2.0000 |
| Others | 372 (34.2) | 15 (1.1) | 2.0000 |
| Do not know | 66 (6.1) | ||
| Frequency of vaccination (N = 672, N = 1281) | |||
| Every year | 500 (74.4) | 1273 (99.4) | 0.0000 |
| Every 6 months | 118 (17.6) | 83 (6.0) | 2.0000 |
| others | 54 (8.0) | 24 (1.7) | 2.0000 |
| Did you hear of any local ordinance? | |||
| Yes | 711 (65.4) | 824 (59.7) | 1.9963 |
| No | 377 (34.6) | 556 (40.3) | 0.0037 |
| What the local ordinance is all about? (N = 711, N = 824) | |||
| Local ordinance | 448 (63.0) | 749 (90.9) | 0.0000 |
| Responsible pet ownership | 148 (37.0) | 75 (9.1) | 2.0000 |
| Any presence of Rabies Program of the LGU? | |||
| Yes | 834 (76.7) | 1325 (96.0) | 0.0000 |
| No | 254 (23.3) | 55 (4.0) | 2.0000 |
| What the program is all about? (N = 834, N = 1325) | |||
| Dog vaccination | 777 (93.2) | 1192 (89.9) | 1.9916 |
| Rabies seminar | 51 (6.1) | 71 (5.4) | 1.5072 |
| Dog neutering | 1 (0.1) | 55 (4.2) | 0.0000 |
| Others | 5 (0.6) | 7 (0.5) | 1.2391 |
| Parameter | Pre-Implementation N = 1088 (%) | Post-Implementation N = 1380 (%) | p-Value |
|---|---|---|---|
| Number of dogs owned | |||
| 1–2 | 868 (79.8) | 1134 (82.2) | 0.1304 |
| 3–4 | 183 (16.8) | 205 (14.9) | 1.8021 |
| 5 and above | 37 (3.4) | 41 (2.9) | 1.5192 |
| Vaccination History (N = 2193, N = 2421) | |||
| 2015 | 1272 (58.0) | 890 (36.8) | 2.0000 |
| 2016 | 1300 (54.0) | ||
| 2017 | 890 (36.8) | ||
| Biting Incidence | |||
| Yes | 225 (20.7) | 292 (21.2) | 0.7618 |
| No | 863 (79.3) | 1088 (78.8) | 1.2382 |
| Owner of biting dog | |||
| Owner’s dog itself | 116 (51.6) | 102 (35.0) | 1.9999 |
| Stray with owner | 77 (34.2) | 117 (40.1) | 0.1544 |
| Stray without owner | 50 (22.2) | 72 (18.5) | 1.6944 |
| Others | 5 (2.2) | 1 (0.4) | 1.9533 |
| First aid adopted | |||
| Washed with soap | 186 (82.7) | 150 (51.4) | 2.0000 |
| Applied with garlic | 38 (16.9) | 24 (8.2) | 2.0000 |
| Visited ‘tandok‘ | 64 (28.6) | 63 (21.6) | 1.9957 |
| Did nothing | 24 (10.5) | 12 (4.1) | 2.0000 |
| Consulted Animal Bite Treatment Center | 116 (51.6) | 113 (38.7) | 2.0000 |
| Others | 20 (8.9) | 38 (13.9) | 0.0040 |
| Action done to the biting dog (N = 225, N = 292) | |||
| Observed | 58 (25.8) | 95 (32.5) | 0.0980 |
| Killed instantly | 20 (8.9) | 34 (11.6) | 0.3196 |
| Killed and head brought to laboratory | 1 (0.4) | 3 (1.0) | 0.4401 |
| Did nothing | 139 (61.8) | 154 (52.7) | 1.9616 |
| Others | 7 (3.11) | 6 (2.0) | 1.5758 |
| Parameter | PRI N = 1088 (%) | POI N = 1380 (%) | p-Value |
|---|---|---|---|
| What to do if animal develops symptoms of rabies | |||
| Immediately kill the dog | 220 (20.2) | 189 (13.7) | 2.0000 |
| Report to authority | 286 (26.3) | 871 (63.1) | 0.0000 |
| Capture & observe | 46 (4.2) | 183 (13.3) | 0.0000 |
| Do Nothing | 147 (13.5) | 83 (6.0) | 2.0000 |
| Others | 389 (35.8) | 54 (3.9) | 2.0000 |
| Where to report suspect animals? (N = 286, N = 871) | |||
| Provincial Vet Office | 27 (9.5) | 133 (15.3) | 0.0137 |
| Barangay Officials | 192 (67.3) | 696 (79.9) | 0.0000 |
| Police | 5 (1.9) | 3 (0.3) | 1.9954 |
| City/Municipal Agriculture Office | 25 (8.6) | 28 (3.2) | 1.9998 |
| Rural Health Unit | 17 (6.0) | 8 (0.9) | 2.0000 |
| Others | 25 (8.6) | 3 (0.3) | 2.0000 |
| Parameter | Pre-Implementation N = 1088 (%) | Post-Implementation N = 1380 (%) | p-Value |
|---|---|---|---|
| How should dog be taken care of? | |||
| Submit dogs for vaccination | 379 (34.8) | 1083 (78.5) | 0.0000 |
| Do not allow dogs to roam freely | 310 (28.5) | 360 (26.1) | 1.9463 |
| Register dogs | 84 (7.7) | 134 (9.7) | 0.0082 |
| Provide dogs with shelter/food | 309 (28.4) | 854 (61.9) | 0.0000 |
| Others (provide vitamin supplements, bathe regularly) | 351 (32.3) | 77 (5.6) | 2.0000 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barroga, T.R.M.; Basitan, I.S.; Lobete, T.M.; Bernales, R.P.; Gordoncillo, M.J.N.; Lopez, E.L.; Abila, R.C. Community Awareness on Rabies Prevention and Control in Bicol, Philippines: Pre- and Post-Project Implementation. Trop. Med. Infect. Dis. 2018, 3, 16. https://doi.org/10.3390/tropicalmed3010016
Barroga TRM, Basitan IS, Lobete TM, Bernales RP, Gordoncillo MJN, Lopez EL, Abila RC. Community Awareness on Rabies Prevention and Control in Bicol, Philippines: Pre- and Post-Project Implementation. Tropical Medicine and Infectious Disease. 2018; 3(1):16. https://doi.org/10.3390/tropicalmed3010016
Chicago/Turabian StyleBarroga, Toni Rose M., Ilene S. Basitan, Themis M. Lobete, Rona P. Bernales, Mary Joy N. Gordoncillo, Emelinda L. Lopez, and Ronello C. Abila. 2018. "Community Awareness on Rabies Prevention and Control in Bicol, Philippines: Pre- and Post-Project Implementation" Tropical Medicine and Infectious Disease 3, no. 1: 16. https://doi.org/10.3390/tropicalmed3010016
APA StyleBarroga, T. R. M., Basitan, I. S., Lobete, T. M., Bernales, R. P., Gordoncillo, M. J. N., Lopez, E. L., & Abila, R. C. (2018). Community Awareness on Rabies Prevention and Control in Bicol, Philippines: Pre- and Post-Project Implementation. Tropical Medicine and Infectious Disease, 3(1), 16. https://doi.org/10.3390/tropicalmed3010016





